Diagnostic Utility of Synovial Fluid Analysis and Musculoskeletal
advertisement

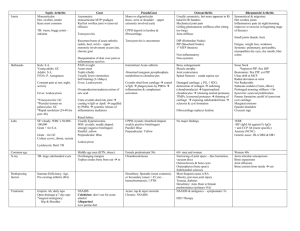
EL-MINIA MED. BULL. VOL. 20, NO. 2, JUNE, 2009 Ali et al DIAGNOSTIC UTILITY OF SYNOVIAL FLUID ANALYSIS AND MUSCULOSKELETAL ULTRASONOGRAPHY IN CRYSTALS INDUCED ARTHRITIS By Rasha Ali*, Abdou Ellaban*, Ashraf El-Shereef**, Shreen Refaat**** and Hanaa Ahmed**** Departments of *Rheumatology and Rehablitation; **Diagnostic Radiology (A) Minia Faculty of Medicine. ABSTRACT: The types of crystals associated with joint disease include monosodium urate (MSU), calcium pyrophosphate dihydrate crystals (CPPD) and basic calcium phosphate crystals (BCP), including hydroxyapatite (HA). Aim; the aim of the current study was to detect the rule of synovial fluid analysis (using polarized light microscopy) and musculoskeletal ultrasonography for the diagnosis of crystals induced arthritis. Patients and methods: sixty patients with knee effusion available for aspiration. There were 34 male (56.7%), and 26 female (43.3%), the age of the patients ranged from 25 to 70 years with a mean of 49±9.3 years. All patients had; imaging technique (plain radiography and musculoskeletal ultrasonography), and synovial fluid analysis. Patients were classified according to presence of CPPD crystals into 2 groups group I (+ve CPPD, 38 patients) and group II (-ve CPPD, 22 patients). Results; calcification characteristic of CPPD were found in knee joint in 32 (84.2%) patients, wrist joint in 18 (47.4%) patients, Achilles tendon in 22 (57.9%) patients, and plantar fascia in 6 (15.8%) patients in group I, calcification characteristic of MSU (double contour sign) was found in 4 (18.2%) patients in group II, and calcification characteristic of HA was found in 2 (5.3%) patients in group I and 2 (9%) in group II. Conclusion: the most reliable method of diagnosis of crystal deposition in articular and extra-articular tissue is invasive needle aspiration for synovial fluid analysis and identification of crystals on polarizing microscopy. Ultrasonography is a useful indirect sign for the presence of CPPD crystal deposition disease. KEY WORDS: Synovial Fluid Musculoskeletal Arthritis crystals (CPPD and BCP) are common components of osteoar-thritic synovial fluids 3-5. INTRODUCTION: Crystal deposition pathology is one of the most frequent situations that rheumatologist is confronted with in their practice. The types of crystals associated with joint disease include monosodium urate (MSU), calcium pyrophosphate dihydrate crystals (CPPD) and basic calcium phosphate crystals (BCP), including hydroxyapatite (HA). The attacks of acute arthritis are the characteristic clinical manifestations1,2. Calcium-containing The most reliable method of diagnosis of crystal deposition pathology is invasive needle aspiration for synovial fluid analysis and identification of crystals on polarizing microscopy6-8. McCarty and colleagues9, were the first to discover non-urate crystals, 308 EL-MINIA MED. BULL. VOL. 20, NO. 2, JUNE, 2009 identified by X-ray diffraction as CPPD, in knee synovial fluid from patients with acute synovitis and cartilage calcification visualized on standard radiographs. Studies identified CPPD as the most common cause of radiographic articular calcification at the knee (Chondrocalcinosis’ (CC))10. Ali et al with a mean of 49±9.3 years, and the disease duration ranged from 0.1-12 years with a mean of 3.4±3.5 years. Patients with known auto-immune disease or patients younger than 20 years or older than 70 years were excluded from the study. All patients had; full history, clinical examination, laboratory investigations, imaging technique, and synovial fluid analysis. Detection of typical calcifications on plain radiographs; usually of the knees, the wrists and the pelvis, allows the diagnosis of CC. However, radiographs are relatively insensitive and detect only sizeable CPPD deposits11. High frequency US has proved to be an excellent technique for accurate evaluation of articular and juxta-articular alterations in crystal related diseases2,8,12. Ultrasonography (US) is an emerging technique that could be used for detection of the CPPD deposits (hyperechoic deposits), particularly those that are too small to be visible on plain radiographs13. US demonstrate a high specificity and good sensitivity for detection of the CPPD crystals induced calcification, using microscopic analysis as the positive standard8,13. Also studies confirms the usefulness of US in revealing signs of CPPD deposits in peri-articular structures (Achilles tendon) that show no calcification on plain radiographs14. Musculoskeletal ultrasonography: Conventional grey-scale ultrasound (US) and power Doppler (PDS) examinations were carried out using 7-12.5 linear transducers. Musculoskeletal ultrasonography and power Doppler US were done for: Joints (Shoulder, elbow, wrist, MCP, knee, MTP joints), tendons (rotator cuff tendons, triceps tendon, achilles tendon, quadriceps tendon and plantar fascia), bursa (subacromial bursa, olecranon, prepatellar , pes-anserine, retrocalcaenal bursa and Backer's cyst), heels (cortical bone of posterior and inferior aspects of the heel), and sites of enthesis, and the patellar surface. Ultrasonographic Examination was carried out bilaterally and symmetrically, with both longitudinal and transverse scans. Examinations