neurological fetal
advertisement

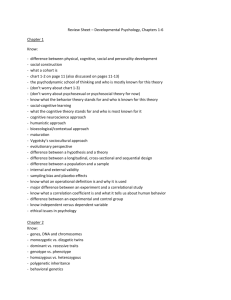
Can long term neonatal outcome be predicted by antenatal surveillance? S. Škrablin, D. Kalafatić, E. Juretić, G. Zlopaša, T. Goluža, I. Kuvačić INTRODUCTION A growing body of evidence strongly suggests that the majority of longterm developmental handicaps, especially neurologic, originate from fetal asphyxial insults during intrauterine life, rather than during labor (1,2). Intrauterine growth retardation (IUGR) is a well-recognized risk factor for permanent neurologic damage (3). Significantly higher incidence of minor motor and cognitive deficits, such as hyperactivity, short attention span or learning difficulties, are observed in those cases, especially when preterm birth or postnatal complications supervene (3,4). Furthermore, major neurologic deficits, such as infantile cerebral palsy, can be attributable to insults occuring in early pregnancy (5). Various parameters of fetal circulation, registered by Doppler ultrasonography, are able to predict IUGR and adverse perinatal outcome. The earliest and most sensitive detectors of IUGR and fetal hypoxia are the cerebralumbilical and cerebral-aortic ratios of blood flow pulsatility indices (6). Fetuses with IUGR and dramatic circulatory disturbances of the umbilical artery (absent or reverse end-diastolic flow) had a three-fold increase in the risk for neurologic damage compared with fetuses with IUGR only (7). On the other hand, most studies (8,9), although not all (10), failed to confirm that increased cerebral blood flow was an additional risk factor for intracranial haemorrhagic and ischemic lesions, as well as for permanent neurologic disabilities. Recent longitudinal study of Ley and co-workers was the first one to reveal the significance of abnormal blood flow pattern in fetal aorta in prediction of minor neurological deficits at seven years of age (11). Therefore, it seems obvious that changes in fetal hemodynamics, both independently and in combination with well-known obstetrical risk factors, play an important role in the postnatal neurodevelopment. The aim of our study was to reveal the most significant perinatal predictors of neurologic abnormalities in children at 3 to 5 years of age. MATERIALS AND METHODS We performed fetal blood flow velocity examinations in 132 high-risk pregnancies, over a three year period, at the Department of Obstetrics and Gynecology in Zagreb. Ultrasonographic biometry and Doppler blood flow measurements were performed using 3,5 MHz transabdominal transducer and 50 Hz wall filter. Doppler flow analysis was carried out during episodes of fetal apnea. Peak systolic (PSV) and end-diastolic velocity (EDV), as well as resistance indices (RI) were obtained for fetal middle cerebral artery, umbilical artery and fetal descending aorta. The results of the last set of measurements (median: 6 days before delivery) was used for the analysis. Pregnancy and newborn characteristics that were collected and analyzed regarding neurodevelopmental outcome included: gestational age at delivery, birth weight, body weight ratio (neonatal birth weight divided by expected birth weight at the 50th centile for the corresponding gestational age), 1- and 5- minute Apgar scores, fetal heart rate pattern, neonatal acid-base status, clinical signs of neonatal hypoxic-ischemic encephalopathy, other early neonatal complications: infection, additional oxygenation or artificial ventilation, if needed, emergency caesarean section rate and neonatal intensive care unit (NICU) admission. The diagnosis of IUGR was made when birthweight was below the 5th centile according to reference growth curves for our population (12). Thirty-eight out of 132 children (28,8%) met that criterion and were considered as being small for gestational age. Six of them died in utero and 3 infants died during the early neonatal period. The blood velocity waveforms in the umbilical artery and fetal aorta were converted into blood flow classes: BFC I (normal, positive blood flow during the whole cycle), BFC II (no end-diastolic velocity) and BFC III (no positive flow throughout diastole or reverse diastolic flow). Cerebral-umbilical ratio was calculated by dividing middle cerebral artery RI with umbilical artery RI. Values below one were considered abnormal. RESULTS One hundred and twenty-eight singleton pregnancies were included in the analysis. Eight children died in utero and 6 subsequently died during the early neonatal period. Asphyxia was the principal cause of perinatal death, being responsible for death in 9 out of 14 children (64,3%). At three years of age 19 infants suffered neurologic illness: 4 of them major neurologic impairment and 15 minor or mild form of the disease. Three out of 4 children with major neurologic