Solutions ED overcrowding
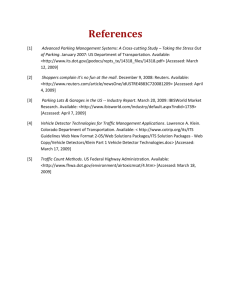
advertisement

18 August 2009 Confidential to the ED Advisory Group and MoH contributors until approved for web publication Solutions to emergency department (ED) overcrowding: a literature review July 2009 Introduction Emergency Departments need to be viewed in the context of the communities they serve, because ED improvements must 1. result from tailored solutions to meet each community’s own specific set of needs for the right treatment to be available at the right time in the most appropriate place (Alberti G, 2007) and 2. not be limited to the ED, but made across the whole hospital and social care community (Richardson DB, 2001, Sprivulus PC, Da Silva J-A, et al, 2006, Wilson MS, Siegel B, Williams M, 2005). The Working Group for Achieving Quality in Emergency Departments stated that “solutions to ED problems will need to address the underlying causes, and therefore span not only the ED, but the whole of the hospital and indeed the whole acute care system…Implementing such solutions requires engagement and co-ordination from the highest levels of the health system, including the Ministry and DHB CEOs” (Working Group, 2008). Purpose To support District Health Boards (DHBs) to achieve the Health Target announced in April 2009, to have 95% of presentations to EDs admitted, transferred or discharged within six hours, potential solutions need to be identified to problems with ED service quality, with special reference to factors that contribute to overcrowding. The following literature review is intended as a resource for the Ministry of Health and DHBs, to stimulate discussion on ways of reducing ED overcrowding and length of stay, to meet the ED length of stay target. Method The founding documents for the following literature review were the report of the Working Group for Achieving Quality in Emergency Departments (Working Group, 2008) and the UK systematic review (Cooke M, Fisher J, et al 2005). A series of literature searches covered journal articles and other published works. The search method, sources and key words are in the Appendix. Studies were selected for the likely relevance of their findings for reducing ED length of stay in NZ and fell, with a few overlaps, into the following eight categories: 1. Developing and adopting a national acute care strategy 2. Using master plans within hospitals 3. Concentrating on ‘primary care’ presentations 4. Managing acute demand 5. Hospital capacity planning / managing access block 6. Developing the ED workforce 7. Using other wards and units as an alternative to the ED 8. Improving data quality and monitoring. 1 18 August 2009 Confidential to the ED Advisory Group and MoH contributors until approved for web publication Limitations Without a body of NZ ED research, it was necessary to look to international studies. The limitations of those are that 1. extensive research programmes are still needed to help to inform the major changes occurring in the delivery and organisation of emergency health care (Cooke M, Fisher J et al 2005) and 2. there is a lack of consistent outcome measures and definitions which makes it difficult to combine study results and to assess whether they can be generalised. A key example of the problem with definitions is the lack of an agreed and clear definition for reporting on access block. Such a definition is important for ED governance, management, performance and accountability but in August 2008, there was no agreement across Australia that the ACEM definition applies (Government of Western Australia, Department of Health, 2008). Defining access block That debated definition of access block is “the situation where patients in the ED requiring inpatient care are unable to gain access to appropriate hospital beds within a reasonable timeframe. It is expressed as the proportion of patients requiring admission to a hospital who have a total ED time greater than eight hours” (Forero R, Mohsin M, et al, 2004). The following diagram and explanatory notes illustrate the thinking underpinning the definition: ACHS–ACEM1 definition: Total time in the emergency department (from arrival time to departure time) exceeding 8 hours. NSW Health definition 1: Active treatment and delay time (from medical assessment time to departure time) exceeding 8 hours. NSW Health definition 2: Delay time (from ready for departure time to departure time) exceeding 4 hours. Time delay definition: Delay time exceeding 2 hours. (Forero R, Mohsin M, et al, 2004) UK evidence for solutions to reducing ED overcrowding, applied to NZ As a starting point for this literature review, a small group of NZ experts gave their opinion on the key findings from the UK evidence for solutions to reducing attendances and waits (ED length of stay) as presented in a seminal UK systematic review (Cooke M, Fisher J, et al 2005). The summary of those findings and the NZ experts’ opinions are presented in the following table: 1 ACHS–ACEM = Australian Council on Healthcare Standards and Australasian College for Emergency Medicine. 2 18 August 2009 Confidential to the ED Advisory Group and MoH contributors until approved for web publication UK findings (Cooke M, Fisher J, et al 2005). NZ expert opinion – from Ministry of Health Chief Advisors and senior managers across a range of teams. It is possible to divert some 999 calls to advice lines but the safety of such systems is still being evaluated. Broadly agree but it is unclear in NZ what proportion of 111 calls could be managed safely elsewhere and Healthline is not intended as an alternative to 111 calls. Rather than diverting calls from 111, the approach for primary care is to have formalised arrangements that provide better management of acute demand. For this to happen effectively, the primary sector must be equipped with the right skills and capacity. The UK evidence is reasonably compelling (Mason S and Knowles E, et al, 2007) (Mason S, O’Keeffe C, et al, 2007) (Gray JT and Walker A, 2008). However, there is a risk of using paramedics in making appropriate destination decisions in the NZ context because the competency requirements and training opportunities may be less well developed than in the UK. The role of paramedics in either discharging patients from the scene or deciding on appropriate destinations had not been adequately studied to confirm its safety and effectiveness. Individuals usually make their own destination decisions, and so assisting paramedics, including the 100 new ones, to take on this decision-making role will be important and at least as safe as individuals making those decisions themselves. The perverse incentive to transport patients will need to be addressed in NZ. At present, ACC only pays for patients who are transported. There are also perverse incentives that encourage hospital transfer. To avoid confusing staff on the phones, St Johns has adopted a policy of giving the same message for medical calls and ACC calls. There is no evidence for the effects on ED length of stay of general practitioners working in EDs. Broadly agree. The Working Group and the Australasian College of Emergency Medicine concur with this view (ACEM 2001, 2004a and 2004b). Nelson Marlborough DHB has used general practitioners in their ED in the past but due to increasing complexity of patient presentations and the volume of presentations, it was mutually agreed to staff a separate after hours primary care facility and retain the ED using senior medical officers to provide cover2. Their ED staff may refer patients to the GP service adjacent to the ED but the ED needs to be resourced for very acute and emergency needs of the district (Nelson Marlborough DHB, 2008). There is no NZ evidence of the effect of having GPs in EDs on ED length of stay. Resource utilisation and admission rates may well be 2 The ED is now covered 0800 – 2300 by non-vocationally registered Senior Medical Officers and as a consequence there is reduced demand on inpatient SMOs to assist in the ED now that the new SMO model has taken effect. (Conversation with Wairau Hospital staff, July 2009). 3 18 August 2009 Confidential to the ED Advisory Group and MoH contributors until approved for web publication UK findings Primary care gatekeeping can reduce ED attendance but its safety is unknown. equivalent when the GP works in the ED, but maybe the question should be about the impact of this approach on the right people getting the right care in the right setting, rather than just on length of stay. NZ expert opinion Not sure if this applies in NZ because the role of primary care could be broader than just gatekeeping and probably needs to be. For example, it may be that the impact of shifting even a small percentage of emergency services to primary care is greater than previously thought. Modelling is needed to assess the impact comparatively. That aside, it is true to say that primary care acts as a gatekeeper to much of the health system3. For instance, ambulances sometimes transport patients to primary care for assessment prior to transport to ED. More of this could be done, and may result from the Urgent Care Community Pilot being conducted in Kapiti, which is achieving good results4. Walk-in centres and NHS Direct have not been demonstrated to reduce ED attendances. Countries with strong primary health systems can perform gatekeeping functions well, so it is difficult to see why the UK evidence is that its safety is unknown. Perhaps it would be better to say that there is no evidence that such an approach is unsafe. These do not appear to be relevant ways of reducing ED presentations in NZ. In the NZ context, we have good access to same day general practice services and one of the lowest rates of people using ED services for primary health care services. These are two findings are from the Commonwealth Fund and appear to be related (Davis K, Schoen C et al, 2007). See also comments under “phoning for advice” below. In NZ, ‘minors’ are more likely to attend an A&M clinic than an ED and therefore NZ EDs may have a different case-mix from UK ‘A&Es’, with a smaller proportion of people presenting for minor emergencies and consequently less value to gain from walk-in centres and minor injury clinics. Walk-in centres and telephone advice appear to focus on convenience rather than severity and so it is understandable that they have not been demonstrated to reduce ED attendances. NHS Direct refers to a health advice and information service while NZ has HealthLine and Homecare Medical Ltd. Neither of these services is a triage service used in emergency situations. To evaluate the Healthline service, a 3 The impact of primary care gatekeeping is likely to be greater in mid-sized and smaller EDs, and less in tertiaries. It is also likely, although unclear, that ED attendances will be reduced in those mid-sized cities that have A&M clinics which handle lower acuity presentations. 4 To date, there is only anecdotal evidence of good results. Conversation with Andy Long, Manager, Kapiti Community Care Pilot 4 18 August 2009 Confidential to the ED Advisory Group and MoH contributors until approved for web publication general public survey was conducted in 2001, with positive findings such as Q7a 93% of those 431 people surveyed agreed or strongly agreed that Healthline is a good alternative if you cannot get to a doctor and Q7e 63% agreed or strongly agreed that they would call Healthline if they wanted to check up on advice or medicine they had been given (BRC, 2002). UK findings Triage is a risk management tool for busy periods but may cause delays in care (Asplin BR, 2001 and George S, Read S, et al, 1992). Triaging out of the ED can reduce numbers but more work is required to assess the safety of such systems5. NZ expert opinion Primary and secondary care need to work to the same patient pathways and protocols if triage tools, as opposed to streamlining, are to be effective – otherwise ways to game the system proliferate. Workforce limitations restrict the use of triage tools. Triage always causes a delay in care but sometimes does enough good to provide net benefit. Not sure is this applies in NZ. The College of Emergency Nurses is opposed to triaging out (triaging away) because health care should not be denied to any patient requesting care from an ED there is no provision by the Ministry of Health or ACEM for utilising the triage interview and decision to restrict access to the ED and because there is no support in the literature for the practice of triaging away (CENNZ-NZNO, 2007). The Working Group that reported on improving quality in EDs in 2008 and also developed the Sector Disposition Tool is opposed to it also (Working Group, 2008). On the other hand, AMPA, the Association for A&M Clinics supports triaging out but not to all general practices; their view is that AMPA trained doctors6 must be part of the arrangements and proper contractual and funding arrangements must be made. They wrote: AMPA supports ACEM's views on Emergency Department matters generally, including its views on triaging out, and acknowledges the importance of issues such as of access block (inability to transfer patients from the ED to a ward) in ED waiting times. Accident and Medical practitioners and Clinics treat all patients who attend, including those referred from 5 The ED Working Group Report (2008) summarises Cooke, Fisher, et al on the topic of triaging out as follows: “Between 15 and 27 percent of patients can be ‘triaged out’ (i.e. referred from the ED triage desk to primary care). However: Only a third may be willing when asked and one percent will be dissatisfied Up to a third of patients may be triaged our inappropriately, although many studies report no adverse outcomes One percent may subsequently be admitted to hospital”. Cooke, Fisher, et al refer to Society for Academic Emergency Medicine’s position statement on the ethics of triage which is that “if the principle of ‘triage out’ is to be adopted, then its acceptability to patients, its safety and it efficacy must all be assessed.” Their reference for this is: Schmidt TA, Iserson KV, Freas GC, et al (1995). Cooke, Fisher et al list the present policy status of triage out as ‘local decision’ (Cooke M, Fisher J, et al, 2005). 6 AMPA’s view is that they must first train doctors, get that right and then move on to training nurses (conversation with AMPA’s Chief Executive in July, 2009). 