Primary Cultural Issues
advertisement

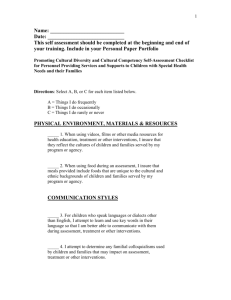
Cultural Issues in Medical Care Physicians, trained in the American medical system, may make assumptions about people’s behavior that are based on American cultural beliefs, values, and practices that are not shared by members of other ethnic groups. Familiarity with the beliefs, values and practices of specific ethnic groups, on the other hand, may lead to stereotyping. Culture is best used to understand behavior, rather than to predict it, since variation within a culture is usually greater than that between cultures. Individuals, especially those living in the United States, may hold a mosaic of cultural beliefs. It is literally impossible to predict for any specific individual which beliefs they will hold. As such, a realistic goal for physicians with regard to culture is to realize that individuals from different cultures may react in ways that are different from what is most typical of American society, that there are ways one might try to elicit preferences, and that it's important to try to pick up on clues that an individual or family may have been made uncomfortable by something which the physician might never have imagined was anything but innocuous. Generally, the more acculturated the individual, the greater the chance that they will have adopted more American ways. A quick measure of acculturation is English language skills. But, again, it is impossible to predict which aspects of American culture any specific individual will have adopted, and which aspects of traditional culture will be retained. It is also important to remember that cultures are not static, but always in the process of changing. Remember: every culture has certain values, beliefs, and practices, which may be held to a greater or lesser degree by the individual members of that culture. Major dimensions along which cultures vary include: Desire for information Response to authority Decision-making Emotional expressiveness Time orientation World view/beliefs Patient /provider relationship Gender Roles Communication style Racism Listed below are some of the variations that are found. I have listed cultures which exhibit one aspect of the spectrum or another, but this does not mean that individual members of that cultural group will necessarily share that cultural pattern. Desire for information: Some may want a lot of information; others may want very little. Some families may want information withheld from the patient. In Jewish culture, for example, knowledge is often highly valued. Knowledge = control. (Perhaps due to a history of being asked to leave one country or another without much in the way of material possessions. Thus, knowledge, which can never be taken away, became highly valued. As a result, some patients may want as much information as possible up front. E.g., they may want to know all the side effects of different treatments prior to receiving the results of a biopsy which may determine whether or not any treatment is needed. In rural Vietnamese culture, for example, verbalizing something (negative) may be believed to increase the chances that it will occur. Thus, someone who held this belief may not desire very much information about the negative consequences of their condition. It also makes signing informed consent problematical if consent covers negative possibilities. In many cultures which value the family over the individual (e.g., many Asian & Hispanic cultures), it is seen as inappropriate to reveal a fatal prognosis to a patient. Instead, the information should be given to a family member, who will decide whether or not to inform the patient. It can be thought to create a sense of hopelessness & hasten the dying process. Others see it as insensitive. Those who are devoutly religious may believe that only God knows when someone will die. A culturally competent way to deal with this issue: Ask the patient how much information they would like to be given. Ask if they want information about their condition to be given to them or to some other family member whom they designate. Response to authority: Different cultures hold varying amounts of respect for authority In traditional Asian cultures, which are hierarchical, respect for physicians is high. In order to show respect, a patient may agree to whatever the physician says, but may not follow through. The emphasis is on showing respect to the individual’s face. A culturally competent way to deal with this: to increase the chances that a patient will follow through, ask them what problems they might encounter in adhering to your recommendation. Ask them if there is anything you can do to make it easier for them to adhere. Ask if they’ve ever known anyone who did what you ask who later had problems as a result. In other words, try to find out what concerns they may have to adhering. In many cultures where there is respect for authority (.e.g, many Asian and Hispanic cultures) individuals may indicate comprehension & agreement when it is not present. This can also be true in order to avoid the shame of not understanding something. A culturally competent way to deal with this: be sure to ask open-ended questions to ascertain whether or not the patient truly understands what you have said. Don’t rely on a yes or no response. In cultures where there is an emphasis on individual autonomy (e.g., Anglo American & African American cultures since the baby boom generation) individuals may openly challenge the physician. A culturally competent way to deal with this: make the patient a partner in the decision-making process. Ask what problems they might encounter in complying. Ask them if there is anything you can do to make it easier for them to comply. In cultures where