2nd edition
advertisement

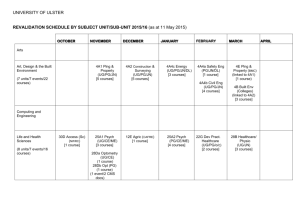
Students With A Cause The Medical Society at the U of T is full of talented student leaders that continually enrich student life and add to the surrounding community. This year, when I began my term as President, there were two goals that I wanted to accomplish. First, I wanted to see the Medical Society fulfill its potential as a body of student government, and to gain exposure within the university and the Toronto community. Secondly, I wanted to help cultivate an environment in which student leaders received the support and encouragement that is necessary for achievement and mutual learning. We began the year in a new, centrally located office that allowed for greater visibility and increased contact with the student body. In addition, we re-created the Toronto Meds webpage so that students could readily access information about student life & student government. Early in the year, MedSoc got to work to stretch our budget as far as was possible to support student initiatives. Student clubs allow students to showcase our various talents, explore academic and non-academic areas of interest, hold events for students and community members, and help those that are less fortunate within our community. This year, in conjunction with the Student Affairs office and the MAA, MedSoc re-invented what used to By Tasleem Murji, OT7 be the Functions Committee and helped create the new MedLife committee. Medlife brings you everything from career nights, to cooking nights. While working hard to support student initiatives, we quickly realized that creating a safe and comfortable place to hold students events should also be a priority. With this in mind, MedSoc, is pleased to announce that in the New Year, we shall see a new security system installed in the Alumni Lounge. We hope that with this new security in place, we will be able to invest in improving the resources in the lounge for student use. Together, with your input, we will begin making some real changes to our lounge space! Things have been just as busy on the academic side. We have been working to implement the changes that students and the accreditation committees have suggested. Also, in October we took our MedSoc publications to the AAMC in Boston and strengthened our market share south of the border. We are looking forward to bringing you MedSoc’s latest publication, the Pharmacology Hand Book, in the spring of 2005. We have strengthened our relationship with external bodies like the CFMS, AAMC, CMA, PAIRO, and OMA. In October, we had our first ever OMAPhysician panel discussion in 1 January 2005 response to student concern about the OMA-MOHLTC agreement proposal. The positive feedback for this event was overwhelming and served to demonstrate that our medical students are deeply concerned about the future of their profession as it pertains to them and to patient care. MedSoc has also been very involved in the debate on rising student tuition. In November, we were invited to sit at a round table discussion and a town hall meeting with the Honorable Bob Rae. In January, we have also arranged to have Mr. Rae meet with Toronto medical students to discuss issues related to post secondary education. We still have many goals to accomplish this year, and we hope to continue serving the student body and representing your interests in the New Year. I cannot over-emphasize just how lucky we are to have so many talented students at this school. I have learned so much from working with each of you these last few months and I thank you all for your support, great ideas, and good advice. It is an absolute pleasure working in an environment of students who are motivated, creative, and driven by a strong sense of both individual and group convictions. I believe our student body is held together by a combination of diversity and solidarity that lends us our great strength. News/Editorials The State of Canada's National Drug Plan: A Federal-Provincial Stalemate By Sarah Munroe With an annual cost of nearly $15 billion a year, paying for prescription drugs is the fastest growing health care expense in Canada. i Premiers and territorial leaders met at the Health Care Summit this past July to propose a solution to alleviate this immense financial burden. In what seemed to be an unusual show of unity, the leaders agreed to a plan in which the federal government would fund a national pharmacare program. Although details were not provided, the federal government would be asked to take over the purchasing of drugs and to fund standardized coverage for all Canadians. This would allow the provinces to redirect funds to other areas, such as reducing wait times for diagnostic procedures and surgeries. While the provincial leaders were unanimous in their support of what they saw as a means to fulfill Prime Minister Paul Martin's campaign promise to create a national drug program, the federal government did not show the same enthusiasm. According to Health Minister Ujjal Dosanjh, the federal government is more focused on decreasing wait times than on