Black Cohosh Clinical Trial Not Representative of
advertisement

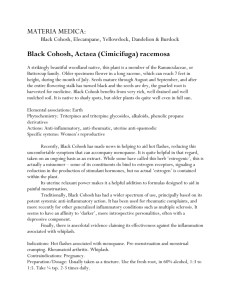
Black Cohosh Clinical Trial Not Representative of Previous Research Showing Positive Results American Botanical Council Clarifies Recent Clinical Trial Date: December 21, 2006 To: Selected ABC Members and Stakeholders From: American Botanical Council A recently-published clinical trial testing the popular herb black cohosh is inconsistent with the positive outcomes for treating menopause symptoms seen in the majority of published clinical trials, says the American Botanical Council. [1] “The medical literature contains many controlled and uncontrolled trials that support the efficacy of the two leading black cohosh preparations for treating menopause symptoms,” said Mark Blumenthal, founder and executive director of ABC, the leading herbal nonprofit research and education organization. Numerous herb experts cautioned that this trial must be seen in context of the entire body of clinical research on black cohosh. According to Mary Hardy, MD, a physician in Los Angeles who has been researching herbal dietary supplements for over a decade, and an expert on black cohosh clinical trials, “This study should not be considered the definitive study on black cohosh. These results should be placed in the context of all of the black cohosh trials -- many of which have shown efficacy for other commercially available products.” Gail Mahady, PhD, an associate professor of pharmacognosy at the University of Illinois, said, “Since 2003 there have been about 10 clinical studies on black cohosh published and all were positive.” Dr. Mahady, one of the principal authors of the black cohosh monograph for the World Health Organization, has reviewed these trials in several journal publications. [2,3] She added, “Thus, one negative study does not neutralize all of the other 10 positive trials.” Dr. Mahady is also currently a co-investigator on an ongoing black cohosh trial funded by the National Institutes of Health (NIH) and the National Center for Complementary and Alternative Medicine (NCCAM) which also funded the recently-published trial. The year-long trial did not show any significant benefit in reducing hot flashes or night sweats for two different black cohosh preparations -- one a black cohosh extract and the other black cohosh with other herbs added -- or a combination of the black cohosh/herbal mixture with an enhanced soy diet. (The authors acknowledged that it was difficult to ensure compliance of the added soy diet for an entire year.) One group of women in the trial used conventional hormone replacement therapy (HRT) but this treatment was terminated after researchers in another trial on HRT discovered adverse cardiovascular and cancer effects associated with the conventional hormones in 2002. Called the Herbal Alternatives for Menopause Trial (HALT), the study, published in the Annals of Internal Medicine on December 19, was a one-year, randomized, double-blind, placebo-controlled, 5arm trial. Researchers at the Center for Health Studies in Seattle assigned 351 women aged 45 to 55 to one of 5 different groups (arms): (1) a black cohosh extract (CimiPure®, produced by Pure World Inc. of Hackensack, NJ), (2) a multi-herb pill with black cohosh and 9 other ingredients* (Progyne, Progena, Albuquerque, NM), (3) the same multi-herb pill plus counseling to ensure the increased consumption of dietary soy, (4) conventional hormone replacement therapy (estrogen with or without progestin; this was terminated before the other arms when the Women’s Health Initiative trials were prematurely halted in 2002 due to observations that HRT actually increased the incidence of cardiovascular disease and cancer), (5) a placebo (dummy pill). The lead researcher was Katherine M. Newton, PhD, of the Group Health Center for Health Studies, Seattle, and the University of Washington, and colleagues. The trial was funded by the National Institute on Aging (NIA) and NCCAM. Criteria for inclusion of the women in this trial consisted of at least 2 or more vasomotor symptoms per day (e.g., hot flashes, night sweats, etc.). Although this study appears to be the longest placebo-controlled trial on black cohosh and one of the largest, there are still some potentially serious limitations, which the trial authors have acknowledged. By dividing the total number of women into 5 groups (arms) to test 4 different therapies (including HRT) against placebo, the number of women in each group drops to a point where the statistical significance of the outcomes (whether positive or negative) are greatly diminished. The authors wrote, “The study was too small to detect small changes in symptom frequency (less than 1.5 hot flashes per day).” [1] Dr. Hardy also noted that “despite the relatively large number of participants, the complex design (5 arms) means that each group had relatively few participants