Pregnancy, Parturition, Dystocia Pregnancy Gestation length
advertisement
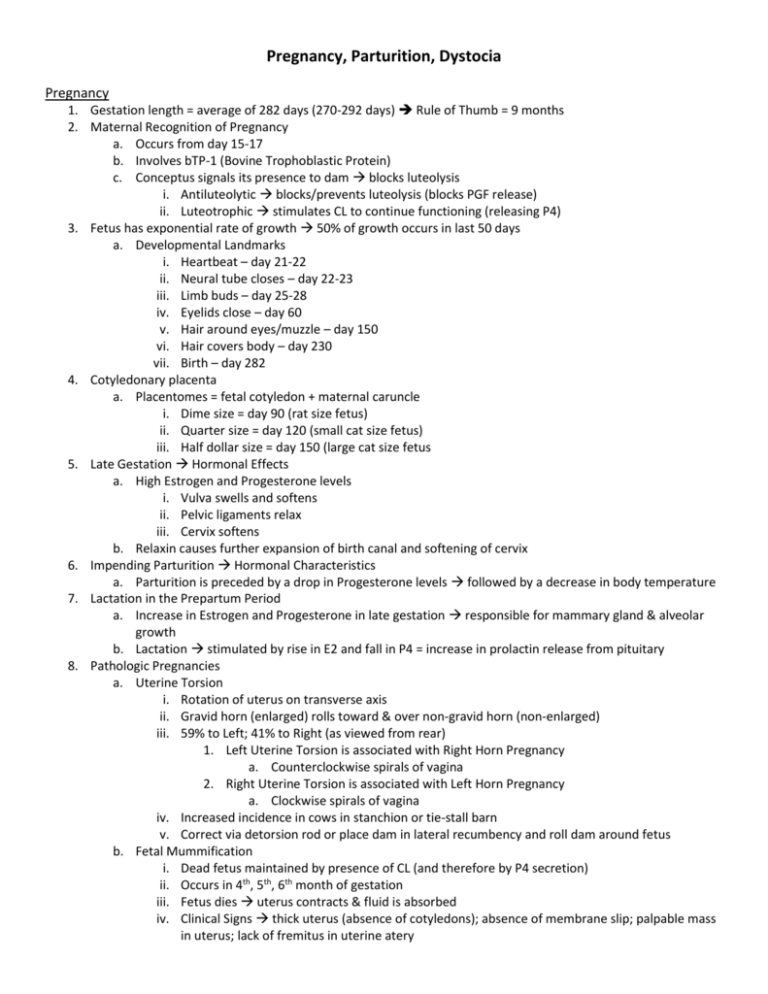
Pregnancy, Parturition, Dystocia Pregnancy 1. Gestation length = average of 282 days (270-292 days) Rule of Thumb = 9 months 2. Maternal Recognition of Pregnancy a. Occurs from day 15-17 b. Involves bTP-1 (Bovine Trophoblastic Protein) c. Conceptus signals its presence to dam blocks luteolysis i. Antiluteolytic blocks/prevents luteolysis (blocks PGF release) ii. Luteotrophic stimulates CL to continue functioning (releasing P4) 3. Fetus has exponential rate of growth 50% of growth occurs in last 50 days a. Developmental Landmarks i. Heartbeat – day 21-22 ii. Neural tube closes – day 22-23 iii. Limb buds – day 25-28 iv. Eyelids close – day 60 v. Hair around eyes/muzzle – day 150 vi. Hair covers body – day 230 vii. Birth – day 282 4. Cotyledonary placenta a. Placentomes = fetal cotyledon + maternal caruncle i. Dime size = day 90 (rat size fetus) ii. Quarter size = day 120 (small cat size fetus) iii. Half dollar size = day 150 (large cat size fetus 5. Late Gestation Hormonal Effects a. High Estrogen and Progesterone levels i. Vulva swells and softens ii. Pelvic ligaments relax iii. Cervix softens b. Relaxin causes further expansion of birth canal and softening of cervix 6. Impending Parturition Hormonal Characteristics a. Parturition is preceded by a drop in Progesterone levels followed by a decrease in body temperature 7. Lactation in the Prepartum Period a. Increase in Estrogen and Progesterone in late gestation responsible for mammary gland & alveolar growth b. Lactation stimulated by rise in E2 and fall in P4 = increase in prolactin release from pituitary 8. Pathologic Pregnancies a. Uterine Torsion i. Rotation of uterus on transverse axis ii. Gravid horn (enlarged) rolls toward & over non-gravid horn (non-enlarged) iii. 59% to Left; 41% to Right (as viewed from rear) 1. Left Uterine Torsion is associated with Right Horn Pregnancy a. Counterclockwise spirals of vagina 2. Right Uterine Torsion is associated with Left Horn Pregnancy a. Clockwise spirals of vagina iv. Increased incidence in cows in stanchion or tie-stall barn v. Correct via detorsion rod or place dam in lateral recumbency and roll dam around fetus b. Fetal Mummification i. Dead fetus maintained by presence of CL (and therefore by P4 secretion) ii. Occurs in 4th, 5th, 6th month of gestation iii. Fetus dies uterus contracts & fluid is absorbed iv. Clinical Signs thick uterus (absence of cotyledons); absence of membrane slip; palpable mass in uterus; lack of fremitus in uterine atery v. Treat with prostaglandins fetus should be expelled in 48-72 hours 1. 90-95% will be expelled with 2 treatments c. Fetal Maceration i. Can occur at any stage of gestation ii. Fetal death with partial cervical dilatation 1. Open cervix leads to uterine contamination (uterine contents contaminated also) iii. Clinical Signs abdominal straining; foul, fetid vulvar discharge; fever; anorexia; drop in milk production; distended, swollen fetus iv. Treat by removing fetus (if cervix is partially to fully dilated) 1. If cervix is closed give prostaglandin v. Poor future reproductive prognosis ( endometrial damage is usually extensive) d. Hydrops Conditions (Allantois & Amnion) i. Prognosis is poor for survival (due to systemic shock & high incidence of retained placenta) ii. Allantois vast majority (90%) 1. Associated with diseased uterus 2. Occurs late in gestation 3. Characterized by rapid abdominal enlargement 4. Difficult to palpate fetus or placentomes (due to uterine turgidity) iii. Amnion 10% of cases 1. Associated with genetically or congenitally defective fetus 2. Characterized by slowly developing abdominal enlargement 3. More flaccid uterus fetus and placentmes more easily palpable (than in w/ allantois) e. Prolonged Gestation never results in normal calf i. Homozygous recessive autosomal gene Holstein & Ayshires 1. 