Pharmacology 9a – Drugs of the Heart
advertisement

Pharmacology 9a – Drugs of the Heart
Anil Chopra
1. To be able to describe the mechanisms regulating heart rate and contractility that
are therapeutic targets in the heart
2. To be able to describe the determinants of myocardial oxygen supply and demand
and how these are favourably influenced by
a. Beta blockers
b. Organic nitrates and potassium channel openers
c. Calcium antagonists
3. To know the major adverse effects of:
a. Beta blockers
b. Organic nitrates and potassium channel openers
c. Calcium antagonists
4. To know the basis of the Vaughan Williams classification and understand its
limitations
5. Know the major uses of and be able to describe the mechanisms of action of:
a. Adenosine
b. Verapamil
c. Amiodarone
d. Digoxin and cardiac glycosides
6. To be able to describe the mechanisms of action of cardiac inotropes and their
clinical uses
Control of Heart Rate and Contractility
Sympathetic Control of HR and Contractility:
Increased force of contraction – positive inotropic effects
Increased HR – positive chronotropic effect
Increased automaticity
Repolarisation and restoration of function following cardiac depolarisation
Reduced cardiac efficiency – oxygen consumption increased mores than cardiac work
Effects largely due to β1 activation
β1 activation stimulates adenyl cyclase → increased cAMP → increased intracellular
Ca+ due to effects on L-type calcium channels. Also stimulates Na/K ATPase in
cardiac Myocytes
Parasympathetic Control of HR and Contractility:
Cardiac slowing and reduced automaticity
Inhibition of Av conductance
Increased preload (venous return) increases force of contraction
Increased afterload (arterial circulation impedance) reduces stroke volume
Determinants of myocardial oxygen supply and demand
Myocardial ischaemia arises from an imbalance in oxygen supply and demand
Oxygen Supply:
Blood flow
O2 saturation
HR
Oxygen Demand:
HR
Preload
Afterload
Contractility
»
Beta-blockers prevent sympathetic effects on the heart, reduce demand and so
reduce angina
»
Organic nitrates act as venodilators, reduce venous return and preload and so
reduce cardiac work (Frank-Starling)
»
Potassium channel openers open KATP channels and so act as NO donors causing
venodilation and arterial dilation
»
Calcium antagonists inhibit L-type calcium channels causing arterial dilation
causing reduced afterload and so
reduced cardiac work
Targets of anti-anginals
Angina = myocardial ischaemia
Sympathetic NS
Myocardial oxygen supply
Myocardial oxygen demand
Beta blockers
Heart rate
Contractility
Coronary artery
constriction
CCB Nitrates
Venous tone
Coronary blood flow
Arterial O2 content
Heart Rate
Heart Rate
Preload
Afterload
Contractility
Beta blockers
Names
Atenolol (β1 selective),
propranolol (β1 & β2 non selective)
Preload
(venous return)
Arterial tone
Nitrates
Afterload (CCB)
Calcium antagonists
(PVR)
Other arterial vasodilators
Nitrates
In addition to treating symptoms due to myocardial ischaemia
therapy is required to reduce the risk of a myocardial infarction
(aspirin, statin, beta-blocker, ACEI)
Uses
• Angina – myocardial ischaemia
• Post myocardial infarction
• Cardiac dysrhythmias
• Chronic heart failure
• Hypertension (4th line of treatment – β1 antagonists preferred).
• Also thyrotoxicosis, glaucoma, anxiety states, migraine prophylaxis, benign
essential tremor
Mode of Action
The sympathetic nervous system acts on the heart by using noradrenaline to innervate
β1 adrenoceptors on the cardiac monocyte and cause an increase in heart rate and
contractility. This is done by producing cyclic AMP from ATP which in turn results
in an increase in Ca2+ in the cell.
Beta blockers act by competitively blocking these β1 receptors and so:
– Reduce cardiac output
– reduce renin release by the kidney
– diminish noradrenaline release by sympathetic nerves,
– lipophilic agents (e.g. propranolol) exert central sympatho-inhibitory actions.
Side Effects
Because beta-blockers also affect β2 receptors, their use may result in:
– Worsening of cardiac failure
– Bradycardia (heart block)
– Bronchoconstriction
– Hypoglycaemia (in diabetics on insulin)
– Increased risk of new onset diabetes
– Fatigue
– Cold extremities and worsening of peripheral arterial disease
– impotence
– CNS effects (lipophilic agents) e.g. nightmares
Nitrates
Names
Glyceryl trinitrate, Isosorbide mononitrate
Uses
• Angina
• Acute and chronic heart failure (nitrates - symptoms)
• BP control during anaesthesia (nitrates
Mode of Action
Act through an effect on Frank-Starling relationship to reduce preload (stroke volume
increases with venous return) and mainly cause venodilation. They cause the release
nitric oxide in smooth muscle cells and stimulate guanylate cyclase. This increases
venous capacitance and so decreases venous return.
Frank Starling relationship
Increased
afterload
S
V
Increased
venous return
0
20
10
LVEDP (mmHg)
S
V
0
20
10
LVEDP (mmHg)
It also has slight antiplatelet function, causes vasodilation of the coronary artery,
(increases O2 supply) and reduces systemic arterial resistance.
Nitrates however undergo “first pass” metabolism by the liver (its concentration is
greatly reduced before it reaches the systemic circulation). Therefore Glyceryl
trinitrate, given sublingually (under the tongue) has a half life of 5 minutes and is used
for rapid angina relief. For longer lasting effects, it is given via a transdermal patch or
Isosorbide mononitrate is used
Side Effects & Pharmacokinetics
• Hypotension, headaches and flushing as a result of vasodilation
• Glyceryl trinitrate is explosive.
