File - Krista Winchester
advertisement
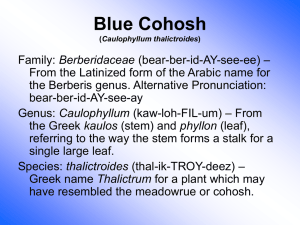
Running header: HOT FLASH: BLACK COHOSH USE DURING MENOPAUSE Hot Flash: Black Cohosh Use During Menopause Loretta de Guzman, Lacou Flipse, Cecilia Garcia, Amanda Larson, Nadiya Tolstikhina & Krista Winchester DFM 655 October 30, 2014 1 HOT FLASH: BLACK COHOSH USE DURING MENOPAUSE 2 Introduction Menopause occurs when a year has passed since a woman’s final menstrual cycle. This change can be accompanied by many symptoms including night sweats, hot flashes, and mood changes, which vary greatly in their intensity and longevity. The typical protocol used in the past to minimize these symptoms, a combination of estrogen and progesterone as hormone replacement therapy, were found to increase cancer and cardiovascular disease risk (Hormone Therapy, 2012), and are no longer the standard treatment. Many women opt for alternative “natural” treatments, like black cohosh, an herb sold as a dietary supplement, to treat their menopausal symptoms. As dietary supplements do not undergo the same rigor as medications regulated by the Food and Drug Administration (FDA), the long-term safety and efficacy of black cohosh may be a concern for those taking the herb to relieve uncomfortable symptoms. History and Description Black cohosh is the common name for Actaea racemosa a member of the buttercup family of herbs and shrubs. Black cohosh is a perennial plant native to North America (Pengelly & Bennett, 2011). The black roots are made up of thick gnarled rhizomes. The roots are the source of the plant’s medicinal value and have been used for hundreds of years. “Cohosh” translates to “rough” in the Native American language spoken by the Algonquin people. The plant’s gnarled, rough, and dark roots give it the name black cohosh when translated to English (Leung, 1996). Traditionally, Native Americans used the roots of the black cohosh plant to treat a variety of ailments ranging from gynecological to snake bites (Pengelly & Bennett, 2011). At the turn of the century, early Americans’ use of black cohosh as a remedy for childbirth and menstruation was similar to the use of Native Americans (Pengelly & Bennett, 2011). Black HOT FLASH: BLACK COHOSH USE DURING MENOPAUSE 3 cohosh grew in popularity as part of Lydia E. Pinkham’s vegetable compound used by women to ease “all those painful complaints and weaknesses so common to our best female population” (Geller & Studee, 2005). Beginning in the 1940’s, Germany has used and studied black cohosh for the treatment of premenstrual, menstrual, and menopausal neurovegetative symptoms (Lieberman, 1998). In America, Europe, and China, black cohosh has been consumed for centuries to treat hypotension (Lieberman, 1998). Uses and Doses The use of black cohosh has been common throughout the world to treat a variety of ailments over time. Native Americans used it to treat malaise, gynecological disorders, kidney disorders, malaria, rheumatism, sore throat, colds, cough, constipation, and hives (U.S. Department of Health and Human Services, 2008). Black cohosh was used in 19th century America for rheumatism, fever, as a diuretic, and for problems associated with women’s reproductive organs (HHS, 2008). Black cohosh is currently utilized as an alternative medicine to help alleviate menopausal symptoms. It is specifically used to help prevent or reduce the severity and occurrence of hot flashes commonly experienced during menopause (Johnson & Fahey, 2012). The historical and modern doses of black cohosh remain under debate as there is a lack of documentation. In the early 20th century, pharmacist John Uri Lloyd determined that the recommended dose was 1-30 drops (one drop equaling 65mg) of fresh black cohosh root, soaked in a 50% alcohol solution for 10 days (Johnson & Fahey, 2012). Lloyd did not specify in his research the period of time in which individuals may ingest the herb before any harmful side effects may surface. Currently, there is not a universally agreed upon dose for the herb, as it is HOT FLASH: BLACK COHOSH USE DURING MENOPAUSE 4 still being tested in clinical trials. Two clinical studies comprised of 244 and 304 postmenopausal patients in Germany found significant improvement in climacteric symptoms associated with menopause and the ingestion of black cohosh (Wuttke et al., 2014). The herb administered in the trials contained two 20 mg pills, with a concentration of 4-8 mg of black cohosh extract (Wuttke et al., 2014). Contrarily, two clinical studies conducted in the United States of America yielded negative results (Wuttke et al., 2014). The main difference between the German and American studies was the dose of black cohosh administered. In the American trials, up to 200 mg of black cohosh was used in the study (Wuttke et al., 2014). According to various clinical studies, the dose of black cohosh could play a key role in its effectiveness. Scientific Research The effectiveness and safety of black cohosh as an alternative treatment to hormone replacement therapy (HRT) is still under exploration. The