comprehensive drug coverage.i Both Martin and Dosanjh have commented that the federal government is only committed to creating a ‘catastrophic drug coverage plan’.ii A ‘catastrophic drug plan’ would only cover drug costs for people with extremely high annual drug expenses. The plan proposed by provincial leaders has been estimated to cost $12 billion annually, while at least one proposal for ‘catastrophic coverage’ was estimated at a much lower $1 billion.ii There are many potential benefits to having a nationwide plan controlled, at least in part, by the federal government. By purchasing drugs in bulk, costs can be reduced by as much as 21 to 51 per cent.iii In Australia this strategy has saved $2 billion.iv The federal government purchasing drugs does seem appropriate since patent laws, trade agreements, and drug regulations also affect cost and are controlled by this level of government. iv While prescription drugs are undoubtedly necessary for many Canadians, they cannot stand alone in medical treatment. Some critics of the proposed plan urge that to be effective, it must be integrated with the rest of healthcare. The Canada Health Act, which ensures free medical care for all Canadians, only covers medications when they are administered in hospitals.iv Outpatient medications, what a pharmacare plan would cover, would need to be added to the Act to ensure an appropriate balance between outpatient medication and inpatient services. iii 2 After discussions at the September Health Care Summit, the premiers withdrew the proposed plan in exchange for increased provincial health care funding. It was agreed that a task force would be set up to develop a ‘national drug strategy’ by 2006.v Although this seemed to end discussions, a meeting of provincial and federal health ministers in October raised the issue again. Health Minister Dosanjh remained firm that a national plan would not be created; however, a 14-member task force was established to report on the issue in January.vi In the end, a lack of integration could leave patients in the middle of a federal-provincial battle that may compromise patient care. i CBC News Online. "Wait times priority, not drugs, says health minister." August 17, 2004. ii Anis, Aslam H. "National pharmacare: a dog's tale." Canadian Medical Association Journal. 171(6). September 14, 2004. iii CBC News Online. "Martin agreed to pharmacare working group." September 14, 2004. iv Government of Canada. "Canada Health Act Overview" November 25, 2002. www.hcsc.gc.ca/english/media/releases/2002/hea lth_act/overview.htm v CBC News. "Anatomy of an agreement." September 16, 2004. vi Matas, Robert. "Dosanjh rejects drug plan proposal." The Globe and Mail. Monday, October 18, 2004. News/Editorials Superbugs: How the Biggest Threat to Your Patients Could Be You By Mark Sinyor, OT7 “Until that moment, when I stood there looking at the sign on his door, it had not occurred to me that I might have given him the infection. But the truth is I may have. One of us certainly did.”i For those of us in preclerkship, it may be difficult to appreciate the gravity of the struggle taking place in hospitals around the world to stem the epidemic of antibiotic resistant bugs. With Sir Alexander Fleming’s discovery of penicillin in 1928, and the wave of drugs that followed, doctors were in a position, at least for several decades, to win the war on bacteria. But at the outset of the new millennium, superbugs such as methicillin-resistant Staphylococcus aureus (MRSA) and vancomycin-resistant enterococci (VRE) are launching an assault on patients. And an unlikely ally, the health care worker, is helping them do it. The issue of antibiotic resistant bacteria is particularly meaningful for me because my late grandfather, Jean Bercovici, who himself was a physician for forty years, was infected with MRSA in 2001 while being treated at a hospital in the GTA. But before I get to that, I will provide a brief background. Staphylococcus aureus and enterococci are part of the normal bacterial flora in humans, being found most commonly in the nose and gut, respectively. As a result of widespread use of methicillin and vancomycin, a small number of bacterial clones have acquired genes conferring resistance against these antibiotics. As these strains of bacteria, MRSA and VRE, do not respond to the standard therapy, they have flourished in the hospital environment, spreading through wards at an extraordinary rate. How widespread are these infections? In 1992, there were fewer than 500 cases of MRSA and no cases of VRE reported in Ontario. Between 1999 and 2002, roughly 33,000 patients were identified as either colonized or infected with MRSA. Nearly 2,000 patients tested positive for VRE (Department of Microbiology, Mount Sinai Hospital). The annual cost of antibiotic resistance to the Canadian health care system is believed to be as much as $200 million. ii Sadly, the vast majority of new cases of MRSA and VRE can be attributed to health care workers who have not properly gowned, or worse, have not bothered to wash their hands between patients. In truth, I