20-90 days past normal gestation length 2. Calves have marked adrenal insufficiency ii. Autosomal recessive in Guernseys 1. Hydrocephalus,cyclopia with aplasia of anterior pituitary iii. Iatrogenic causes 1. Decapitation of fetus 2. Administration of progesterones/progestogens 3. Vitamin A deficiencies f. Fetal Emphysema i. Associated with prolonged dystocias (greater than 24 hours) ii. Fetus dies at or near parturition organisms from vagina invade uterus/fetus = emphysema iii. Treatment fetotomy, C-section; traction on fetus Parturition 1. Stage 1 2-6 hours (preparation of fetus & dam for birthing process) a. Initiation of myometrial contraction Removal of P4 block i. ↑ pressure ↑ fetal ACTH ↑ fetal cortisol 1. Removal of myometrial “P4 block” contractions 2. ↑ reproductive tract secretions b. Uterine contractions irregular to regular c. Rotations of fetus (into proper Presentation, Position, Posture – hopefully) i. Anterior longitudinal, dorso-sacral, head/neck/forelimbs extended d. Dilation (softening) of cervix due to relaxin e. Relaxation of pubic symphysis due to relaxin f. Chorioallantois evagination into cervix & ruptures (provides lubrication) signals end of Stage I 2. Stage 2 ½ - 1 hour a. Fetus is forced through the birth canal via active uterine & abdominal contractions i. Modulated by oxytocin release b. Amnion ruptures c. Fetus is delivered end of Stage 2 3. Stage 3 2-12 hours a. Chorionic villi loosen and detach b. Afterbirth is shed end of Stage 3 4. Normal a. Presentation – relationship of fetal spine to maternal spine i. Longitudinal – spines aligned parallel (anterior = head; posterior = rump) ii. Transverse – spine perpendicularly aligned iii. Normal Presentation Anterior Longitudinal b. Position – relationship of fetus dorum to pelvic quadrants (longitudinal presentation) i. Dorso-sacral ii. Left/right dorso-ilial iii. Left/right dorso-pubic (dorso-pubic is completely upside down – 180° rotation = RARE) iv. Normal Position Dorso-Sacral c. Posture – refers to position of fetus only i. Extremities may be flexed, extened, retained ii. Normal Posture head, neck forelimbs extended 5. Induction of Parturition save dam or calf; prevent dystocia; prevent excessive udder edema; truncate calving season a. Long acting corticosteroids i. IM injection ~1 month prior to calving parturition 4-26 days afterwards ii. Preexisting health conditions may be exacerbated iii. Incidence of RFM is low iv. High incidence of calf mortality b. Short acting corticosteroids i. IM injection 2 weeks prior to calving ii. Parturition 24-72 hours afterwards iii. No increase in calf mortality if within 2 weeks iv. Increased incidence of RFM c. Prostaglandins similar to short acting corticosteroids d. Estrogens “old methods” with poor efficacy i. Can be combined with corticosteroids (does not decrease RFM) Dystocia 1. Etiologies a. Hereditary i. Abnormal genital tract (persistent hymen); twinning; increased fetal head size (fetal monsters & hydrocephalus); prolonged gestation; mummified fetus; double muscling; ankylosed joints b. Nutritional Management i. Decreased pelvic size of dam; fat in pelvic cavity (“fat cow syndrome” due to overfeeding) c. Uterine Inertia dam isn’t efforting; due to the primary weakness or absence of: i. myometrial contractions: may be due to myometrium’s inability to respond to hormonal