illness had fully expressed cerebral palsy with spastic diplegia; the remaining child suffered mental retardation with severe generalized convulsions. Analysis of variance revealed that the mean gestational age at birth of healthy children was significantly higher in comparison to any of the remaining groups. In comparison to all other groups, children that died had significantly lower Apgar indices and were significantly more often in need for artificial respiration. In comparison to healthy children, those who suffered minor or mild neurologic disease had significantly lower Apgar score values; they were significantly more often growth retarded, their mean birth weight was lower and newborn encephalopathy observed more frequently. They spent significantly longer period in neonatal intensive care unit and they needed additional oxygenation and artificial respiration more frequently. Children from both groups, those that died and those with mild/minor neurological handicap were, in comparison to healthy children, significantly more often growth retarded, their birth weight was significanlty lower and they suffered signs of perinatal hypoxia more often. No differences in Apgar score values, pH, base deficit, birth weight and body weight ratio were observed between healthy children and children who suffered major neurologic impairment. No one was growth retarded, and in only one antenatal FHR showed alterations suggestive of hypoxia. In comparison to healthy children, gestational age at birth in children with major disabilities was, however, significantly lower. Their NICU admission was more frequent, as was their need for additional oxygenation significantly longer than in healthy children. In l out of 4 newborn encephalopathy was diagnosed. Caesarean section rate, umbilical arterial, fetal aortic and middle cerebral artery PSV and EDV were equally distributed between the groups. In two out of 96 healthy newborns positive neonatal neurosonography was encountered in a form of mild subependimal haemorrhagic lesions in two growth- retarded infants. Positive neonatal neurosonography was more frequent in neurologically disabled children: in three out of four (75%) with major neurologic deficit third degree periventricular leucomalatia (PVL) eventually occured after a period of periventricular echodensities. Intraventricular haemorrhage was observed in two, third degree PVL in one, second degree PVL in two, subependimal haemorrhage in two and diffuse edema in one out of 14 newborns with milder neurologic handicap. There was no difference in C/U ratio between children with mild/minor abnormalities or those with major abnormalities and healthy ones and no difference in middle cerebral artery RI between any of the groups. Umbilical artery RI was significanlty higher and C/U ratio significantly lower in children that died than in those remaining healthy and in those suffering major difficulties. Importantly, mean aortic RI was significantly higher in the group of children with minor form of neurologic disease, compared to the healthy and major abnormality group. Converting blood velocity waveforms in fetal aorta and umbilical artery into semi-quantitative blood flow classes (BFC), it turned out that 111 out of 132 children (84,1%) had positive blood flow in the umbilical artery throughout the heart cycle. Twenty children (15,2%) had no end-diastolic velocity (BFC II) and only 1 child (0,7%) had reversed diastolic flow (BFC III). Eleven out of 104 liveborns with umbilical arterial BFC I (10,3%) and 4 out of 17 liveborns with umbilical arterial BFC II (23,5%), showed positive neonatal neurosonography, (p=NS). One hundred and six out of 132 children (80,3%) had BFC I in the aorta, 23 (17,4%) had no end-diastolic blood flow, and 1 child (0,7%), who had reverse end-diastolic flow in the umbilical artery, also had reverse diastolic flow in the aorta. That child subsequently died from asphyxia in the 32nd week of gestation, complicated by severe IUGR and oligohydramnios. Positive neonatal neurosonography was observed in 9 out of 103 liveborn children with aortic BFC I (8,7%) and in 6 out of 20 (30%) liveborns showing aortic BFC II (p<0,01). Absent or reversed aortic flow shows danger of either dying during the perinatal period or suffering intracranial pathology during the early neonatal period, although most of the newborns with subsequent sequellae showed umbilical arterial and aortal BFC I. Univariate analysis revealed significant association between aortic RI, gestational age at birth, IUGR, 1’ and 5’ Apgar score, FHR tracing, birth weight, body weight ratio, newborn hypoxic-ischemic encephalopathy, the need for arteficial oxygenation, positive neonatal neurosonography and minor neurologic dysfunction. The results of the univariate analysis are