5 18 August 2009 Confidential to the ED Advisory Group and MoH contributors until approved for web publication Emergency Departments. AMPA does not object to the concept of "triaging out"7. Others say that triaging out may be a good thing, given the absence of adverse outcomes for up to a third of the people triaged out “inappropriately” (with reference to footnote 5, bullet point 2 above). They see that a core function of any health worker is to refer people to other parts of the health system that may better meet their needs. ED staff do this already when they are presented with someone needing hospital specialist expertise. UK findings NZ expert opinion Fast track systems for minor True in NZ and already done in some places, with ACC injuries reduce ED length of funding of Accident and Medical Clinics’ services. Senior stay and ideal configurations Staff (doctors and nurses) need to provide mentoring and include senior staff. support, not always to see people directly. Attendance by the elderly, True in NZ and work being done by the Ministry of Health those with long term and DHBs in the areas of Acute Demand Management and conditions and those with Long Term Conditions Management are important. The multiple attendances may be Ministry of Health’s Primary Health Care Implementation reduced by various plan covers better integration of social services with primary interventions. Trials are care and care of the elderly which will help reduce ED needed in this area, attendances. Sustainability of services for older people is a including the role of social service risk DHBs have not focused on and in particular workers. they have not focused on the risks associated with increasing obesity, reduced workforce, and the growing proportion of older people. The benefit of patient Yes. Patient education as part of discharge planning and education is unproven in increased integration with social services (see under most areas except long term attendance by the elderly above) is likely to be beneficial for conditions management. long term condition management, but it is difficult to know what kinds of national patient education on ED use would be relevant in NZ because drivers of acute demand differ significantly across the country. For instance there is disproportionate ED demand driven by Māori in Middlemore Hospital but not in Capital and Coast DHB. Also, we do not know if there are differences in the benefit of patient education for Māori and Pacific populations as compared with the rest of the population. Also, even in long term conditions management, many education packages are proven to be ineffective. Phoning for advice before Agree. With reference to overnight ED attendance, phoning going to the ED may reduce for advice is likely to be effective in reducing ED attendances. attendances, but only if general practices have 24 hour cover arrangements in place as required of them in their contracts with their PHOs. Many GPs now have phones diverted to HML but do not always have the required faceto-face arrangements formalised as back-up. Another risk for effective service delivery is that sharing of primary/secondary clinical information is difficult without electronic health records. Specialist nurse care in Not sure if this applies in NZ. These have not been 7 Email from AMPA’s Chief Executive 17th August 2009 6 18 August 2009 Confidential to the ED Advisory Group and MoH contributors until approved for web publication heart failure, chronic obstructive pulmonary disease (COPD) and deep vein thrombosis (DVT) can reduce hospital admissions. evaluated in NZ and comparing results of care across the different disease states is risky. However, the systematic literature review of the interventions that may reduce Ambulatory Sensitive Hospitalisations (ASH) found that programmes that combined educational interventions with comprehensive disease management programmes were likely to be beneficial and comprehensive, multidisciplinary, team-based medical care programmes were also likely to be beneficial (Health Services Assessment Collaboration, 2008). Current resources seem focused on known patients (i.e. the group referred to as frequent flyers to hospitals). Also, we would need to look at high risk patients who have not used hospital systems. We need an integrated approach to address social determinants, otherwise we are only addressing symptoms of an underlying problem. UK findings Observation wards may reduce ED length of stay and avoid admission. Home support (medical and social) can reduce hospital admissions. There is a lack of evidence in innovations in bed management. Such specialist nursing care is likely to be part of effective care pathways and needs to be included in planning for the shift of some emergency services from secondary to primary settings. NZ expert opinion Yes. In NZ, the systematic literature review referred to above (Health Services Assessment Collaboration, 2008) with reference to Specialist Nurse Care showed that disease specific observation units in EDs were associated with reducing ASH for specific conditions. Also, many PHOs already have Primary Options for Acute Care (POAC) programmes and utilise overnight stay and observation in the private sector. The results to date from CMDHB POAC projects are promising, but are not yet proven to be sustainable, or even generalisable8. The unique circumstances of CMDHB may well have been responsible for the impact of the initiatives (Gribben B, 2003). In NZ, observation wards may not necessarily reduce length of stay and they may be just another holding pen for patients who slip through the cracks. Strong agreement. Good evidence from NHS. In NZ: Home support is included in the Primary Health Care implementation plan and includes case management by nurses Home Based Rehabilitation is funded by ACC. Not sure if this applies in NZ. There are some innovative practices, for example in Auckland DHB, and perceptions of success. However, bed management studies are hard to do because monitoring data is lacking on admissions from ED, and consequently it is difficult to find if the patient in ED with 8 The unique circumstances of CMDHB may well have been responsible for the impact of the initiatives (Gribben B, 2003). 7 18 August 2009 Confidential to the ED Advisory Group and MoH contributors until approved for web publication Allowing ED staff to admit patients to wards will reduce delays. There is a lack of evidence about innovations to reduce delayed discharges from hospital. UK findings Most evidence looks at the causes of delay rather than the solutions. Teams of staff available for unpredicted surges may reduce delays. Rotational allocation of patients may be better than clinical self-determination10. Senior staff may reduce admissions and delays. Nurse practitioners are safe the next most serious problem is the one admitted next. This is likely to be important for NZ but there is a risk that wards will fill up to the extent that nobody can admit unless there is surge capacity planning and prediction of demand9. Yes, but Primary Care may not have sufficient infrastructure and capacity to take on all devolved work when innovative models of care begin to be implemented. Further, the discharge process is not only about delay. Generally the process needs to be improved and to be part of jointly constructed care pathways that include social support and access to prescriptions. Good communication is essential between Planning and Funding decision makers and provider arm ED services. Change is system-wide. Delivery of ED services, delivery of elective services and devolution of some secondary services to primary must not be seen in isolation from each other. NZ expert opinion Agree and this also highlights the disincentives for greater productivity / performance. Configuration of primary care as competitive providers with capitation based on enrolled patients, stifles innovation spread. Each DHB should be doing an analysis. For instance, if there is more capacity in primary care, how does that impact on ED service delivery and overcrowding. Yes, depending on the cause of the delay. It is better than rostering surplus staff in cases of peak demand which usually does not happen. A contingency plan responding to early ED overcrowding is important, particularly in instances where predictable overcrowding happens at certain times of the week. No comment. Strong anecdotal support but it depends where the problem is and how the supervision is managed. Also, despite an increase in FACEMs in some DHBs, it is not clear that there have been reduced admissions and fewer delays, compared with hospitals that have not had these staff improvements. It could be argued that FACEMs at one end of the scale increase the number of admissions because they are more likely to identify potential problems than junior staff who may miss risk factors, but this increase is balanced by FACEMs’ ability to discharge or refer other patients who can be safely managed in the community. A clinical leader with an inclusive management style is a good predictor of a high performing ED (Coombs M, 2009). The safety and effectiveness of NPs working in EDs is hard 9 There is a demand prediction tool developed by Kaiser Permanente. Once located and when permission is given for it to be used, this needs to be added to the ED Tools database. 10 This means changing from a system where individual doctors determine their own work rate, by seeing the next patient when they are ready. 8 18 August 2009 Confidential to the ED Advisory Group and MoH contributors until approved for web publication and effective but their effect on ED length of stay is unknown. to measure and some consider their cost-effectiveness is the major issue. However, the cost effectiveness of any part of the ED workforce is difficult to measure. There is a need to look at the best resource for the task in hand. The role of other health care Yes, but unless we say EDs are usually going to handle professionals in emergency low-medium acuity as well as high acuity patients, it is not care needs evaluation. clear what value other health professionals would add here. Despite the range of practitioners that have been tried in other countries (physician assistants etc) there is no clarity about the ideal ED workforce. The remainder of the literature review presents and comments on the findings from the literature searches, grouped under the eight headings listed above under “Method” on page 1. 1. Developing and adopting a national acute care strategy One approach is to have a whole of system strategy for addressing problems in acute care, and particularly those problems which manifest as ED overcrowding are repeatedly suggested by expert commentators as an important part of the solution. One suggested model describes three areas of contribution to ED overcrowding – preload (the number and complexity of patients seeking acute care); contractility (the ability of the system to accommodate these patients, including the physical and human resources and the processes for getting things done); and afterload (the ease of getting the patient to the next phase of care, most notably into a hospital bed) (Ardagh M, 2006). “Focusing on a single solution (for example, efforts to reduce low acuity patient presentations, or opening more hospital beds), independent of other contributing factors, will frustrate those attempting to fix the problem. So will attempts to fix the problem of ED overcrowding by focusing on the ED only, when two of the three contributing areas (preload and afterload) are outside the ED’s influence. Therefore, from this model, two principles fall: 1. The causes and solutions are multi-factorial and should be considered together. 2. Two of the three areas of contribution are outside the authority of the ED, so solutions need to be driven at a DHB level. Four further principles are: 3. Unnecessary steps in the patient journey should be identified and eliminated. 4. The narrowest bottlenecks in the patient journey should be fixed first. 5. Important tasks in the patient journey (value added tasks) need an appropriately staffed and resourced place dedicated to undertaking that task efficiently and effectively. 6. When the patient has completed that task, he or she moves to the next place, for the next task” (Ardagh M, 2006). There is an opportunity to apply clinically appropriate incentives to manage acute demand across the patient care continuum. The focus of incentives should be on driving the right behaviours that target patients (Acute Demand Management Working Party, 2007). An example of an appropriate incentive to reduce ED 9 18 August 2009 Confidential to the ED Advisory Group and MoH contributors until approved for web publication overcrowding is supporting after hours services11 in line with DHB acute demand management approaches in the primary health care setting (Ministry of Health, 2008). There is a section on approaches to managing acute demand on pages17– 21 below. 2. Using master plans within hospitals To address whole-of-hospital issues that have the potential to impact on ED overcrowding, it is useful to look at a range of overarching hospital plans. 11 Beginning in the finanical year to 30 June 2009, the Government made $9M available per annum to those DHBs that submitted acceptable proposals for improved after hours service coverage. 10 18 August 2009 Confidential to the ED Advisory Group and MoH contributors until approved for web publication 1. Using a set of basic principles and / or a combination of approaches. One example of principles for effective emergency care services was developed in the UK and built on best practice in ED management: (a) all services must be designed from the point of view of the patient (b) patients should receive a consistent response, regardless of where, when and how they contact the services (c) patients’ needs should be met by the professional who is best able to deliver the service they need (d) information obtained at each stage in the patient’s journey should be available to other professionals the patient may be referred to (subject always to the patient giving their agreement and to the introduction of appropriate safeguards to preserve confidentiality) (e) assessment and treatment should not be delayed through the absence of diagnostic or specialist advice (f) emergency care should be delivered in ways which are clear, consistent, and measurable (g) standards which cover each element of the service and the whole of the patient’s journey (Cooke MW Higgins J and Kidd P, 2003). Two other studies point to the need for a combination of approaches to ED overcrowding. In a Melbourne study of 17 participating public hospital EDs, 15 strategies to reduce over-crowding were introduced to the EDs including care co-ordination teams, short stay units, psychiatric services, chest pain units, pharmacy services, sexual assault service and hospital in the home. Facilitative initiatives included nurse initiated management, fast track processes, multidisciplinary triage, disposition nurses/communication clerks and day treatment clinics. Many traditional inpatient services were incorporated into the EDs which now provide a different and expanded paradigm of care (Taylor D McD, Bennett DM, Cameron PA, 2004). In Memphis, Boston and Atlanta, the three cities with hospitals that form the Learning Network, a comprehensive list of policies and operational imperatives was developed when the National Association of Public Hospitals and Health Systems commissioned a report based on the findings of the Urgent Matters Learning Network. That list includes the overarching themes that drove success in each of the Learning Network hospital’s change efforts: (a) Hospitals must recognise that ED crowding is a hospital-wide problem, not an ED problem (b) Multi-disciplinary, hospital-wide teams are essential to overseeing and implementing change (c) A “champion” for change must be identified or cultivated in the institution (d) Senior leadership must send a clear and consistent message that improving patient flow is a priority (e) Hospitals must learn and use formal improvement methods, such as rapid cycle change12, on a daily basis – and track results Institutions 12 Rapid Cycle Change (RCC) is a quality improvement technique that allows hospital staff to initiate and test a large number of small changes related to patient flow very quickly by monitoring the effectiveness of those changes using small data samples. 11 18 August 2009 Confidential to the ED Advisory Group and MoH contributors until approved for web publication must commit themselves to using rigorous metrics, because ‘we can’t fix what we can’t measure’ (f) Transparency around initiatives and data must become an organisational value, so that all stakeholders have the information they need to do their jobs (Wilson MJ, Siegel B, Williams M, 2005). 