Basic Arterial Blood Gases - VCA Specialty Animal Hospitals
advertisement

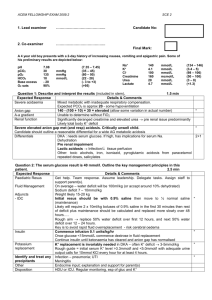
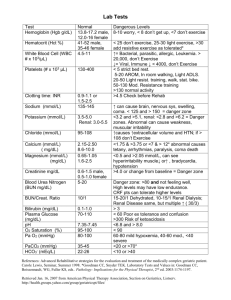
Arterial Blood Gas Analysis Teresa M. Rieser, VMD, DACVECC Getting Started Blood gases can be drawn using either specialized blood gas syringes or with a standard 1 cc syringe that has been coated with an anticoagulant (sodium heparin). The sample should have all air expressed from the needle and then should be capped. Some common pitfalls Dilution of samples can occur if the syringe is not filled fully. When at all possible, try to acquire a full 1 ml sample for analysis. Initially, taking an arterial sample can be a challenge and it is not uncommon to draw a venous sample instead of an arterial sample. This can cause great confusion as the values for normal can vary significantly between an arterial and venous sample. When in doubt, pull a known paired venous sample. Analyze both samples and compare. The pO2, and pH tend to be lower in a venous sample and the pCO2 tends to be higher. If the samples are very similar then it is likely that you have drawn a venous sample instead of an arterial one. It is important to collect the sample anaerobically. Any gas bubbles that occur during sampling should be expelled immediately and the sample capped off (usually with a cube) from outside air. If this does not occur, the sample will begin to equilibrate with room air which has a pO2 of 150 mmHg and a pCO2 of 0 (both values are at sea level). The sample should be run immediately. Measured blood gas values can change in as little as ten minutes at room temperature. If the sample can not be run immediately it should be stored in ice water (rater than just on ice) until analysis. A sample will be stable in this fashion for up to 6 hours. Basics of blood gas analysis Blood gas analysis is useful as an assessment of pulmonary function (with arterial blood gases) as well as an indication of acid-base status of the patient. Normals Arterial blood gas • pH • pO2 • pCO2 • HCO3• TCO2 • BE 7.35-7.45 90-100 (mmHg) 35-45 (mmHg) 20-24 (mmol/L) 19-25 (mmol/L) -4-+4 Venous Blood Gas • pH • pO2 • pCO2 • HCO3• TCO2 • BE 7.35-7.45 30-42 (mmHg) 45 (mmHg) 20-24 (mmol/L) 19-22 (mmol/L) -4-+4 Definitions: o Acidemia – a blood pH of <7.35 o Alkalemia – a blood pH of >7.45. o Acidosis or alkalosis refers to the underlying disturbance that results in acidemia or alkalemia. Metabolic acidosis – the primary gain of acid or loss of base (HCO3-) Major causes for a metabolic acidosis include the following: 1. Lactic acidosis – increased lactate production secondary to poor perfusion for any reason results in lactic acidosis. 2. Diabetic ketoacidosis (DKA)- excess production of ketones result in acidosis. 3. Renal failure- the failing kidney’s inability to recycle bicarbonate or adequately excrete hydrogen causes acidosis 4. GI loss- usually due to a loss of alkaline fluid in diarrhea or vomiting. 5. Intoxications- certain toxins act as acids and can result in a metabolic acidosis. A classic example is ethylene glycol which metabolizes to both oxalic and glycolic acid which contribute to a “high anion gap metabolic acidosis”. Metabolic alkalosis – the primary loss of acid or gain of base. Most common cause is GI loss of HCl with vomiting. Respiratory acidosis – retention of CO2 due to a failure of alveolar ventilation to keep up with carbon dioxide production. Examples include pleural space disease and upper airway diseases. Respiratory alkalosis – the removal of carbon dioxide by ventilation in excess of production. Excellent example is the nervous or painful panting animal. Interpreting the Arterial Blood Gas Oxygenation o Evaluate the ability to oxygenate. If the pO2 is low, calculate the A-a gradient. The A-a gradient will allow you to assess pulmonary function independent of ventilation. o To calculate the A-a gradient you can use the following equation: pAO2 = 150 –[(1.1)(pCO2)] o This equation is only valid at sea level with the patient breathing room air. o Once you have calculated pAO2 , subtract the paO2 for the A-a gradient o Normal < 10 o Gray zone 10-15 o Abnormal > 15 o The value of the A-a gradient is that it provides information about the presence of pulmonary parenchymal dysfunction. It does not differentiate between different types of lung pathology. PaO2/FiO2 Ratio o This is useful for assessing lung oxygenating efficiency when the patient is breathing a higher oxygen concentration than room air. To calculate the value, the PaO2 is divided by the inspired oxygen concentration (FiO2) expressed as a decimal. o Normal = 500 o Mild oxygenating inefficiency = 300-500 o Moderate oxygenating inefficiency = 200-300 o Severe oxygenating inefficiency < 200 Venous Oxygen o Mixed venous oxygen represents the balance between whole body oxygen delivery and oxygen consumption. When oxygen delivery is decreased the tissues continue to draw their normal amount of