summarized in Table 1. The results of the multivariate analysis are presented in Table 2. It is important to notice that only positive cranial ultrasonography and aortic BFC II showed significant independent predictive value regarding postnatal neurodevelopment. Multivariate analysis of the risk of selected factors on the occurence of major neurologic sequellae (stepwise logistic regression) did not reveal significance of any of the factors tested. Table 1. Summary of univariate analysis of significantly different variables between healthy children and children with minor/mild neurologic impairment Healthy Minor/mild children impairment p (N=99) (N=15) Gestational age (weeks) 37,9 35,3 <0,01 Birthweight (g) (mean) IUGR (N,%) 2722 2099 <0,01 22 (22,2) 7 (46,7) <0,001 Body weight ratio 0,91 0,86 <0,05 Aortic RI (mean) 0,86 0,92 <0,05 Aortic BFC II (N,%) Neonatal USG (N, % positive findings) Suspected perinatal hypoxia (FHR) (N,%) Apgar 1' (median) 15 (15,2) 6 (40,0) <0,05 2 (2,0) 8 (53,3) <0,001 20 (20,2) 7 (46,7) <0,05 10 7 <0,05 Apgar 5' (median) 10 9 <0,05 Neonatal encephalopathy (N,%) Neonatal infection (N,%) Arteficial oxygenation (N,%) 4 (4,0) 5 (33,3) <0,001 9 (9,1) 5 (33,3) <0,05 1 (1,0) 2 (13,3) <0,01 Table 2. Multivariate analysis of risk to minor/mild neurologic impairment (logistic regression) 95% confidence Odds ratio p interval Preterm birth 0,79 0,51-1,05 0,4597 Birthweight 1,01 0,90-1,21 0,3233 IUGR 1,76 1,08-2,67 0,0775 Body weight ratio 0,24 0,15-0,45 0,7717 Aortic RI > mean + 2 S.D. 1,46 1,21-1,85 0,1154 Cranial USG 3,12 2,15-7,59 0,0082 Aortic BFC II 2,03 1,25-5,36 0,0105 Positive FHR 0,61 0,42-0,91 0,1132 Apgar 1' (<7) 0,88 0,78-1,01 0,2748 Apgar 5' (<7) 0,59 0,41-0,95 0,8894 Newborn encephaloptahy 1,28 1,15-1,44 0,7443 Newborn infection 0,74 0,66-0,88 0,8691 Arteficial oxygentaion 1,31 0,85-2,21 0,2101 CONCLUSION As pathological patterns of fetal blood flow distribution are often associated with various obstetrical complications per se, it is difficult to distinguish permanent neurologic disability independently predicted by various complications of pregnancy and/or early neonatal period and those somehow predicted by some circulatory abnormality. Positive neonatal cranial ultrasonography showed significant predictive value regarding both major and minor neurologic impairment later in life. Blood circulation in fetal aorta could be an important milestone in detection of fetuses at increased risk, perhaps irrespective of their gestational age at birth. We therefore recommend cranial ultrasonography examination to all neonates with absent or reversed blood flow in descending aorta. The combination of both positive findings, regardless of gestational age at birth, carries a significantly increased risk of permanent neurologic damage. REFERENCES 1. Godfrey KM. Maternal regulation of fetal development and health in adult life. Eur J Obstet Gynecol Reprod Biol 1998;78:141-50. 2. Garaizar C, Prats-Vinas JM. Brain lesions of perinatal and late prenatal origin in a neuropediatric context. Rev Neurol 1998;26:934-50. 3. Calame A, Fawer CL, Claeys V, Arrazola L, Ducret S, Jaunin L. Neurodevelopmental outcome and school performance of very low birthweight infants at 8 years of age. Eur J Pediatr 1986;145:461-6. 4. Michelsson K, Noronen M. Neurological, psychological and articulary impairment in five-year-old children with a birthweight of 2000 g or less. Eur J Pediatr 1983;141:96100. 5. Michaelis R, Rooschz B, Dopfer R. Prenatal origin of congenital spastic hemiparesis. Early Hum Dev 1980;4:243-55. 6. Arbeille P. Fetal arterial Doppler-IUGR and hypoxia. Eur J Obstet Gynecol Reprod Biol 1997;75:51-3. 7. Valcamonico A, Danti L, Frusca T, et al. Absent end-diastolic velocity in umbilical artery: Risk of neonatal morbidity and brain damage. Am J Obstet Gynecol 1994; 170: 796-801. 8. Scherjon SA, Smolders-de Haas H, Kok JH, Zondervan HA. The "brain-sparing effect": antenatal cerebral Doppler findings in relation to neurologic outcome in very preterm infants. Am J Obstet Gynecol 1993;169:169-75. 9. Arias F. Accuracy of the middlecerebral-to-umbilical-artery resistance index ratio in the prediction of neonatal outcome in patients at high risk for fetal and neonatal complications. Am J Obstet Gynecol 1994;171:1541-5. 10. Scherjon S, Briet J, Oosting H, Kok J. The discrepancy between maturation of visualevoked potentials and cognitive outcome at five years in very preterm infants with and without hemodynamic signs of fetal brain-sparing. Pediatrics 2000;105:385-91. 11. Ley D, Laurin J, Bjerre I, Marsal K. Abnormal fetal aortic waveform and minor neurologic disfunction at 7 years of age. Ultrasound Obstet Gynecol 1996;8:152-9. 12. Dražančić A, Pevec-Stupar R, Kern J. Fetal growth in Zagreb. Jugoslav Ginekol Perinatol 1988;1-2:13-20.