stimuli or to a reduction in the level of these hormones ii. incomplete dilation of the cervix: this may be brought about by inadequate preparation with estrogen and relaxin. This frequently happens during premature births or abortions before estrogen and relaxin have reached optimal levels iii. secondary weakness or absence of myometrial contractions: develops when an obstructive dystocia has existed for an abnormally long time and has resulted in exhaustion of the myometrium and abdominal musculature d. Displacement of gravid uterus i. Pathological displacement of the uterus may arise when movement occurs around its longitudinal axis (uterine torsion) or about its transverse axis (ventroflextion of the uterus) ii. Clinical signs of Uterine torsion: animal may behave normally or it may show colicky pains (kicking at abdomen). The vulva or perineum may appear sunken. The cow may stand with the tail elevated and exhibit a variable degree of straining. iii. Clinical signs of Ventroflexion: a dropped abdomen and a sunken vulva are prominent signs, abdominal straining is generally absent e. Fetopelvic Disproportion i. a dystocia caused by a disparity in size between the fetus and maternal pelvis, when the cervix is fully dilated and vagina and vulva are relaxed ii. divided into several entities: Absolute fetal oversize, Small maternal pelvis, Narrow birth canal iii. Clinical signs: Strong and continuous but unproductive straining, Vaginal passage is found to be dry, Difficult to distinguish fetopelvic disproportion from ineffective labor after the intrauterine fluids have been lost and uterine contractions and abdominal straining are weak or absent f. Constriction of Vulva, Vestibulum, and Vagina i. Caused by: Insufficient relaxation of the perineal area, Underdevelopment of the posterior birth canal, Narrowing of the vestibulum due to a persistent, overdeveloped hymenal ring, Fibrosis due to injury at a previous parturition, Incorrect treatment of severe vaginitis ii. Clinical signs: labor may be strong initially and it is obvious that the expulsion stage has commenced, the fetal feet may be visible at the vulva but further progress is arrested at this point, the perineum may bulge excessively g. Deformities of the Birth Canal i. Congenital and acquired deformities in the pelvis, cervix, vagina, or vulva may lead to dystocia by altering the shape and volume of the birth canal ii. Deformities of the Osseous Pelvis: -a reduction in size of the pelvic inlet may be caused by extensive callus formation in healed fractures -dislocation of the sacroiliac joint with downward displacement of the sacrum results in the permanent reduction in the vertical pelvic diameter iii. Congenital Deformities of the Genital Tract: -remnants of the Mullerian ducts may occasionally be strong enough to cause dystocia -double cervix has been reported in cows which have given unassisted birth to live calves -a persistent hymen occasionally permits conception, but causes dystocia iv. Neoplasia of the Genital Tract: -most neoplasms do not greatly impede fertility, but they may cause dystocia in several ways -lymphatic tissue neoplasia of the uterus causes reduced elasticity in the uterine wall and ineffective myometrial contractions -other tumors can obstruct the birth canal -vaginal granulomas and squamous cell epitheliomas of the vulva cause little interference h. Death and Decomposition of the Fetus during Parturition i. The bovine fetus may die 3 to 12 hours after the onset of the expulsion stage of parturition. When death occurs before correct fetal alignment is attained this may cause a dystocia or aggravate an existing