2 Optimising the Patient's Journey In NZ, OPJ is specially aimed at improving the quality of care from the patient's perspective. It is a national collaborative programme for improving the quality of care, particularly in hospitals. The programme focuses on improving a patient's journey within the inpatient setting from before the patient's entry to hospital to discharge from that episode of care. The programme also focuses on the management of patients with chronic conditions who present at the hospital for treatment, and on the flow of patients from primary care through to the hospital. OPJ is also aimed at improving the efficiency of service provision. Early indications are that the programme is reducing the cost per patient episode. It is anticipated that efficiency should also improve if the number of cancelled operations can be reduced along with the number of admissions and the number of emergency department attendances for long term conditions13 (Health Policy Monitor, 2008). 3. Applying the principles of the Clockwork ED The US Healthcare Advisory Board undertook a seminal piece of work published in 1999 as “the Clockwork ED”, which is available only to member hospitals of the Council of International Hospitals and is subtitled “Best practices for maximising emergency department throughput and capacity (Hughes G, 2008). It led to the Advisory Board Company’s Clockwork ED initiative, to track 20 evidence-based best practices and this initiative was supported by the ED Log, a database for understanding ED utilisation. The ED log went live in 2002 and stores patient tracking information from EDs including a variety of length of stay measures, patients who left without being seen, admission rates and return rates. The data are used to identify opportunities and priorities and to track improvements (LSU Health Sciences Center). The following two examples illustrate how the Clockwork ED works in practice. (a) St Joseph’s Medical Center, Towson, Maryland A study of changes in St Joseph’s, a regional medical center, focused on patient input, throughput and output: 13 Each Collaborative will run for a defined period of time: 18 months for the phase 1 collaborative on Lean Thinking (June 2008 to March 2009), 24 months for the phase 2 collaborative on the management of long term conditions (February 2009 to March 2011), after which materials and learning from the project will be published. 12 18 August 2009 Confidential to the ED Advisory Group and MoH contributors until approved for web publication Input changes Throughput changes Output changes Revamping the triage and admission processes with a simple yet effective means of flagging diagnostic results. Charts for new patients to be seen were placed upright, while charts ready for disposition were turned on their sides in the physicians’ rack. Modifying the physical layout of the urgent care area to maximise efficiency in staff movement and communications. Identifying causes of delays in discharges and admissions. Changing staffing patterns to match anticipated patient volume. Instituting the practice of flagging the charts of patients ready for discharge. Revising policies regarding exchanges with radiology staff. Implementing admission orders to decrease patient waiting times. The changes were implemented at first in urgent care and then in the main ED which was split into three zones, instead of one, each having nine beds with additional nurses’ stations in the two new zones. This removed the flow problems which had resulted in physicians having patients scattered all over the department, nurses constantly walking back and forth between the order rack and the rooms farthest from the nurses’ station, and doctors and nurses constantly looking for each other during the shift. Key results were that patients began to be placed in treatment beds minutes after arrival, are seen promptly and the ED is no longer overcrowded. In August 2004, door-to-provider intervals and length of stay dropped. The performance levels of part-timers compared with full time staff was reviewed and part-timers were given the opportunity to improve their performance. The support of senior management was found to be essential to the turn-around. The stage was set for eliminating the “silo mentality” and fostering interdepartmental cooperation. Significant untapped hospital and staffing capacity was found by streamlining processes and changing mindsets. The researchers believe that process improvement can be a valuable tool in alleviating, if not eliminating, ED overcrowding (Twanmoh JR, Cunningham GP, 2006) (b) Children’s Hospital Medical Center of Akron, in Akron Ohio With internal process improvement expertise and affiliation with a healthcare consulting group, the ED leadership at the Children’s Hospital Medical Center of Akron, in Akron Ohio identified opportunities to implement best practice initiatives with the 13 18 August 2009 Confidential to the ED Advisory Group and MoH contributors until approved for web publication overarching goal to improve patient throughput. A working group involved several ancillary departments in the hospital and conducted weekly meetings over a six month planning phase. Researchers wrote up the initiatives in a poster for the NACHRI & N.A.C.H14 Creating Connections Conference, to illustrate the impact of the doorto-doctor time interval. The first initiative which they describe is called “toggelled rapid triage”, discriminates when ED capacity allows for rapid triage practice at the patient entry-point. The toggling process featured: (i) Traffic stoplights in the ED waiting room and main work station inform patients and staff of ED capacity. (ii) A green light when there is room to take patients immediately to an exam room, while a red light indicates that the ED is at capacity and a wait to see a doctor might be expected. (iii) Comprehensive triage, which was performed in the patient's room instead of the ED entry point during "green light." (iv) Pre-emptive testing, which was utilised when the ED was at capacity. The second initiative, “bedside registration”, decreases door-to-doctor time by placing the patient registration process in parallel with other ED visit-related activities instead of in series. Toggled rapid triage and bedside registration practices had been in place for one month at the time of this poster submission. When compared to the same time one year ago, there has been a 25 percent (34 to 22 minutes) decrease in door-to-doctor time interval and a 12 percent decrease in overall length of stay (112 to 99 minutes). At the time of presenting the results in this poster, the researchers expected to have more comparison measures such as more complete throughput data, patient satisfaction measures and incidence of patients who left before evaluation (Lee T, Johnson N, 2009). 3. Concentrating on ‘primary care’ presentations to the ED While EDs will often see patients with primary care problems, particularly after hours, the evidence for having primary care practitioners in the ED, or for redirecting patients to a primary care facility, is poor. Despite perceptions that EDs see a large number of primary care patients, numbers of primary care presentations at EDs were found to be surprisingly small. Only three percent of primary care patients attended an ED in preference to visiting their GP (Eagar K, 2005). It has been proven that general practice (GP) patients do not cause access block or ED overcrowding and persistence of this belief is detrimental to finding real solutions (Sprivulus PC, 2004). This important view is based on studies showing that while a proportion of patients attending EDs could have been seen in primary care, these patients typically present with low complexity. Removal of the 20 percent of patients with lowest complexity in an ED may only reduce the workload on the department by 3.5 percent – removing such patients would therefore have a marginal impact (Stone K, 2008). The 14 National Associations of Children’s Hospitals and Related Institutions and National Association of Children’s Hospitals 14 18 August 2009 Confidential to the ED Advisory Group and MoH contributors until approved for web publication perception that GP or primary care appropriate patients are a relatively unimportant contributor to ED problems is shared by many, though not all, clinical leaders in NZ EDs (Working Group, 2008). A study that took place in New South Wales between 1999 and 2006 examined trends in potential 'primary care' presentations at EDs, comparing these with other ED presentations and to primary care attendances in the community. Primary care presentations at EDs increased marginally in the period under consideration, as did primary care presentations in the community. There was a substantial increase in other ED presentations. The proportion of ED presentations that were potentially for primary care decreased over the period, possibly because of new guidelines for the application of triage categories in 2001. However, trends over time do not show acute alterations and they continue to hold for the subsequent period after the introduction of the new guidelines. The researchers concluded that primary care presentations at EDs are not responsible for recent changes to ED overcrowding in New South Wales (Siminski P, Bezzina A, et al, 2008). Diversion of low acuity (i.e. GP) presentations and use of telephone services to decrease ED presentations were found not to work for reducing access block and ED overcrowding (Forero R. and Hillman K, 2008). Also, researchers have suggested increasing co-located after hours GP services to reduce ED presentations, but these have been unsuccessful in Australia (Forero R. and Hillman K, 2008). A ‘diversion strategy’ was proposed by a group of researchers at Wollongong University for situations where there might be a goal to divert primary care attendances from EDs to GPs. The researchers found that “multi-faceted service at ED” is a far more important reason for ED attendance by primary care patients than “GP unavailability”. Accordingly their solution was to promote practices with convenient multi-faceted services, for patients to view as a one-stop-shop, but the benefits of such a service seem questionable and the costs high, given the small percentage of primary care patients found to be attending an ED rather than a GP (Eager K, 2005). Some hospitals have used systems where, after initial triage, primary care appropriate problems are referred to GPs or community primary care rather than being dealt with at an ED (Murphy AW, Bury G, Plunkett PK, 1996), (Pereira S, Oliveira E, et al, 2001), (De Silva, 2009). One NZ evaluation of a process that referred patients back to the community found that of those patients that they could follow up (only 37 percent), 60 percent did not seek community medical care although most cases improved (Elley, CR, Randall P-J, et al, 2007). Similar results were found in a Los Angeles study of 156 patients who used the ED on weekdays from 7:00am to 3:00pm and who met the criteria for deferred care. The researchers found that clinically detailed standardised screening criteria can safely identify patients at public hospital EDs for referral to next-day care. “Patients assigned to next day care did not demonstrate clinically important disadvantages in health status or physician visits compared with usual care patients.” The researchers note that larger studies are needed to assess the possibility of adverse effects (Washington DL, Stevens CD, et al, 2002). There is no clear consensus between professionals regarding the concept of ‘appropriateness’ of ED attendances which has implications for any interventions aimed at addressing ED overcrowding (Richardson S, Ardagh M, Hider P, 2006). 15 18 August 2009 Confidential to the ED Advisory Group and MoH contributors until approved for web publication If expert panels show poor agreement in deciding which cases could be handled in primary care, when the case is assessed retrospectively with diagnosis and outcomes known, how are we to expect patients or even triage nurses to do better? (Elley, CR, Randall P-J, et al, 2007). Redirecting them is seen as risky, especially if serious cases such as meningitis could be missed. Redirecting is also time-consuming, and not always in the patients’ best interest (Elley CR. Randall PJ, et al, 2007). “A common and unfortunate response to a perceived excess of preload has been to deny or obstruct care to those considered inappropriate for presentation at the ED. The assessment of ‘appropriateness’ at triage has consistently been shown to be inaccurate and, in addition to potentially contravening rights of access to care, triaging patients out of the ED is dangerous and does not reduce costs. Lowering barriers to more appropriate care is a better solution than raising barriers to perceived inappropriate care” (Ardagh M and Richardson S, 2004). A prospective study in Portugal found lower rates of ‘inappropriate’ ED use, although one criterion for ED appropriateness was that a patient would need to have a diagnostic test performed, which differs from criteria used in a Portuguese University Hospital study, where many tests could be performed from primary care (Pereira S, Oliveira E, Silva A, et al, 2001). This again raises the issue of whether ‘primary care appropriate’ and ‘ED appropriate’ are mutually exclusive or whether there is substantial overlap, particularly in the case of minor trauma. Clearly, more prospective audits are needed (Elley CR, Randall P-J, et al, 2007). A number of approaches to primary care presentations to ED have been described in the literature and some of these are summarised below. 1. There is some research giving limited support to the idea that individual general practitioners can manage primary care patients and less serious emergencies effectively and with lower flow-on costs than junior ED staff (Murphy AW, Bury G, et al, 1996). However, co-locating primary care facilities within EDs was proposed for Dunedin in 2005 but was found to be based on a “naïve and simplistic” premise, namely attributing overcrowding in ED to “excessive numbers of GP type attendees” (Wilson H, 2005). The proposal does not address how patients are processed within the ED or how they are transferred to wards later if required (‘access block’). This article also discusses some other unresolved issues including the GP co-operative continuing to carry the financial risk for the new (private) service within ED. “As some patients who currently attend ED because of zero cost will now be seen by GPs and charged for their consultations (…and may be unable to pay….), it could be argued that the local DHB is simply shifting the burden of providing ‘free’ health care to a private facility. The patient, who is at the centre of these changes, is now caught between two....organisations keen to reduce their financial risk. Furthermore, commercial viability of the new facility could be compromised if a new private Accident and Medical clinical sets up at the old site, as has been mooted” (Wilson H, 2005). 2. Some argue that although EDs undoubtedly see a proportion of patients who could have been managed in primary care, it may be better for the patient that they present to an ED. For instance, it may be to the disadvantage of the patient with long term condition(s) to be managed without continuity of care, but for those cases which could be managed in either setting there may be 16 18 August 2009 Confidential to the ED Advisory Group and MoH contributors until approved for web publication little cost benefit to transfer care as the cases are at the lower cost end of the ED casemix (Elley, CR, Randall P-J, et al, 2007). 