of joints for (effusion, calcification, erosion, and tophi) AIM OF THE WORK: The aim of the current study was to detect the rule of synovial fluid analysis (using polarized light microscopy) and musculoskeletal ultrasonography for the diagnosis of crystals induced arthritis. Examination of the heels (cortical bone of posterior and inferior aspects of the heel) for (Enthesophytosis (hyperechoic bony spur interrupting the cortical profile), determining the characteristic shadowing and erosions of the posterior and inferior aspects of the heel). PATIENTS AND METHODS: This study included 60 patients with knee effusion available for aspiration. There were 34 male (56.7%), and 26 female (43.3%), the age of the patients ranged from 25 to 70 years Examination of the Achilles tendon for (Calcifications, entheso- 309 EL-MINIA MED. BULL. VOL. 20, NO. 2, JUNE, 2009 pathy (thickening of the insertional tract of the tendon), pretendtious edema, and Power Doppler sonography (PDS) was performed for the presence of intratendinous color activity was attributed to vascularization). Ali et al Using SPSS for windows version 17.015, two-tailed tests were used throughout and statistical signifycance was set at the conventional 0.05 level. The following statistics were carried out: Descriptive statistics (the range, means and standard deviation were calculated for interval and ordinary variables and frequencies and percentages for categorical variables16, group comparisons (Student's t-test and the chi-squared (²) test)17, correlations (Bivariate Correlations procedure computes Pearson’s correlation coefficient with its significance levels)16, and Sensitivity and specificity. Examination other tendons for calcification. Plantar fascia examination for (calcifications, plantar fasciitis (thickening of the insertional tract of the fascia, measured where it crosses the antero-inferior border of the calcaneus), perifascial edema, Power Doppler sonography (PDS) for the presence of color activity of the plantar fascia was attributed to vasculari-zation). Examination of bursa for (bursal involvement, Power Doppler sonography (PDS) for the presence of intrabursal color activity was attributed to vascularization). Backer's cyst (comma shaped fluid accumulation between the medial head of gastrocnemius and semimembranosus tendon). RESULTS: Microscopic examination (using polarized light microscopy) for identification of crystals in the studied patients showed that; 44(73.3%) patients were positive for crystals and 16(26.7%) patients were negative for crystals, they were distributed as follows; calcium pyrophosphate deposition disease (CPPD) crystals in 38 (63.3%) patients, Monosodium urate (MSU) crystals in 7(11.7%) patients and hydroxyappatite (HA) crystals in 26(43.3%) patients. There was overlap between types of crystals. Enthesis (Around the patella (in the superior part, at the quadriceps tendon insertion and in the inferior part, at the patellar tendon insertion) and around the calcaneus (at Achilles tendon and plantar fascia insertion)). Patella (for the irregularity of the anterior surface of the patella). Synovial Fluid Analysis: 1- Gross (macroscopic) examination (viscosity, colour, clarity). 2- Microscopic examination (using polarised light microscopy) (wet film preparation, for cell count and birefringent crystals determination, stained film examination (for nonbirefringent crystals examination using Alezarin red stain and cytological examination for differential leucocytic count using Wright's Stain). According to the results of synovial fluid analysis for identification of CPPD crystals we divided the patients into two groups; Group I: Patients positive for CPPD crystals, including 38(63.3%) patients and Group II: Patients negative for CPPD crystals, including 22(36.7%) patients. Table (1) shows the demographic data of patients in the two groups. Table (2) represents the comparison between synovial fluid analysis in Statistical analysis: 310 EL-MINIA MED. BULL. VOL. 20, NO. 2, JUNE, 2009 patients with +ve CPPD and patients with –ve CPPD. Plain radiography identify calcification in knee joint (chondrocalcinosis) 5(13.2%) patients and 33(86.8%) patients show no calcification, while in group II; no calcify-cation was found, with no statistically significant differrence between the 2 groups. No radiological findings of calcification were found at other sites (wrist, spines, and pelvis, AT or PF). Ali et al For MSU crystals there were 7 patients (11.7%) had MSU crystals, 3 patients of them had MSU crystals in association with CPPD crystals and 4 of them had MSU crystals alone; those 4 patients with MSU crystals alone showed the knee calcification characteristic of MSU (double contour sign), first metatarsophalyngeal joint calcification characteristic of MSU (double contour sign) and erosion, and metacarpophalyngeal joints calcifications characteristic of MSU (double contour sign) and erosion. Ultrasonographic findings of calcification (knee, shoulder, wrist, 1st MTP joints, MCP joints, Achilles tendon (AT), and plantar fascia (PF)) was present in 32 patients (84.2%) in group I and in 6 patients (27.3%) in group II, this difference was statisticcally significant (p=0.0001) (Figure 1). For hydroxyappatite (HA) crystals; there were 26 patients (43.3%) had hydroxyappatite (HA) crystals, 24 patients of them had