one. ii. Parturient deaths are mainly due to: Anoxia, Congenital defects, Trauma during prolonged parturition iii. Clinical signs: thin, foul-smelling, sanguineous vaginal discharge, or a strand of discolored fetal membranes hanging from vulva, dam appears dull and may strain intermittently i. Fetal Malformation i. Caused by abnormal development of the conceptus during the embryonic period ii. May be attributed to: genetic causes, infection, nutritional deficiencies, toxic substances iii. Clinically all malformations can be iv. divided into three major groups: (1) malformations characterized by fetal dropsy (2) malformations characterized by deformity or absence of fetal parts (3) malformations characterized by multiplication of fetal parts 2. Abnormal Presentation, Position, Posture 3. 4. 5. 6. a. Normal Anterior Longitudinal - Dorso-Sacral - Head, Neck, Forelimb Extension b. Abnormal Anterior Presentations i. Carpal flexion ii. Partial elbow flexion hooves at level of fetal muzzle instead of well beyond iii. Shoulder flexion iv. Lateral deviation of head/neck v. Ventral displacement of head c. Posterior Presentations (abnormal by definition) i. Hock flexion ii. Bilateral hip flexion Dystocia in Heifers vs Cows: a. In Heifers: i. A heifer is still growing, so she will be smaller than a mature cow. ii. Also a heifer has never had a calf before, so the tissues of the birth canal (cervix, vagina, and vulva) have not ever been dilated. iii. Thus, dystocia in heifers is often due to the birth canal not dilating or stretching sufficiently. b. In Cows: i. When dystocia occurs in cows however, it is usually the result of a more serious problem. ii. The size of their birth canal is less restrictive than that of a heifer so when dystocia occurs there may commonly be another disease process going on (i.e. Milk Fever), the calf is extremely large, or the calf is malformed or malpositioned. iii. For these reasons even mild dystocia in a cow may increase the likelihood of a stillbirth and live calves may be more significantly compromised than those born to a heifer with dystocia. OB equipment a. Wire introducer, (2) 60” obstetrical chains, 3 obstetrical chain handles; fetal extractor; fetotome; Krey hook; 2 wire handles; 2 blunt eye hooks; detorsion rod; fetotomy knife; obstetrical wire; sleeve; lubricant Approach to correction a. Rectal exam first clean out feces – then vaginal exam b. Mutation return fetus to normal presentation, position, posture i. Repulsion – push fetus out of pelvic cavity and into abdominal cavity ii. Rotation – turn fetus on long axis into dorso-sacral position iii. Version – rotation of fetus on its transverse axis iv. Limb extension (most frequently done) 1. Repulsion of proximal limb 2. Lateral rotation of medial portion 3. Traction of distal limb c. Forced extraction do not use excessive force i. Indications uterine inertia; post mutation correction; large fetus; posterior presentation; to avoid fetotomy ii. Chain placement 1. 2 loops one above and one below fetlock (will prevent fracture of limb) 2. Around neck of DEAD fetus ONLY!! iii. Procedure 1. 