3. There are approaches to reducing ED overcrowding in the context of long term conditions management, including: (a) the Year-Plan Model in which community based bundles of support are provided for people with long term conditions, or with risk factors for developing long term conditions. The model is based on three populations: Level 1: those at risk of developing a long term condition, Level 2: those who already have a long term condition and Level 3: those with complex co-morbidities. Services are planned according to each of the three population groups. These include for Level 1, Expert Patient Programmes, smoking cessation programmes and yoga; for Level 2, practice nursing, general practitioner, and outreach services; and for Level 3, home help, district nursing and social services (Degeling P, Close H and Degeling D, 2006). Strategies to improve services provided in primary care settings are being implemented to reduce emergency bed days by 5 percent in England (DoH, 2005). The strategies are based on evidence that redesigning existing modes of service delivery to people with long term conditions, concentrating efforts in primary care, will improve the prognosis and day to day lives of people (WHO, 2004) and reduce “the impost of present failures in primary care service provision on the acute care sector” (Degeling P, Close H and Degeling D, 2006). (b) comprehensive disease management programmes designed to reduce ASH15. 51 out of 146 NZ studies evaluated the role of such programmes and out of the 51 studies, 29 (57%) found significant reductions in ASH. Twenty of the 29 studies (69%) found that well-coordinated, multidisciplinary care programmes were effective in reducing hospitalisation or re-hospitalisation for elderly patients recovering from chronic heart failure. The researchers commented that “Comprehensive, multidisciplinary, team-based medical care programmes where patients were involved in discharge planning, were provided education in either a one-on-one setting or using interactive discussions, and were regularly followed up, were likely to be beneficial compared to programmes that included only one or none of these components” (Health Services Assessment Collaboration, 2008). 4. Providing low cost or free general practice services. Capital and Coast DHB reports that the Te Aro clinic has done this for more than a decade, using their strong links into the homeless community and to other people living in the inner city struggling with poverty, addiction, mental illness, and perhaps cultural and language barriers. In 2004/05, in response to increasing demand on unfunded outreach provided by Te Aro clinic staff, specific funding was provided for a mobile primary care service to homeless people and those in very transient living situations such as shelters and boarding houses. An evaluation of the programme documents the effect on ED use and hospital admissions for a cohort of patients who have utilised this service and continue to do so. 15 The review only considers one outcome: hospitalisation or not. Studies included in the review reported multiple outcomes including reductions in unscheduled ED visits and ED Length of Stay 17 18 August 2009 Confidential to the ED Advisory Group and MoH contributors until approved for web publication Key findings were that: (a) ASH rates are low compared with other areas of NZ and continue to decrease (b) ED use has decreased for people who enrol with a PHO which suggests that continuity and care and proactive care are being provided by general practices, which is the ideal situation. However, the situation is not ideal, because in parallel with that decrease, utilisation at the Kenepuru A&M clinic has increased, with the highest A&M attendance rates being among children and high deprivation groups. This suggests that the A&M clinic is being used for more than the backup services for which it is intended. Capital and Coast DHB comment that this pattern is not surprising given the high levels of unmet need in the Porirua group most likely to use the A&M. The unmet need exists because of limited primary care capacity, despite additional investment. (Capital and Coast DHB, 2009). 4. Managing acute demand Much of the acute demand literature focuses on ED use by older people and on alcohol in injury-related presentations to EDs. 1. Older people Older adult (65+ years) hospital admissions (frequency and rate) and ED presentations (frequency) increased significantly over the 12-year period 1996 – 2007. Frequency of admissions increased by 83 percent, admission rate by 46 percent if same day admissions are included in the analysis, reducing to 50 percent and 27 percent if they are excluded, while frequency of ED admissions increased by 111 percent (Monash University Accident Research Centre Victorian Injury Surveillance Unit, 2009). Falls account for 77 percent of hospital admissions and 54 percent of ED presentations in this age group16. Complex patients are twice as likely to have unplanned hospital admissions via the ED. In a New South Wales study, 526 (239 men and 287 women) people aged 55 years and over were interviewed. Musculoskeletal disorders, hypertension, gastrointestinal disorders and ischaemic heart disease were the most frequently reported of the chronic illnesses surveyed. A total number of 70 people from the survey group with a total of 115 admissions through emergency departments were recorded. The researchers concluded that there was significant association between multiple chronic diseases and emergency admissions for older people. Of these, hypertension and ischaemic heart disease were found to be significant predictors. Age per se was found to be of borderline significance (Chan DKY, Chong R, et al, 2002). Older patients more frequently present to the ED than younger patients and are more frequently admitted to hospital. At presentation, there is often a history of short-term decline in health. This raises the theoretical possibility 16 Elderly patients with hip fractures were the subject of a New York study where the researchers found that this group was at risk for underassessment of pain, considerable delays in analgesic administration after pain is identified, and treatment with inappropriate analgesics in the ED. The more overcrowded an ED, the poorer the pain management (Hwang U, Richardson LD, et al, 2006). 18 18 August 2009 Confidential to the ED Advisory Group and MoH contributors until approved for web publication that, if there could be some intervention after older patients start to decline but before they reach the stage at which they require admission, it might be possible to improve their health enough to avoid admission to hospital. A New South Wales prospective, randomised, controlled trial with 18 months of follow-up study designed to assess the effects of comprehensive geriatric assessment (CGA) and multidisciplinary intervention on elderly patients sent home from the ED found that multidisciplinary intervention improved health outcomes of older people at risk of deteriorating health and reduce unplanned admissions to hospital. The researchers studied the discharge of the elderly from the ED (DEED) because patients aged 75 and older who are discharged from the ED have a greater risk of being admitted to the hospital over the following two weeks or month and are at increased risk of death. The researchers suggest that patients aged 75 and older should be referred for CGA after an ED visit (Caplan GA, Williams AJ, et al, 2004). A nursing discharge planning risk assessment tool applied to 2139 elderly patients in Queensland, men and women over 70 years of age, reduced the risk of re-presentation with the same condition by 16 percent and decreased the re-admission rate by 6 percent. Overall length of stay in hospital was reduced from 6.1 to 5.4 days. An unexpected finding was the decrease in representations in frequent flyers, those who re-presented to the emergency department three or more times per month. The study aimed to ascertain whether a model of risk screening carried out by an experienced community nurse was effective in decreasing re-presentations and re-admissions and the length of stay of older people presenting to the ED. It was apparent to the researchers that older people presenting to the emergency department have complex care needs. The researchers found that undertaking risk screening using an experienced community nurse to ascertain the correct level of community assistance required and ensuring speedy referral to appropriate community services has positive outcomes for both the hospital and the patient. They suggest that the decrease in re-presentations was the result of increased referral and use of community services. It appeared that the use of a specialist community nurse to undertake risk screening rather than the triage nurse may impact positively on service utilisation (Hegney D, Buikistra E, et al, 2006). In the UK, paramedics with extended skills were found to provide a clinically effective alternative to standard ambulance transfer and treatment in an emergency department for elderly patients with acute minor conditions such as those resulting from falls (Mason S and Knowles E, et al, 2007, Mason S, O’Keeffe C, et al, 2007, Gray JT and Walker A, 2008). These findings underpin the Urgent Community Care pilot being conducted with funding from ACC and Capital and Coast DHB17. 17 For this to be effective in NZ, ambulance paramedics will in future need to be registered health care professionals, so that they can see and treat or treat and refer to PHC professionals and leave in the community – and not worry about not being paid. At present, ambulance paramedics are funded to see and transport. They can only see and treat if they are recognised as being health care professionals (conversation with Andy Long, Manager, Kapiti Urgent Community Care Pilot, July 2009). 19 18 August 2009 Confidential to the ED Advisory Group and MoH contributors until approved for web publication 2. Alcohol in injury-related presentations to ED An international study, the first international attempt to quantify the role of alcohol in injured persons from several different countries using the same methodology based on ED data, suggests that 10-18 percent of injured patients attending EDs are alcohol-related cases (WHO, 2007). NZ, based on an Auckland site, reported the second highest proportion of alcohol-related injury presenting to an ED, which was 36 percent (Richards G, 2008). More data gathering and analysis has been called for in international studies of alcohol-related injury. For example, alcohol-related ED visits studied at a national level using data from the USA’s National Hospital Ambulatory Medical Care Survey for 1992 through 2000 were found to be approximately three times higher than previous estimates. The study found that alcoholrelated diseases and injuries pose a significant burden on hospital EDs. Because patients often fail to disclose their drinking habits to physicians, and ED physicians sometimes fail to identify signs of alcohol abuse, the number of alcohol-related ED visits may have been underestimated (McDonald AJ III; Wang N, Camargo CA Jr, 2004). In the absence of more conclusive evidence, the researchers used 37 diagnoses that could be alcohol-related to estimate the total number of alcohol-related ED visits from 1992 through 2000. Patients aged 30 to 49 had twice the rate of ED visits with diagnoses that were considered to be completely attributable to alcohol than patients aged 15 through 29, or 50 and older. The visit rate for males with diagnoses 100 percent attributable to alcohol was three times higher than for females, and the visit rate for blacks with such diagnoses was approximately two times that for whites. "Although U.S. public health officials recognize that EDs throughout the United States face an enormous burden from alcohol-related diseases and injuries, this study shows that the current literature significantly underestimates the magnitude of this burden," write the authors. "Our nineyear study also reveals a rising trend in the number and rate of alcoholrelated ED visits and a widening gap between sexes and a shrinking gap between races among those seen in the ED with certain alcohol-related diagnoses." The researchers conclude that "… improving the frequency of ED screening may lead to more appropriate referrals and interventions during alcohol-related ED visits, with a reduction in subsequent illness and additional visits to the ED" (McDonald AJ III; Wang N, Camargo CA Jr, 2004). Literature relating to the burden of alcohol-related injury in NZ is described in a brief guide (Richards G, 2008) but the impact of alcohol-related injury on ED presentations is only covered in only two of the studies to which Richards refers (Humphrey G, Casswell S, Han DY, 2003) and Connor J, Broad J, Jackson R, 2005). One of the studies took place during December 2000 using a random sample of patients who were interviewed and breath tested in the ED continuously for a three-week period (Humphrey G, Casswell S, Han DY, 2003). This study reports that: 20 18 August 2009 Confidential to the ED Advisory Group and MoH contributors until approved for web publication (a) there is comparatively little research in NZ that examines the role of alcohol in injury occurrence, and none that clearly documents the level of alcohol’s involvement. They refer to a study of NZ rugby injury, which found 14 percent of males and 8 percent of females participating reported that injuries they sustained in the previous 12 months were the result of their drinking (Quarrie K, Feehan M, et al, 1996). That 1996 study also found that heavier drinking was the norm, with 61 percent of males and 38 percent of females consuming six drinks or more in one session at least weekly. (b) there had been an earlier study that used the New Zealand Health Information Service database to examine the incidence of death and hospitalisation from assault occurring in and around licensed premises (Langley J, Chalmers D, Fanslow J, 1996). In this 1996 study, in spite of some recording inconsistencies, the researchers found that when place of assault was recorded, 10 percent of these assaults took place in or around licensed premises, 17 percent involved people under 20 years of age, and males were over-represented in all assault figures. Alcohol-related injury patients were more likely to report heavy typical consumption patterns, to have experienced prior alcohol-related injury, and were unlikely to use health care services other than the ED. The other comprehensive NZ research into this topic was conducted in 2005 (Connor J, Broad J, et al, 2005 and 2005a). The key findings from this research were that “Injury was a major contributor to alcohol-related mortality, being responsible for 51 percent of deaths (532) and 72 percent of years of life lost (12,434 YLLs) Most alcohol-related deaths before middle age were due to injury.” Cancers and other chronic diseases contributed to the remaining alcohol-related mortality. Not enough is known about the numbers of ED presentations due to alcohol in NZ. If data were gathered consistently across time and place, the likely impact of alcohol-related presentations on ED overcrowding at certain times of the year18 and in certain parts of the country could be described and analysed – and solutions developed. Most potential sources of data on alcohol-related harm are subject to extraneous influences, which vary over time and space. A NZ study used the five solutions19 for deriving indicators which were developed by the World Health Organisation in their International Guide for Monitoring Alcohol Consumption and Related Harm (MACRH). The researchers found that MACRH needs to be revised to include criteria for a valid outcome indicator (Langley J, Kypri K et al, 2008). 