social status is highly valued (e.g., many Middle Eastern cultures), individuals who share this value may insist on speaking with the “top man.” Males may also be preferred since males have higher status that females. A culturally competent way to deal with this: this is a tricky one. One way to deal with it is to emphasize your knowledge and status with regard to the particular issue. Another way is to make a referral. Decision-making: In cultures where an egalitarian social structure is seen as the ideal, even if it is not the reality (e.g., Anglo American culture), individuals may want to be a partner in making decisions about their own life & health. Since this is in alignment with the values of the medical profession, it should not pose a problem, except among more authoritarian physicians. In some Arab cultures, it is believed that since the physician has the expert knowledge, he should take responsibility for making the decision. In hierarchical cultures (such as many Asian cultures) where the physician has a great deal of authority and often acts in a paternalistic manner, some patients may expect to be told what to do. In cultures where relative sexual equality exists, at least as an ideal (e.g., Anglo American culture since the feminist movement) women may feel comfortable making decisions by themselves. In cultures where men are dominant (e.g., many Hispanic, Asian, & Middle Eastern cultures), traditionally oriented women may defer decision-making to their husbands, whether it be for themselves or their children. (In many Middle Eastern cultures, which have a patrilineal kinship organization, chidlren “belong” to the father, not the mother, and thus it is appropriate to defer to the father.) In cultures where the family is the primary unit (e.g., many Hispanic and Asian cultures), individuals may prefer to have decisions made by the family, rather than the individual. In Romany (“Gypsy”) culture, where the clan is the primary unit, and decisions may be deferred to clan elders. A culturally competent way to deal with this: when decisions need to be made, ask the patient how they would be most comfortable arriving at a decision. Do they want to consult with family members. Sometimes the physician must be willing to take a more active role if the patient wants that. One study (Browner, et. al. 2003) indicated that Mexican patients interpreted the shared decision-making approach of the physician in determining whether or not to get prenatal testing as an indication that it wasn’t important. “If it were important, he would have insisted upon the test.” Expression of emotions: Different cultures allow or encourage a greater or lesser expression of emotion; individuals vary along these lines as well. For example, most Asian cultures – especially Japanese—see emotions, particularly negative ones, as something private and not to be shared with strangers. Native American, Northern European, and American WASP cultures tend to encourage greater stoicism and emotional control. Many Hispanic, Middle Eastern & Southern European cultures allow more emotional expressiveness in their members. A culturally competent way to deal with this: make no assumptions about an individual’s level of pain or distress based upon their verbal expression. Do not make the mistake of ignoring, for example, a Middle Eastern woman crying out in pain by stereotyping her as “just another Arab woman exaggerating her pain.” Her expressiveness may indicate a serious problem. Nor should you make the mistake of assuming a Japanese patient is not in pain, simply because he is quiet. Time Orientation: planning ahead Many individuals who are either poor or come from 3rd world countries tend to be present oriented. Poverty often forces one to live in the present; planning for the future is a luxury of wealth. This may impact their health care behavior; if they feel fine now, they may resist preventive care. They may not want to know what the future holds (in terms of genetic testing) because the future is not as real to them. A culturally competent way to deal with this: When it comes to preventive behavior, this may require more patient teaching. In terms of genetic testing, see below. Middle and upper class individuals from 1st world countries tend to be future oriented and may be concerned with the future. They may be more likely to want to know whether or not they have a genetic disease which could manifest sometime in the future, so that they can plan their life around knowing. A culturally competent way to deal with this: First, make no assumptions as to whether or not someone would want to know their genetic risk of getting a disease. Second, ask whether or not they want to know. Third, do not impose your own biases on them. Some people may want to know only if they can change the outcome, and if it cannot be changed, they don’t want to know. Others may want to know because the knowledge will lead them to make different life choices. World View: controlling nature Some cultures, particularly those that are industrialized, manifest a belief that humans can control nature. This is reflected, for example, in the American assumption that given enough time and money, any disease can be cured. An individual holding such a belief may be more likely to be proactive in their health care. In contrast, in cultures with a particularly harsh environment, or where there is much poverty, people are more likely to take the attitude that humans are powerless against the forces of nature and the supernatural, except as their prayers & beliefs can cause higher forces (e.g., god(s)) to act on their behalf. This is reflected in such sayings as, Que será, será (Hispanic – what will be, will be). Bahala na (Filipino – what will be, will