hydroxyappatite (HA) crystals in association with CPPD crystals and 2 of them had hydroxyappatite (HA) crystals alone. Those 2 patients who had hydroxyappatite (HA) crystals alone and 2 of the patients who had hydroxyappatite (HA) crystals in association with CPPD crystals had shoulder calcification characteristic of HA deposition (hypoechoic deposits). Difference between plain radiography and ultrasonography in the identification of calcification (Figure 2). Table (3) show the comparison between ultrasonographic findings of joint in patients with +ve CPPD and patients with –ve CPPD. The sensitivity of ultrasonography for detection of calcification was 86.4% in all patients while the sensitivity of plain radiography was 11.4%, the specificity of both ultrasonography and plain radiography for detection of calcification was 100% in all patients with positive predictive value 1 for both ultrasonography and plain radiography, negative predictive value was 0.73 for ultrasonography and 0.29 for plain radiography. Table (4) represents the comparison between ultrasonographic findings of Achilles tendon in patients with +ve CPPD and patients with –ve CPPD. Table (5) represents the comparison between ultrasonographic findings of plantar fascia in patients with +ve CPPD and patients with –ve CPPD. Table (6) shows the ultrasonographic examination for frequency of calcification characteristic of CPPD in patients with +ve CPPD crystals. The sensitivity of ultrasonography for detection of calcification (knee, wrist) in patients with +ve CPPD crystals was 84.2% while that of plain radiography was 13.2%, the specificity of both 311 EL-MINIA MED. BULL. VOL. 20, NO. 2, JUNE, 2009 ultrasonography and plain radiography for detection of calcification was 100%. The sensitivity of ultrasonography for detection of calcification in Ali et al Achilles tendon was 57.9% and the specificity was 100%. For plantar fascia the sensitivity of ultrasonography for detection of calcification was 15.8% and the specificity was 100%. Tables and Figures: Table (1): Demographic and clinical data of patients with +ve CPPD and those with –ve CPPD crystals. Sex Age (years) Male Group I +ve CPPD (n = 38) 23 (60.5%) Group II -ve CPPD (n=22) 11 (50%) Female 15 (39.5%) 11 (50%) Range 27-65 25-70 51.1±8.7 45.4±12.2 0.2-10 0.1-12 3.9±3.2 2.5±4 10-45 15-45 Mean±SD 23.3±10.4 23.9±12.2 NO. (%) 35 (92.1%) 9 (40.9%) 5-15 5-10 Mean±SD 8.1±3.1 7±2.6 NO. (%) 31 (81.6%) 9 (40.9%) 2-9 5-9 7.2±1.5 7.1±1.2 Mean±SD Disease duration (years) Range Mean±SD Morning stiffness duration (min) Inactivity stiffness duration (min) Range Range Numerical rating scale Range Mean±SD By (x2) test and student's t-test *Significant P-value <0.05. **Significant P-value <0.01. ***Significant P-value <0.001. 312 p-value x²/t 0.629 0.5 2.135 0.03* 1.378 0.1 -0.150 18.675 0.8 0.0001*** 0.986 8.403 0.3 0.008** 0.299 0.7 EL-MINIA MED. BULL. VOL. 20, NO. 2, JUNE, 2009 Ali et al Table (2): Comparison between synovial fluid analysis in patients with +ve CPPD and patients with –ve CPPD crystals. Viscosity Aspect Birifringient MSU Hydroxyapatite (HA) Leucocytic count Group I +ve CPPD (n = 38) Group II -ve CPPD (n=22) Normal 10 (26.3%) 16 (72.7%) Decreased 28 (73.7%) 6 (27.3%) Clear 37 (97.4%) 0 (0%) 1 (2.6%) 0 (0%) Birifrigient 38 (100%) 4 (18.2%) Non Birifrigient Positive 24 (0%) 2 (9.1%) 3 (7.9%) 4 (18.2%) Negative 35 (92.1%) 18 (81.8%) Positive 24 (63.2%) 2 (9.1%) Negative 14 (36.8%) 20 (90.1%) Range 4000-30000 300-30000 Mean±SD 16197±5372 4918±8341 90%-94% 28%-93% 91.9%±1.3% 49.3%±26 Turbid Range PMN cells Mean±SD By student's t- test and (x2) test **Significant P-value <0.01. ***Significant P-value <0.001. MSU: Monosodium urate HA: Hydroxyappatite PMN: Polymorphonuclear neutrophil 313 p-value x²/t 12.222 0.001** 0.598 1.000 44.416 0.0001*** 1.431 0.4 16.587 0.0001*** 6.376 0.0001*** 10.127 0.0001*** EL-MINIA MED. BULL. VOL. 20, NO. 2, JUNE, 2009 Ali et al Table (3): Comparison between ultrasonographic findings of joints in patients with +ve CPPD and patients with –ve CPPD crystals. Calcification (For MSU Double contour sign) Calcification (For CPPD hyperechoic deposits ) Backer cyst Calcification (For MSU 1st MTP joint Double contour sign) Erosion Effusion Shoulder joint Calcification (For CPPD hyperechoic deposits ) Calcification (For HA hypoechoic deposits) Calcification (For CPPD Wrist joint hyperechoic deposits ) Calcification (For MSU MCP Double contour sign) Erosion Effusion By (x2) test *Significant P-value <0.05. ***Significant P-value <0.001. Group I +ve CPPD (n = 38) 0 (0%) Group II -ve CPPD (n=22) 4 (18.2%) x² Pvalue 7.403 0.02* 32 (84.2%) 0 (0%) 39.699 0.0001*** 24 (63.2%) 0 (0%) 3 (13.6%) 4 (18.2%) 13.806 0.0001*** 7.403 0.02* 0 (0%) 2 (5.3%) 0 (0%) 4 (18.2%) 4 (18.2%) 0 (0%) 7.403 2.584 - 0.02* 0.2 - 2 (5.3%) 2 (9%) 0.328 0.6 18(47.4%) 0 (0%) 14.887 0.0001*** 0 (0%) 2 (9%) 3.574 0.1 0 (0%) 1 (2.6%) 2 (9%) 2 (9%) 3.574 1.224 0.1 0.5 Knee joint MCP: Metacrpophalyngeal joints HA: Hydroxyappatite 1 st MTP: First metatarsophalyngeal joint 314 EL-MINIA MED. BULL. VOL. 20, NO. 2, JUNE, 2009 Ali et al Table (4): Comparison between ultrasonographic findings of Achilles tendon in patients with +ve CPPD and patients with –ve CPPD crystals. Group I +ve CPPD (n = 38) 22 (57.9%) Calcification Pattern of Pattern I 16 (42.1%) calcification Pattern II 4 (10.5%) 2 (5.3%) Pattern III 4 (10.5%) Cortical bone surface irregularity Group II -ve CPPD (n=22) 0 (0%) 0 (0%) 20.111 0.0001*** 6 (15.8%) 0 (0%) 4 (10.5%) 2 (5.3%) 2.481 0.4 0 (0%) 16 (42.1%) 16 (42.1%) 0 (0%) 0 (0%) 4 (10.5%) 22 (57.9%) Enthesophytosis 9 (23.7%) Entheseopathy 8 (21%) Vascular sign 5 (13.2%) Bursitis By (x2) test *Significant P-value <0.05. ***Significant P-value <0.01. 