• Patients can develop tolerance to nitrates– i.e. a loss of effect and benefit – this is
avoided by eccentric (asymmetric) dosing.
Pharmacokinetics:
• Extensive first pass metabolism
• Often administered as sub-lingual tablet or spray for rapid angina relief
• Longer duration of action via transdermal patches
Potassium Channel Openers:
Name - nicorandil
Mode of Action
Open KATP channels and also act as NO donors. Cause venodilation and arterial
dilation
Side effects - hypotension and headaches
Calcium Antagonists
Names
Verapamil, Diltiazem, amlodipine
Uses
Hypertension (mainly dihydropyridines)
Angina
Verapamil is used to treat paroxysmal superventricular tachyarrhythmias (SVT)
and atrial fibrillation (assuming no abnormal conduction pathways).
Mode of Action
There are 2 classes of calcium antagonists:
Phenylalkylamines- (Verapamil) and benzothiazepines (Diltiazem) reduce Ca2+
entry into cardiac and smooth muscle cells.
Dihydropyridines (amlodipine) reduces Ca2+ entry into just smooth muscle cells.
The inhibition of the Ca2+ ions into the cells results in a negative inotropic effect
(weakening of force of contraction) and also inhibits conduction through the AV
node.
» Bind to L-type calcium channels and prevent Ca2+ entry
» Ca2+ causes increased force of contraction in the heart and vessel
» Drugs giving cardiac and smooth muscle actions bind to channels in heart and
vessels, smooth muscle acting drugs only bind in the vessels and not the heart
» Vasodilation predominantly affects arterial supply
L-type calcium
channel
extracellula
r
intracellula
r
Side Effects
Verapamil
• Bradycardia and AV block
• Worsening of heart failure
• Constipation
Dihydropyridines
• Ankle Oedema
• Headache / Flushing
• Palpitations
Dysrhythmias
-
Common: affect around 700 000 people in UK.
Treatment involves reduction of sudden death, prevention of strokes and symptom
alleviation.
Involve both brady- & tachycardia and are classified according to site of origin e.g.
o Supraventricular arrhythmias (e.g. amidoarone, verapamil)
o Ventricular arrhythmias (e.g. flecainide, lidocaine).
o Complex (supraventricular + ventricular arrhythmias) (e.g. disopyramide).
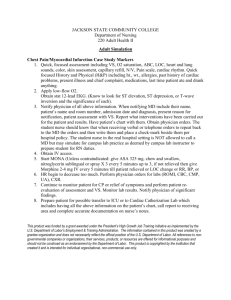
The Vaughan-Williams classification of anti-arrhythmic drugs
This is a system used to classify where drugs act, (however many drugs do not fit into
any one category). The graph shows whereabouts in the cardiac cycle the various
drugs act:
Class Mechanism of action
1
2 Class 2
I
Sodium channel blockade
II
Beta adrenergic blockade
III
Prolongation of repolarisation
('Membrane stabilisation', often
mainly due to potassium
channel blockade)
IV
Calcium channel blockade
Class 4
0
Class 1
3 Class 3 and 1a
4 Class 2
Name
Adenosine
Uses
Given intravenously to terminate superventricular tachyarrhythmias (SVT). Its actions
are short-lived (20-30s) and it is consequently safer than verapamil.
Mode of Action
It acts of A1 (adenosine) receptors on the cardiac muscle tissue causing them to
hyperpolarise and therefore slow the conduction through the AV node.
Side Effects
Chest pain, shortness of breath, dizziness and nausea
Names
Amiodarone
Uses
An effective antidysrhythmic useful for a number of superventricular and ventricular
tachyarrhythmias.
Mode of Action
Blocks multiple ion channels and possible anti-thyroid functions.
Side Effects
- Has a long half-life (10-100 days) and therefore accumulates in the body.
- photosensitive skin rashes
- hypo- or hyper-thyroidism
- pulmonary fibrosis
- corneal deposits
- neurological and gastrointestinal disturbances
Names
Digoxin and cardiac glycosides
Uses
Slowing down ventricular rate in atrial fibrillation.
Symptom relief in chronic heart failure
Mode of Action
Digoxin inhibits Na-K-ATPase (Na/K pump) resulting in increased intracellular Na+
which in turn increases intracellular Ca2+ via Na+/Ca2+ exchange. It also stimulates
the vagus nerve and therefore results in reduced conduction rate through the AV node.
Side Effects
Dysrhythmias (e.g. AV conduction block, entopic pacemaker activity)
Clinically important interactions with drugs that reduce excretion and tissue binding
e.g. amiodarone, verpamil, and drugs that reduce plasma K+ e.g. diuretics.
Name
Ivabradine
Uses
Angina
NOT TO BE USED IN:
• severe bradycardia / sick sinus syndrome / 2-3rd degree heart block
• cardiogenic shock
• recent myocardial infarction
Mode of Action
Blocks If channel (f is for “funny”) – a Na/K channel important in the sinoatrial node
resulting in a reduction in heart rate.
Cardiac Inotropes
Names
Dobutamine
Uses
Acute heart failure. (e.g. after cardiac surgery or in cardiogenic or septic shock).
Mode of Action
They are β1 receptor agonists and so increase the force of cardiac contraction but do
not have a significant effect on heart rate.
Heart Failure:
Serious condition with high mortality
Heart does not fulfil needs or does so only at raised filling pressures – causing
oedema, fluid retention and fatigue
Due to ischaemic heart disease, hypertension, cardiomyopathy or a combination
ACE inhibitors, beta blockers and spironolactone (aldosterone antagonist) shown
to improve survival
Drugs used in heart failure