and thus the study was not powered to find any but large effects.” The trial had set a criteria for inclusion at a minimum of 2 hot flashes per day, a relatively low level at which reductions are more difficult to produce and/or monitor in a trial like this (although the actual median level was actually 6). In a corresponding editorial Carol M. Magione, MD, MSPH of the David Geffen School of Medicine in Los Angeles wrote, “Black cohosh is not effective.” – basically relying on this trial as the sole arbiter of the efficacy of black cohosh. [4] Dr. Mangione’s conclusion contrasts with other randomized controlled trials (RCTs) that have shown measurable efficacy for the two most well-researched black cohosh preparations (e.g., Remifemin® and Klymadynon®, both from Germany). At least 15 clinical trials attest to the efficacy of Remifemin (Schaper and Bruemmer, Salzgitten, Germany, imported by Enzymatic Therapy, Green Bay, WI) and 6 do so for Klymadynon® (Bionorica, Neumarkt, Germany, imported by Bionorica USA, Eugene, OR). Several experts noted that some information on this trial has been published previously. According to Dr. Hardy, “This is the second time data from this trial has been reported in the medical literature, so care must be taken not to count this study twice in looking at the whole body of literature.” Referring to the relatively large placebo response in this trial (about 30% of the women on placebo reported beneficial effects, Dr. Hardy stated that “Research in menopausal treatments, besides estrogen, are often confounded by very large placebo effects.” Daniel Fabricant, PhD, Vice-president of Scientific Affairs at the Natural Products Association with a doctorate in Pharmacognosy from the University of Illinois, which is also conducting an NCCAMfunded grant on the same black cohosh extract, said in an email to ABC, "The body of clinical evidence on black cohosh preparations spans more than 3,000 subjects and 50 years using the herbal extract for relief from climacteric (menopausal)/vasomotor symptoms. The weight of the evidence from those studies has been overwhelmingly positive.” Dr. Fabricant also noted that a potentially significant flaw in the trial is the lack of data on secondary trial outcomes in this article: “vaginal cytology; serum lipids (total cholesterol, HDL and LDL cholesterol, triglycerides); bone mineral density (hip and spine dual energy x-ray absorptiometry scan); glucose metabolism (insulin, fasting blood glucose); and coagulation factors (fibrinogen, PAI-1) would all provide valuable information regarding both the botanicals and the risks that have been seen with conjugated equine estrogens (CEE) in previous studies.” Another question about the study was raised by Francis Brinker, ND, of the University of Arizona Program for Integrative Wellness and author of several highly-regarded reference books on herbal medicine, including Herb Contraindications & Drug Interactions 3d ed. Dr. Brinker states, “I do not have a problem with acknowledging the negative outcome, but I reject the extrapolation of the results to all forms of black cohosh products. The more medical (and herbal) minds are challenged on this sort of lazy assumption, the sooner they'll recognize legitimate distinctions among various herbal preparations and their effects. Not all products from the same herb are created equal, so we shouldn't blame, say, Peter Cohosh for the failings of Paul Cohosh (or reward Peter for Paul's success), unless there is some good evidence for bioequivalency” -- the ability to show that one preparation has the same physiological effect as another. That has not been demonstrated in this trial, so it is not possible to extend the results of this trial to other clinically tested black cohosh products. Dr. Brinker also commented that the extract studied in this trial was a daily dose of 160 mg of a 70% ethanolic extract, whereas the positive studies with Remifemin tablets used 40 mg daily of a 40% isopropanolic extract. Eckehard Liske, PhD, research director at Schaper & Bruemmer, the German company that manufacturers and markets Remifemin, the most clinically-researched black cohosh product, observed that the black cohosh product used in this trial did not appear to have met stability testing that should have been required of any herbal substance that was being employed for a 12-month trial. “The primary packaging does not protect the study medication as well as a blister packaging,” he wrote. This was acknowledged by the trial authors in their writing that they were not able to detect several characteristic [chemical] marker substances. Thus, this absence of blistered medication, according to Dr. Liske, suggests a possible instability of the study medication (i.e., the black cohosh extract may have degraded in some manner over time). Fredi Kronenberg, PhD, professor of clinical physiology at Columbia University College