9 (40.9%) 0 (0%) 0 (0%) 0 (0%) 1.610 6.130 5.344 3.158 22 (57.9%) 3 (7.9%) 2 (5.3%) 2 (5.3%) x² Unilaeral Bilateral p-value (for group I) (for group I) 0.3 0.02* 0.02* 0.1 0 (0%) 6 (15.8%) 6 (15.8%) 3 (7.9%) Patterns of calcification in Achilles tendon: Pattern I: Multiple thin linear bands Pattern II: Single fine linear bands. Pattern III: Thick solid bands. Table (5): Comparison between ultrasonographic findings of plantar fascia in patients with +ve CPPD and patients with –ve CPPD crystals. Group I +ve CPPD (n = 38) 6 (15.8%) Calcification Pattern of Pattern I 6 (15.8%) calcification Pattern II 0 (0%) Pattern III 0 (0%) Cortical bone surface 30 (78.9%) irregularity Group II -veCPPD (n=22) 0 (0%) 7 (31.8%) 23 (60.5%) 10 (45.5%) Enthesophytosis 16 (42.1%) 4 (18.2%) Plantar fasciitis By (x2) test **Significant P-value <0.01. Patterns of calcification in plantar fascia: Pattern I: Multiple thin linear bands Pattern II: Single fine linear bands. Pattern III: Thick solid bands. 315 pUnilaeral x² value (for group I) 3.860 0.08 0 (0%) 0 (0%) 0 (0%) 0 (0%) 13.092 0.001** 0 (0%) Bilateral (for group I) 6 (15.8%) 6 (15.8%) 0 (0%) 0 (0%) 30 (78.9%) 1.279 3.589 23 (60.5%) 16 (42.1%) 0.3 0.09 0 (0%) 0 (0%) EL-MINIA MED. BULL. VOL. 20, NO. 2, JUNE, 2009 Ali et al Table (6): Ultrasonographic examination for frequency of calcification characteristic of CPPD in patients with +ve CPPD crystals. Number Frequency % Unilateral Bilateral Knee calcification 32 84.2% 8 (21.1%) 24 (63.2%) Pattern of calcification Pattern I 0 0% - - Pattern II Pattern III Pattern I&II Pattern I&II&III Site of Articular surface calcification Fibrous cartilage Tendons Joint recesses Wrist calcification 21 2 8 1 9 30 0 3 18 55.3% 5.3% 21.1% 2.6% 23.7% 78.9% 0% 7.9% 47.4% 0 (0%) 18 (47.4%) Pattern of calcification Pattern I Pattern II Pattern III Articular surface Fibrous cartilage Tendons 0 18 0 0 18 0 0 0% 47.4% 0% 0% 47.4% 0% 0% - - 22 6 0 57.9% 15.8% 0% 6 (15.8%) 0 (0%) - 16 (42.1) 6 (15.8%) - Site of calcification Joint recesses Achilles tendon calcification Plantar fascia calcification Shoulder calcification Patterns of calcification in the knee joint: Pattern I: Hyperechoic band. Pattern II: Several thin hyperechoic spots (Punctate pattern). Pattern III: Homogenous hyperechoic nodular or oval deposits. 316 EL-MINIA MED. BULL. VOL. 20, NO. 2, JUNE, 2009 Ali et al Figure (1): Frequency of ultrasonographic findings of calcification in patients with +ve CPPD and patients with –ve CPPD crystals. Frequency of US findings of calcification in patients in group I and group II 35 30 25 32 (84.2%) 20 15 10 6 (27.3%) 5 0 Group I Group II Figure (2): Plain radiography and ultrasonography findings of calcification in patients with +ve CPPD crystals. Plain radiograhy and US findings of calcification in patients in group I 35 30 25 20 32 (84.2%) 33 (86.8%) 15 10 5 6 (15.8%) 5 (13.2%) 0 Plain rad Calcification Plain rad No calcification US Calcification 317 US No calcification EL-MINIA MED. BULL. VOL. 20, NO. 2, JUNE, 2009 Ali et al that calcification (chondrocalcinosis) was found in 5 (8%) patients. In agreement with our results; Richette et al.,23, reported a crude prevelance of radiographic calcification (CC) in 7% of patients with no difference between men and women. Also Neame et al.,24, reported a crude prevelance of radiographic calcification (CC) is 7%. However, in the study of Malavia et al.,25, the prevelance of chondrocalcinosis was lower; it was 2% of the adult Kuwaiti and other MiddleEastern Arab patients. In the current study, there were statistically significant difference between patients in group I and group II concerning patients' age (p=0.03) being older in patients in group I. Although there were patients with old age in group II that may be the cause of the presence of other types of crystals in such patients (MSU and HA). In agreement with our results; Doherty,26, who proved that age is a risk factor for both crystal arthropathies, MSU preferentially deposits in OA joints Roddy et al., 27, and OA predisposes to CPPD Neame et al.,24 deposition. DISCUSSION: In our study, synovial fluid analysis for the identification of crystals showed that; 38(63.3%) patients CPPD crystals, 7(11.7%) patients had MSU crystals, and 26 (43.3%) patients had hydroxyappatite (HA) crystals, in with the note that there were patients with more than one type of crystals. Patients who had CPPD and/ or hydroxyappatite crystals or both represent 70% of patients. In agreement with our results, Derfus et al.,18, they found that 60% of osteoarthritic patients had CPPD, hydroxyappatite crystals or both in their synovial fluid. The frequency of association of CPPD crystals deposits may result from the biological effects of CPPD as they interact with fibroblasts or mononuclear cells. In a study by Viriyavejkul et al.,19, the presence of CPPD crystals was identified in 52.9% of patients with osteoarthritis. Also in the study of Nalbant et al.,20, they found the prevalence of hydroxylappatite crystals