ohr_asset_480077
advertisement

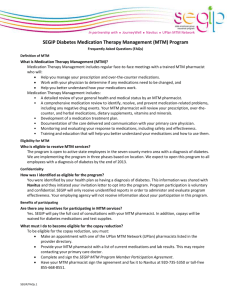
INFORMATION FOR PHARMACISTS’ PARTICIPATION IN THE STATE EMPLOYEE GROUP INSURANCE PROGRAM MTM DIABETES MANAGEMENT PROGRAM 1. 2. 3. 4. 5. 6. 7. DESCRIPTION OF PROGRAM PROGRAM GOALS BENEFIT DESIGN BILLING AND COMPENSATION FOR SERVICES PATIENT ENROLLMENT PHARMACIST MANAGEMENT OF PATIENT AND POPULATION DIABETES MTM LIFESTYLE PROGRAM 1. DESCRIPTION OF PROGRAM The State Employees Group Insurance Program (SEGIP) estimates that 6,000 state employees currently are diagnosed with diabetes. There are several health factors contributing to diabetes that when appropriately managed can improve the health of the members and reduce the cost to the plan. SEGIP has asked our network to assist their members in managing their diabetes and medication use. The UPlan MTM network, on behalf of the 150 participating pharmacist members, has negotiated a contract to provide medication management services to these State of Minnesota employees. This program will start on 1 May 2013. This will be a phased program, beginning with the seven-county Metro area, to be followed by greater Minnesota later in the year. In the first phase, Metro area employees (not family members) with a recorded diagnosis of diabetes will be invited to join the program through a letter and materials describing the SEGIP MTM Diabetes Management Program. As with our UPlan MTM design, the members are able to choose the network pharmacist they wish to use and will initiate their participation by contacting the pharmacist. 2. PROGRAM GOALS For this program we will focus on improving the D5 Goals developed by the Institute for Clinical Systems Improvement (ICSI), as a way to describe the five treatment goals of optimal diabetes care. The five goals that make up the D5 are: Blood pressure, less than 140/90 mmHG LDL is less than 100mg/dl A1c is less than 8% Tobacco free Aspirin, as appropriate UPlan MTM Network/State Diabetes Management Program-4-22-13 1 The purpose of this program is that all patients be at D5 goal. To achieve this, pharmacists will be asked to manage each patient to these goals. This will be a new challenge for many pharmacists: to not only manage the patient but also a defined population of all those members who have chosen your practice. 3. BENEFIT DESIGN This program is designed as an ongoing program with the ultimate goal of enabling the members to better manage their diabetes. To that end, the program recommended that a member meet two or three times during first year of participation (more often if necessary) and twice a year each subsequent year. It is coupled with a lifestyle program. The member, on completion of a lifestyle management program with Journeywell, will receive a $250 deposit to their HRA. The member is requested to bring a lab report from the physician to the first visit. The MTM pharmacist will assist members who don’t have current lab values by contacting their physician. These “base-line values” for the relevant lab values in the D5 will be reported to the network. At each subsequent visit the pharmacist will report these values to the network. This is the way we will track the performance. You will be advised as to the method for reporting these lab values. Please retain the D5 values in your records for each visit, to facilitate these reports at a later time. There are no copayments for the member for the MTM visits. Copayments for diabetes medications and supplies will be waived while a member actively participates in the program. 4. BILLING AND COMPENSATION FOR SERVICES Services will be billed using the same CPT codes as with UPlan (99605, 99606, 99607). Claims will be submitted electronically on a CMS1500 to the relevant carrier as shown on the member card: Preferred One, HealthPartners or Blue Cross. (Please note that MTM visit information for UPlan members will continue to be reported to Medica, and UPlan member enrollment forms faxed to Prime Therapeutics.) Pharmacist-provided services will be compensated in the same manner and with the same fee schedule as with the UPlan program. In addition this program will have a “pay for performance” aspect. Pay for performance, although common for many practitioners, is new for pharmacists. It is expected to be a part of many of the new systems to be developed as part of health-care reform initiatives. UPlan MTM Network/State Diabetes Management Program-4-22-13 2 The pay for performance amount will be keyed to movement toward D5 goals of all enrolled members, over 12 months – across all pharmacists. The network will retain a portion of this payment for administration of the performance system and then allocate the remaining performance payment to pharmacists or pharmacies based on individual performance. 5. MEMBER/PATIENT ENROLLMENT At the first visit, the SEGIP member will complete and bring to the appointment the “SEGIP Medication Therapy Management (MTM) Program Member Participation Agreement.” It should be noted that this Agreement has a section about “participant responsibilities.” After discussing the program and responsibilities with the member, the pharmacist should sign and fax the completed form to Navitus. Navitus will enter the copay waiver into the member’s record. Please advise the member that it may take up to seven business days for the waiver to be effective. The participation agreement and other documents related to the SEGIP Diabetes MTM Program will be available on line. They will be linked to our UPlan MTM provider site: www.umn.edu/ohr/benefits/pharmacy/mtmproviders/SEGIP. 6. PHARMACIST MANAGEMENT OF PATIENT AND POPULATION The pharmacist will conduct an MTM Comprehensive Medication Review at the first appointment with the enrolled member. In addition, the following needs to occur: 1. Document lab and other D5 values. Member has been requested to bring relevant lab values to first appointment. If the member does not have them the pharmacist will need to contact the physician. 2. Report D5 values to the network. (Mechanism to be provided.) 3. Establish future appointment – two or three in the first year and two annually thereafter are recommended. (Pharmacists will need to actively manage these appointments, as they are integral to the success of the program.) 4. At subsequent meetings the pharmacist will need to review progress toward goals and report current D5 values to the network. In managing the population that you are responsible for (all those members who have chosen your practice) the pharmacist will need to periodically review results of your entire group for outliers. It will be important to identify those who are having difficulty in progressing toward goals and work with them to achieve success. This is important because the program is based on progress for the entire group of members in a given pharmacy and the entire enrolled members in all pharmacies. UPlan MTM Network/State Diabetes Management Program-4-22-13 3 8. DIABETES MTM LIFESTYLE PROGAM As a part of the diabetes management program SEGIP has contracted with Journeywell®, a lifestyle coaching program, to further aid the members in managing their health. Enrollment and participation in the Diabetes Medication Therapy Management (MTM) program is required for participation. The members can earn $250 in their Health Reimbursement Account (HRA) by actively participating. The pharmacists should encourage their participation in the lifestyle management program through Journeywell®, as well as ongoing participation in the MTM program. The member can sign up with a health coach at 952-967-5128, 866-977-5128 or TTY 877-222-2794. Or log on to www.journeywell.com/SEGIP to enroll and identify themself as a SEGIP MTM program participant. To be eligible to earn the reward, they need to complete a lifestyle management program with a health coach or complete one of the online programs (10,000 steps, eStress or eWeight). UPlan MTM Network/State Diabetes Management Program-4-22-13 4