Board Meeting - Health in Wales
advertisement

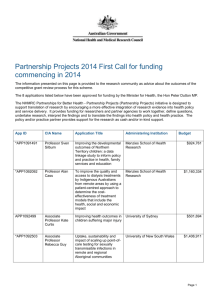
North Wales Transition Board Meeting 6th February 2009 . Neurocritical Care for North Wales STATUS: For Information/For Decision/For Discussion The Transition Board are asked to: Note the impact of the critical care development at the Walton Centre on the care pathway for patients with serious head injury. Agree the proposed action to enable HCW to agree the 2009/10 LTA with the Walton Centre. 1.0 PURPOSE OF PAPER This paper sets out the rationale for increasing neurocritical care provision for patients resident in North Wales, and details the actions necessary in order for HCW to reach agreement with the Walton Centre for the 2009/10 long term agreement. The North Wales Critical Care Network have developed a supporting paper (annex 2) which explains the impact on the regional ICUs of the Walton critical care development in the context of current demand, and explains the financial impact on the North Wales community in the context of the Network’s newly developed ‘severely head injured pathway’. 2.0 INTRODUCTION Neurocritical care is the branch of critical care that deals with patients with neurological illnesses, injury or trauma; it comprises high dependency (level 2) and intensive care (level 3) units. Neurocritical care for patients in North Wales is delivered predominantly by the Walton Centre for Neurology and Neurosurgery NHS Trust; however a significant number of patients with neurological illnesses or trauma receive critical care from the District General Hospitals in North Wales. Last year, ICNARC data showed that in the North Wales Intensive Care Units (ICUs), over 200 bed days were utilised by patients with severe head injury. 3.0 THE RATIONALE FOR CHANGING THE MODEL FOR NEUROCRITICAL CARE One of the recommendations of the Welsh Neuroscience External Expert Review was that the population of North Wales should continue to receive neurocritical care at the Walton centre, and the capacity should be expanded to accommodate appropriate patients (e.g. surgical, spinal and acute neurology patients) who are currently managed within the DGH critical care units.. Whilst the published recommendations for North Wales recommend that 10 – 12 beds would be required for the population1, the source document states that there is a body of opinion that believes these estimates to be excessive and that a responsive neurocritical care service can be delivered with fewer beds. This is based on the Association of British Neurologists estimate that 5 to 7 beds per million are required for neurocritical care. 1 1 North Wales Transition Board 6th February 2009 North Wales Transition Board Meeting 6th February 2009 . The National Institute for Clinical Excellence Clinical Guideline 56 (NICE CG56 2007) ‘Head Injury; Triage, assessment, investigation and early management of head injury in infants, children and adults’ also recognises that transfer (to neurosciences unit with a neurocritical care unit) would benefit all patients with serious head injuries (GCS < 8), irrespective of the need for neurosurgery. This guidance is also consistent with the data from TARN which suggests that outcomes for patients with severe head injuries are better when admitted to neurocritical care unit, than those admitted to a general critical care unit. Disability following neurotrauma is a significant, but under recognised, burden for social and healthcare communities. There is no mechanism to identify the costs of this burden in North Wales but it is likely to be substantial. The Walton Centre currently has an 8 bedded neurocritical care unit to cover its whole catchment area of 3.4 million; however it has been acknowledged for some time that the current service has been under considerable pressure and does not have the capacity necessary to accept all referrals for patients with severe head injuries. In response to TARN data and NICE guidance the Walton Centre have submitted a business case to the North West Specialised Commissioning Group with a series of options for increasing critical care provision within the Trust. The North West England Specialised Commissioning Group has now agreed to support the development of a new build with 6 – 7 beds. Under this model the Trust would have an additional 6.5 beds with occupancy of 87%. This additional capacity will enable the Walton Centre to admit a greater number of patients with serious head injuries from their catchment area of North West England and North Wales. Estimate of Additional Demand and Costs There is limited available benchmarking data available to evaluate the Walton proposal, therefore a series of models have been used to calculate the potential impact. These are detailed in Annex 1. There are three variables to take account of when modelling the impact of the additional demand for North Wales: 1. Number of additional patients – using the various models this varies from 16 to 23 per annum. The view of the North Wales Critical Care Network is that it is likely that actual demand is higher than this, and as such, is undertaking both a retrospective and prospective audit to ascertain both surgical and acute neurological demands. Preliminary results indicate that additional demand is likely to be around 28 per annum (annex 2). However, demand will be constrained by available capacity which in turn will be determined by the demand from the North West England region. 