in synovial fluid from patients with knee OA is between 30% and 60%. The same finding was proved by O'shea and McCarthy,21, who found that the incidence of hydroxyappatite crystals in the synovial fluid from patients with osteoarthritis is at least 30% to 60%. Jaccard et al.,22, found that; calcium pyrophosphate dehydrate was in 55.7% and monosodium urate in 42% of patients. They reported that both types of crystals (calcium pyrophosphate dihydrate and monosodium urate crystals) may coexist and they were found in (2%) of patients, usually in specimens obtained from the knee. Among the patients with a mixed crystal composition, these patients had a higher age. In the current study, the ultrasonographic examination of patients with +ve CPPD versus patients with – ve CPPD for the detection of calcification characteristic of CPPD (hyperechoic deposits; bands, spots or nodules) showed that; calcification was found 32(84.2%) patients; knee calcification was present in 32(84.2%) patients, wrist calcification was present in 18(47.4%) patients in group I and no patient in group II, these difference was statistically significant (P= 0.0001 for both of them). No patient in either group had shoulder calcification characteristic of CPPD deposition. In agreement with our results; Foldes,28, in his study for detection of calcification in the knee joint he found that ultrasonically, detectable calcification In the current study, plain radiography findings of calcification in knee joint (chondrocalcinosis) showed 318 EL-MINIA MED. BULL. VOL. 20, NO. 2, JUNE, 2009 in the knee was present in 17 of 21 patients (81%). However, in the study of Frediani et al.,6, they found that ultrasonically defined CPPD calcifycations were found in all the 11 patients with CPPD crystals (100%). Knee calcification was present in 10 of 11 patients (90.9%), shoulder calcifycation was present in 4 of 11 patients (36%) of patients, and wrist calcifycation was present in 5 of 11 patients (45.5%). The differences from our study that; the calcification in our study was 84.4% while in Frediani et al.,6 it was 100% this may be due to that, the mean age of patients is higher in Frediani et al., 6 than in our current study, racial and genetic factors. Ali et al patients, it was present in all patients who had calcification in this study, it was found in 30(78.9%) patients in the knee (fibrous cartilag, and in 18 (47.4%) patients in the wrist (fibrous cartilage). In agreement with our results Frediani et al.,6 found that; pattern II was the most common pattern of calcification found in the study (found in at least one site in all patients). It was present in all patients who had wrist calcification (5 of 11 (45.5%)) and in the knee in either alone (6 of 11 patients (54.5%)) or in association with pattern I (4 of 11 patients (36.4%)). Also Filippou et al.,13, pattern II (at the minsci) was the most common pattern found and it was present in all the patients who had calcification (14 patients of 14) and pattern I at the articular cartilage in 4 of 14 patients. In the current study, shoulder calcification that was found in 2 patients in group I and also 2 patients in group II who were –ve for CPPD crystals calcifications was characterized by hypoechoic appearance that was characteristic of hydroxyappatite depositon (CPPD calcification characterized by hyperechoic deposits), and synovial fluid of these 4 patients showed hat the 2 patients in group I had hydroxyappatite (HA) crystals in association with CPPD crystals and in the 2 patients in group 2 had also hydroxyappatite (HA) crystals alone. In agreement with our result; Frediani et al.,6, found that calcifications that presented a hypoechoic appearance with posterior shadowing were considered as crystalline deposits of another nature than CPPD, probably due to hydroxyapatite (HA) crystal deposition disease deposits. These calcifications were found in four control group patients and none of patients in the group of patients with positive CPPD crystals. In the current study it was found that, all patients who had calcification had CPPD crystals in their synovial fluis and no patient without CPPD crystals in the synovial fluid analysis had either radiographic chondrocalcinosis or ultrasonographic finding of calcification characteristic of CPPD. In agreement with our results Frediani et al.,6, who found that in all patients with ultrasonographically defined CPPD deposits, CPPD crystals were found in the synovial fluid, however, standard radiographic examination did not show evidence of the calcific deposits that were identified by ultrasonography in all cases, and CPPD crystals were not found in the synovial fluid of controls without ultrasonographically defined CPPD deposits or radiographic chondrocalcinosis. However in the study of Filippou et al.,13, they found the presence of CPPD calcifications without the presence of CPPD crystals in synovial fluid. In the current study, patten II of calcification was the most common pattern of calcification found among 319 EL-MINIA MED. BULL. VOL. 20, NO. 2, JUNE, 2009 In the current study, the sensitivity of ultrasonography for detection of calcification was 84.2% patients in group I (+ve CPPD = 38) while that of plain radiography it was 13.2%, and the specificity of both ultrasonography and plain radiography for detection of calcification was 