18 An anecdotal report from Waikato Hospital describes such surges. In early 2009, Waikato Hospital reported its busiest day ever with almost 191 patients assessed and treated in a 24-hour period illustrated by a surge of alcohol-related injuries. There were no major trauma cases so ED clinical nurse manager Jenni Yeates put the busy day down to an increased number of people in the city. “It was a huge day for us. We had an increased number of young people and alcohol related injuries which is probably all the events happening in the city with Waikato University’s O-week” (Waikato DHB, 2009). 19 (i) use only alcohol-specific cases (ii) identify subsets of events known to be highly alcohol-related, (iii) utilise control indicators that are rarely alcohol-related, (iv) estimate alcohol attributable fractions and (v) develop composite indicators. 21 18 August 2009 Confidential to the ED Advisory Group and MoH contributors until approved for web publication The Alcohol Advisory Council would like to see emergency departments routinely recording the number of patients presenting with alcohol-related injuries to help show the size of the problem. Chief Executive Gerard Vaughan was quoted in the Otago Daily Times as saying that such figures could then be used to see how effective any changes to the availability of alcohol were. He was commenting on a report in the Otago Daily Times (on 27 April 2009) in which Dunedin Hospital ED consultant Dr John Chambers linked extended opening hours to an increase in the number of people attending the department with injuries following alcohol consumption. Mr Vaughan said if figures were kept, they could be made available to general practitioners, who could then be advised when one of their patients was involved with an alcohol-related injury or accident. "There would then be the opportunity for the GP to administer a brief intervention by questioning their patient about their alcohol consumption." There were ways of recording the information in such a way that the level of intoxication was indicated. Mr Vaughan said the Council was one of many bodies wanting better information and data collection relating to alcohol use (Otago Daily Times, 28 April 2009). 5. Hospital capacity planning / managing access block Evidence that more hospital beds, or better hospital bed management, improves ED overcrowding is not strong in the literature. However, intuitively and based on perceptions in relation to efforts in this regard, it is reasonable to conclude that hospital capacity planning is an important part of the solution. Will hospital capacity planning reduce ED length of stay? There is no conclusive answer to this because relatively little research has examined the correlation between hospital bed occupancy and length of stay in the ED. One study found that “modest decreases in hospital occupancy resulted in highly significant reductions in ED waiting times…..and….emergency department overcrowding due to large numbers of admitted patients awaiting hospital admission is a major cause of ED dysfunction.” (Dunn R, 2003, quoted in Ali W, 2006). In a descriptive review of acute hospital bed occupancy and length of stay for patients in the ED, the total time spent in the ED was found to relate to the immediate availability of an inpatient bed (Ali W, 2006). It is important to note that in that review, no studies were included that evaluated the effectiveness of interventions to manage hospital bed occupancy and the impact on the associated time spent in the ED. ED overcrowding is associated with inability to access hospital inpatient beds (access block). As noted on page 2 above, access block is a term used to describe the delay experienced by ED patients who need hospital admission when their inpatient bed is unavailable (Forero R, Hillman K, 2008). There is strong evidence for access block as a cause of overcrowding (Ardagh M, Richardson S, 2004), (Bradley VM, 2005), (Estey A, Ness K, Saunders D, 2003), (Proudlove NC, Gordon K, and Boaden R, 2003). Further, the significance of access block as a cause of overcrowding has been illustrated in a number of studies that found that the time interval between the order of admission for a patient and the time when the patient is actually transferred to the assigned bed appears to be most affected by the immediate availability of the bed rather than by other causes (Bagust A, Place M, Posnett JW, 1999), (Kyriacou DN, Ricketts V, et al, 1999), (Cooke MW, 2003), (Dunn R, 2003), (Forster AL, Stiell I, et al, 2003), (Gorelick MH, Yen K, Yun HJ, 2005). 22 18 August 2009 Confidential to the ED Advisory Group and MoH contributors until approved for web publication Prolonged ED length of stay, exceeding 8 hours, has been studied and attributed to an increase in the frequency of access block at many hospitals (Cooke MW, Wilson S, et al, 2004), (Ali, 2006). Access block has been correlated with total hospital inpatient bed occupancy of 90 percent or greater and a target occupancy of 85 percent has been suggested as an ideal level in order to balance between the possibilities of either unused bed capacity or inefficient inpatient flow (Sprivulis PC, Da Silva J-A, et al, 2006). According to a number of commentators, high inpatient occupancy levels lead to an inefficient patient flow in the hospital, which with other factors can then lead to overcrowding in the ED (Emergency Nurses Association, 2006). In Australia “there is clear evidence that the main cause of access block and ED overcrowding is a combination of major increases in emergency admissions and ED presentations with almost no increase in the capacity of hospitals to cope with the demand. Between 2002 and 2007 the rate of available beds in Australia was reduced from 2.65 beds (1998 – 99 level) per 1000 population to 2.4 in 2002, and has since remained steady between 2.5-2.6 per 1000 population. In the same period the number of ED presentations has increased over 38 percent from 4.1m to 6.7m, (from 3.5m in 2006-07)” (Forero R. and Hillman K, 2008). Only a small part of the solution to access block resides within EDs (Forero R. and Hillman K, 2008), (Richardson DB and Mountain D, 2009). There is no similar NZ study of the rate per 1000 of available acute beds but it would be useful to establish that rate, for comparison with other countries. Access block is likely to be best addressed by increasing the capacity of the system, most directly by increasing the number of beds available at all levels of care within hospitals. Hospitals must recognise that ED crowding is a hospital-wide problem, not an ED problem (Wilson MJ, Siegel B, Williams, 2005). This means 1. having more inpatient beds by optimising patient flow to increase bed availability and 2. using different approaches to increasing the effectiveness of ED staffing. The prevalence of ED overcrowding may rise in developed economies as age-related demand for hospital services grows over the coming 10 to 15 years. Additionally, economic incentives tend to favour higher, rather than lower, occupancy. It may be necessary to realign the incentives that favor high occupancy at the expense of emergency access (Sprivulis P, Da Silva J-A, et al, 2006). One approach to optimising patient flow is streaming. Researchers at the Flinders Medical Centre, a 500-bed teaching general hospital in Adelaide, designed a study to illustrate in some detail the methods used in, and outcome of, applying Lean Thinking in establishing streams for patient flows20 (King DL, Ben-Tovim DI, Bassham J, 2006). They gained an understanding of the impact of Lean Thinking through process mapping with staff, followed by the identification of value streams (those patients likely to be discharged from the ED, those who were likely to be admitted) 20 Pioneered in the automotive manufacturing industry by Toyota, the Lean process is a management philosophy aimed at eliminating waste and improving overall customer value (Womack JP, Jones DT, Roos D, 1991). “Being “Lean” is about understanding value from the customer's perspective and delivering exactly what is required at the right time with minimum effort and no waste in a safe environment” (Kulkarni RG, 2007). 23 18 August 2009 Confidential to the ED Advisory Group and MoH contributors until approved for web publication and the implementation of a process of seeing those patients that minimised complex queuing in the ED. The researchers found that streaming had a significant impact on waiting times and total durations of stay in the ED. There was a general flattening of the waiting time across all groups. A slight increase in wait for Triage categories 2 and 3 patients was offset by reductions in wait for Triage category 4 patients. All groups of patients spent significantly less overall time in the department and the average number of patients in the ED at any time decreased. There was a significant reduction in number of patients who did not wait and a slight decrease in access block. The streaming of patients into groups of patients cared for by a specific team of doctors and nurses, and the minimising of complex queues in this ED by altering the practices in relation to the function of the Australasian Triage Scale improved patient flow, thereby decreasing potential for overcrowding (King DL, Ben-Tovim DI, Bassham J, 2006). In Central London, competition between patients with emergency needs and those with routine (elective) needs led to disruption of both services. This issue was addressed by increasingly separating elective and emergency workload into different ‘paths’ of work, each with dedicated resources in hospital and primary care settings. This required additional investment and an additional £40 million was allocated to support the implementation of nurse-led minor injuries and conditions services. The reforms encouraged a whole systems approach, involving NHS Direct, primary and social care, Ambulance Trusts, and secondary care in improving access and reducing waiting times in line with the targets outlined in the NHS plan. The streaming of services for patients with minor injuries and conditions was central to the reforms. (DoH, 2002) A key streaming study found that the introduction of a separate stream for minor injuries can produce an improvement in the number of trauma patients waiting over an hour by about 30%. If this is associated with an increase in consultant presence on the shop floor it may be possible to achieve a 50% improvement. Accordingly, it was recommended that departments use a separate stream for minor injuries to decrease the number of patients enduring long waits in A&E departments (Cooke MW, Wilson S and Pearson S, 2002). Another approach which is likely to be useful for increasing the effectiveness of ED staffing is to use queuing theory21, to estimate the number of providers needed during each staffing interval. Analytic models such as queuing models can never capture all characteristics of an actual operational setting. However, models can be invaluable in providing decision support greatly improving performance, particularly in complex environments. Queuing models are useful in EDs because they apply where resources are tight relative to demand and small changes in staffing can have a dramatic impact upon delays. One study examined the response of one ED measure of performance, left without being seen (LWBS), to a provider staffing reallocation based on queuing theory. A software package was used to document a single queue of arrivals assuming an unlimited waiting room and a constant rate. The daily pattern of peaks and valleys was quite consistent but the overall average volume across a week had greater variation, indicating that the policy of identical staffing levels for all days of the week needed to be revisited (Green LV, Soares J, et al, 2006). 21 Queuing theory is a widely studied topic within operations research and follow the work of A.K. Erlang and the NHS used lessons from Erlang theory in their training material (NHS Modernisation Agency, 2002). 24 18 August 2009 Confidential to the ED Advisory Group and MoH contributors until approved for web publication 6. 1. Developing the ED health workforce Focusing on the healthcare professional (HCP) / teamwork In Singapore, placing a senior emergency physician with the triage nurse reduced waiting times for walk-in cases. One third of attendances were treated and discharged quickly, allowing the ED and Patients Activity Score 1 / PACS 2 doctors to act more efficiently (Travers JP, Lee FCY, 2006). In this study, the HCP performed the same jobs: assessing, recording treating and discharging over one third of cases as soon as they came through the casualty department doors, did not require further intervention and did not need to wait to be seen in a consultation room. Limitations of the study are that not all hospitals would be able to use the team triage described here as they may have separate problems because of a different case-mix. Not all hospitals would be prepared to merge the roles of the triage doctor and nurse, to produce a ‘healthcare professional’ as a team. However, on a more positive note, the study found that “potential exists for a large number to be discharged within a few minutes of arrival if appropriate senior assessment skills are available at first contact, and this may require more senior assessment than is currently used” (Travers JP, Lee FCY, 2006). This observation could be applied in NZ where it was found that the rapid management of patients with problems that do not require prolonged assessment or decision making is beneficial not only to those patients but also to other patients sharing the same limited resources (Ardagh MW, Wells JE, et al, 2002). A transition team was created in Rochester New York, where ED overcrowding proved to be a complex problem deeply rooted in “issues of inpatient capacity, inadequacy of alternatives for hospitalisation, and hospital resource shortages” (Schneider S, Zvemer F, et al, 2001). Overcrowding was only alleviated after hospital administration and the local administration realised that system reform was necessary. Hospital administration created a short-stay observation unit and a transition team to expedite the care of patients being boarded in the ED. The local department of health developed effective early warning systems and contingency plans. These interventions had a great impact on ED overcrowding and ambulance diversion (Schneider S, Zvemer F, et al, 2001). To alleviate overcrowding and better ensure the safety of ED patients, communities struggling with ED overcrowding must tackle the crisis with a similar multi-disciplinary system wide approach (Trzeciak S and Rivers EP, 2003). St. Joseph Hospital of Orange implemented a new ED programme, the Rapid Assessment and Discharge in Triage (RADIT) programme, designed to reduce patient waiting time and, importantly for the study and for the patient group, to improve overall patient satisfaction. ED visitors presenting nonurgent problems were served by a roving RADIT team. The hospital established a goal of 90 minute average time in RADIT and sought to reduce overall time in ED. 25 18 August 2009 Confidential to the ED Advisory Group and MoH contributors until approved for web publication ED average length of stay with RADIT (N=35,065) versus (N=31,936) Group Prior to RADIT July – Oct 2005 Total outpatient or discharged home 2 hr 48 mins patients RADIT patients – Total ER patients oputpatient) (all inpatient and 3 hrs 07 mins period prior to RADIT With RADIT Dec 2005 – Mar 2006 2 hr 57 mins 1 hour 37 mins (97 mins) 3 hrs 18 mins After six months, results indicated that RADIT patients were discharged on average in 97 minutes. Also, a patient satisfaction survey indicated that about 96% of RADIT patients rated the quality of service received as either good or excellent. For this success, the researchers credit the CQI process, which had a goal of improving existing processes and outcomes, and sustaining the improved performance (Vega V and McGuire SJJ, 2007). 