Medical Terms Made Easy - Oklahoma State University
advertisement
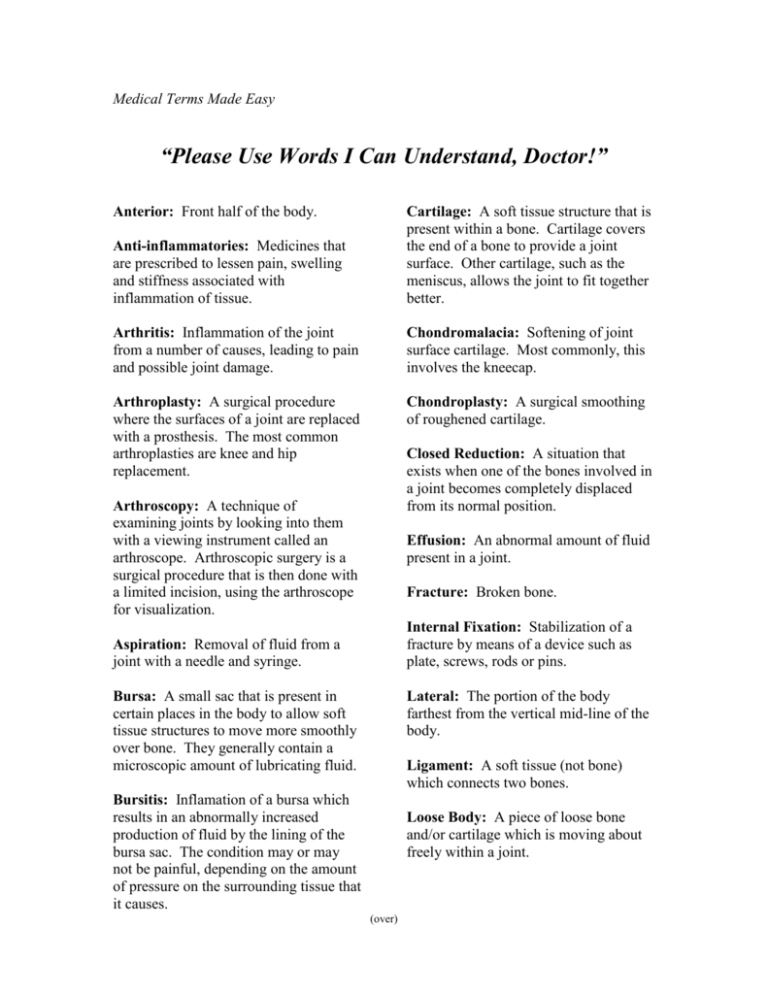
Medical Terms Made Easy “Please Use Words I Can Understand, Doctor!” Anterior: Front half of the body. Anti-inflammatories: Medicines that are prescribed to lessen pain, swelling and stiffness associated with inflammation of tissue. Cartilage: A soft tissue structure that is present within a bone. Cartilage covers the end of a bone to provide a joint surface. Other cartilage, such as the meniscus, allows the joint to fit together better. Arthritis: Inflammation of the joint from a number of causes, leading to pain and possible joint damage. Chondromalacia: Softening of joint surface cartilage. Most commonly, this involves the kneecap. Arthroplasty: A surgical procedure where the surfaces of a joint are replaced with a prosthesis. The most common arthroplasties are knee and hip replacement. Chondroplasty: A surgical smoothing of roughened cartilage. Closed Reduction: A situation that exists when one of the bones involved in a joint becomes completely displaced from its normal position. Arthroscopy: A technique of examining joints by looking into them with a viewing instrument called an arthroscope. Arthroscopic surgery is a surgical procedure that is then done with a limited incision, using the arthroscope for visualization. Effusion: An abnormal amount of fluid present in a joint. Fracture: Broken bone. Internal Fixation: Stabilization of a fracture by means of a device such as plate, screws, rods or pins. Aspiration: Removal of fluid from a joint with a needle and syringe. Bursa: A small sac that is present in certain places in the body to allow soft tissue structures to move more smoothly over bone. They generally contain a microscopic amount of lubricating fluid. Lateral: The portion of the body farthest from the vertical mid-line of the body. Ligament: A soft tissue (not bone) which connects two bones. Bursitis: Inflamation of a bursa which results in an abnormally increased production of fluid by the lining of the bursa sac. The condition may or may not be painful, depending on the amount of pressure on the surrounding tissue that it causes. Loose Body: A piece of loose bone and/or cartilage which is moving about freely within a joint. (over) Medial: Potion of the body closer to the vertical mid-line. Open Fracture: When a fracture is associated with a wound of the skin and soft tissue overlying the bone that allows the fracture to be exposed to air. This can vary from a small puncture wound of the skin to a situation where the bone actually protrudes through the skin. Open Reduction: Correction of a bone deformity associated with a fracture or dislocation that requires surgical techniques opening the skin. Orthotic: A fancy word for a brace. Plica: A fold of joint lining (synovium) which may become injured or scarred and then be a source of pain in the knee. A plica sometimes mimics symptoms of chondromalaci or a torn cartilage. Posterior: Back half of the body. Prone: Lying on the stomach. Prosthesis: An artificial body part, such as a knee or hip