find it difficult to be passionate about statistics. My attitude has been coloured far more by my experience with my grandfather, just one of those 33,000 patients to test positive for MRSA. Like most people who contract MRSA, he was merely colonized. The bacteria did not infect him nor did it directly impair his health, it simply appeared in a routine swab of his 3 tracheostomy tube. Someone had not washed his or her hands. As a result, my grandfather spent many of what were to be the last months of his life lying alone in a room isolated from the world. The perpetual solitude had a terribly negative influence on him, and all of this in the hopes that his quarantine would protect other patients from suffering his fate. In retrospect, it makes it all the more heartbreaking that my family would frequently see members of the health care team going in and out of his room without a gown or without washing their hands properly, each time putting another patient at risk. The life of a medical student is demanding and fast paced, but proper hygiene can be the most important thing you ever do for your patients. Even before trying to heal, a doctor’s first responsibility is to do no harm. Take the extra fifteen seconds to wash your hands. I know I will. Mark Sinyor gives special thanks to Dr. Mary Vearncombe, medical director of infection prevention and control at Sunnybrook and Women's College Health Sciences Centre, for her advice and input. i Atul Gawande, General and Endocrine Surgeon, Brigham and Women's Hospital. New England Journal of Medicine 349; 25:2383-2386, Dec 18, 2003. ii Globe and Mail [Toronto]. 2001 May 30; Sect A:19). From a Patient’s Point of View The Whispering Disease By Fatima Uddin “I’m a very healthy woman,” begins Francesca, her vibrant eyes sparkling with life. “At the time I was 54. I had never been to a hospital except to deliver two sons. I was working hard, living well, and really looking after myself.” Then, in late May of 2000, Francesca began to feel fatigued and bloated. A vague discomfort radiated below her navel. Alarmed by these symptoms, she went to her family physician. Without conducting a full history, he decided that she had Irritable Bowel Syndrome (IBS). On a second visit, the family physician revealed that there was blood in her urine. Despite Francesca’s concerns, he insisted that she was suffering from IBS and referred her to a gastroenterologist. “He was very glad to be rid of me.” Francesca shakes her head in disappointment. “When I went back for a third visit, he greeted me with a terse ‘What are you doing here?’ He seemed disappointed that I had come back to bother him.” By this time, Francesca was suffering from diarrhea, constipation, and pelvic pain. “I really was not feeling well and I broke down weeping in my GP’s office. He didn’t even say to me ‘What is bothering you?’ He didn’t pursue it at all!” On a fourth and final visit, Francesca’s physician performed a pelvic exam. “I was screaming! The pain was excruciating,” she recalls with tears in her eyes. “He said not a word. He didn’t explain what he was doing, or why. I’ll never forget it as long as I live!” After the exam, without any discussion, he ordered an ultrasound and arranged for her to meet with a gynecologist. Francesca also started to see the gastroenterologist. “She was very kind. She wanted me to be healthy, but she wasn’t really connecting the dots.” The gastroenterologist obtained her ultrasound results, which unfortunately revealed an abnormal right ovary. “What does this mean?” Francesca asked. All she received in response was “I don’t know.” The physician persisted in her belief that Francesca had IBS and arranged for her to have a barium follow-through. Francesca finally met with the gynecologist in August. For the first time, a physician conducted a full, in-depth interview. He also performed a pelvic exam, but the experience was completely different. “He explained everything to me. He paid a lot of attention to me. Most of all, he didn’t jump to the easiest conclusion, which was IBS.” The following day, Francesca went to have her barium follow-through. As she walked into the hospital, she saw her gynecologist. “I waved, and he waved back” Francesca remembers. “I was petrified to ingest anything at this point, but they made me swallow a thing of shaving cream 4 consistency. The technician said it would cause me to be constipated, but I was already constipated. My gynecologist waved to me, and he knew that I was having the procedure done. He suspected ovarian cancer but he let me go through the barium follow-through anyway. They put me through this sadistic torture anyway. It was bad enough what I was going through, but there were horrific acts imposed on me without concern, without empathy, without listening, without explaining to me what my risks were, or where they were going with my treatment”. The next time she visited her gynecologist, he had the results of a second ultrasound. “I have some very bad news,” he said. “I’m very sorry. You have ovarian cancer. I didn’t want to tell you until I had all the pieces together.” “My