100%. In agreement with our results, Foldes,28, found that the sensitivity and specificity of ultrasonography for the diagnosis of chondrocalcinosis were 80% and 100% respectively. Also Filippou et al.,13, who proved that, ultrasonography demonstrated good sensitivity (equal to 86.7%) and a high specificity (equal to 96.4%) in the diagnosis of chondrocalcinosis. Ali et al calcification in only 25% of Achilles tendons of patients with CC. Also Gerster et al.,30, described fine linear calcifications in 13% of the Achilles tendons in patients with articular CC, concluding that this radiographic pattern was a useful indirect sign of CPPD crystal deposition disease. Gerster et al.,30, described 3 cases of Achilles tendinitis associated with linear calcification of CPPD as a rare presentation of extraarticular CC. In the current study; the sensitivity of ultrasonography for detection of calcification in Achilles tendon was 57.9% and the specificity was 100%. In agreement with our results, Falsetti et al.,14, who found that ultrasonography was found to be 57.9% sensitive, and 100% specific for detection of Achilles tendon calcifications which was a useful indirect sign for the presence of CPPD crystal deposition disease. In the current study, Achilles tendon calcification was present in 22 (57.9%) patients in group I and no patient in group II (p= 0.0001), calcification of the Achilles tendon was charactarized by hyperechoic deposits within the fibrillar tendon structure not in continuity with the bone profile. The pattern of calcifycation was pattern I (multiple thin linear bands) in 16 (84.2%) patients who were bilateral in all of them, pattern II (single fine linear bands) in 4 (10.5%) patients who were unilatreal in all of them, and pattern III (thick solid bands) in 2 (5.3%) patients who were unilateal in all of them. In agreement with our results, Falsetti et al.,14, who found that US examination showed Achilles tendon calcifications in 57.9% (33/57 patients) of CC and no patient in the control group (OA without CPPD) had calcification (p= 0.0001) it was bilateral in 25 of 57 cases (43.8%). The sonographic patterns of these calcifications were multiple thin linear bands in 72.4% of cases, single fine linear bands in 17.2%, and thick solid bands in 10.3%. However, in disagreement with our results, Pereira et al.,29, they described thin linear bands of In the current study, plantar fascia calcification was present in 6 (15.7%) patients in group I (who were bilateral in all of them) and no patient in group II, with no statistically significant difference between the 2 groups, and the pattern of calcification was pattern I (multiple thin linear bands) in all of them. Calcifications of the plantar fascia insertional tract were charactarized by hyperechoic deposits in the superficial region of the insertional tract of the fascia, not in continuity with the bone profile. In agreement with our results, Falsetti et al.,14, who found that; plantar fascia calcifications was present in 15.8% (9/57 patients) of CC (it was bilateral in all cases); but they found plantar fascia calcifications in 2% (1/50 patients) of OA (control group) (p not significant). Falsetti et al.,14, found that calcifications of the plantar fascia appeared in all cases as a single fine linear echoic band located 320 EL-MINIA MED. BULL. VOL. 20, NO. 2, JUNE, 2009 Ali et al in the superficial region of the insertional tract of the fascia, apparently not in continuity with the cortical bone. In disagreement with our results, Gerster et al.,30, they described fine linear calcifications in 0.5% of the plantar fascia in patients with articular CC, concluding that this radiographic pattern was a useful indirect sign of CPPD crystal deposition disease. finding of calcification characteristic of CPPD. In the current study; the sensitivity of ultrasonography for detection of calcification in plantar fascia was 15.8% and the specificity was 100%. In agreement with our results, Falsetti et al.,14, found that ultrasonography was found to be 15.8% sensitive, and 100% specific for detection of plantar fascia calcifications which was a useful indirect sign for the presence of CPPD crystal deposition disease. Ultrasonography is a useful indirect sign for the presence of CPPD crystal deposition disease, it has high specificity in all the examined sites, good sensitivity for joint calcification; however the low sensitivity in Achilles tendon and plantar fascia calcifycations, suggests a moderate accuracy for using the ultrasonographic finding of Achilles tendon and plantar fascia calcifications alone as a method for diagnosing CPPD crystal deposition disease without searching for other sites of calcification characteristic of CPPD. So we can conclude that; the most reliable method of diagnosis of crystal deposition in articular and extraarticular tissue is invasive needle aspiration for synovial fluid analysis and identification of crystals on polarizing microscopy. Conclusion and Recommendation From the result of the current study it was found that ultrasonography (US) has proved to be an excellent technique for accurate detection of calcification in articular and juxta-articular in crystal induced arthritis. Ultrasonography was found to be more sensetive for identification of calcification in articular and extra-articular tissues than plain