2. Innovative roles An Australian study (Victorian Department of Human Services, 2005) found that the main developments identified from the literature that were relevant to their project, which was in the area of work analysis in EDs, intensive care units and radiology departments, were (a) The emergence of a new health worker that could be classified as a paramedical officer (b) The importance of the use of supplementary health workers who provide health care services and perform procedures on predominantly low acuity patients (c) Developing the role of the nurse practitioner (see below) and (d) Creation of specialist units and/or use of staff trained in other than emergency care. New and developing roles were found to be taking over some of the medical staff tasks such as triage, ordering and reading x-rays, minor trauma, prescribing over-the-counter and prescription drugs – as a response to the realisation that many people present to the ED with associated or underlying non-medical conditions. A useful example of how one new role is changing EDs is that, in response to increasing numbers of people presenting to the ED with a mental illness, some hospitals in Australia have established ‘psychiatric sub-units’ in the ED and /or use ‘mental health nurse consultants’ in the ED (Joyce PR,2005). Other examples of innovative roles that impact on ED use are: (a) Expanded Scope Paramedics (ESPs) in rural locations where interactions between ambulance services and rural communities had an overall benefit for health care including emergency response capability (Stirling CM, O’Meara P, et al, 2007). (b) Emergency Care Practitioners (ECPs), considered by Sir George Alberti to be “one of the great innovations of the new NHS” (Skills for Health). Within the overarching framework provided by competency 26 18 August 2009 Confidential to the ED Advisory Group and MoH contributors until approved for web publication requirements, ECP roles can be deployed in a variety of ways to support local services. Examples included working in GP surgeries, conducting home and community visits, providing care in minor injury units and delivering after hours services. ECPs are also able to facilitate referral to other services, which improves the overall patient experience. Working in this way, an elderly patient suffering minor injuries from a fall can be assessed and treated in their own home with a follow-up referral made to the community nursing service (Skills for Health). Care provided by ECPs appears to reduce the need for subsequent referral to other emergency and unscheduled care services in a large proportion of cases (Mason S, O’Keeffe C, et al, 2007). ECPs help to prevent attendances and admissions by delivery of clinical care and assessment at point of access to health care beyond that traditionally provided by UK ambulance services (Gray JT and Walker A, 2008). The ECP role is considered to be likely to be incorporated into any urgent community care services that develop as a result of the Kapiti Urgent Community Care pilot22. 3. Exploring the more extensive use of ED nurses and ED nurse practitioners (NPs) In Australasia, triage is carried out by emergency nurses. It is recognised that because triage is so important to both the smooth running of an ED and the outcome of the patients, it should be carried out by staff who are both specifically trained and experienced (ACEM, 2000). The literature supports the practice of nurse-initiated x-rays at triage and nurses have been doing this in the UK, Canada and Australia for many years, with varying degrees of reduction in waiting times. Conventional triage processes often extend waiting times for lower acuity patients unless secondary triage takes place. Secondary triage includes nurse-initiation of xrays, investigations and administration of intravenous fluids. Conventional triage with its ‘one portal’ system is disadvantaging many patients, particularly those with minor conditions. Improved patient flow after triage may alleviate this problem (Rudd J, 2005). In a systematic review of the literature from Australia, the US, the UK, Scotland and Canada the impact of NPs on cost, quality of care, satisfaction and wait times in the ED it was found that although some questions remain, NPs can reduce wait times for the ED, lead to high patient satisfaction and provide a quality of care equal to that of a mid-grade resident23. Cost, when compared with resident physicians is higher; however data that compares NPs with hiring additional medical professionals (e.g. more residents, another attending physician or a physician/s assistant) is lacking (Carter AJE and Chochinov AH, 2007). In a UK “see and treat” model using NPs, the average wait time to see a practitioner dropped from 56 to 30 minutes, the average time in the department decreased from I hour and 39 Minutes to 1 hour and17 minutes, 22 Conversation with Andy Long, Manager, Kapiti Urgent Community Care Pilot, July 2009 It needs to be noted that the role of Nurse Practitioner varies from country to country so the different NP studies will sometimes be relevant in NZ and sometimes not. The NZ NP is modelled on the USA NP, rather than on the UK one. There is wide variation in the role across the UK and sometimes within different UK departments as well. 23 27 18 August 2009 Confidential to the ED Advisory Group and MoH contributors until approved for web publication and the wait time for all patients in the department was lower after the introduction of this model (Rogers T, Ross N, Spooner D, 2004). Most studies examined NPs in minor treatment areas; however two studies suggested that NPs could also reduce wait times by seeing higher acuity patients (Blunt E, 1998), (Tachakra S and Stinson A, 2000). In a study in Victoria, Australia, researchers found that NPs appeared from the overseas examples to offer the opportunity for provision of ED services with limited supervision required from medical staff. The range of tasks performed by NPs included minor procedures, ordering investigations, prescribing, admitting and discharging – all within established clinical practice guidelines. They supported the establishment of ED Nurse Practitioners in Victoria, a model in its infancy in Victoria in 2005, because, providing they could discharge patients, they would reduce: the workload of doctors waiting time in EDs (Victorian Department of Human Services, 2005). 7. Using other wards and units as an alternative to the ED A variety of models of care, with different referral processes and hospital configurations, result in different parts of hospitals being used in emergencies. The area of GP referrals direct to inpatient teams, which is widespread across NZ 24, is an area in which NZ is set apart from Australia where the vast majority of referrals from GPs are to ED staff. The models of care include: (a) Auckland Hospital’s Emergency Care Centre with its Acute Assessment Unit co-located within its ED (b) Hawkes Bay DHB’s model in which all comers are seen, including GP referrals for admission (c) Use of very senior inpatient staff to field admission request calls from the GP/ED. For example, Nelson Marlborough DHB has a referral pathway for medical admissions from the ED which goes direct to the medical specialist, which anecdotally appears to be an important determinant of reducing the length of stay in the ED for that referred group of patients. While there is uncertainty about the most efficient model of emergency care (Australian Health Workforce Advisory Committee, 2006), several different models are reported in the literature. 1. Integrated model An attempt was made to improve the process of emergency care in a hospital in Cambridge UK by developing an integrated model in which a clinical decision unit replaced the more traditional observation unit. In this model, the medical admissions unit was relocated onto the existing ED and came under the four-hour target. Medical case records were redesigned to provide a common assessment document for all patients presenting as an emergency. Medical, surgical and paediatric short-stay wards were opened next to the ED. (Boyle AA, Robinson SM, et al, 2007). With this model it was found that integrated emergency care has the ability to use spare capacity within emergency care. If offers significant advantages 24 Correspondence with ED Advisory Group member, July 2009. Anecdotally, patients who are referred by their GP to an inpatient ward wait longer for review in comparison with direct presentation to the ED. 28 18 August 2009 Confidential to the ED Advisory Group and MoH contributors until approved for web publication beyond the ED. However, improved efficiency in processing emergency patients placed the hospital at a financial disadvantage. 2. Observation units Over the past two decades, the use of observation units to treat such common conditions as chest pain and asthma has greatly increased. These units allow patients to be directed out of ED acute care beds while potentially avoiding inpatient admission. Many studies have demonstrated the clinical effectiveness of care delivered in such a setting compared to the ED or inpatient ward and it has been shown that increased admission to an Observation Ward reduced admission to inpatient wards for selected diagnoses (Williams AG, Jelinek GA, et al, 2000). However, although observation units have emerged as a cost saving alternative to traditional ward admission for many paediatric illnesses (Mallory MD, Kadish H, et al, 2006) there are limited data published about observation unit finance (Baugh CW and Bohan JS, 2008). Subtraction of costs from payments may significantly underestimate the financial value of an observation unit admission. However, the positive value generated by an observation unit bed must be considered in the context of other projects available to hospital administrators (Baugh CW and Bohan JS, 2008). In NZ, the establishment of disease specific observation units in EDs is associated with ambulatory sensitive hospitalisations for specific conditions (Health Services Assessment Collaboration, 2008). A management protocol introduced into an existing ED observation unit for heart failure safely decreased ED visits by 56%. The protocol included diagnostic and therapeutic algorithms, cardiology consultation, close monitoring, patient education and discharge planning (Health Services Assessment Collaboration, 2008). 3. A range of different kinds of wards and units It is important to distinguish among the different kinds of wards and units that are associated with EDs. There are holding wards, clinical decision units, short stay units, all with slightly different functions. For instance, some hospitals have instituted holding areas for patients waiting for transfer to wards (Gantt LT, 2004). In a Melbourne study of 17 EDs where a range of traditional inpatient services were incorporated into EDs, short stay units were found to decrease patient admissions and average length of stay (ACEM, 2006) without compromising re-presentation rates upon discharge (Taylor D McD, Bennett DM, Cameron PA, 2004). Physically separating boarding patients from those still requiring emergency care gives clarity about the numbers of patients waiting and also enables staff to focus on the most appropriate care delivery for each group of patients. However such separation could also be viewed as adding another queue to the system rather than removing barriers to transfer (Bichan I, 2005). 8. Improving data quality and monitoring The ED Working Group recommended that enhancements could be made to the National Non-Admitted Patient Collection (NNPAC) in order to collect more detailed 29 18 August 2009 Confidential to the ED Advisory Group and MoH contributors until approved for web publication patient-level data from EDs. By 2010/2011 this could enable more nuanced monitoring of ED length of stay data, and exploration of the relationship between length of stay and patient outcomes (Working Group, 2008). In response to this recommendation, there are planned enhancements to the NNPAC. The Ministry of Health is planning to introduce additional fields to the NNPAC collection in order to supply the following information for emergency department patients: 1. Triage category 2. Time of presentation to the department 3. Time of first contact with doctor or other clinician offering definitive 4. assessment and treatment 5. Time of departure from the department (discharge, transfer to inpatient ward, or transfer to another facility). Introduction of these additional fields is expected to take place beginning with the 2010/2011 year. Conclusion In the literature, there is a wide range of innovative approaches and solutions to ED overcrowding and many of these are supported by good evidence. However, evidence from NZ is very sparse. As the table on pages 3 – 8 above shows, NZ experts concurred to a large extent with many of the findings of the UK systematic review (Cooke M, FisherJ, et al, 2005) but both the UK researchers and the NZ experts noted that many of those innovations have not been researched. Some suggestions follow, based on the expert opinion summarised on those pages, for work that might be done by DHBs to describe what happens at present and where they might make improvements for the purpose of reducing ED overcrowding: 1. Diversion of 111 calls, supported by after hours arrangements 2. Fast track systems for minor injuries 3. Interventions to reduce attendance by the elderly and those with long term conditions 4. Patient education in long term conditions management 5. Phoning for advice before going to the ED 6. Use of observation wards 7. Home support 8. Allowing ED staff to admit patients 9. Discharge from hospital that includes jointly constructed care pathways, social support and access to prescriptions 10. Teams of staff available for unpredicted surges 11. Use of senior staff, particularly clinical leaders with an inclusive management style 12. Use of Nurse Practitioners and other health care professionals. Some of these overlap with the following suggestions for further research which are based on research findings under the eight headings of the literature review. 