joint. Steroids: Cortisone or its derivatives which are used to treat inflammation, not to be confused with anabolic steroids which are used for muscle building. The use of these anabolic steroids is restricted. Subluxation: A situation that exists when one of the bones involved in a joint becomes partially displaced. A subluxation is between a normal position and a completely dislocated position. Supine: Lying on the back. Synovial fluid: The fluid that is present within a joint. The normal synovial fluid lubricates and nourishes the cartilage of the joint surface. Tendon: A soft tissue structure that connects muscle to bone. Tendinitis: Inflammation of a tendon and its surrounding sheath. Total Hip replacement: A surgical procedure where the ball and socket of a hip joint is replaced with a prosthetic device. Source: Orthopedic & Arthritis NEWS, May, 1994, A publication of The McBride Clinic and Bone & Joint Hospital. Prepared by Thomas C. Howard, III, M.D., Clinical Associate Professor, Department of Orthopedic Surgery, University of Oklahoma College of Medicine. Dr. Jan Park, Gerontology Specialist, Oklahoma Cooperative Extension Service, OSU. (Handout) Efficiency Principles If you plan and organize your tasks and workspaces, you will eliminate unnecessary steps, which saves time and energy. This helps reduce fatigue. Hasty movements are no more quickly accomplished than organized movements and they often end in extra work. As the saying goes, “Haste makes waste”. Both tension and fatigue are increased when we feel rushed. Plan -- Determine the following: Is the task necessary? Can the task be simplified? Who should perform the task? What steps are involved in completing the task? In what order will these steps be most efficient? What is the best time of day or week to perform the task? Do you need rest periods to complete the task? What is the best body position to use to complete the task? Examples of How to Outsmart Arthritis Start large tasks well before the deadline so you can pace yourself, e.g., income tax, school papers, bills, greeting cards. Make entertaining easier. Spread tasks over several days. Select foods that you can prepare ahead of time. Get help for heavy cleaning. Alternate repetitive cooking tasks such as cutting, chopping and stirring to reduce stress on your hands. Take short breaks when cooking large quantities. Alternate sitting and standing to reduce fatigue and joint stress. Buy vegetables and condiments already chopped in the frozen food and produce section of your grocery to simplify cooking. Salad bars at grocery stores are an excellent place to purchase fresh precut vegetables and fruits. List your regular cleaning tasks. Create a cleaning schedule that works for you. Consider spreading out light cleaning tasks over a week. Schedule one or two heavy cleaning tasks per month. Complete them on a “good day”. Use computer address and return labels for mail to reduce writing strain. Source: Lorig, K. & Fries, J. (1995). The Arthritis Helpbook, 4th Edition. Dr. Jan Park, Gerontology Specialist, Oklahoma Cooperative Extension Service, OSU