PERCUTANEOUS URINARY INTERVENTIONS - e
advertisement

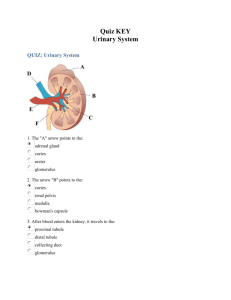
PERCUTANEOUS URINARY TRACT INTERVENTIONS Author: Arnold S. Rappoport, M.D. Objectives: Upon the completion of this CME article, the reader will be able to: 1. Describe the technique that is used for percutaneous access to the renal collecting system. 2. Explain how kidney stones are removed from the renal pelvis through a nephroscope. 3. Describe the complications associated with percutaneous urinary tract interventions. Basic angiographic techniques using needles, guidewires and catheters may be employed in percutaneous interventions of the kidney. All of these concern abnormalities in the renal collecting system. The procedures discussed below include: 1. External drainage of the renal pelvis (percutaneous nephrostomy) 2. Double J stent placement for internal drainage of the collecting system 3. Removal of stones from the renal pelvis (nephrostolithotomy) 4. Dilation of strictures 5. Pressure studies in evaluation of urinary obstruction 6. Percutaneous endoscopic pyelotomy Basic Anatomy: The collecting system can be viewed as a series of “champagne glasses”, the stems of which join to form a single funnel called the renal pelvis. A single duct called the ureter continues from the renal pelvis and drains into the urinary bladder. The “cups” of the champagne glasses are called calyces and the stems are called infundibula. The renal papilla, which is shaped like an inverted cone, projects into a calyx. It is part of the renal parenchyma and contains many small ducts, which drip urine from the kidney into the collecting system. Regarding urinary tract interventions, one anatomic fact regarding the blood supply of the kidney is important to know. As the main renal artery enters the kidney, it divides into ventral and dorsal branches. Therefore, theoretically, there is a band of renal parenchyma laterally where the terminal branches from the dorsal renal artery and the ventral renal artery meet, which is a relatively avascular zone. Indications for Urinary Interventions: The main indications for urinary tract intervention are hydronephrosis and or renal stones. Hydronephrosis by definition is the dilatation of the collecting system and ureter. The more common causes for the development of this disorder are a stone blocking the ureter, a stricture of the ureter (which is either benign or malignant), a tumor in the retroperitoneum encasing the ureter or a bladder tumor blocking the ureter. Regarding renal calculi (stones), the largest is known as a staghorn calculus because it resembles a stag’s antlers. It often fills the entire collecting system. Other stones that often require intervention are large calculi within the collecting system that are refractory to shock lithotripsy (breaking up the stone with electric shock waves). Techniques: The renal pelvis must be visualized, and this can be done either by ultrasound or by performing antegrade pyelography. An antegrade pyelogram is always performed under aseptic conditions. The patient is placed prone on a fluoroscopy table and the back is prepared with Betadine and draped with sterile cloth. For antegrade pyelography, the skin is infiltrated with local anesthetic and a 22g needle is advanced under fluoroscopic guidance into the expected location of the renal pelvis. Suction is applied to the needle as it is advanced and when urine is aspirated, contrast agent is then injected (which opacifies the collecting system). When ultrasound is utilized, a calyx is visualized and then punctured using a small gauge needle. Percutaneous Access: The basic technique for accessing the collecting system is as follows. Ideally, an access site is chosen in a lower pole calyx because this is below the costal margin and will usually cause the least amount of pain. The calyx is identified by either ultrasound or by the contrast agent from the antegrade pyelography. If possible, a lateral approach should be chosen and an attempt is made to pass the needle through the lateral renal parenchyma in the zone of relative avascularity to minimize bleeding complications. When the needle is advanced into the calyx and urine is aspirated, a guidewire is then advanced through the needle and positioned in the renal pelvis or may be advanced into the ureter system. Applications: One application for this technique is external drainage of the renal pelvis for hydronephrosis or infected hydronephrosis (also called pyonephrosis). With the guidewire well seated in the collecting system or ureter, a tract is dilated over the wire through the skin and subcutaneous tissue utilizing a dilating catheter. When this is completed, the nephrostomy catheter is then advanced over the guidewire. The construction of the catheter is such that it has several holes at its distal end. There is a thread, which passes through the lumen of the catheter, that exits one of the distal holes and is then fixed to the tip of the catheter. By pulling on the thread, the tip of the catheter is then approximated