30 18 August 2009 Confidential to the ED Advisory Group and MoH contributors until approved for web publication Approach or strategy Draft suggestions for NZ research 1. Using a national acute care strategy Contractility (throughput) studies (p.9) and perhaps a study based on or replicating the throughput changes in the St Joseph’s study (p.11) Pages 9 – 13 – a range of research possibilities 2. Using master plans within hospitals 3. Concentrating on ‘primary care’ presentations 4. Managing acute demand 5. Hospital capacity planning 6. Developing the ED workforce 7. Using other wards and units as an alternative to the ED 8. Improving data quality and monitoring Prospective audits of appropriateness of ED presentations (p.13 ) Replicate NSW DEED study (p.16) EDs screen for alcohol-related injury (p.18) Rate per 1000 of available acute beds (p.19) Studies of streaming using Lean (p.20) A range of new roles, use of NPs, expanded scope paramedics and other expanded scope professionals (pp. 24–27) Models of care: studies based on EDs in Auckland, Hawkes Bay and Nelson Marlborough DHBs (page 27) Run a health information research programme parallel to NNPAC improvements (p.24) ___________________________________________________________________ 31 18 August 2009 Confidential to the ED Advisory Group and MoH contributors until approved for web publication References ACEM Australasian College for Emergency Management (2000) Guidelines for Implementation of the Australasian Triage Scale in Emergency Departments http://www.medeserv.com.au/acem/open/documents/triageguide.htm (accessed April 2009) ACEM Australasian College for Emergency Management (2001) Fact Sheet: Urban emergency services – ATS 4 and 5 patients http://www.acem.org.au/media/ats_4_5_factsheet.pdf ACEM Australasian College for Emergency Management (2004a) Policy document. P31 Patient’s right to access Emergency Department care http://www.acem.org.au/media/policies_and_guidelines/patient_right_accesscare.pdf ACEM Australasian College for Emergency Management (2004b) The relationship between Emergency Department Overcrowding and Alternative After-Hours GP Services http://www.medeserv.com.au/acem/open/documents/after_hoursgp.pdf (accessed July 2009) ACEM Australasian College for Emergency Management (2006) Policy on the Australasian triage scale (adopted 1993, reviewed 2006) http://www.google.co.nz/search?hl=en&q=acem%2Btriage&btnG=Google+Search&m eta=&aq=f&oq= (accessed April 2009) Acute Demand Management Working Party (2007) Report Ministry of Health, Wellington Alberti G (2007) Emergency access: clinical case for change http://www.dh.gov.uk/en/Publicationsandstatistics/Publications/PublicationsPolicyAnd Guidance/DH_063288 Ali W (2006) Acute hospital bed occupancy and length of stay for patients in the Emergency Department (Unpublished descriptive review) Clinical Decision Support Unit, Christchurch School of Medicine and Health Sciences University of Otago Ardagh MW, Wells JE, Cooper K, Lyons R, Patterson R, O’Donovan P (2002) Effect of a rapid assessment clinic on the waiting time to be seen by a doctor and the time spent in the department, for patients presenting to an urban emergency department: a controlled prospective trial. NZ Med J 115:U28 http://www.nzma.org.nz/journal/115-1157/28/ (accessed April 2009) Ardagh M, Richardson S (2004) Emergency department overcrowding - can we fix it? The New Zealand Medical Journal 20;117(189):774 http://www.nzma.org.nz/journal/117-1189/774/ (Accessed April 2009) 32 18 August 2009 Confidential to the ED Advisory Group and MoH contributors until approved for web publication Ardagh M (2006) The case for a New Zealand acute care strategy NZ Med J 119 (1247) http://www.nzma.org.nz/jpurnal/119-1247/2360/ (accessed April 2009) Asplin BR (2001) Undertriage, overtriage or no triage? Annals of Emergency Medicine 38:282-285 http://emj.bmj.com/cgi/content/abstract/25/7/398 (accessed July 2009) Australian Health Workforce Advisory Committee (2006) Health workforce planning and models of care in emergency departments http://www.nhwt.gov.au/documents/Publications/2006/Health%20workforce%20plann ing%20in%20emergency%20departments.pdf (accessed May 2009) Bagust A, Place M, Posnett JW (1999) Dynamics of bed use in accommodating emergency admissions:stochastic simulation model. British Medical Journal 319(7203): 155 Baugh CW, Bohan JS (2008) Estimating observation unit profitability with options modeling Ac Emerg Med 15(5):445 Bichan I (2005) Patient flow in a New Zealand Emergency Department A research Report submitted in partial fulfilment of the requirements for the degree of Master of Nursing Massey University Library Blunt E (1998) Role and productivity of nurse practitioners in one urban emergency department J Emerg Nurs 20:7 Boyle AA, Robinson SM, Whitwell D, Myers S Bennett TJH, Hall N, Haydock S, Fritz Z and Atkinson P (2007) Integrated hospital emergency care improves efficiency Emerg Med J 25:78 Bradley VM (2005) Placing Emergency Department Crowding on the Decision Agenda Journal of Emergency Nursing 31:247 BRC (2002) The evaluation of the Healthline service. Final evaluative report http://www.moh.govt.nz/moh.nsf/pagesmh/702?Open (accessed August 2009) Capital and Coast DHB (2009) Monitoring of Capital and Coast DHBs’ Primary Care Framework. Monitoring Primary Care Framework.pdf Caplan GA, Williams AJ, Daly B, Abraham K (2004) A randomized, controlled trial of comprehensive geriatric assessment and multidisciplinary intervention after discharge of elderly from the emergency department – the DEED II study J Am Geriatr Soc 52:1417 Carter AJE and Chochinov AH (2007) A systematic review of the impact of nurse practitioners on cost, quality of care, satisfaction and wait times in the emergency department CJEM 9(4):286 33 18 August 2009 Confidential to the ED Advisory Group and MoH contributors until approved for web publication CENNZ – NZNO (2007) Position statement: Triaging away http://www.cennz.co.nz/CENNZ_Postn_Statement_Triaging_Away_2009.pdf (accessed May 2009) Chan DKY, Chong R, Basilikas J, Mathie M et al (2002) Survey of major chronic illness and hospital admissions via the emergency department in a randomized older population in Randwick, Australia Emergency Medicine 14:387 Connor J, Broad J, Jackson R, Vander Hoorn S, Rehm J (2005) The burden of death, disease and disability due to alcohol in New Zealand ALAC Occasional Publication no.23. Auckland, N.Z.: Alcohol Advisory Council of New Zealand http://www.alac.org.nz/FileLinks/12067_BurdenFull.516b09e5.pdf (accessed April 2009) Connor J, Broad J, Rehm J, Vander Hoorn S, Jackson R (2005a) The burden of death, disease and disability due to alcohol in New Zealand New Zealand Medical Journal, 118 (1213):1412 http://www.nzma.org.nz/journal/118-1213/1412/content.pdf (accessed April 2009) Cooke MW, Wilson S, Pearson S (2002) The effect of a separate stream for minor injuries on accident and emergency department waiting times EMJ 19:1 http://pt.wkhealth.com/pt/re/emj/abstract.00041859-20020100000009.htm;jsessionid=KdSZRxkLtpyg1QnNpBhhhx11vf2TCj7M9VbyvSNzmGFhwHv MxG3V!-847254088!181195628!8091!-1 (accessed July 2009) Cooke MW Higgins, J. and Kidd, P. (2003) Standards for the provision of emergency admission services: A review of the evidence http://74.125.155.132/search?q=cache:ilpjZIbQ1ioJ:www2.nphs.wales.nhs.uk:8080/D esignedforLifeDocs.nsf/85c50756737f79ac80256f2700534ea3/fdb61bce0797d74780 2570d60038c4a8/%24FILE/Emergency%2520Admissions%2520Literature%2520su mmary%25201%252011%252005%2520(2).doc+MW+Cooke%2Bemergency+depart ment&cd=36&hl=en&ct=clnk&gl=nz (accessed July 2009) Cooke MW (2003) Reforming the UK emergency care system. Emergency Medicine Journal 20:112 Cooke MW, Wilson S, Halsall J, Roalfe A (2004) Total time in English accident and emergency department is related to bed occupancy. Emergency Medicine Journal 21(5):575 Cooke M, Fisher J, Dale J, McLeod E, Szczepura A, Walley P, Wilson S (2005) Reducing attendances and waits in Emergency Departments: A systematic review of present innovations - Report to the National Co-ordinating Centre for NHS Service Delivery and Organisation R&D (NCCSDO) http://www.sdo.nihr.ac.uk/files/project/29final-report.pdf (accessed May 2009) 34 18 August 2009 Confidential to the ED Advisory Group and MoH contributors until approved for web publication Coombs M (2009) A review of seminal management and leadership papers in the UK Intensive Crit Care Nurs 25(3): 128 http://www.ncbi.nlm.nih.gov/pubmed/19318252?ordinalpos=12&itool=EntrezSystem2 .PEntrez.Pubmed.Pubmed_ResultsPanel.Pubmed_DefaultReportPanel.Pubmed_RV DocSum (accessed July 2009) Davis K, Schoen C, Schoenbaum SC, Doty MM, Holmgren AL, Kriss JL and Shea KK (2007) Mirror mirror on the wall: an international update on the comparative performance of American health care The Commonwealth Fund http://www.commonwealthfund.org/~/media/Files/Publications/Fund%20Report/2007/ May/Mirror%20%20Mirror%20on%20the%20Wall%20%20An%20International%20U pdate%20on%20the%20Comparative%20Performance%20of%20American%20Heal t/1027_Davis_mirror_mirror_international_update_final%20pdf.pdf (accessed June 2009) Degeling P, Close H, Degeling D (2006) Re-Thinking Long Term Conditions: A Report on the Development and Implementation of Co-Produced, Year-Based Integrated Care Pathways to Improve Service Provision to People with Long Term Conditions Centre for Clinical Management Development, Durham University http://www.southampton.ac.uk/healthsciences/research/projects/WDP/year_care/inde x.html (accessed April 2009) De Silva PT (2009) Why are we waiting? GP Registrar Audit 2008. GP Pulse The Royal New Zealand College of General Practitioners March issue http://www.rnzcgp.org.nz/assets/Uploads/docs/GP-Pulse-March-2009.pdf (accessed June 2009) DoH Department of Health (2002) Reforming Emergency Care Chief Nursing Officer Bulletin http://www.publications.doh.gov.uk/cno/bulletin8.htm#04 (accessed May 2009) DoH Department of Health (2005) Supporting people with long term conditions HMSO, London www.dh.gov.uk/en/Publicationsandstatistics/Publications/PublicationsPolicyAndGuid ance/DH_4100252 (accessed April 2009) Dunn R (2003) Reduced access block causes shorter emergency department waiting times: An historical control observational study. Emergency Medicine Australasia 15(3): 232 Eagar K (2005) The relationship between GP availability and use of EDs by primary care patients Centre for Health Services Development, University of Wollongong, powerpoint presentation http://chsd.uow.edu.au/Publications/2005_pubs/relationship_between_ed_and_gp.pd f (Accessed April 2009) 35 18 August 2009 Confidential to the ED Advisory Group and MoH contributors until approved for web publication Elley CR, Randall P-J, Bratt D, Freeman P (2007) Can primary care patients be identified within an emergency department workload? NZ Med J 120(1256):U2583 Emergency Nurses Association (ENA) (2006) Emergency Nurses Association Position Statement: Crowding in the Emergency Department Journal of Emergency Nursing 32(1):42 http://www.prnewswire.com/mnr/ena/26785/docs/Position_Statement_Emergency_D epartment_Crowding.doc (accessed April 2009) Estey A, Ness K, Saunders D (2003) Understanding the causes of overcrowding in emergency departments in the Capital Health Region in Alberta: a focus group study. Canadian Journal of Emergency Medicine 5(2):87 Forero R, Mohsin M, Bauman AE, Ieraci S, Young L, Phung HN, Hillman KM, McCarthy SM, Hugelmeyer CD (2004) Access block in NSW hospitals, 1999 – 2001: does the definition matter? MJA 180 (2): 67 http://www.mja.com.au/public/issues/180_02_190104/for10259_fm.html (accessed May 2009) Forero R, Hillman KM (2008) Access Block and Overcrowding: A Literature Review prepared for the Australasian College of Emergency Management (ACEM), Simpson Centre for Health Services Research, South Western Sydney Clinical School, and the University of New South Wales. This report was presented to the Access Block Summit organised by ACEM in Melbourne on 12 September 2008. http://www.acem.org.au/media/Access_Block1.pdf (accessed April 2009) Forster AL, Stiell I, Wells G, Lee AJ, van Walraven C (2003) The Effect of Hospital Occupancy on Emergency Department Length of Stay and Patient Disposition. Academic Emergency Medicine 10:127 Gantt LT (2004) A strategy to manage overcrowding: development of an ED holding area J Emerg Nurs 30(3):237 George S, Read S, Westlake L, Williams B, Fraser-Moodie A and Pritty P (1992) Evaluation of nurse triage in a British accident and emergency department British Medical Journal 304:876-878 http://www.bmj.com/cgi/content/abstract/304/6831/876 (accessed July 2009) - ref to full article to come Gorelick MH, Yen K, Yun HJ. (2005) The effect of in-room registration on emergency department length of stay. Annals of Emergency Medicine 45(2):128 Government of Western Australia, Department of Health (2008) Emergency Department Access Block: Reporting Definition Paper prepared by Information Management and Reporting Gray JT and Walker A (2008) Avoiding admissions from the ambulance service: a review of elderly patients with falls and patients with breathing difficulties seen by Emergency Care Practitioners in South Yorkshire Emerg Med J 25 168 http://emj.bmj.com/cgi/content/abstract/25/3/168 (accessed July 2009) 36 18 August 2009 Confidential to the ED Advisory Group and MoH contributors until approved for web publication Green LV, Soares J Giglio JF, Green RA (2006) Using queuing theory to increase the effectiveness of emergency department provider staffing Journal of Academic Emergency Medicine 13:61 http://www.hbs.edu/units/tom/seminars/2007/docs/lgreen3.pdf (accessed July 2009) Gribben B (2003) Implementing integrated care in Counties Manukau NZMJ 116:1169 http://www.nzma.org.nz/journal/116-1169/323/ (accessed July 2009) Health Policy Monitor (2008) http://www.hpm.org/en/Surveys/The_University_of_Auckland/12/Optimising_the_pati ent_s_journey.html (accessed June 2009) Health Services Assessment Collaboration (2008) The Effectiveness of Interventions for Reducing Ambulatory Sensitive Hospitalisations Health Sciences Centre, University of Canterbury http://www.healthsac.net/downloads/publications/ASH%20Report.pdf (accessed June 2009) Hegney D, Buikistra E Chamberlain C, March J et al (2006) Nursing discharge planning in the emergency departments: a Toowoomba, Australia study J Clinical Nursing 15:1033 Hughes G ( 2008) The Clockwork ED Emergency Medicine Journal 25:546 Humphrey G, Casswell S, Han DY (2003) Alcohol and injury among attendees at a New Zealand emergency department NZMJ 116:1168 http://www.nzma.org.nz/journal/116-1168/298/ (accessed April 2009) Hwang U, Richardson LD, Sonuyi TO, Morrison RS (2006) The effect of emergency department crowding on the management of pain in older adults with hip fracture J Am Geriatr Soc 54:270 Joyce PR (2005) Editorial Australian & New Zealand Journal of Psychiatry. 