first area of interest with an herbal remedy is whether it is effective in treating the symptoms, in this case hot flashes and night sweats. In a randomized, double-blind, clinical trial of over 300 women assigned various herbal remedies, HRT, or a placebo, and surveyed at 3, 6, 9, and 12 months, there were no significant differences in the menopause symptoms of those receiving herbal remedies compared to the placebo (Newton et al., 2006). The one exception in the herbs was found in the 80 women in the black cohosh group, who at 3 months “had 0.38 less night sweat per day than the placebo” (Newton et al., 2006). In another randomized, double-blind, clinical trial of 84 postmenopausal women, Mohammad-Alizadeh-Charandabi, Shahnazi, Nahaee, and Bayatipayan (2013) found there was a statistically significant reduction in menopausal symptoms for those taking black cohosh when compared to the control group. This study was shorter in duration, lasting only 8 HOT FLASH: BLACK COHOSH USE DURING MENOPAUSE 5 weeks with results collected at 4 and 8 weeks. The evidence supporting the effectiveness of the treatment continues to be inconclusive due to conflicting results from trials. Several findings have suggested that black cohosh has a systemic “estrogen-like” effect on some menopausal symptoms. However, black cohosh has a broad range of components that are complex, including triterpene glycosides, but does not include any of the classic phytoestrogens (Viereck, Emons, & Wuttke, 2005). A study at the University of Illinois at Chicago illustrated that black cohosh roots and rhizomes do not contain any compounds that serve as ligands for the estrogen receptors (Betz, et al. 2009). Viereck, Emons and Wuttke (2005) compared clinical studies between phytoestrogens, particularly isoflavones, and black cohosh in treatment of hot flashes, night sweats and psychic problems like mood swings and brain fog. The trials they reviewed suggested that a diet rich in phytoestrogens, found only in whole food products and not isolated phytoestrogens, reduced the risk of these symptoms. The participants reported only a minor reduction of symptoms. In contrast, postmenopausal women who took 40 mg of isopropanolic extract of black cohosh showed significant improvements in hot flushes, night sweats and psychic problems compared to placebo in the two randomized trials they reviewed (Viereck, Emons & Wuttke, 2005). It was determined and confirmed by Betz et al. (2005), that black cohosh increases the response of the gene for tyrosine hydroxylase, which is involved with dopamine in hot flushes. The study was able to verify only one clear association but was not able to determine how black cohosh improves the other symptoms. “Natural” remedies are perceived as safe by many consumers, unfortunately, there is lack of definitive opinion on the safety of herbal remedies. Joy, Joy, and Duane (2008) reported on two cases of liver toxicity related to the use of black cohosh. One woman was admitted with a HOT FLASH: BLACK COHOSH USE DURING MENOPAUSE recurring headache and the other woman was admitted with a 2-week history of epigastric pain, although both women had normal lab and physical examination results. Following abnormal liver tests, and upon further questioning, it was revealed that both women self-medicated with black cohosh. Both were advised to discontinue use and a week later were found to be asymptomatic with normalized liver function (Joy, Joy, & Duane, 2008). Because black cohosh has been reported to cause liver damage in rare cases, taking it with other substances that can affect the liver, such as alcohol and medications like NSAIDs, hormones, blood thinning medications, pain killers, and antidepressants may increase risk (Black Cohosh - Oral, 2014). Discussion The recent studies related to black cohosh efficacy to reduce climacteric complaints revealed controversial findings. In a one year randomized, double-blind, placebo-controlled study in the U.S., Newton et al. (2006), found insignificant effects of black cohosh on menopausal symptoms compared to the placebo. In a separate randomized, double-blind, placebo-controlled 8-week trial conducted in Iran by Mohammad-Alizadeh-Charandabi et al. (2013), there was noticeable decrease of vasomotor, psychiatric, and physical symptoms as well as increase of libido in postmenopausal women. In a review of clinical trials of black cohosh on climacteric complaints, Viereck, Emons and Wuttke (2005) found that three of the studies showed evidence of reducing manifestations of hot flushes, night sweats and psychic disorders. A group of postmenopausal women with breast cancer failed to show improvement, which was believed to be caused by parallel treatment with Tamoxifen (Viereck, Emons & Wuttke 2005). Efficacy of black cohosh on postmenopausal symptoms seems to depend on a variety of factors, such as dosage, length of treatment, interaction with other herbs and drugs, and even the 6 HOT FLASH: BLACK COHOSH USE DURING MENOPAUSE 7 type of plant. A higher dose of 160 mg administered in the study by Newton