be). Inshallah (Arabic – God willing). Although individuals who hold such a belief may have less faith in scientific medicine to provide a cure than someone who believes that we can control nature, they may also have more hope if they are religious, for in most religious traditions, God can cure anything. Such a belief may also develop as a result of life experiences and can be found among individuals of any culture. A culturally competent way to deal with this: it may be especially important to address the patient’s spiritual needs. Encourage prayer when appropriate. Consider involving religious practioners in the decisionmaking process. Another perspective is one held in cultures where people have traditionally lived close to the land. This is the view that humans are a part of nature. It is not unusual to find such a belief in Native American cultures and Chinese culture. Disease may be interpreted as a lack of balance between natural forces (yin/yang in Traditional Chinese Medicine; hot/cold in many Latin American systems). Individuals who hold such a view may prefer natural, herbal-based remedies. Patient/Provider relationship: the expected nature of the relationship between provider and patient may vary according to culture. One dimension along which this may vary is related to degree of personal familiarity – e.g., many Middle Easterners may expect a personal connection with their physician. Providers often have a close, warm relationship with family, & get involved in their personal life. That kind of relationship is often seen as unprofessional in the US, and thus American health care providers may be perceived as cold and uncaring to someone who expects personal involvement. American physicians are trained to ask many questions of their patients. It is a way to gain information and to develop rapport. In some cultures, for example some Native American and Asian cultures, the “competent” physician will know through observation and intuition what is wrong with the patient. Only the “incompetent physician” will ask a lot of questions. In some countries, such as the Philippines, it is seen as inappropriate for nurses, for example, to ask any personal questions of the patient. They are not trained nor are they expected to deal with psychosocial issues. That is the job of the family, and it would be seen as intrusive on the part of a nurse. Nurses from such a background may sometimes be perceived by American patients as “good at providing technical care, but cold & unfriendly.” From the perspective of the nurse, her behavior is “professional.” A culturally competent way to deal with this: If you are having trouble developing rapport with your patient, it may be because you are perceived as either uncaring or as too intrusive. If you are comfortable doing so, you may want to adapt your style to show more or less familiarity. There is not too much that can be done with regard to asking “too many questions” other than have an assistant ask them. Gender Differences: There are numerous issues raised by gender differences in various cultures. Gender of the physician: In some cultures there is strict sexual segregation (e.g., Muslim and Orthodox Jewish cultures). A culturally competent way to deal with this: female patients should be treated by female physicians and male patients by male physicians whenever possible. Rules against opposite sex touching and eye contact may impede good health care delivery. If it is not possible, respect requests that male physicians where gloves when treating a female patient, and that the woman be kept covered. Gender preferences: In some cultures there is a strong preference for one sex over the other, due to the role of one gender in carrying on the family name or providing for elderly parents. In most cases, if one sex is preferred, it is usually the son. In countries such as China, which has a one-child-per-family policy, this has led to an increase in abortion and infanticide of daughters. If a child is born with ambiguous genitalia, parents may be biased toward raising the child as a son. A culturally competent way to deal with this: Ask the patient if they have a preference for a son or daughter. In the case of a child with ambiguous genitalia, a great deal of explanation may be required if you think it is best to raise a child as a daughter. Communication Styles: While many individuals may prefer direct communication, some may prefer an indirect approach. For example, among traditional Navahos, there are many taboos, which can make direct communication problematical. A culturally competent way to deal with this: If you have a Navaho patient who appears traditional in dress, talk in the 3rd person. For example, rather than say, “X will happen if you don’t do Y,” say you knew someone who didn’t do Y, and X happened. It’s safest to present information by telling a story. Fear of Racism It is not uncommon for individuals who belong to oppressed minorities to show a lack of faith in the American medical system, which is largely perceived as a white institution. A long history of racism and daily experience of discrimination have left many African Americans, for example, with a highly sensitive “radar” for racism. Many suggestions on the part of white physicians may be seen as racially motivated, even when they are not. A culturally competent way to deal with this: Be especially sensitive to how your patient may perceive any suggestions that could be interpreted as racially motivated. E.g., suggesting a woman with ten children limit her fertility may be seen as rational and objective by the white physician suggesting it, but be interpreted as a plan of racial genocide by the African American patient. Preface any such suggestions with your reasons for suggesting it.