PRINCIPLES OF DIFFUSION OF GASES
advertisement

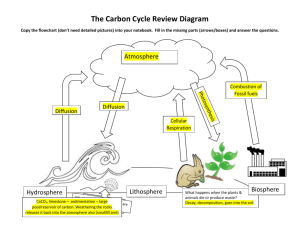
PRINCIPLES OF DIFFUSION OF GASES LEARNING OBJECTIVES At the end of the lecture ,student should be able to understand the basic concepts of, • Gas Exchange • Mixed Gases and Partial Pressure • Physical Principles of Gas Exchange • Mechanisms of Gas Movement • Bulk flow principles • Diffusion of gases • Gas Laws • Diffusion coefficient • Diffusion Capacity • Factors affecting rate of diffusion Gas Exchange • Gas Exchange in the respiratory system refers to diffusion of O2 & CO2 in the lungs and in the peripheral tissues . • O2 is transferred from alveolar gas into pulmonary capillary blood and ultimately, delivered to the tissues, where it diffuses from systemic capillary blood into the cells. • CO2 is delivered from the tissues to venous blood, to pulmonary capillary blood and is transferred to alveolar gas to be expired. Gas Exchange • Alveoli supplied with oxygen; carbon dioxide removed from bloodstream • Occurs on respiratory membrane • Depends on: – Partial pressures of gases involved – Diffusion of molecules from gas into a liquid Gas Exchange Mixed Gases and Partial Pressures • Atmospheric pressure at sea level = 760 mm Hg • Atmosphere made up of different gases – One gas alone makes up partial pressure • Sum of all partial pressures = atm pressure • Partial pressure determines rate of diffusion Physical Principles of Gas Exchange • Diffusion of gases through the respiratory membrane Depends on – membrane’s thickness, – the diffusion coefficient of gas, – surface areas of membrane, – partial pressure of gases in alveoli and blood Relationship between ventilation and pulmonary capillary flow – Increased ventilation or increased pulmonary capillary blood flow increases gas exchange – Physiologic shunt is deoxygenated blood returning from lungs Physical Principles of Gas Exchange • • Partial pressure – The pressure exerted by each type of gas in a mixture – Dalton’s law – Water vapor pressure Diffusion of gases through liquids – Concentration of a gas in a liquid is determined by its partial pressure and its solubility coefficient – Henry’s law Mechanisms of Gas Movement • • Bulk Flow (convection) Diffusion Transition from bulk flow to diffusion • Respiratory bronchioles – Transition from bulk flow to diffusion • Alveolar Ducts and Alveoli – Diffusion the sole mode for gas movement. – Different gases diffuse at different rates – Diffusion forces – contribute to net movement of O2 and CO2 across the alveolar-capillary membrane. Terminal Bronchiole (Transition from bulk flow to diffusion). DIFFUSION • Random movement of molecules from higher concentration to lower concentration is called gas diffusion. • Some molecules also bound to move from lower to higher concentration. • Simple diffusion occurs at two levels: 1- lipid bilayer 2- protein channels • Exchange of oxygen and CO2 across cell membrane and capillary wall occurs by simple diffusion. • They are lipid soluble so they have high rate of diffusion across the cell membrane. • These high rate can be attributed to the large surface area for diffusion provided by the lipid component of the membrane. Bulk flow Principles • Movement of gas mixtures from a region of high pressure to one of low pressure. • Gases always diffuse in the direction of lower partial pressure but not always in the direction of lower conc. • All gases move together because they are subjected to the same pressure head. Bulk Flow and Breathing • Inspiration: Alveolar pressure becomes sub-atmospheric. Air “pushed” (sucked?) into lungs. • Expiration: Alveolar pressure becomes supraatmospheric. Air “pushed” out of lungs. Changes in Partial Pressures Gas laws • General gas law: the product of pressure times volume of a gas is equal to the number of moles of the gas multiplied by gas constant and temperature. PV = nRT • Where P = pressure (mm Hg) v = volume n = moles (mol) R = gas constant T = temperature (k) Dalton’s law of partial pressure • It states that the partial pressure of a gas in a mixture of gases is the pressure that gas would exert if it occupied the total volume of the mixture. • The pressure of a specific gas in a mixture is called its partial pressure (Px). • Thus the partial pressure is the total pressure multiplied by the fractional conc. Of dry gas. Px = PB x F • The relationship for humidified gas is determined by correcting the barometric pressure for the water vapor pressure. Thus , Px = (PB – PH2O) x F Where : Px = partial pressure of gas (mm Hg) PB = barometric pressure (mm Hg) PH2O = water vapor pressure at 370C (47 mmHg) F = fractional conc. of gas (no unit) Atmospheric pressure • • • Airflow is governed by the same principles of flow, pressure and resistance as blood flow. The pressure that drives respiration is atmospheric (barometric) pressure- the weight of air above us. The pressure, called 1 atmosphere (1atm), is enough to force a column of mercury 760 mm up an elevated column. 