2. Length of Stay – National data from neurocritical care units subscribing to the ICNARC Case Mix Programme Database during 2007 and 2008 showed an average length of stay (ALOS) 7.9 days; However, data from the Walton Centre indicates that the ALOS for Welsh patients is 10.94 days . One possible explanation for the comparatively high length of stay at the Walton Centre may be due to the difficulties experienced with repatriation to DGHs in North Wales. (see section 5.0) 3. Bed day cost – this is £1641 under the current contract with Walton 2 North Wales Transition Board 6th February 2009 North Wales Transition Board Meeting 6th February 2009 . 3.0 FINANCIAL CONSEQUENCES As the bed day costs are fixed at £1641, the only variables are demand and length of stay. The rationale for the demand and length of stay figures are explained in detail in annex 1. These are summarised in the table overleaf. Demand 162 184 235 286 16 18 23 28 16 18 23 28 16 18 23 28 LOS 4.63 4.6 4.6 4.6 9.67 9.6 9.6 9.6 10.98 10.9 10.9 10.9 149 14 14 14 Bed day cost £1,641 £1,641 £1,641 £1,641 £1,641 £1,641 £1,641 £1,641 £1,641 £1,641 £1,641 £1,641 £1,641 £1,641 £1,641 £1,641 Total £120,777 £135,874 £173,617 £211,360 £252,057 £283,564 £362,332 £441,100 £286,190 £321,964 £411,398 £500,833 £367,584 £413,532 £528,402 £6443,272 The Walton Centre requires a response from HCW to allow for the lead time in getting staff and infrastructure in place. The NICE costing template is clear that the bulk of costs are offset by opportunity savings within the secondary care services. However, feedback from the North Wales Critical Care Network indicates that these services are currently oversubscribed; therefore the expansion of capacity at the Walton Centre represents an additional cost pressure for commissioners. The results from the North Wales Critical Care Network retrospective audit indicate that a further ten patients could benefit from admission to the Walton Centre Critical Care Unit. Therefore if demand was not constrained by available capacity, the number of patients admitted could be as high as 28 per annum, this would represent an additional cost pressure of approximately £500,000 for the North Wales health community. However, it is likely that the available capacity for North Wales patients will be constrained by the impact of demand from the North West health community. The Walton Centre estimated that demand is approximately 18 patients per annum, and have applied an average length of stay of 14 days to calculate a cost of £413,532 per annum. However, the Trust has now provided further data which indicates that the average length of stay for Welsh patients is 10.9 days, Applying this figure to an estimated demand of 18 patients, reduces the cost to £321,964. This estimate (highlighted in the table above) provide 2 Demand derived using NICE costing tool, excluding paediatric population. LOS based on NICE costing tool 4 Demand derived from Walton Centre estimate. 5 Demand derived from Mersey and Cheshire Critical Care Network Audit 6 Demand derived from North Wales Critical Care Network Retrospective Audit 7 LOS based on Hospital Episode Statistics average length of stay 8 LOS based on Walton data for Welsh patients 9 LOS based on Walton initial estimate 3 3 North Wales Transition Board 6th February 2009 North Wales Transition Board Meeting 6th February 2009 . a realistic starting point for discussion between HCW and the North Wales transition project board about the level of additional funding required to commission additional activity from the Walton Centre. The Annual Operating Framework for 2009/10 states that there “should be a working assumption that the distribution of the HCW allocation to the new LHBs in the second half of 2009/2010 will be on a notional basis only, and that, in practice, the commitments entered into by HCW at the beginning of 2009/2010 will be honoured throughout 2009/2010. There will be exceptions to this which will need to be carefully managed during 2009/2010, and will be dependent on the establishment of successor arrangements for HCW.” It also emphasises the need for HCW to work closely with the transition project teams to ensure that there is transparency on how funds will be committed, and how that funding will be sourced from the new LHBs once the funding for specialised services has been fully distributed. As this new development will open in October 2009, agreement is needed between the transition project board for North Wales and HCW, on the arrangements for contracting with the Walton Centre in 2009/10. Furthermore, as no additional resource has