physicians knew that I had abdominal discomfort and pelvic pain,” she tells me, pointing to a list of symptoms on an ovarian cancer fact card. “They knew I felt bloated and fatigued. They knew of my frequent urination, loss of appetite, and change in bowel habits. The tests they ordered revealed an abnormal right ovary and blood in my urine. I had every classic symptom of ovarian cancer, yet they failed to recognize it. I was exactly at the mean age at which a woman gets ovarian cancer. The mean age is 54, and I was exactly that!” “They call it the whispering disease,” Francesca laughs “but I was shouting all the way.” From a Patient’s Point of View Last year was supposed to be the best year of my life. I had just graduated from U of T and I was getting married. I was looking forward to starting a new chapter in my life. What I didn’t know was that the year would be full of challenges. It all started during my final exams in April 2003. I woke up one day with double vision. I visited Health Services and the doctor referred me to see a neurologist instead of an ophthalmologist, which I found to be a bit strange. A few days later, my double vision disappeared as mysteriously as it had appeared. I didn’t want to defer writing my exams, so I skipped the neurologist appointment. I passed my exams and graduated with honours. My next attack was on my wedding day in the summer. I had numbness and tingling in my foot. I walked down the aisle with almost a limp and I had to lean on my father. A friend of mine who was also a medical student asked what had happened. After I explained, she told me to see the neurologist. My foot problem was gone during my honeymoon and so I pushed it to the back of my mind. I was so happy starting a new life with my husband. As the summer ended however, new problems began. One day in September, I woke up feeling dizzy and I couldn’t walk straight. I could no longer ignore my health problems so I phoned my friend. I showed her that I couldn’t walk and told I have Multiple Sclerosis By Anonymous her that I didn’t follow up with my leg problem since my wedding. She began to ask me questions about tingling, numbness, painful sensations, slurred speech, blurred or double vision, bladder problems, and fatigue. When I told her about my double vision, she was even more worried. My friend knew what was wrong with me, but she had such a hard time telling me. She kept saying that she was only a second year medical student and didn’t know enough to diagnose me, but she insisted that I see the neurologist. I finally pinned her down and insisted that she tell me. She then looked at me with tear-brimmed eyes and told me that I probably had MS. That moment will always be in my memory. I didn’t know much about MS, but I knew it was a horrible, chronic disease that crippled people. After the initial shock, my friend tried to explain the disease to me. She showed me some websites. She also warned me about telling my husband in case he might leave me. I was really mad at her for suggesting such a thing, but then I began to worry. We had been married for less than two months and he was only 24. He could easily find someone else who wasn’t defective like me. I spent the afternoon agonizing over how to tell my husband. When he came home, I told him quite bluntly that I had MS. He was shocked at first, but 6 then he was very supportive. We cried together all night. My husband and I went to see a GP the next day. The doctor also thought I had MS, but said that I had to undergo some diagnostic tests. He referred me to a neurologist the next week. After all the tests had been performed, the neurologist confirmed that I had MS. I was prepared for the diagnosis and up for the challenge. The neurologist said that there was no cure for MS, but there were ways to control it. There was a drug that had to be given daily by needle. I didn’t mind it too much, but it was expensive. My husband’s work did not offer a drug plan. I was no longer covered by my parents’ drug plan, nor was I covered by my old student drug plan. My parents were quite supportive with paying for my medications, but I couldn’t depend on them forever. After a long discussion with my husband, I decided to go back to graduate school. Some U of T graduate programs offered reasonable stipends and my drugs would be covered by the SAC drug plan. I contacted my old thesis project supervisor and he agreed to take me on as a Masters student. My MS is now well controlled and I haven’t had an attack since. The past year has brought many challenges, but it has made me stronger. It has strengthened my marriage and made me appreciate my health – something which I had never done before. INTERVIEW WITH A FACULTY MEMBER Dr. Monica Branigan: Ethics in Action By Jessica Ahn As an undergraduate student, I knew little about Dr. Branigan prior to interviewing her. But I was told that she seemed like an interesting person, so I set up a meeting. Little did I know that I was about to encounter someone who would provide me with a whole new perspective on what medicine is all about. I met Dr. Branigan