radiography. It is recommended to do ultrasonographic examination for any patient presented with joint effusion in cases suspected to have crystals induced pathology prior to proceeding to needle aspiration for synovial fluid analysis and identification of crystals on polarizing microscopy, and to keep needle aspiration for cases with high suspicion of crystals induced arthritis and in whom no characteristic findings of calcification was found in ultrasonographic examination or in patients in need for therapeutic injection . In the current study it was found that, all patients who had either radiographic chondrocalcinosis or ultrasonographic finding of calcification characteristic of CPPD had CPPD crystals in their synovial fluid and no patient without CPPD crystals in the synovial fluid analysis had either radiographic chondrocalcinosis or ultrasonographic finding of calcification characteristic of CPPD, however there are patients with CPPD crystals in their synovial fluid but they had not either radiographic chondrocalcinosis or ultrasonographic REFERENCES: 1. OLivieri F and Punzi L. (2003). L'inflammazione articolare da microcristalli. Reumatisoma; 55 (1): 16-27. 2. Fodor D, Albu A, Gherman C. (2008). Crystal-Associated Synovitis Ultrasonographic Features and Clinical 321 EL-MINIA MED. BULL. VOL. 20, NO. 2, JUNE, 2009 Correlations. Orthopedia Trumatologia Rehabilitacja ; 2(6): 99-110. 3. Pay S and Terkeltaub R. (2003). Calcium pyrophosphate dihydrate and hydroxyapatite crystal deposition in the joint: new developments relevant to the clinician. Curr Rheumatol Rep. Jun; 5(3):235-43. 4. Ea HK and Lioté F. (2004). Calcium pyrophosphate dihydrate and basic calcium phosphate crystal-induced arthropathies: update on pathogenesis, clinical features, and therapy. Curr Rheumatol Rep. Jun; 6(3):221-7. 5. Rosenthal AK. (2007). Update in calcium deposition diseases. Curr Opin Rheumatol. Mar; 19(2):158-62. 6. Frediani B, Filippou G, Falsetti P, et al. (2005). Diagnosis of calcium pyrophosphate dihydrate crystal deposition disease: ultrasonographic criteria proposed. Annals of the Rheumatic Diseases; 64:638-40. 7. Announ N and Guerne PA. (2007); Calcium pyrophosphate dihydrate crystal induced arthropathy. Rev Med Suisse Mar 21; 3(103):740-2, 744, 746. 8. Filippou G, Frediani B, Gallo A, et al. (2007). A "new" technique for the diagnosis of chondrocalcinosis of the knee: sensitivity and specificity of highfrequency ultrasonography Annals of the Rheumatic Diseases; 66:1126-28. 9. Ryan LM and McCarty DJ. (1985). Calcium pyrophosphate crystal deposition disease, pseudogout and articular chondrocalcinosis. In: McCarty D, eds. Arthritis and allied conditions. Philadelphia: Lea and Febiger: 15151546. 10. Richette P, Bardin T, Doherty M. (2009). An update on the epidemiology of calcium pyrophosphate dihydrate crystal deposition disease Rheumatology; 48 (7): 711-715 11. Abreu M, Johnson K, Chung CB, et al. (2004). Calcification in calcium pyrophosphate dihydrate (CPPD) crystalline deposits in the knee: Ali et al anatomic, radiographic, MR imaging, and histologic study in cadavers. Skeletal Radiol; 33:392–8. 12. Falsetti P, Frediani B, Fioravanti A, et al. (2003). Sonographic study of calcaneal entheses in erosive osteoarthritis, nodal osteoarthritis, rheumatoid arthritis and psoriatic arthritis. Scand J Rheumatol; 32: 229-34. 13. Filippucci E, Gutierrez Riveros M, Georgescu D, et al. (2009). Hyaline cartilage involvement in patients with gout and calcium pyrophosphate deposition disease. An ultrasound study. Osteoarthritis Cartilage; 17:178–81. 14. Falsetti P, Frediani B, Acciai C, et al. (2004). Ultrasonographic study of achilles tendon and plantar fascia in chondrocalcinosis. J Rheumatol; 31: 2242–50. 15. (SPSS) Statistical Package for the Social Sciences, Inc., 2000. 16. Bland M. (1987). An introduction to medical statistics. Chrchill Livingstone. 17. Armitage and Berry. (1987). An introduction to medical statistics. Chrchill Livingstone. 18. Derfus BA, Kurian JB, Butler JJ, et al. (2002). The high prevalence of pathological crystals in pre-operative knees. J Rheumatology; 29: 570-574. 19. Viriyavejkul P, Wilairatana V, Tanavalee A, et al. (2007). Comparison of characteristics of patients with and without calcium pyrophosphate dihydrate crystal deposition disease who underwent total knee replacement surgery for osteoarthritis. Osteoarthritis Cartilage; 15(2): 232-5. 20. Nalbant S, Martinez JA, Kitumnuaypong T, et al. (2003). Synovial fluid features and their relations to osteoarthritis severity: new findings from sequential studies. Osteoarthritis Cartilage; 11(1): 50-4. 21. O'shea FD and McCarthy GM. (2004). Basic calcium phosphate crystal deposition in joint-a potential thera- 322 Ali et al EL-MINIA MED. BULL. VOL. 20, NO. 2, JUNE, 2009 peutic target in osteoarthritis. Curr Opin Rheumatol; 16: 273-278. 22. Jaccard YB, Gerster JC, Calame L. (1996). Mixed monosodium urate and calcium pyrophosphate crystal-induced arthropathy. A review of seventeen cases. Rev Rhum Engl Ed; 63: 331–5. 23. Richette P, Bardin T, Doherty M. (2009). An update on the epidemiology of calcium pyrophosphate dihydrate crystal deposition disease. Rheumatology; 48 (7): 711-715 24. Neame RL, Carr AJ, Muir K, et al. (2003). UK community prevalence of knee chondrocalcinosis: evidence that correlation with osteoarthritis is through a shared association with osteophyte. Ann Rheum Dis; 62: 513-518. 