been allocated to implement the recommendations of the neurosciences review, it is clear that this additional capacity represents an additional cost pressure of approximately £322,000 for the North Wales health community. Consideration needs to be given about the process for agreeing the level of prioritisation of this development against existing and emerging commitments for the North Wales health community. It is clear that this development will enable the Walton Centre to admit a higher proportion of referrals to neurocritical care; however the development will not be sufficient to admit all appropriate referrals. Therefore, it is likely that a number of patients who would benefit from admission to the Walton Centre will continue to receive Critical Care within the North Wales DGHs. 4.0 STAKEHOLDER ENGAGEMENT The development of neurocritical care at the Walton Centre offers the potential to change the care pathway and to improve the outcomes for patients with serious head injury. It will only be possible to provide a commitment to the Walton Centre if the proposed change is supported by the North Wales transition project board and the new LHBs. 5.0 IMPACT ON OTHER SERVICES The North Wales Critical Care Network has, in collaboration with the Walton Centre, developed referral and repatriation pathway. The Network has also written a ‘care bundle’ for those patients who remain in the local DGH units. The pathway aims to enhance the consistency of referrals from North Wales as well as the timeliness of repatriations returning to the local critical care units for their ongoing care and management. Concomitant work on local critical care patient flows demonstrated frequent cancelled operations due to lack of critical care beds, transfers for non-clinical reasons i.e. insufficient critical care beds, premature discharges from critical care (to free up critical care capacity) as well as significant delays in repatriations from the Walton centre. The Lyon’s et al study (2000) indicates that critical care capacity in North Wales is short by 15 level 3 (ICU) beds and 36 level 2 (HDU) beds. It is acknowledged that these figures may 4 North Wales Transition Board 6th February 2009 North Wales Transition Board Meeting 6th February 2009 . be overestimated so the Network has commissioned some specific capacity modelling to assess the shortfall; the results of which are due soon. The most recent patient flow study, undertaken by the Network in July 2008, confirmed delays repatriating three patients from Walton totalling 234hrs – the equivalent of almost 10 days (66, 72 and 96hrs). These delays were all as a direct result of lack of capacity in the North Wales critical care units. 6.0 HUMAN RIGHTS AND WELSH LANGUAGE ACT The subject of this report has been checked for compliance with the Human Rights Act, the Race Relations Acts and Welsh Language Acts There is full compliance with the Acts 7.0 ACTION PLANNED HCW is due to meet with the Walton Centre on the 18th February to commence discussions on the 2009/10 long term agreement. The Walton Centre has requested that HCW confirm it’s commitment to commissioning additional neurocritical care capacity from October 2009 onwards. 8.0 RECOMMENDATIONS The North Wales Transition Board is recommended to: Advise on the level of commitment that HCW had provide to the Walton Centre regarding the development as part of the 2009/10 service level agreement. Prepared by: Date: Ian Langfield, HCW Sue O’Keefe obo North Wales Critical Care Network 4th February 2009 5 North Wales Transition Board 6th February 2009 North Wales Transition Board Meeting 6th February 2009 . Annex 1 Estimated Financial Impact of Neurocritical Care Expansion at Walton Centre The following models have been used to estimate the financial impact of neurocritical care at the Walton Centre. Walton Estimate Walton has estimated that approximately 18 additional patients per annum, who are currently unable to access the service, will be admitted into the expanded neurocritical care. They have applied an average length of stay of 14 days and a unit cost of £1641 to arrive at a cost of £413,000, per annum. This would represent approximately additional one bed per annum within the expanded unit. This estimate does not include the increased transfer costs that will be incurred by the Welsh Ambulance Service. Walton has since provided data on the LOS of Welsh patients receiving neurocritical care at the Trust, this indicates that the average length of stay for all indications is 10.9 days. NICE Costing Tool NICE have developed a costing tool to accompany clinical guidelines on the management of adults and children with serious head injuries. The costing tool identifies the impact of transferring the critical care activity from secondary care to tertiary care centres. Using the Standard Assumptions within the costing tool (excluding the paediatric population, as they receive neurosurgical critical care from Royal Liverpool Children’s Hospital), it estimates that there would be 16 