in her office in the Medical Sciences Building, and she told me about her work within the Faculty of Medicine. As the Ethics theme coordinator for the M.D. program at U of T, she is responsible for finding ways to create an environment where students can become the best doctors they can be: doctors who will use both their minds and their hearts in their future practices. Dr. Branigan attended medical school at the University of Ottawa, and trained in British Columbia. She practiced in a family medicine clinic for over 20 years, and is currently working in community-based palliative care. You may wonder, why palliative care? When Dr. Branigan was an intern, her father passed away very suddenly, and she was left to deal with his physician. The doctor was emotionally detached. He failed to provide Dr. Branigan and her family with any emotional comfort, merely offering details of the procedures he had performed. Her father passed away fearful, without any family members to comfort him, in a moment that should have been personal and loving. In our culture, Dr. Branigan notes, we place so much emphasis on perfection and excellency that we often overlook the fact that doctors are human. It is important to recognize that doctors should be people who can show compassion, people who can help patients and their families during the most painful and overwhelming times of their lives. Dr. Branigan and her family were deeply affected by this experience. When she worked in a clinic as a family physician, she often felt too restricted in the amount of time she could spend with her patients. She wanted to form real human relationships with her patients, and 15 minutes with a patient just didn’t allow for that to happen. Ultimately, these are the qualities that patients want in their physicians, and Dr. Branigan has tried to incorporate many of these ideas into The Healer’s Art, an ethics-related elective for medical students. Having gathered a great deal of experience from her 20 years in family medicine, she felt prepared to dive into palliative care. I, for one, am truly glad that patients and the community have someone like Dr. Branigan to look to in times of great need. 7 Dr. Branigan leads a very balanced life. She tries to make time for yoga, and just recently went on a trip to participate in a yoga instructor course. She is married to a physician, and they have two children. She had been skeptical at first about marrying another physician, but at the end of the day, Dr. Branigan now finds it wonderful to go home to someone who understands her work and her motivations. She is an avid reader who remembers devouring the works of the Brontë sisters in high school, staying up late into the night on the weekend to read and coming out of her room on Sunday just exhausted. Even nowadays, she tries to fit a lot of reading into her busy schedule. She says it’s great to always have something uplifting and inspirational to read. My interview with Dr. Branigan made me appreciate her important role in shaping medical students’ education, and in emphasizing the aspects of medicine that go beyond prescriptions and diagnoses. Her efforts to form real relationships with her patients make her not only an outstanding physician, but an inspiring role model. Once in a while, you meet a person who makes you stop, take a look around, and really think about yourself and your community. For me, Dr. Branigan is one of those people. INTERVIEW WITH A FACULTY MEMBER Dr. Ian Taylor: Beyond the Myth Integral to every new medical student’s orientation week is the inevitable warning about Dr. Ian Taylor. Before the first anatomy lecture is even held, every first-year knows not to come late to Dr. Taylor’s classes without a very good excuse. Dr. Taylor, director of the pre-clerkship phase of the M.D. program and of the Structure & Function unit that spans the first five months of medical school, doesn’t seem to mind his notoriety. “It’s probably a good thing that I’m not starting from zero every year,” he comments. “Last year, I actually had a complaint from a former student, now a physician in the city, who said I was slacking up, getting soft in my old age. I’m mindful as well of the reputation that I have to maintain. “I do think it’s important to be respectful, students of their profs and profs of their students. It’s very difficult to concentrate when people are walking in and out,” he continues. “I also see it as important down the road. You’re going to expect patients to arrive on time to appointments, and equally, patients will have a reasonable expectation that you should arrive on time.” In his 31st year in the Faculty of Medicine, Dr. Ian Taylor is a familiar face to several generations of medical students. “I’ve seen the curriculum change, I’ve seen the students change. Many By Layla Dabby, OT8 professors have come and gone, and I’m still here. I’ve greatly enjoyed U of T; it’s been very good to me.” Dr. Taylor was born and raised in Manchester, England, and received his M.D. from the University of Manchester. His devotion to the Manchester United football club well precedes the era (or even the birth) of David Beckham: it was originally a matter of avoiding the wrath of schoolyard bullies fiercely loyal to Man U. “I left in 1972. I went to Edmonton initially for two years before coming to U of T. “I originally trained as a neurosurgeon in England. I met my wife there, who was a head nurse. Given the relative status of senior sisters and lowly doctors, she was kind enough to agree to marry me. Senior sisters are very senior. If they said ‘jump,’ then junior doctors said ‘How high? Yes, ma’am!’ So it was very good of her to marry me. We’ve been married thirty years.” As the director of Structure & Function, Dr. Taylor is responsible for a tenweek block of gross anatomy. “I hated anatomy when I was a student,” he admits. “I disliked it intensely, and finding myself teaching it was a very big surprise. When I did have the opportunity to teach anatomy, I decided that I was going to try to make it as interesting as I possibly could. “We all spent thousands of hours learning minutiae, as 7 well as the big stuff, and never had a sense of what was important and why. When I originally took over the anatomy course in 1985, and subsequently brought in the new curriculum, I was determined to do it very differently from the way it was done even in Toronto. “Almost everyone in the class wants to be a clinician, so the first thing is to take an enormous amount of facts and prune it down to the facts that are actually useful. A week or two into the class, you can actually begin to make tentative diagnoses, although there are often other possibilities that you don’t even know about yet; you can see how investigations can demonstrate anatomy, both normal and disordered. Anatomy is a discipline which opens up broader vistas. You can practice anatomy on your significant other, your mum, your offspring, somebody else’s offspring.” Dr. Taylor doesn’t foresee any major future changes to Structure & Function. “In anatomy, of course, there are no new muscles. But there are different ways of looking at those muscles.” Of the M.D. program in general, he thinks that “there needs to be a pushing of the pendulum back to primary care, particularly in the pre-clerkship. Most doctors are currently practicing in family medicine.” Is retirement anywhere on the horizon? “Mike Wiley says that I’m good until I’m eighty. I don’t think my wife will tolerate my teaching for that long...” ARTS & Literature Arrival By Trevor Balena I am sick. Perhaps dying. My streets are littered with the dead. Friends. Family. Strangers. My houses are dark, decaying into ruins, with only the dim light of failing fires inside hinting at those who yet survive. My churches, though far quieter than before, ring with the voices of those who see the face of the apocalypse in their dreams, and in each other. And, on the horizon, the specter of war looms ever larger; why deal but one cruel blow, the Fates must think, when more will suffice? Once, I was the jewel of my country; home of the Royal Residence; outlet for the dreams of Edward the Confessor and Harold, his successor. Once, I was the finest city in all of Britain. But now I am sick, perhaps dying. I am London. And the Black Death has arrived to claim me. by Daniel Saul, OT7 - charcoal and pencil 10 Shouts and Murmurs by Goldie Kurtz, OT8 Want to impress your next date? Is Grant’s the only museum you have visited this year? Then take advantage of Toronto’s cultural scene! Here are some current and upcoming events to whet your artistic appetite…and maybe wow a prospective amour! Oh Picasso! The U of T Art Centre in University College is hosting a collection of Pablo Picasso’s ceramic sculptures, in conjunction with the Gardiner Museum of Ceramic Art. Over 80 pieces are featured, many from the Picasso family’s private collection. Several works have been borrowed from the Louvre in Paris and the Museu de Ceramica in Barcelona. This exhibit is on campus (U.C.). Until January 23rd: Tues-Sun. 10-6 pm; Fri 10-9 pm. $12 for students. Royal Ontario Museum: Come See the (Fascinating) Mess – Architecture and construction to create the “Renaissance ROM” - take a free tour of the development starting January 12th. "Pearls: A Natural History" - Brilliant deep-sea gems from all over the world. Pearls owned by Marilyn Monroe, Marie Antoinette, and Audrey Hepburn are on display. Until Jan 9th. Tickets: $12 for students. Do you have a passion for fashion? Want to learn more about Asian art? "Touched by Indigo" is coming to the ROM in January. Witness the beauty of embroidery and weaving, and discover how traditional creations have given rise to modern style. Until April 10th. Tickets: $12 for students. Art Gallery of Ontario: "Modigliani: Beyond the Myth" - Amadeo Modigliani, born in Italy in 1884, helped usher in the modern art era. He broke the conventions of portraiture and created his own unique style for depicting others. Until January 23rd. Tickets: $15 for students. The A.G.O. continues the theme of the Modigliani show with complimentary exhibits of portraiture including: "Stargazing: Portraits of 19th and 20th Century Celebrities, Eye of the Beholder" (both until Jan. 9), and "Reading Faces" (until Jan 31.) If you prefer sculpture, don’t miss their permanent Henry Moore collection – the largest collection of his work in the world! Music and Theatre "Da Kink in My Hair": Celebrate the stories of six West Indian women who meet in a hair salon and share the tales of their lives. Princess of Wales Theatre, 300 King St. W. Jan 11- Feb 27. Yanni (yes, Yanni - unplugged! back with a vengeance, spinning his signature post-bohemian-alt-soft-classicalrock.) At the ACC. Date: February 2nd. Tickets: starting at $55.50. 