I. ABO Incompatible Kidney Transplants
advertisement

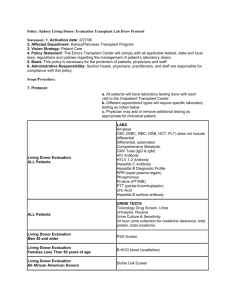
Kidney Transplant Program Standard Operating Procedure Manual Policies and Procedures KID-POL: 0200022.002 High-Risk Renal Transplant Guidelines: ABO Incompatible Transplant Treatment Guidelines Implementation Date: January 1, 2005 Obsolete Date: 3/1/2010 Review Dates: Next Review Date: 01/2009 3/1/2013 Revision Dates: 3/1/2010 Principle and Purpose: Scope: The Transplant Center has established written guidelines for the treatment of ABO incompatible kidney transplants. Transplant Center Multidisciplinary Team Materials: Not applicable Equipment: Not applicable References: Medicare Condition of Participation §482.94 Patient and Living Donor Management Policy/Description: I. ABO Incompatible Kidney Transplants A. Patient Selection 1. Patients without a living ABO compatible donor 2. Living donor ABO incompatible (related or unrelated) 3. A2 donors same as non-A2 B. Removal of Anti-A and Anti-B Antibodies 1. Plasmapheresis prior to and day of transplant (number of PP/IVIG dependent on titer) a. Pre-Tx coordinator to arrange b. 1 plasma volume exchange, replace with 5% albumin c. Follow pheresis with IVIG 100 mg/kg (may round to 10 grams) in ITC d. Last exchange on morning of transplant e. 4 units donor blood type specific fresh frozen plasma given after last exchange prior to the transplant to replenish coagulation factors f. Coordinate pheresis with dialysis to complete both early in the day a) Try to avoid the need for both pheresis and dialysis at the end of the day g. Pre- and post pheresis measurement of Anti-A or B immunoglobulin G (IgG)/IgM titers – use minimal blood volumes KID-POL: 0200022.002 03/10/2010 1 Kidney Transplant Program Standard Operating Procedure Manual Policies and Procedures h. Check CBC daily at time of pheresis C. Immunosuppressive regimen 1. Mycophenolate mofetil 750 mg po bid start with first pheresis 2. Pre Thymoglobulin induction (1.5 mg/kg) for 5 consecutive days prior to transplant, continue through and after transplant as per standard protocol 3. Corticosteroid therapy as in standard TAC/MMF/Pred protocol D. Post-transplant management 1. Daily measurement of donor type antibody titer day 1-7 then qod x 1 weeks a. Anti-A test = isoagglutinin A, test # b. Anti-B test = isoagglutinin B, test # 2. Protocol plasmapheresis/IVIG POD#1, 3 3. Plasmapheresis/IVIG to maintain donor IgG isoagglutinin <1:8 first week, <1:16 week 2. 4. Protocol biopsy at time of renal perfusion intraoperatively, days 3, 7 post transplant. 5. All post-transplant allograft biopsy should include the following studies: Light microscopy, C4d and frozen core in liquid nitrogen and electron microscopy. 6. Process biopsies same day 7. Daily CBC with differential, lyte panel, Prograf. 8. If transfusion necessary, may use standard RBC transfusion. E. Renal allograft dysfunction 1. Urgent biopsy will be considered for rise in s Creatinine >15% or for fever >100.5 F, or evidence of intravascular hemolysis. 2. Biopsy studies to include Light, C4d- process same day, try to get early in day so PP/IVIG can be done if needed. F. Humoral Rejection 1. 2. 3. 4. 5. Plasmapheresis same day if signs of HR on biopsy. Set up pheresis to be early in the day Call Transfusion Medicine Resident on call (127-05160) to set up. Measure antibody titer daily x 7 days prior to every PP/IVIG. Utilize albumin as replacement fluid and follow with 100 mg/kg IVIG rounded to 10 grams. Pulse methylprednisolone following routine protocol described for the treatment of kidney acute rejection. H. Cellular Rejection- same as for ABO compatible kidney transplants KID-POL: 0200022.002 03/10/2010 2