additional patients per annum, at a cost of £115,000 per annum. These assumptions include an average length of stay of 4.6 days and unit cost of £1555, both of which are significantly lower than the Walton figures. Benchmark Data There is limited benchmark data available to assess against the Walton estimate. Average length of stay data has been sourced from the 2006/7 Hospital Episode Statistics (9.6 days), and the ICNARC Case Mix Programme 2007/8 (7.9 days) and average costs have been sourced from the work undertaken by the Programme Management Unit in collaboration with the Welsh Critical Care Networks (£1,564). NB: these costs are based on general ICU cost not neuro critical care costs. That said there are currently no reliable neuro critical care costs for Wales. Mersey and Cheshire Critical Care Network Audit The Mersey and Cheshire Critical Care Network undertook an audit of unmet need for critical care in 2004, which identified that 144 patients with serious traumatic brain injuries were managed on non specialist critical care units. North Wales represents 16% of the activity at the Walton Centre, this would equate to 23 patients. 6 North Wales Transition Board 6th February 2009 North Wales Transition Board Meeting 6th February 2009 . North Wales Critical Care Network Audit The North Wales Critical Care Network undertook a snapshot audit of unmet need for critical care in 2008, which identified that there were 13 transfers to the Walton Centre and 51 patients who remained within the North Wales DGHs intensive Care Units. Not all of these patients in the DGHs would be suitable for transfer, as in some cases the prognosis may be very poor, whilst other patients may have required non-surgical critical care support. If 53%10 of these patients were appropriate for transfer to the Walton Centre (28 patients), there would be an increased cost of approximately £500,000. This is supported by the findings of the networks recent retrospective audit of neurocritical care which identified that an additional 28 patients per annum would benefit from admission to the Walton Centre (annex 2). 10 In the 60% of hospitals that submit data to TARN, only 53% required neurointensive care. 7 North Wales Transition Board 6th February 2009 North Wales Transition Board Meeting 6th February 2009 . Annex 2 NORTH WALES CRITICAL CARE NETWORK Neurocritical Care in North Wales Introduction Following the HCW North Wales Stakeholders Board on the 26th January Ian Langfield from HCW, Sue O’Keeffe Network Manager for the North Wales Critical Care Network and Paul Birch Medical Director of Ysbyty Gwynedd and Chair of the Surgery, Head Injury, Spinal, Critical Care and Radiology sub-group of the Neuroscience Implementation Group have been asked to state the position of neurocritical care in North Wales. The Board have requested an assessment of the impact on the regional ICUs of the proposed increase in funding for neurocritical care at the Walton centre in the context of current demand. They have also been asked to explain the financial impact on the North Wales health community in the context of the Network’s newly developed ‘severely head injured pathway’. Retrospective Neurocritical Care Audit A retrospective audit has recently been undertaken by the Network. The case notes of all acute neuromedical and neurosurgical patients who were cared for in the local DGH units from January 1st 2008 to December 31st 2008 were studied. The audit showed that in total there were 57 neurocritical care patients admitted to local Intensive Care Units (ICU) during the year. Four patients were neuromedical; two were not referred for a neurological opinion but two were referred to and seen by Outreach Consultant Neurologists from the Walton Centre. 52 patients were therefore referred to the Walton Centre for tertiary care. 17 patients were accepted and an additional 28 would have been appropriate for specialist care. The audit highlighted gross inconsistencies of acceptance of patients, most likely due to tertiary capacity. For example, patients with very similar conditions had disparate decisions made. Hospital Total Medical ReferredAccepted 3 6 ReferredRefused 7 14 Wrexham Glan Clwyd 11 23 1 2 (1x not Bangor 23 1 8 14 1 11 Total NW 57 3 4 17 35 4 28 8 referred) Not Referred 0 3 (inc Appropriate 4 13 medical pt) Not Appropriate 3 2 (see not referred) Recommendations: o To note the current volume of neurocritical care referrals to the Walton Centre (>90% of all cases). 