11 Interdisciplinary Page BMC…More than just Textbook Illustrators By Kari Francis, BMC Hi, my name is Kari Francis, and I am one of 9 BMC graduate students. I was a part of the OT8 first year medical course, Structure and Function. Throughout the course, I had the chance to meet and talk with a bunch of wonderful med students, and from this interaction one thing became clear—no one had any idea what BMC stood for, why we had class with them, or how our program is incorporated into the medical profession. So, let me take this opportunity to clear up what BMC stands for, what we do, how we are integrated into the medical field, and why our expertise is so critically needed. Keep reading and I hope you come to fancy the wonderful world of Biomedical Communications (BMC) as much as I do! BMC is the only accredited program for medical illustration in Canada, and one of only five in North America! BMC is a professional graduate program that prepares an interdisciplinary group of 8-10 artists each year to become critical thinkers, problem-solvers and professional communicators. The program combines design and communication theory with scientific knowledge to produce visual material for health promotion, medical education, and the process of scientific discovery. The one comment I get a lot when trying to explain the BMC program is “oh, you’re the people who draw the pretty pictures in medical textbooks”. To which I respond, “We sure do, but that’s not all, have you seen CSI?” If you have, think of the realistic animations of a bullet ripping through skin and lodging into the vertebral column, or when the heart is pumping inside its pericardium and red blood cells are whizzing through an artery. Medical animation is being used in new ways each year, and our graduate program is one of the leaders in this field. Although CSI is a good example of the type of entertainment animation that a BMC graduate can do, the majority of the work done is to educate. The goal of a BMC graduate is to stimulate the audience visually and to make difficult concepts easier to understand for everyone. For example, a set of parents who have a child with cystic fibrosis. They try to read all available information on CF, but are severely limited by endless, mindboggling medical terminology. As a result, they become frustrated and mad that they are unable to fully understand the condition that is afflicting their child. However, a BMC student working with CF specialists are able to replace the obstacles, such as difficult terminology and complicated ideas, with a flowing, and conceptually accurate animation or interactive website. BMC graduates are professionals at bridging the gap between what 12 doctors know and what people want and need to learn. As you can imagine, the necessity of this type of work is boundless as it is critical for medical education and communication. In addition to the 3D animation (visualization design), BMC also offers specialization in new media design. Graduates from this stream create and evaluate interactive, computerbased multimedia for teaching and learning. The outstanding work done by BMC graduates is all that is needed to prove that this program is one of the leaders in the field of medical illustrations. To see examples of students’ work and to learn more about the program, including its incredible professors such as Dr. Linda Wilson-Pauwels and Margot Mackay, please go to http://brodel.med.utoronto.ca/bmc /. I hope you enjoyed this quick walk through the BMC program, and I hope you now all have a better understanding of what BMC graduates do. For more information feel free to contact me at kari.francis@utoronto.ca. I would love to hear from anyone interested in the program, or in the work of BMC graduates! The next edition of The Pulse will include drawings from students in our department… Sorry, I could not include pictures in this edition because I ran out of space! So stay tuned!! Clubs/Organizations Women In Medicine By: Karen Hershenfield, Women in Medicine Co-chair 2004-2005 Left to right: Sara Cohen-Gelfand, Mickey Zeller and Karen Hershenfield (WIM co-chairs), Dr. Anna Day and Dr. Edward Shorter at the “History of Medicine” wine and cheese held earlier this year. The Women in Medicine (WIM) group is an organization for medical students at U of T that provides an opportunity to meet female role models in medicine in an informal setting. By participating in WIM events, students are also given a chance to foster leadership skills and to learn