oxygen, so oxygen extraction increases and venous oxygen decreases. o 40-50 (mmHg) normal o 30-40 low; does not require action o 20-30 very low; corrective action needed o <20 Extremely low; life threatening Ventilation o Evaluate the ability to ventilate. This is determined by looking at the pCO2. If this value is elevated and is not part of compensatory change in response to an acidbase disturbance there is impairment of ventilation. o Causes for impaired ventilation include pleural space disease, upper airway disease, end-stage pulmonary parenchymal disease, insufficient mechanical ventilation, CNS disease. Rib fractures, flail chest, and abdominal lesions which result in pressure on the diaphragm can all lead to hypoventilation. o Hyperventilation occurs in response to hypethermia, stress, pain, anxiety, hypovolemia, CNS disease, inappropriate ventilator settings, and as a compensatory response to metabolic acidosis. Acid-base Status o Evaluate the pH o If acidemia, decide if it is metabolic or respiratory. a. Respiratory acidosis pCO2 > 45 b. Metabolic acidosis HCO3- < 20 or BE < -4 o If alkalemia, decide if it is metabolic or respiratory. a. Respiratory alkalosis pCO2 < 35 b. Metabolic alkalosis HCO3- > 26 or BE > +4 o Assess for compensatory changes. a. A disturbance in the respiratory or metabolic acid-base status will provoke an opposite compensatory response. b. Lungs compensate quickly (within minutes) c. Kidneys compensate slowly (days) d. The degree of compensation may provide insight into the chronicity of the disturbance e. Remember, the body does not overcompensate. Mixed Acid-Base Disturbances o Occurs when there is more than one primary acid-base disturbance in a patient. o Blood gas disturbance is described as simple when there is a single primary disturbance and the appropriate compensatory change. o In identifying a mixed disturbance, it is important to figure out what is an appropriate compensatory change. Disturbance Metabolic acidosis Guide for compensation 1 mEq/L ↓ HCO3- then PCO2 ↓ 0.7 mmHg Metabolic alkalosis 1 mEq/L ↑ HCO3- then PCO2 ↑ 0.7 mmHg Respiratory Acidosis Acute 1 mmHg ↑ PCO2 then HCO3- ↑ by 0.15 mEq/L Chronic 1 mmHg ↑ PCO2 then HCO3- ↑ by 0.35 mEq/L Respiratory Alkalosis Acute 1 mmHg ↓ PCO2 then HCO3- ↓ by 0.25 mEq/L Chronic 1 mmHg ↓ PCO2 then HCO3- ↓ by 0.55 mEq/L Consider a mixed disturbance when: o The pH is normal but the pCO2 and bicarbonate values are not. o When pCO2 and bicarbonate change in opposite directions o Compensation does not appear appropriate based on calculated compensatory change expected. (However, consider if the animal has had enough time for full compensation to occur). The Anion Gap This can be helpful for differentiating between hyperchloremic and high anion-gap acidosis. The anion gap represents the difference between the unmeasured anions and unmeasured cations. The normal value is 19 +/- 5 mEq/L. Anion Gap = ([Na+] + [K+]) – ([Cl-] + [HCO3-]) Electroneutrality is always maintained so if there is a decrease in bicarbonate there must be a concomitant increase in either Cl- or unmeasured anion. In most instances, an increase in anion gap implies an accumulation of organic acids in the body. Decreases in the anion gap are rarely seen. When the anion gap is normal, the difference between sodium concentration and chloride concentration may be helpful. Normally the difference is about 36 mEq/L. An increase is indicative of metabolic alkalosis (usually with hypochloremia) while a decrease indicates a metabolic acidosis (usually hyperchloremic). Example 1 • pH • pCO2 • HCO3• BE 7.26 56 (mmHg) 24 (mmol/L) +1 Example 2 • pH • pCO2 • HCO3• BE 7.20 38 (mmHg) 15 (mmol/L) -10 Example 3 • pH • pCO2 • HCO3• BE 7.52 28 (mmHg) 22 (mmol/L) -1 Example 4 • pH • pCO2 • HCO3• BE 7.24 28 (mmHg) 12 (mmol/L) -14 Example 5 • pH • pCO2 • HCO3• BE 7.38 76 (mmHg) 42 (mmol/L) +8 Example 6 • pH • pCO2 • HCO3• BE 7.39 25 (mmHg) 15 (mmol/L) -11 Example 7 • pH • pCO2 • HCO3• BE 7.44 24 (mmHg) 16 (mmol/L) -9 Example 8 • pH • pCO2 • HCO3• BE 7.56 40 (mmHg) 34 (mmol/L) +13 Example 9 • pH • pCO2 • HCO3• BE 7.55 52 (mmHg) 44 (mmol/L) +15 Example 10 • pH • pCO2 • pO2 • HCO3• BE • Hb • O2Sat 7.375 37.2 (mmHg) 59.3 (mmHg) 21.8 (mmol/L) -3.5 13.3 g/dl 89.4% Example 11 • pH • pCO2 • pO2 • HCO3• BE • Hb • O2Sat Example 12 • pH • pCO2 • pO2 • HCO3• BE • Hb • O2Sat Example 13 • pH • pCO2 • pO2 • HCO3• BE • Hb • O2Sat Example 14 • pH • pCO2 • pO2 • HCO3• BE • Hb • O2Sat Example 15 • • • • • • • pH pCO2 pO2 HCO3BE Hb O2Sat 7.211 74.0 (mmHg) 58.2 (mmHg) 29.8 (mmol/L) +1.7 14.3 g/dl 82.2% 7.354 24.8 (mmHg) 105.1 (mmHg) 13.5 (mmol/L) -11.6 15.7 g/dl 96.1% 7.514 48.6 (mmHg) 111.2 (mmHg) 38.5 (mmol/L) +16.1 10.0 g/dl 98.1% 7.144 69.4 (mmHg) 43.7 (mmHg) 24.0 (mmol/L) -5.2 16.6 g/dl 64.1% 7.368 19.9 (mmHg) 47.6 (mmHg) 11.4 (mmol/L) -13.8 3.0 g/dl 80.5% Example 16 • • • • • • • pH pCO2 pO2 HCO3BE Hb O2Sat 7.336 13.9 (mmHg) 288.8 (mmHg) 7.5 (mmol/L) -18.6 8.0 g/dl 99.9%