DRAFT
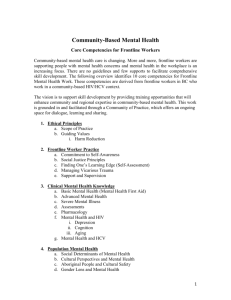
advertisement

#39 PROJECT NAME: Bridging the Gap: Safety Forums for Executive Teams and Frontline Staff Institution: UTHealth Science Center Houston/Children’s Memorial Hermann Hospital Primary Author: Caryn Douma MS, RN Secondary Author: Robert Yetman, MD Project Category: General Quality Improvement Purpose/Aim: Early detection of potential harm and improved communication and teamwork at all levels is critical to providing safe care. Current adverse event detection methods often fail to capture up to 90% of adverse and near miss occurrences for timely intervention or prevention. Multiple organizations have implemented executive rounding processes to improve relationships between frontline staff and physicians and senior leaders and increase reporting or recognition of potential safety events. Exposure to front line teams enables leaders to demonstrate their commitment to building a culture of quality and safety and increase transparency. A recent increase in the number of patients in the children’s hospital emergently transferred from the pediatric floors to the ICU led to a series of conversations with frontline staff and physicians in an attempt to understand potential failures leading to the change. Themes from the focus groups revealed a failure to recognize deterioration or reluctance to escalate concerns to appropriate personnel. The feedback was consistent with safety climate survey results from 2011 and 2012 that revealed opportunities for improvement (safety climate score < 80%, difficulty speaking up to attending physicians<60%, difficulty discussing errors <70%, leadership rounding impact < 70%). The purpose of our project was to design and implement an innovative process for frontline staff and physicians to have regular interaction with the executive team to discuss and resolve existing and potential patient safety concerns. The overall goal was to create an atmosphere of transparency to facilitate reporting of identified process and clinical care issues through a series of communication strategies. A formal process for meeting and closing the loop on identified concerns did not exist. The executive teams round regularly with frontline staff but many barriers are currently in place that limit effectiveness, The setting is a quaternary care, academic, fully integrated, 308-bed women’s and children’s hospital. Key stakeholders are: parents, patients and families, senior leadership, frontline staff and physicians. Global aim: Increase frontline staff and physician safety climate survey scores from a baseline of < 80% to > 80% in the Children’s hospital by March 2014 through the implementation of a communication bundle. Specific aim: Implement a standardized process for frontline staff and physicians to meet with the executive team to discuss and resolve existing and potential patient safety concerns before October 2013. Tools and Measurement: Focus groups with frontline staff and physicians were held Stakeholder analysis completed Fishbone exercise with frontline staff, leadership and physicians (see figure 1) Review of reported events obtained from the hospital event reporting system Driver Diagram (see figure 2) Pilot executive rounding Figure 1 Figure 2 Measures: Improvement in Safety Culture survey results pre and post intervention. o Goal: increase overall safety climate score > 80% for CMHH before March 2014, Increase leadership rounding impact scores to >80% before March 2014 100% of events identified through Leadership Forums will be reported back to staff and physicians with resolution or follow up plan Intervention and Improvement: Following review of pre-intervention data, and a pilot of executive rounding, our team determined that instead of creating a new process for executive team interaction, we would utilize existing meetings, interdisciplinary rounds and huddles where safety concerns are currently discussed but not recorded and resolved. The executive rounding pilot revealed numerous barriers to success including, difficulty scheduling executive team members, finding frontline staff and physicians free to interact, and unit geography that only allowed discussion with 5-10 staff members during each rounding interaction. This approach clearly would not impact overall culture or yield enough meaningful events to accomplish our aim. Our intervention included attendance of senior leadership representatives at 12 meetings designated as safety forums instead of random walk rounds. Team members present during the forums included frontline physicians, nursing staff, attending physicians, nursing leadership and supporting services. Each forum served as a PDSA cycle enabling our team to modify the format for maximum effectiveness. Multiple safety concerns and process issues were collected and rich discussion within the group enabled the senior leaders to better understand barriers and process issues interfering with optimal patient care delivery. Intervention Results: Twelve safety forums were held with over 200 frontline staff and physicians impacted. The executive team was able to interact with the groups and create a safe environment to discuss safety concerns. In total, over 100 issues were identified and resolved or referred to appropriate personnel for follow up. The graph below demonstrates results from three pediatric end of the month wrap up meetings. Resolution and action plans were presented back to the groups at subsequent meetings. Items requiring escalation and follow up were assigned to appropriate departments. Some issues were able to be resolved immediately by the executive team member present. Data are currently being collected in Excel and categorized by general content. A more robust database is in development phase and will enable our team to categorize, prioritize and build reports. More detailed results with number of categories, events and outcomes will be available prior to conference presentation. Safety climate survey results will not be available until March 2014 when the organizational survey results are released. . Revenue Enhancement /Cost Avoidance / Generalizability: Decreasing adverse events, waste and inappropriate use of resources, eliminating delays in care, improving care coordination, improving flow and eliminating healthcare associated infections and complications have been demonstrated to decrease cost and patient harm. We expect to be able to quantify avoidable delays in care, improvement in care coordination through decreased length of stay and other metrics with full implementation of our project and utilization of a more efficient database, currently in development. The finance department will assist with quantifying cost savings in the future. Conclusions and Next Steps: This project, when fully implemented, will be a model that can be utilized in other organizations to facilitate communication between senior leaders and frontline staff and physicians. Next steps will include assessment of current meetings and huddles to formalize the forum approach and scheduling senior leaders 6-12 months in advance. The database will assist with improving metrics and communicating formal reports to staff and leaders. In conclusion, we recognized that safety concerns are often discussed in many settings but not reliably recorded or escalated to the appropriate personnel. Executive leaders and frontline teams benefit from shared knowledge and discussion in Safety Forums and follow up processes ensure resolution and improved communication. Objectives: Identify the role of senior leadership in facilitating effective communication with frontline staff and physicians to increase event reporting and improve patient outcomes Demonstrate the impact of the Safety Forum approach to improve recognition and reporting of identified or potential safety events between senior leaders and frontline teams References: Resar RK, Griffin FA, Kabcenell A, Bones C. Hospital Inpatient Waste Identification Tool. IHI Innovation Series white paper. Cambridge, Massachusetts: Institute for Healthcare Improvement; 2011. (Available on www.IHI.org) 'Global Trigger Tool' Shows That Adverse Events In Hospitals May Be… Classen, David C;Resar, Roger;Griffin, Frances;Federico, Frank;Frankel, Terri;Kimmel, Nancy;et al. Al. Health Affairs; Apr 2011; 30, 4; ProQuest Nursing & Allied Health Source pg. 581 Yee PL, Edwards ML, Dixon J, Gleason NS. Implementation of Patient Safety Rounds in a Children’s Hospital.Nurs.Admin Q; 2009: Vol 33,148-53