et al. (2006) was less effective compared to lower doses of 40mg in the study conducted by Viereck, Emons and Wuttke (2005), the 6.5 mg given by Mohammad-Alizadeh-Charandabi et al. (2013) in their trial, or the studies in Germany which also used small doses (Wuttke et al., 2014). Short length of treatment (8 to 12 weeks) with black cohosh demonstrated better outcomes than its long term (1 year) administration (Betz et al., 2009). Liver toxicity was reported as a result of black cohosh intake, but it might be caused by other factors such as alcohol or drug intake (Betz et al., 2009). Even type of plant might play a role in the reduction of symptoms. American and Asian black cohosh herbs look different (Wuttke et al., 2014), and their efficacy in reducing postmenopausal psycho-vegetative symptoms may vary. Conclusion There is a growing body of evidence that suggests black cohosh may have a wide array of therapeutic benefits including reduction of menopausal symptoms. Currently, there is contradicting information as to the best way to measure effectiveness, length of treatment, and which dose is most appropriate in treating menopause symptoms with black cohosh, while avoiding unwanted side effects. This lack of balance between efficacy and documented science is the crux of the problem faced by practitioners when cautiously recommending black cohosh. The fact remains that humans have been self-medicating long before clinical trials and FDA approval and regulation. As a patient, it is important to understand treatments, and how supplements may interact with existing medications. Health is a personal responsibility and whether it be an approved pharmaceutical or natural remedy the individual must be allowed to make informed decisions. HOT FLASH: BLACK COHOSH USE DURING MENOPAUSE 8 Resources Betz, J. et al. (2009). Black cohosh: Considerations of safety and benefit. Nutrition Today, 44(4), 155-162. Geller, S., & Studee, L. (2005). Botanical and Dietary Supplements for Menopausal Symptoms: What Works, What Does Not. Journal of Women's Health, 14(7), 634-649. Johnson, T. L. & Fahey, J. W. (2012). Black cohosh: coming full circle? Journal of Ethnopharmacology, 141, 775-779. Retrieved October 25, 2014, from http://0www.sciencedirect.com.opac.sfsu.edu/science/article/pii/S0378874112002127 Joy, D., Joy, J., and Duane, P. (2008). Black cohosh: a cause of abnormal postmenopausal liver function tests. Climacteric, 11(1), 84-88. Retrieved October 22, 2014, from http://www.luminpdf.com/files/6438754/28444671.pdf Leung, A., & Foster, S. (1996). Encyclopedia of common natural ingredients used in food, drugs, and cosmetics (2nd ed.). New York: Wiley. Lieberman, S. (1998). A review of the effectiveness of Cimicifuga racemosa (black cohosh) for the symptoms of menopause. Journal of Women’s Health, 7. Retrieved October 23, 2014, from http://0 web.a.ebscohost.com.opac.sfsu.edu/ehost/pdfviewer/pdfviewer?sid=c528034a-a752-4ecf81f3-fbb43befa218%40sessionmgr4005&vid=1&hid=4206 MayoClinic.org. Hormone Therapy: Is it right for you? (2012). Retrieved October 29, 2014, from http://www.mayoclinic.org/diseases-conditions/menopause/in-depth/hormonetherapy/art-20046372 MedicineNet.com. Black Cohosh - Oral (2014). Retrieved October 22, 2014, from http://www.medicinenet.com/black_cohosh-oral/article.htm Mohammad-Alizadeh-Charandabi, S., Shahnazi, M., Nahaee, J., and Bayatipayan, S. (2013). Efficacy of black cohosh (Cimicifuga racemosa L.) in treating early symptoms of menopause: a randomized clinical trial. Chinese Medicine, 8(20). Retrieved October 22, 2014, from http://www.cmjournal.org/content/8/1/20#abs Newton, K.M., et al. (2006). Treatment of Vasomotor Symptoms of Menopause with Black Cohosh, Multibotanicals, Soy, Hormone Therapy, or Placebo: A Randomized Trial. Annals of Internal Medicine, 145(12), 869-W244. Retrieved October 22, 2014, from http://0-web.a.ebscohost.com.opac.sfsu.edu/ehost/pdfviewer/pdfviewer?sid=140b64a70b54-4070-a8e6-022140c37bcf%40sessionmgr4002&vid=1&hid=4204 Pengelly, A., and Bennett, K. (2011). Appalachian Plant Monographs. Frostburg State University. Retrieved October 26, 2014, from http://www.frostburg.edu/fsu/assets/File/ACES/actaea racemosa- final(1).pdf HOT FLASH: BLACK COHOSH USE DURING MENOPAUSE U.S. Department of Health and Human Services, National Institutes of Health. (2008). Black cohosh: Fact sheet for health professionals. Retrieved October 25, 2014, from http://ods.od.nih.gov/factsheets/BlackCohosh-HealthProfessional/#h4 Viereck, V., Emons, G., and Wuttke, W. (2005). Black cohosh: Just another phytoestrogen? Trends in Endocrinology & Metabolism, 16(5), 214-221. Retrieved October 23, 2014 from http://www.sciencedirect.com.opac.sfsu.edu/science/article/pii/S1043276005000974 Wuttke, W. et al. (2014). The non-estrogenic alternative for the treatment of climacteric complaints: Black cohosh (Cimicifugia or Actaea racemosa). Journal of Steroid Biochemistry and Molecular Biology, 139, 302-310. Retrieved October 25, 2014 from http://0-www.sciencedirect.com.opac.sfsu.edu/science/article/pii/S0960076013000381 9