1 atm = 760 mmHg This is the average atmospheric pressure at sea level ; fluctuate from day to day and is lower at high altitude. • Atmospheric air is a mixture of gases • Oxygen, nitrogen, CO2, water vapor, plus other gases present in small quantities. • Atmospheric pressure is the sum of the pressures of all these gases: = PN2+ PO2 +PH2O + PCO2 +P other gases • Partial pressure of gases in inhaled air: • • • • • • PN2 = 0.786 X 760 = 597.4 mm Hg PO2 = 0.209 X 760 = 158.8 mmHg PH2O = 0.004 X 760 = 3.0 mmHg PCO2 = 0.0004 X 760 = 0.3 mmHg P other gases =0.0006 x 760 = 0.5mmHg. Total pressure = 760.0 mmHg The percentages of gases • The percentages of gases in dry air at a barometric • • • • pressure of 760 mmHg are: Oxygen = 21% (0.21) Nitrogen = 79% (0.79) CO2 = 0.04% (0) H2O vapor pressure = 47 mmHg at 37C. Partial pressure of gases in inhaled air • These partial pressures determine the movement of oxygen and CO2 between atmosphere and lungs, b/w lungs and blood, b/w blood and body cells. • The greater the difference in partial pressure, the faster the rate of diffusion. Relative pressure • • Matter to flow is the difference b/w atmospheric pressure and intrapulmonary pressure. Since atmospheric pressure vary from one place and time to another. • A relative pressure of -3mmHg means 3mmHg below atmospheric pressure ;a relative pressure of +3 mmHg above atmospheric pressure. • So at an atmospheric pressure of 760 mmHg these would represent absolute pressures of 757 and 763 mmHg, respectively. • • Henry’s law Henry law states that the quantity of gas that will dissolve in a liquid is proportional to the partial pressure of the gas and its solubility. Henry’s law is used to convert the partial pressure of gas in the liquid phase to the concentration of gas in the liquid phase (e.g., in blood). • The concentration of a gas in solution is expressed as volume percent (%), or volume of gas per 100ml of blood ( mL gas/100mL blood) Henry’s law: CX = PX x solubility Where: CX = concentration of dissolved gas (mLgas/100mLblood). • PX = partial pressure of gas (mm Hg). • Solubility = solubility of gas in blood (mL gas/100 mL blood/ mm Hg). • Conc. Of a gas in solution applies only to dissolved gas that is free in solution and it does not include any gas that is present in bound form. Diffusion of gases – Fick’law • Transfer of gases across cell membrane or capillary walls occurs by simple diffusion. Diffusion is described by Fick’s law of diffusion. • According to this law : • The rate of transfer by diffusion (VX) is directly proportional to the driving force, a diffusion coefficient(D) and the surface area available for diffusion(A); it is inversely proportional to the thickness of the membrane(T) • O 2 P 2 CO A 2 A D Vgas ( P1 P2 ) T P 1 T • Total AREA available for diffusion of gases is large in human ~50-100 m2 Diffusion PATH LENGTH is very small, <1 µm Diffusion of gases • the driving force for diffusion of gas is the partial pressure difference of the gas (P) across the membrane, not the conc. Difference. • the diffusion coefficient of a gas (D) depends on molecular weight, and the solubility of the gas. • Diffusion coefficient • Diffusion coefficient is defined as a constant, which is the measure of a dissolved substance diffusing through the conc. gradient. • The diffusion coefficient for CO2 is approximately 20 times higher than the oxygen. Diffusing Capacity of the Lung (DL) • • It is defined as the volume of gas that diffuses through the respiratory membrane each minute for a pressure gradient of 1 mmHg. DL combines the diffusion coefficient of the gas (D), surface area of the membrane (A) and the thickness of the membrane ( T). Diffusing Capacity (DL) lumps together: – Diffusivity – Area – Thickness From Fick Equation: Vgas A D DL T P1 P2 Diffusivity (D) D Solubility of gas molecular weight • Each gas has unique value • Essentially a diffusion coefficient DL for oxygen and CO2 • DL for oxygen is 21 ml/min/1mmHg • DL for CO2 is 400 ml/min/1mmHg • Thus DL for CO2 is 20 times more than that of oxygen. Factors affecting rate of diffusion 1- Partial pressure difference: Rate of diffusion is directly proportional to pressure difference Pressure diff is directly proportional to rate of diffusion. 2 - Solubility of gas: Rate of diffusion capacity is directly proportional to solubility of gas. Dgas Solubilitygas 3- Surface area available for gas exchange. Rate of diffusion is directly proportional to the surface area. 4 - Molecular weight of the gas: Rate of diffusion is inversely proportional to molecular weight of the gas. D gas = 1 GMW 5 - Thickness of respiratory membrane: It is inversely proportional to the thickness of the membrane Relation b/w DL and factors affecting • Rate of diffusion PxSxA Mw x D Where: • • • • • P = pressure difference S = solubility of gas A = surface area of membrane Mw = molecular weight D = thickness of membrane References Textbook of medical physiology by Guyton & Hall Review of medical physiology by W.F.Ganong Anatomy & physiology by Saladin