about the opportunities available within medicine. Lastly, this group educates the student body about challenges faced by female physicians in the past. WIM was founded by members of the OT5 class and is currently in its third year of existence, co-chaired by Sara Cohen-Gelfand, Mickey Zeller and Karen Hershenfield. Our events this year started out with a IT’S A BOY !!! “meet and greet” in October for medical students and female faculty and staff. It was great to see such a large turnout of interested students! Our second event, held on November 10th, was a “History of Women in Medicine” wine and cheese featuring talks by Dr. Edward Shorter, history of medicine professor at U of T and Dr. Anna Day, a respirologist at Sunnybrook and Women’s College. It was both a very informative and enjoyable evening!! In expanding WIM this year, we have made connections with Canada’s national group, the Federation of Medical Women of Canada (FMWC). We attended a great FMWC leadership conference for students in the summer and have been amazed at the support available for female physicians, residents, and students at the national level. WIM is looking forward to its big event of the year: the spring gala!! Last year’s event was absolutely superb and we hope to set up an even more enjoyable event this year, with dynamic speakers and interesting physicians to speak with our students. We must thank the MAA and MedSoc for helping to make all of our events possible. See you all at the spring gala! If you have questions, please email womeninmeds@yahoo.ca. MAZEL TOV – Jewish for congratulations. Ari (0T7) and Stephanie Greenwald are thrilled to announce the birth of their son, Gabriel, who was born 8lb 2oz at 4:37 am on November 2, 2004 at the wonderful Women’s College Hospital. Gabriel’s arrival has brought tremendous joy to his entire family (including aunt Ilana, 0T6), and especially to his big sister, Adira. Ari and Stephanie wish to thank the entire student body and faculty for all of their tremendous support and best wishes. Special thanks goes to Dr. Chapman who has been especially helpful throughout this busy and exciting time. 11 Clubs/Organizations New Student Group Addresses Adolescent Body Image Issues By David Wasserstein, OT7 This year (2004/5) is the inaugural year of a new medical student community health group – Healthy Body Image. The goal of our group is to promote health in adolescents through education and discussion on issues of body image. We hope to create an open, comfortable environment to allow high school students to discuss how body image can affect a person’s health. Many medical problems in young people, including eating disorders and body dysmorphic disorders, are tied into this image. On a deeper level, factors such as low self esteem, the media and societal and peer pressures may influence an impressionable young person. Adolescents need to be aware that activities that have become commonplace, such as compulsive exercising, occasional starving to lose weight and taking over-thecounter supplements (e.g., stool softeners or performance enhancers), have a health risk of their own and may lead to the development of more serious conditions. Our group has chosen to use established (in peer-reviewed journals – for you DOCH II addicts) educational materials developed by Sheena’s Place and the Hospital for Sick Children. This approach attempts to address underlying risks for developing body image disorders, including low self esteem and peer pressure, as opposed to direct education. If you decide to help out with our group – and we hope you do – our plan is to visit 3 local high schools during the second semester. We will be recruiting and training volunteers in January. Depending on the number of volunteers and/or your interest, volunteering should require a commitment of training plus one session only. If interested, please contact David Wasserstein or Alex Palombo at david.wasserstein@utoronto.ca or a.palombo@utoronto.ca. We feel it is important for young people to discuss these topics in an open environment. They need to be made aware of pressures, reflect on their own values, know where they can obtain guidance and information, and learn about the risks of activities of which they may be unaware. With some hard work and your participation – the Healthy Body Image group hopes to deliver this messa The Pulse 2004/05 Editorial Staff Co-Editors In Chief Amelia Ciofani, OT7 & Amanda Hu, OT6 News/Editorials Dharini Mahendira, OT6 & Alessandra Palombo, OT7 From a Patient's Point of View Louie Chan, OT7 & Brian Kim, OT7 Interview With a Faculty Member Layla Dabby, OT8 & Shazeen Suleman Clubs/Organizations /Announcements Michelle Levy, OT7 & Laura Saunders, OT7 Arts & Lit Joanna Mansfield OT6 & Daniel Saul, OT7 Interdisciplinary Page Kari Francis, BMC Faculty Advisors Dr. Anne Agur, Dr. William Chapman & Dr. Kelly O’Brien Contact us at amelia.ciofani@utoronto.ca Check out our website at http://individual.utoronto.ca/amandahu/ The Pulse is sponsored by the Medical Alumni Association and the Medical Society. Happy New Year from The Pulse! 12 13