3-point traction; dorsal and posterior – first direction; ventral and posterior – second direction after head is at vulva; alternate traction on limbs; rotate fetus 30° before fetal pelvis enters maternal pelvic cavity (to prevent hiplock) d. Following Correction i. Examine uterus for additional fetuses ii. Examine uterus for tone iii. Examine birth canal for lacerations Step by Step Assisting Malpresentation: a. Anterior Presentation: i. first the head needs to be brought into the pelvis ii. the legs must be straightened before the head is brought into the pelvis iii. to avoid shoulder block, pull legs alternately a few inches at a time using OB chains; one leg is usually 6 inches in front of the other iv. shoulder block occurs when traction is applied to both legs at the same time v. after the shoulders are delivered, rotate the fetus into partial dorso-ileal position to facilitate passage of the hips and stifles vi. rotation must take place while the fetal lumbar area is at the dams pelvic inlet vii. hip block occurs from failure to rotate calf during delivery -proper rotation of hips to 90 degrees maximizes pelvic space available viii. the calf should be rotated as soon as the head is outside the vulva ix. calf should be rotated by crossing front legs and pulling calf down and to one side b. Posterior Presentation: i. repel one hind leg while pulling on other hind leg to avoid hip block ii. a second method is to tie a pole between the legs and then rotating the calf 90 degrees iii. once the calf’s hips are in the pelvis, the calf must be rotated back; hip rotation places rib cage in a position which will not enter the pelvis iv. re-rotation of the calf permits entry of the rib cage 7. Fetotomy a. Reduce fetal size, avoids C-section (prevents abdominal contamination); minimal assistance necessary; decreased trauma to dam; less aftercare b. May cause lacerations of birth canal; more work; possible lacerations to operator c. Indications dead fetus; relative or absolute oversized fetus; incomplete cervical dilatation i. Relative oversized fetus – normal fetal size & small maternal pelvis ii. Absolute oversized fetus – abnormally large fetus & normal maternal pelvis d. Assessment of fetal reflexes i. Depress eye eye flutter or globe movement ii. Suckling reflex iii. Anus contractin iv. Withdrawal reflex (pinch skin or flex limb distally) 8. C-section a. Indications live fetus; fetotomy impossible due to small birth canal uterine torsion; fetal mummification; uterine inertia; hydrops condition; vaginal or vulvar stenosis; hypoplastic genital tract 9. Pelvic Splitting a. Only performed on first calf heifers (< 27 months of age) b. Usually restricted to beef cows on pasture c. Requires an epidural Postpartum 1. Normal Uterine Involution usually complete in 30-40 days after parturition a. Myometrial contraction and expulsion of lochia i. Facilitate discharge of fluids and tissue debris ii. Compress uterine vasculature iii. Reduce overall size of uterus b. Endometrial repair c. Resumption of ovarian function d. Elimination of bacterial contamination of reproductive tract 2. Postpartum Problems a. Retained Fetal Membranes i. Toxic syndrome 1. Clinical signs fever, anorexia, depression, ketosis, enlarged fluid filled uterus, fetid odor 2. Treatment monitor temp, feed consumption, milk production; systemic antibiotics (ceftiofur, penicillin); NSAIDS; uterine lavage? 3. Prevention don’t manually remove placentas ii. Non-toxic syndrome 1. Clinical signs slight depression; fetid odor; retained placenta visible 2. Treatment leave placenta alone; systemic antibiotics +/-; re-examine prior to breeding b. Uterine Prolapse (“Casting of the calf bed”) i. Emergency exposure of uterine mucosa; possible trauma; hemorrhage likely ii. Predisposed via long mesometrial attachment; strong tenesemus; atonic uterus; RFM iii. Increased incidence 1. In first calf heifers, stanchioned cattle, post dystocia, hypocalcemic cows iv. Treatment treat hypocalcemia; light epidural; wash uterus; remove edema; elevate uterus; replace cervix first; administer oxytocin after replacement; Buhner suture (stays for 2-3 days – until cervix contracts