of Physicians and Surgeons, an expert in menopause, and author of a review paper on complementary and alternative approaches to menopausal symptoms, [5] cautions that in science one must look at the whole body of research in a field. “This study,” she said, “must be considered in the context of the other studies over years of research on black cohosh, the majority of which have positive outcomes. The study was as well designed, if not better than some others. It has a negative outcome on hot flash frequency. But each study uses slightly different populations of women, some only postmenopausal women, some, like this study, examining both menopausal and peri-menopausal women. Half of the women in this study were peri-menopausal – with estrogen levels still fluctuating and thus impacting hot flashes. While the investigators did control for this in their analysis, it points out the challenges for interpreting results across studies.” Dr. Kronenberg, who is also a Trustee of ABC, continued, “Of critical importance when reviewing black cohosh studies is that we know little about how the different extraction techniques of black cohosh preparations and resulting formulations may impact hot flash physiology. The extract in this study was an ethanolic extract. There have been positive studies with both ethanolic and isopropanolic black cohosh extracts. We are in a phase of poorly funded research, so we must accumulate the results of many relatively small studies since we do not have any large studies underway at this time. The media does a disservice to the public by using catchy headlines and not taking the time for the in-depth analysis so needed in reporting on what are complex issues.” In sum, Dr. Fabricant emphasized, “This new study should not be called conclusive by any stretch.” About Black Cohosh Black cohosh, also known by either its scientific names (Actaea racemosa and Cimicifuga racemosa) is a member of the buttercup family (Ranunculaceae) and is native to the Eastern United States. The roots and rhizomes (lateral roots) of the herb have a long history of traditional use by native American tribes to deal with genitourinary complaints in women. An isopropanolic extract of black cohosh (Remifemin®) has been used in German clinical practice since the mid-1950s with safe and effective results, and black cohosh preparations have been approved by the German government as safe and effective nonprescription medications for treatment of menopausal symptoms. [6] In the past few years black cohosh has become increasingly popular as the most widely-used natural alternative to hormone replacement therapy (HRT). The herb’s popularity with middle-aged women and gynecologists grew significantly after the summer of 2002 when a large-scale governmentsponsored clinical trial on HRT was halted prematurely after evidence that HRT was responsible for an increase in cancer and cardiovascular disease in menopausal women. Black cohosh preparations ranked eighth of all single-herb supplements sold in mainstream retail outlets in 2005, according to data from Information Resources in Chicago as reported in the new issue of HerbalGram (#71), ABC’s quarterly journal.[7] * Ingredients in :Progyne: Black cohosh, alfalfa (Medicago sativa), boron citrate, chaste tree (Vitex agnus-castus), dong quai (Angelica sinensis), false unicorn root (Chaemelirium luteum), licorice root (Glycyrrhiza glabra), oat straw (Avena sativa), pomegranate (Punica granatum), “Siberian ginseng” (Eleutherococcus senticosus) References 1. 2. 3. 4. 5. 6. 7. Newton KM, Reed SD, Lacroix AZ, Grothaus LC, Ehrlich K, Gultinan J. Treatment of vasomotor symptoms of menopause with black cohosh, multibotanicals, soy, hormone therapy or placebo: A randomized trial. Ann Intern Med 2006;145:869-879. Mahady GB, Doyle B, Locklear T, Cotler S, Guzman-Hartman G, Krishnaraj R. Black cohosh (Actaea racemosa) for the mitigation of menopausal symptoms: recent developments in clinical safety and efficacy. Women’s Health 2006;2;773-783. Mahady GB. Black cohosh (Actaea/Cimicifuga racemosa): review of the clinical data for safety and efficacy in menopausal symptoms. Treat Endocrinol. 2005;4(3):177-184. Mangione CM. A randomized trial of alternative medicines for vasomotor symptoms of menopause [editorial]. Ann Intern Med 2006;145:924-925. Kronenberg F, Fugh-Berman A. Complementary and alternative medicine for menopausal symptoms: A review of randomized controlled trials. Ann Intern Med. 2002;137:805-813. Blumethal M, Busse WR, Goldberg A, Gruenwald G, Hall T, Riggins CW, Rister RS (eds.). Klein S, Rister RS (trans.). The Complete German Commission E Monographs – Therapeutic Guide to Herbal Medicines. Boston: Integrative Medicine Communications; Austin: American Botanical Council, 1998. Blumenthal M, Ferrier GKL, Cavaliere C. Total sales of herbal supplements in the United States show steady growth. HerbalGram. 2006;71:64-66.