8 o To note the amount of patients refused vs. those deemed appropriate. North Wales Transition Board o To2009 note that, in light of NICE guidance, an additional 28 patients should be 6th February cared for in a tertiary centre per annum. North Wales Transition Board Meeting 6th February 2009 . Impact on the Regional Critical Care Units The average length of stay for Welsh patients admitted to the Walton Centre is cited as being 10.9 days. It should be noted that a possible explanation for the comparatively high length of stay at the Walton Centre may be due to the difficulties experienced with repatriation to DGHs in North Wales (the Network identified delays repatriating three patients from Walton totalling 234hrs, in one month). If all 28 patients deemed appropriate for specialist care were transferred to the Walton Centre it could be argued that 305 bed days would be ‘freed up’ per annum. The Network has undertaken extensive work to assess the capacity and demand of the critical care beds in North Wales. During the summer of 2008 patient flow study 580 hours were identified as ‘virtual beds’. This meant that, in one month, as a result of lack of critical care beds patients were cared for outside of an ICU for a total of 580 hours. Extrapolating these figures over a year equates to 290 bed days. These figures alone do not take into account; o Patients who receive alternative management due to lack of critical care beds o Level 2 patients who are cared for on general wards o Premature discharges from critical care due to lack of beds The inference is that even if 100% neurocritical care patients were accepted and transferred to the tertiary centre local units would immediately backfill this capacity with unmet demand and would still be significantly oversubscribed resulting in frequent cancelled operations due to lack of critical care capacity and transfers for non-clinical reasons. The Network has commissioned some specific capacity modelling for North Wales to assess how many additional critical care beds are required and which ICU they are required in. The preliminary results are expected at the end of this week. Recommendations: o To understand the unmet demand of the North Wales critical care units in relation to current capacity. o To recognise that not all neurocritical care patients will be accepted by the Walton Centre due to tertiary capacity or patient appropriateness. o To recognise that capacity created by transfers to Walton will immediately be backfilled by known ‘unmet demand’ o To note that funding additional capacity in Walton, whilst necessary, is an additional cost pressure to the North Wales Health Community (i.e. it cannot be a transfer of resources). 9 North Wales Transition Board 6th February 2009 North Wales Transition Board Meeting 6th February 2009 . Severely Head Injured Pathway In response to the National Institute for Clinical Excellence Clinical Guideline 56 (NICE CG56 2007) ‘Head Injury; Triage, assessment, investigation and early management of head injury in infants, children and adults’ the Network set up a collaborative work group with local Intensivists and colleagues from the Walton Centre. A ‘severely head injured pathway’ has thus been written. Previous criticisms have been levied due to inconsistencies in acceptance of patients for tertiary care. The aim of the pathway therefore is to provide consistency across the North Wales Network region for patients with a severe head injury. It includes a referral pathway, ICU maintenance care and repatriation process for all severely head injured patients from the three hospitals. As can be seen from the retrospective audit, 95% (54 of 57) patients were referred to the Walton Centre i.e. in the last year all neurocritical care patients who should have been referred were referred. The pathway in itself will not therefore increase referrals. It should however improve the referral process for both local clinicians and tertiary Consultants. Because the pathway also includes an evidence based ‘care bundle’ for management of the patients remaining in the local units care of the severely head injured should be enhanced. Any direct financial impact resulting from increased transfers to the Walton Centre (from additional capacity) will be primarily incurred by the Welsh Ambulance Service Trust. Recommendations: o To note that implementation of the ‘severely head injured pathway’ will not increase referrals. o To note that the pathway should improve the referral and repatriation process and maintenance care of the patients who remain in the DGH ICUs. Notes: o There are currently gross inconsistencies in acceptance of neurocritical care patients. Most likely due to the Walton Centre’s critical care capacity. o Funding additional capacity for neurocritical care patients from North Wales is necessary, not only to become compliant with NICE CG56, TARN and the Steers Report but also to improve the outcomes of such patients. o Funding needs to be recognised as an additional cost pressure due to the oversubscription of current North Wales critical care capacity. o The ‘severely head injured pathway’ will not increase referrals but enhance the referral and repatriation process. o The ‘severely head injured care bundle’ will improve the maintenance care of head injured patients who remain in the local ICUs. o Additional capacity in the Walton Centre for North Wales patients may have a financial impact on the Welsh Ambulance Service Trust with a potential increase of 28 transfers per annum. 10 North Wales Transition Board 6th February 2009