25. Malaviya AN, Al-Shari IM, AlShayeb AR, et al. (2001). Calcium )pyrophosphatase dihydrate (CPPD crystal deposition disease in a teaching hospital in Kuwait. Ann Rheum Dis; 60 (4): 416-9 26. Doherty M. (2009). New insights into the epidemiology of gout. Rheumatology; 48 (Supplement 2): ii2-ii8. 27. Roddy E, Zhang W, Doherty M. (2007). The changing epidemiology of gout. Nat Clin Pract Rheumatol;3:443–9. 28. Foldes K. (2002). Knee chondrocalcinosis: an ultrasonographic study of ;the hyaline cartilage. Clin Imaging. 26(3): 194-6. 29. Pereira ER, Brown RR, Resnick D. (1998). Prevalence and patterns of tendon calcifications in patients with chondrocalcinosis of the knee: radiologic study of 156 patients. Clin Imaging; 22: 371-5. 30. Gerster JC, Baud CA, Lagier R, et al. (1977) Tendon calcifications in chondrocalcinosis. A clinical, radiologic, histologic, and crystallographic study. Arthritis Rheum; 20: 717-22. الملخـــص العربــــى تعدداإللتهتباتددامإللهية ددناتإللهعاتتددتإلاددلإلتراددفإللهتننددلرلمإلأددرإللهيةا دد إليددلإل ددرإلل يددرل إل لهرلياتازياتإلإلشالااً. ليلإل شبرإلهذهإللهتننلرلمإلتننلرلمإلتارلألاةامإلله اهادال إل عدا رإللهبادارلتاللإلتنندلرلمإلل داا إل الرلمإلله لاال إللإلتننلرلمإلألاةامإلله اهاال إللهقااااتلإللترافإلهذهإللهتننلرلمإلأرإللهيةا إللإل ل عاتتإل ل إلإللهيةا لإللهذهإللهتنندلرلمإليلتدلابإلت دربإلأدرإللهادا إللهاداعلأرإلهنيريدرإللهدذالإل اعاعللإليلإلخشلعتإلإللهيةا .إل لاعاإللهة صإللهيا رلا لترإلهناا إللهااعلأرإلهلإللهطراقتإللهيؤ ابإلهنتشخاصلإللهلإلاااااإل اياإلً أرإلت اااإلعشاطإللهير .إل لهقدداإل ددت إل إاددتخال إللهيلتددامإلأددلتإلله ددلتاتإلهنتبازلهعيددنرإلله ر ددرإلأددرإلتشددخاصإللا د إل ل يرل إللهرلياتازياتإلذلإليتا إلللاعإللههإليزلااإلاااابإلالإلغارهإليلإللهطرتإلل خر إل ا شدعتإل لهااعاتإللل شعتإللهيقطعاتإلللهرعالإللهيغعاطاار .إل لتاددتخا إللهيلتددامإلأددلتإلله ددلتاتإلهنتبازلهعيددنرإلله ر ددرإلأددرإلتشددخاصإللتهتباتددامإللهية ددناتإل لهعاتتتإلالإلترافإللهتننلرلمإللت اااإلتأ ارهاإلانرإللهيةا إللإلل عاتتإل ل إلإللهيةا د لإللاي دلإل الإلطراقإلإاتخاليباإللهتةرقهإلتالإللتهتبافإلله ااإلللهيزيلإلهنيةا د لإللإلااداااإل ايداًإلأدرإلت ااداإل عشاطإللهير إلليا إلتأ ارإللترافإلهذهإللهتنندلرلمإلاندرإللهيةا د إليدلإلتشدلهامإللتا و د .إللتتيادزإل لهيلتامإلألتإلله لتاتإلهنتبازلهعينرإلله ر رإلتقارتباإلانرإلت اااإللهت ناامإلأدرإللهيةا د إلادلإل ل شعتإللهااعات .إل لااتخا إللهة صإلتيلتامإللهالتنرإلأرإلت اااإللهايلاتإلأرإلل عاتتإل ل إلإللهيةا إلليلإل إلت ااداإل عشاطإللهير .إل 323 Ali et al EL-MINIA MED. BULL. VOL. 20, NO. 2, JUNE, 2009 تننددلرلمإلتارلألاددةامإلله اهاددال إل عددا رإللهباددارلتالإلاعددت إلاعبدداإلتددأ ارإلللي د إلانددرإللهيةا د إل لتترافإلهذهإللهتننلرلمإلأرإللهيةا إللإلل عادتتإل دل إلإللهيةا د إليؤاادتإلإهدرإللهت ناداملإللادزالاإل يعدا إلإعتشددارهاإلتزاداابإل ايددارإللهيريدر.إلل هد إلطراقدتإلهنتشددخاصإلهدرإللهة ددصإللهيا رلاد لترإل هناا إللهااعلأرإلللهتعرفإلانرإلهذهإللهتننلرلمإلللتلاإللهت نادامإلأدرإللهيةا د إللإلل عادتتإل دل إلإل لهيةا .إل لتعاإللهيلتامإلألتإلله لتاتإلهنتبازلهعينرإلله ر رإليلإللهطرتإللهبايدتإلأدرإلتشدخاصإللهت نادامإل لإل ايداًإلأددرإللتددلاإلإرتشددافإلأددرإللهيةا د لإلتا و د إلأددرإللهع ددا لإللتددلاإلإهتبددافإلتا اددا إللهز هاددتإل لل غشاتإللهااعلأات .إل اعاإلير إللهعقر إليلإل رإلل يرل إلشالااًإللهترإلتدؤا إلإهدرإلإهتبدافإللهيةا د إللهدرإلتعدت إلادلإل ترافإلتننلرلمإلل اا إلالرلمإلله لاال إلأرإللهيةا د إلللهتدرإلا دعفإلت ااداهاإلتا شدعتإللهاداعاتإل لل شعتإللهيقطعاتإلللهرعالإللهيغعاطاار .إل تا و إللهع ا إلأرإلل شعتإللهااعاتإلإلأرإلير إللهعقر إل إلا برإلإ إلتعداإليدرلرإليدلإل٦إلإهدرإل١٢إلادعتإل تعاإللت اتتإلتاهير .إل لاعتترإللهة صإللهيا رلا لترإلهناا إللهااعلأرإلللهتعرفإلانرإللتلاإللهتننلرلمإليلإل ه إللهطدرتإل هنتشخاصلإلل اياًإلتعتترإللهيلتامإلألتإلله لتاتإلهنتبازلهعينرإلله ر رإليلإللهطدرتإللهبايدتإلأدرإل تشخاصإلير إللهعقر .إل ً هعاكإلعلعإللٓخرإليلإللهتننلرلمإللهلإلتننلرلمإلألاةامإلله اهاال إللهقااااتإللهذ إلادؤا إل ايداإلإهدرإل لتلاإللهت نا امإللخا تإل دل إلية د إلله تدفلإللإلاعداإللهة دصإللهيا رلاد لترإلهنادا إللهاداعلأرإل للهتعرفإلانرإللتلاإللهتننلرلمإللإلإاتخال إللهيلتامإلألتإلله دلتاتإلهنتبازلهعيدنرإلله ر درإليدلإل لهطرتإللهبايتإلأرإلتشخاصإلترافإلهذهإللهتننلرلم .إل الهدف من الدراسة: تبافإلهذهإللهارلاهإلإهرإلتليا إلالرإلإاتخال إلأ صإللهاا إللهااعلأرإللإللهيلتامإللهةلتإل لتات إل هنتبازلهعينرإلله ر رإلأرإلتشخاصإل يرل إللهيةا إللهعاتتتإلالإلترافإلتننلر .إل المرضى وطرق البحث: تييعمإلهذهإللهارلاتإلادتللإليرايداإلهدااب إلإرتشدافإلتية د إللهر تدتلإللتد إلتقادا إلتيادعإللهيريدرإل إ ناعا ااًإللإلتاهة ل دامإللهيعينادتكإل يداإلتد إللهة دصإلتا شدعتإللهاداعاتإللإللهيلتدامإللهةدلتإل دلتات إل هنتبازلهعينرإلله ر رإللإللهة صإللهيا رلا لترإلهناا إللهااعلأر .إل وقد أظهرت النتائج ما يلي: برمإلل شعتإللهااعات إللتلاإللهت ناامإلأرإلاااإليلإللهيريرإل ق إليلإللهترإل برتباإللهيلتامإل لهةلتإل لتات إلهنتبازلهعينرإلله ر رإلأرإلية إللهر تتإللية إللهراغإلللترإل خانا إللتطاعتإل لهقايال إلييازب إلهتراف إلتننلرلم إلتارلألاةام إلله اهاال إل عا ر إللهباارلتال إلللتلا إلت ناام إلأرإل ية إلله تف إلييازب إلهتراف إلتننلرلم إلألاةام إلله اهاال إللهقاااات إللتلا إللهت ناام إلأر إلية إل لهر تتإلللهيةا إلله غاربإلهنااالإلللهقايال .إل لقا إل لي م إللهارلات إل اااااات إللهيلتام إللهةلت إل لتات إلهنتبازلهعينر إلله ر ر إل ر إليلإل ل شعتإللهااعاتإلأرإلإ بارإللهت ناام .إل ومن ذلك أمكن إستنتاج اآلتى: ال رإلتعي إللهيلتامإللهةلتإل لتات إلهنتبازلهعينرإل إليرا إلهااهإلإرتشافإلتية إللهر تتإل قت إللها فإللاي إللهة صإللهيا رلا لترإلهناا إللهااعلأر. 324