The Chronic Care Model_What is It
advertisement

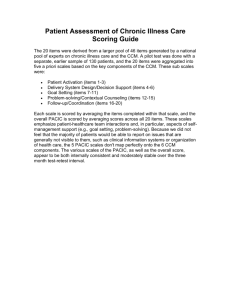
The Chronic Care Model: What is It? The chronic care model (CCM) uses a standardized path to restructuring medical care in a way that builds partnerships between heath systems and communities. The CCM is based on the idea that improvement in care necessitates an approach that incorporates patient, provider, and system-level intervention. CCM has been applied to many chronic conditions including diabetes, congestive heart failure, and asthma. A chronic condition is any that requires ongoing adjustment by the affected person and interactions with the health-care system. Almost half of people have at least one chronic condition. Successful mediations in the care of chronic disease include intricate sets of actions that address psychosocial and lifestyle issues, in addition to physical problems. The CCM model is developed on the belief that improvements in care require an approach that considers patient, provider, and system-level interventions. In any health-care setting, best management of chronic disease and practice improvement must be a priority. Other recommendations for ideal practice include: leadership that is committed and visibly involved; leadership that backs innovation and quality improvement; leadership that develops incentives for providers and patients for better care and to stick to evidence-based practices. Practice leaders must make their expectations clear at all times and provide adequate resources to support chronic care and practice improvement programs. Obviously, practice improvement requires the review of data and trends in individual patients and the practice population. Clinical information systems are organized to include patient, population, and provider data to portray the health of the population and to aid efficient and effective care. The system should include a disease registry that provides information on the population and provider performance of guidelines. In the CCM, this registry might also include a registry regarding patient-specific needs and reminder systems that might generate tailored treatment planning or encounter forms, or provide tailored patient or provider messaging. Delivery system design should allow for appropriate use of all team members, planned patient visits, regular follow-up, and case management. There are seven components of CCM believed to affect functional and clinical outcomes associated with disease management. They are: 1. Health system – organization of health care (ie, providing leadership for securing resources and removing barriers to care) 2. Self-management support – ie, facilitating skills-based learning and patient empowerment. Instead of solving a problem for a patient, the practitioner should teach the patient how to solve problems for themselves. 3. Decision support –ie, providing guidance for implementing evidence-based care. Tools for decision making are often based on information and can include skills such as how to read a food label. 4. Delivery system design – ie, coordinating care processes 5. Clinical information systems – ie, tracking progress through reporting outcomes to patients and providers 6. Community resources and policies – ie, sustaining care by using communitybased resources and public health policies. Coaching the patient to learn to identify, evaluate, and use available resources is an important part of selfmanagement support. Community practice partnerships are especially important with elders, low-income, and underserved individuals. 7. Taking action – this involves readiness to change, sufficient information, goal setting, and ongoing support for change Deficiencies in current care include: Rushed practices not following established practice guidelines Lack of care coordination Lack of active follow-up to ensure best outcomes Patients inadequately trained to manage their illnesses The Robert Wood Johnson Foundation mandated rigorous independent evaluation of the collaborative improvement process and the implementation of the CCM by health systems. In 1999, the RAND corporation and the University of California at Berkeley, in cooperation with the Improving Chronic Illness Care, a national program of The Robert Wood Johnson Foundation, undertook a four-year study of Improving Chronic Illness Care’s three earliest chronic illness care collaboratives, involving 51 participating sites involving almost 4 000 patients with diabetes, congestive heart failure (CHF), asthma, and depression. More than 15 papers were published based on these assessments detailing: Organizations were able to improve, making an average of 48 changes in 5.8 out of 6 CCM areas. Among people with diabetes, cardiovascular risk was significantly reduced. CHF pilot patients were more knowledgeable and more often on recommended treatment with 35% fewer hospital days. Asthma and diabetes pilot patients were more likely to receive appropriate therapy. A year later, care teams reported that 82% of sites had sustained changes and 79% of sites had spread changes to other places or diseases. The example of CCM for diabetes management The Centers for Disease Control (CDC) looked at 16 studies to discern how researchers in the United States have practiced CCM in primary care settings in order to provide improved care for individuals with diabetes and to describe the outcomes of the CCM application. CCM was found to be effective and the following examples of initiation were provided: The original leaders in health-care systems instituted system-level reorganization that improved coordination of care. Disease registries and electronic medical records (EMRs) were used to create patient-centered goals, monitor patient development, and identify negligence in care. Primary care physicians (PCPs) were trained to deliver evidence-based care. PCP office-based diabetes self-management education improved patient outcomes. Specific outcomes of CCM application included: Engaging the governing boards of health-care systems culminated in support for institutionalizing the CCM approach, which was associated with a 1% drop in A1c over a year, as well as improved foot care. Two studies revised the health-care system to reformulate health-care team roles, resulting in improved A1c, blood pressure, cholesterol, and weight. Health-care system reorganization helped to build diabetes self-management training programs that identified and intervened with patients at risk for complications; this improved both clinical and behavioral outcomes. Diabetes self-management education generally improved psychosocial and clinical outcomes. Weekly automated, individualized, phone calls from registered nurses (RNs) are linked to improvement in interpersonal processes of care, physical activity and function, and slightly better metabolic outcomes (ie, A1c, blood pressure, and cholesterol). Use of secure email connection and smartphone apps to upload glucose readings allowed patients to feel more allied with their RN care manager (note that some patients still preferred face-to-face interaction). Computer-based interactive diabetes self-management training modules and toolkits were supported by a “DM passport” or “DM care record” that listed goals, action plans, and labs. Training PCPs on evidence-based guidelines and methods for implementing CCM culminated in improved PCP adherence to clinical guidelines. Training the PCPs led to improved diabetes knowledge among patients and improved A1c and high density lipoprotein (HDL) results. Implementation of the American Diabetes Association’s (ADA’s) Standards of Care and Institute for Clinical Systems Improvement clinical guides increased the number of planned visits solely for diabetes and resulted in improved communication between certified diabetes educators (CDEs), PCPs, and patients. A1cs were improved, patients reported better constancy in medication regimens and adjustment practices, and had stronger support networks in more personalized settings. When diabetes self-management education was provided in PCP offices instead of exclusively in hospitals, two- to three-fold more patients were reached. Collective clinical information systems utilizing disease registries and EMRs allowed multiple providers to review detailed lab and exam results and helped to identify care lapses. References and recommended reading Fiandt K. The chronic care model: description and application for practice. http://www.medscape.com/viewarticle/549040. Accessed December 3, 2015. Improving chronic illness care. Improving Chronic Illness Care website. http://www.improvingchroniccare.org. Accessed December 3, 2015. Stellefson M, Dipnarine K, Stopka C. The chronic care model and diabetes management in US primary care settings: a systematic review. Centers for Disease Control and Prevention website. Prev Chronic Dis 2013;10:120-180. doi:http://dx.doi.org/10.5888/pcd10.120180. The chronic care model. Pittsburgh Regional Health Initiative website. http://www.prhi.org/initiatives/readmissions-reduction/ed-wagners-chronic-caremodel. Accessed December 3, 2015. Contributed by Elaine Hinzey RDN, LD/N Review date: 12/2/15