39(7):531 King DL, Ben-Tovim DI, Bassham J (2006) Redesigning emergency department patient flows: Application of Lean Thinking to Health Care Emergency Medicine Australasia 18 (4): 391 http://www.ncbi.nlm.nih.gov/pubmed/16842310?dopt=AbstractPlus (accessed May 2009) Kulkarni RG (2007) Going lean in the emergency department: a strategy for addressing emergency department overcrowding MedGenMed 9(4):58 http://www.pubmedcentral.nih.gov/articlerender.fcgi?artid=2234328 (accessed April 2009) Kyriacou DN, Ricketts V, Dyne PL, McCollough MD, Talan DA (1999) A 5-year time study analysis of emergency department patient care efficiency. Annals of Emergency Medicine 34(3):326 37 18 August 2009 Confidential to the ED Advisory Group and MoH contributors until approved for web publication Langley J, Chalmers D, Fanslow J (1996) Incidence of death and hospitalisation from assault occurring in and around licensed premises: comparative analysis. Addiction 91:985. Langley J, Kypri K, Cryer C, Davie G (2008) Assessing the validity of potential alcohol-related non-fatal injury indicators Addiction 103(3) http://www.ncbi.nlm.nih.gov/pubmed/18190665 (accessed July 2009) Lee T, Johnson N (2009) Building the clockwork pediatric emergency department” Poster for the National Associations of Children’s Hospitals and Related Institutions and National Association of Children’s Hospitals (NACHRI & N.A.C.H) Creating Connections Conference, March 2009 http://www.childrenshospitals.net/AM/Template.cfm?Section=Posters1&CONTENTID =39181&TEMPLATE=/CM/ContentDisplay.cfm (Accessed May 2009) LSU (Louisiana State University) Health Sciences Center http://www.lsuhsc.edu/hcsd/cmo/hcet/docs/Facts/ED_Log.pdf (accessed May 2009) McDonald AJ III; Wang N, Camargo CA Jr (2004) US Emergency Department Visits for Alcohol-Related Diseases and Injuries Between 1992 and 2000 Arch Intern Med 164 (5): 531 Mallory MD, Kadish H, Zebrack M, Nelson D (2006) Use of pediatric observation unit for treatment of children with dehydration cased by gastroenteritis Pediatric Emergency Care 22 (1):1 Mason S, Knowles E, Colwell B, Dixon S, Wardrope J, Gorringe R, Snooks H, Perrin J and Nicholl J (2007) Effectiveness of paramedic practitioners in attending 999 calls from elderly people in the community: cluster randomized controlled trial BMJ 335 919 http://www.bmj.com/cgi/content/full/335/7626/919 Accessed July 2009 Mason S, O’Keeffe C, Coleman P, Edlin R and Nicholl J (2007) Effectiveness of Emergency Care Practitioners working within existing emergency service models of care Emergency Med J 24 239. http://emj.bmj.com/cgi/content/abstract/24/4/239 Accessed July 2009 Ministry of Health (2008) Statement of Intent 2008 – 2011 Operating Intentions: A. Taking public and primary health care to the next level http://www.moh.govt.nz/moh.nsf/indexmh/soi0811-intentions-a (accessed July 2009) Monash University Accident Research Centre Victorian Injury Surveillance Unit (2009) Unintentional (Accident) Hospital Treated Injury 2007, State Government of Victoria, Department of Human Services, Edition 4 http://www.monash.edu.au/muarc/VISU/reports/Ebulletin%20Edition%204%20Hospital.pdf (accessed May 2009) 38 18 August 2009 Confidential to the ED Advisory Group and MoH contributors until approved for web publication Murphy AW, Bury G, Plunkett PK, et al (1996) Randomised controlled trial of general practitioner versus usual medical care in an urban accident and emergency department: process, outcome, and comparative cost. BMJ 312:1135 Nelson Marlborough DHB (2008) Broadsheet 39 http://www.nmdhb.govt.nz/filesGallery/New%20Website/08Latest%20News%20&%2 0Events/BroadsheetNovember08.pdf (accessed June 2009) Otago Daily Times (28 April 2009) article by Elspeth McLean http://www.odt.co.nz/news/dunedin/52517/emergency-department-urged-keepalcohol-statistics (accessed April 2009) Pereira S, Oliveira E, Silva A, et al (2001). Appropriateness of emergency department visits in a Portuguese university hospital Ann Emerg Med. 37:580 Proudlove NC, Gordon K, and Boaden R (2003) Can good bed management solve the overcrowding in accident and emergency departments? Emergency Medicine Journal;20;149 Quarrie K, Feehan M, Waller A, et al (1996) The New Zealand Rugby Injury and Performance Project: alcohol use patterns within a cohort of rugby players. Addiction;91:1865 Richards G (2008) The burden of alcohol related injuries in New Zealand: a brief guide to the literature Safe Communities Foundation New Zealand / ALAC Alcohol and Community Safety Regional Forums (North Island) http://www.safecommunities.org.nz Richardson DB (2001) The access-block effect: relationship between delay to reaching an inpatient bed and inpatient length of stay MJA 177:492 Richardson DB, Mountain D (2009) Myths versus facts in emergency department overcrowding and hospital access block. Med J Aust 190: 370 Richardson S, Ardagh M, Hider P (2006) New Zealand health professionals do not agree about what defines appropriate attendance at an emergency department NZMJ 119 (1232) http://www.nzma.org.nz/journal/119-1232/1933/ (accessed May 2009) Rogers T, Ross N, Spooner D (2004) Evaluation of a see and treat pilot study introduced to an emergency department Accid Emergency Nurs 12:24 Rudd J (2005) From triage to treatment: an exploration of patient flow systems in Emergency departments, a research paper submitted to the Victoria University of Wellington in partial fulfilment of the requirements for the degree of Master of Nursing (Clinical), Victoria University of Wellington. Wellington NZ Schmidt TA, Iserson KV, Freas GC et al (1995) Ethics and Emergency Department Triage: SAEM position statement Academic Emergency Medicine 2:990 http://linkinghub.elsevier.com/retrieve/pii/S0196064406007049 (Not accessed – referred to by Cooke M, Fisher J et al (2005) cited above) 39 18 August 2009 Confidential to the ED Advisory Group and MoH contributors until approved for web publication Schneider S, Zvemer F, Doniger A, et al (2001) New York: a decade of emergency department overcrowding Acad Emerg Med 8:1044 Siminski P, Bezzina A, Lago L, Eagar K (2008) Trends in Primary Care Presentations at Emergency Departments in New South Wales (1999–2006) Australian Journal of Primary Health 14(3) 35 Skills for health: Emergency care practitioners http://www.skillsforhealth.org.uk/resource-library/~/media/ResourceLibrary/PDF/Emergency_Care_Practitioners.ashx (Accessed July 2009) Sprivulis PC (2004) Pilot study of metropolitan emergency department workload capacity Emergency Medicine Australasia, 16(1):59. Sprivulis PC, Da Silva J-A, Jacobs IG, Frazer ARL, Jelinek GA (2006) The Association between hospital overcrowding and mortality among patients admitted via Western Australian emergency departments MJA 184 (5): 208 http://www.mja.com.au/public/issues/184_05_060306/spr10395_fm.html (accessed April 2009) Stirling CM, O’Meara P, Pedler D, Tourle V, Walker J (2007) Engaging rural communities in health care through a paramedic expanded scope of practice Rural and Remote Health 7: 839 http://www.rrh.org.au/articles/showarticlenew.asp?ArticleID=839 (accessed May, 2009) Stone K (2008) Excellence in Healthcare: Analysis of patient demographics for patients presenting to Rotorua Hospital Emergency Department in August 2008, unpublished report prepared for Lakes DHB by Rotorua Area Primary Health Services. Tachakra S, Stinson A (2000) Emergency nurse practitioners should manage major cases Emerg Nurse 8:12 Taylor D McD, Bennett DM, Cameron PA (2004) A paradigm shift in the nature of care provision in emergency departments Emerg Med J 21:681 http://scholar.google.co.nz/scholar?hl=en&lr=&cluster=4024183129148494867&um= 1&ie=UTF8&ei=2i7tSeaeGpnutQOG88nrAQ&sa=X&oi=science_links&resnum=1&ct=slallversions (accessed April 2009) Travers JP, Lee FCY (2006) Avoiding prolonged waiting time during busy periods in the emergency department: is there a role for the senior emergency physician in triage? European Journal of Medicine 13:342 Trzeciak S, Rivers EP (2003) Emergency department overcrowding in the United States: an emerging threat to patient safety and public health Emerg Med J 20:402 Twanmoh JR, Cunningham GP (2006) When overcrowding paralyzes an emergency department Managed Care http://www.managedcaremag.com/archives/0606/0606.peer_ER.pdf (accessed May 2009) 40 18 August 2009 Confidential to the ED Advisory Group and MoH contributors until approved for web publication Vega V, McGuire SJJ,(2007) Speeding up the Emergency Department: the RADIT Emergency Program at St Joseph Hospital of Orange, Heldref Publications http://heldrefpublications.metapress.com/app/home/contribution.asp?referrer=parent&backto=issu e,4,8;journal,8,23;linkingpublicationresults,1:119927,1 (accessed April 2009) Victorian Department of Health and Human Services (2005) Final Report: Work analysis project: Emergency Department, Intensive Care Unit, Radiology Department Commissioned from Bearing Point (unpublished) Waikato DHB (2009) http://www.waikatodhb.govt.nz/news/pageid/2145843729 (accessed April 2009) Washington DL, Stevens CD, Shekelle PG, Hennemann PL, Brook RH (2002) Nextday care for emergency department users with nonacute conditions Ann Intern Med 137:707 http://www.annals.org/cgi/content/abstract/137/9/707 (accessed July 2009) WHO World Health Organisation (2004) Chronic conditions: The global burden Geneva, WHO www.who.int/healthinfo/global_burden_disease/2004_report_update/en/index.html (accessed April, 2009) WHO World Health Organisation (2007). Alcohol and injury in emergency departments. Summary of the report from the WHO Collaborative Study on Alcohol and Injuries. Geneva, WHO http://www.who.int/substance_abuse/publications/alcohol_injury_summary.pdf (accessed april 2009) Williams AG, Jelinek GA, Rogers IR, Wenban JA, Jacobs IG (2000) The effect on hospital admission profiles of establishing an emergency department observation ward. Med J Aust 179:99 Wilson H (2005) Co-locating primary care facilities within emergency departments: brilliant innovation or unwelcome intervention into clinical care? NZ Med J 26:118 http://www.nzma.org.nz/journal/118-1221/1633/ (accessed April 2009) Wilson MJ, Siegel B, Williams M (2005) Perfecting patient flow: America’s safety net hospitals and emergency department crowding National Association of Public Hospitals and Health Systems. Prepared by the Urgent Matters Program, The George Washington University Medical Center, School of Public Health and Health Services, Department of Health Policy www.rwjf.org/files/publications/other/PerfectingPatientFlow.pdf (accessed April 2009) Womack JP, Jones DT, Roos D (1991)The Machine That Changed the World: Based on the Massachusetts Institute of Technology 5-Million-Dollar 5-Year Study on the Future of the Automobile. New York: Simon & Schuster Working Group for Achieving Quality in Emergency Departments (2008) Recommendations to Improve quality and the Measurement of Quality in New 41 18 August 2009 Confidential to the ED Advisory Group and MoH contributors until approved for web publication Zealand Emergency Departments Wellington: Ministry of Health http://www.moh.govt.nz 42 18 August 2009 Confidential to the ED Advisory Group and MoH contributors until approved for web publication Appendix Search methods A review of the literature was undertaken by searching various electronic databases including Medline, Cochrane, EMBASE, CINAHL, PUBMED, Trip, as well as bibliographic references and snowballing to locate relevant papers. The electronic database searches were restricted to literature published in English language between 1996 and 2009 and editorial or opinion articles were excluded. Grey literature searches were conducted, for government reports, academic reports and conference proceedings. Bibliographies of retrieved articles were searched for relevant citations. The Working Group’s Report references were followed up. Key words for electronic database searches Database: Ovid MEDLINE(R) <1996 to February Week 4 2009> Search Strategy: -------------------------------------------------------------------------------1 Emergency Service, Hospital/ (18106) 2 (emergency adj2 department$).mp. (19880) 3 1 or 2 (28869) 4 3 and (solution$ or "best practice" or "best practices").ab,ti. (427) 5 Crowding/ (710) 6 (overload$ or overcrowd$).mp. [mp=title, original title, abstract, name of substance word, subject heading word] (13463) 7 4 and (5 or 6) (32) 8 (capacity adj2 asses$).mp. (1188) 9 (full adj3 capacity planning).mp. [mp=title, original title, abstract, name of substance word, subject heading word] (0) 10 (surge adj2 (capacity or demand)).mp. (185) 11 (optim$ adj3 size).mp. [mp=title, original title, abstract, name of substance word, subject heading word] (933) 12 (trolley adj2 (stay$ or wait$)).mp. (4) 13 (corridor$ adj2 (stay$ or wait$)).mp. (1) 14 Waiting Lists/ (4561) 15 4 and 14 (11) 16 14 and 3 and reduc$.mp. (57) 17 3 and reduc$.mp. (3722) 18 *Emergency Service, Hospital/og (2446) 19 18 and coordinat$.mp. (58) 20 3 and access block$.mp. and (solution$ or best practice$ or reduc$).mp. [mp=title, original title, abstract, name of substance word, subject heading word] (11) 21 3 and demand manag$.ab,ti. (7) 22 3 and (8 or 9 or 10 or 11 or 12 or 13) (63) 23 3 and reduc$.mp. and (5 or 6) [mp=title, original title, abstract, name of substance word, subject heading word] (88) 24 7 or 15 or 16 or 19 or 20 or 21 or 22 or 23 (287) 25 (England or Ireland or Wales or Scotland or Sweden or Denmark or Holland or France or Spain or Germany or Italy or Canada or Australia).mp. (309408) 26 24 and 25 (48) 27 24 and (systematic review$ or meta-anal$).ab,ti. (5) 28 24 and review$.ti. (9) 29 26 or 27 or 28 (56) 30 queu$ theory.mp. [mp=title, original title, abstract, name of substance word, subject heading word] (45) 31 ambulance diversion$.mp. (77) 32 3 and (30 or 31) and (25 or systematic review$.mp. or meta-anal$.mp.) [mp=title, original title, abstract, name of substance word, subject heading word] (9) 33 29 or 32 (60) 34 limit 33 to (english language and yr="2003 - 2009") (45) 43 18 August 2009 Confidential to the ED Advisory Group and MoH contributors until approved for web publication 35 from 34 keep 1-45 (45) 1 Hospital Bed Capacity/ (1159) 2 Emergency Service, Hospital/ (18106) 3 (emergency adj2 department$).mp. [mp=title, original title, abstract, name of substance word, subject heading word] (19880) 4 1 and (2 or 3) (143) 5 (ward$ adj2 space$).mp. or hospital units/ [mp=title, original title, abstract, name of substance word, subject heading word] (2907) 6 (2 or 3) and 5 (165) 7 (surge adj2 (capacity or demand)).mp. (185) 8 7 and (2 or 3) and plan$.mp. [mp=title, original title, abstract, name of substance word, subject heading word] (40) 9 unscheduled care collaborative.mp. (0) 10 triage/ (3850) 11 patient admission/ (8573) 12 admitting department/ (253) 13 10 and (11 or 12) and (2 or 3) (134) 14 (patient adj2 flow).mp. [mp=title, original title, abstract, name of substance word, subject heading word] (506) 15 patient transfer/ (2740) 16 (14 or 15) and (2 or 3) (712) 17 (England or Ireland or Wales or Scotland or Sweden or Denmark or Holland or France or Spain or Germany or Italy or Canada or Australia).mp. (309408) 18 4 or 6 or 8 or 9 or 13 or 16 (1129) 19 17 and 18 (170) 20 limit 19 to (english language and humans and yr="2003 - 2009") (92) 21 from 20 keep 1-92 (92) 22 ((when or time) adj2 admit).mp. [mp=title, original title, abstract, name of substance word, subject heading word] (14) 23 22 and (2 or 3) (2) 24 23 and 17 (0) 25 18 and (systematic review$ or meta-analysis).mp. [mp=title, original title, abstract, name of substance word, subject heading word] (4) 26 21 or 24 or 25 (96) 27 from 25 keep 1-4 (4) 28 from 26 keep 1-96 (96) Emergency Services Solutions - Cochrane #1 MeSH descriptor Emergency Service, Hospital explode all trees 1264 edit delete #2 (emergency department*):ti,ab,kw 2222 edit delete #3 (#1 OR #2) 2751 edit delete #4 (solution*):ti,ab,kw or (best practice*):ti,ab,kw or (reduc*):au 16731 edit delete #5 (#3 AND #4) 112 edit delete #6 MeSH descriptor Triage explode all trees 156 edit delete #7 MeSH descriptor Patient Transfer explode all trees 104 edit delete #8 "patient flow":ti,ab,kw 19 edit delete #9 MeSH descriptor Patient Admission explode all trees 601 edit delete #10 MeSH descriptor Admitting Department, Hospital explode all trees 4 edit delete #11 MeSH descriptor Hospital Bed Capacity explode all trees 183 edit delete #12 MeSH descriptor Hospital Units explode all trees 2396 edit delete #13 "ward space":ti,ab,kw 0 edit delete #14 MeSH descriptor Crowding explode all trees 15 edit delete #15 (overcrowd* ):ti,ab,kw or (overload*):ti,ab,kw 546 edit delete #16 (capacity):ti,ab,kw 11004 edit delete #17 (corridor stay*):ti,ab,kw or (trolley stay*):ti,ab,kw 1 edit delete #18 (optimum size):ti,ab,kw 59 edit delete #19 MeSH descriptor Waiting Lists explode all trees 219 edit delete 44 18 August 2009 Confidential to the ED Advisory Group and MoH contributors until approved for web publication #20 (access block):ti,ab,kw or (ambulance diversion):ti,ab,kw or (queue theory):ti,ab,kw or (demand manage*):ab 341 edit delete #21 (#3 AND ( #6 OR #7 OR #8 OR #9 OR #10 OR #11 OR #12 OR #13 OR #14 OR #15 OR #16 OR #17 OR #18 OR #19 OR #20 )), from 2000 to 2009 172 edit delete #22 (#21 AND ( solution* OR ( best AND practic* ) OR strateg* OR reduc* )) 71 edit delete #23 (#1 AND ( #6 OR #7 OR #8 OR #9 OR #10 OR #11 OR #12 OR #13 OR #14 OR #15 OR #16 OR #17 OR #18 OR #19 OR #20 )), from 2000 to 2009 128 edit delete #24 (#1 AND ( #6 OR #7 OR #8 OR #9 OR #10 OR #11 OR #12 OR #13 OR #14 OR #15 OR #16 OR #17 OR #18 OR #19 OR #20 )), from 2000 to 2009 128 edit delete #25 (emergency):ti 1745 edit delete #26 (#24 AND #25) 65 edit delete #27 (#26), from 2003 to 2009 43 edit delete 45