to the hole through which the thread exits and thereby forms a loop. The loop is positioned in the renal pelvis, using fluoroscopy. There is a locking device at the catheter’s hub, which locks the thread in place. The loop (called a Cope loop) thus insures that the catheter cannot become dislodged. The catheter is then attached to a urine bag, thereby establishing external drainage. Double J Stent – Internal Drainage: Generally in patients with a malignant stricture of the distal ureter (typically from cervical carcinoma, carcinoma of the colon, or other malignant diseases) or from a stricture of benign causes (from a stone, prior surgical intervention, or retroperitoneal fibrosis) it is desirable to establish internal drainage (figure 1). This is done by passing a guidewire through the stricture of the ureter and then advancing it into the urinary bladder. A double J stent catheter is then placed over the guidewire and advanced so that its leading end enters the urinary bladder and forms a loop. It is also positioned so that its trailing end is positioned in the renal pelvis. When the guidewire is removed, a loop forms at the trailing end of the stent (hence double J stent). The double J stent has drainage holes throughout its entire length so that urine above the stricture enters the stent and exits distally into the bladder. These stents are not permanent and have to be changed every three months. In most instances, urologists use a cystoscopic approach to place the double J stents and this is performed from below through the bladder. Interventional radiologists generally place stents from above only when an urologist is unable to do so from below. The routine maintenance of these catheters requires that they be changed every three months and this is done cystoscopically in almost all instances. Nephrostolithotomy (removal of stone(s) from the renal pelvis): In order to perform this procedure, it is necessary to gain access to the collecting system as described above and to create a nephrostomy tract. Once the renal pelvis is accessed by the needle, a guidewire is inserted and advanced down the ureter into the bladder (figure 2). The interventional radiologist then dilates a tract over this guidewire and places a larger introducing sheath into the kidney through which a second guidewire is passed. This second guidewire is also advanced into the urinary bladder and is left in the nephrostomy tract and collecting system as a safety guidewire. The first wire is referred to as the working wire and it is used to dilate the nephrostomy tract to a size 30 Fr. (1 cm diameter). This is accomplished by advancing a dilation balloon over the wire and positioning it so that it’s tip is just inside the renal calyx. The balloon is inflated, which then dilates the nephrostomy tract. After removing the balloon, a plastic sheath, which is also 1 cm in diameter, is then advanced with a special dilating catheter over the guidewire and positioned in the nephrostomy tract. The inner end of the plastic sheath is therefore inside the collecting system and the outer end projects through the skin. This affords a protected tract into the kidney collecting system. An urologist then uses a viewing instrument (cystoscope or nephroscope), which he places through the introducing sheath, and can view the inside portion of the collecting system. This usually allows he or she to see the stone in the collecting system. The stone is generally larger than the tract and therefore has to be broken up either with an ultrasonic device, a laser device, or with an electrohydraulic device. This process is called lithotripsy. The fragments of stone are then removed using grasping instruments until most, if not all, of the collecting system is free of stone. Balloon Dilation of Strictures: A benign stricture that is caused by fibrosis or adhesions from a prior surgical procedure can be treated by using the same techniques as described above where a guidewire is passed through the stricture area into the bladder. A dilating balloon is then advanced over the guidewire and placed within the stricture area. The balloon is then expanded, which then dilates the stricture. In order to insure that healing occurs in an expanded position, a double J stent is placed across the stricture site and it is generally left in position for six weeks. Pressure Studies (known as the Whitaker Test): This is a test that is generally utilized in children. When a child presents with hydronephrosis, this technique is often employed by urologists to determine whether the finding is due to obstruction. In children, hydronephrosis may be due to reflux and not obstruction. The technique involves gaining access to the collecting system (as described above) and attaching the needle that is positioned in the renal pelvis to a pressure monitor and a pump. Pressures are also measured in the urinary bladder through a Foley catheter. An injection of 10 ml per minute of contrast agent with saline is made into the collecting system. A total of 50-60 ml is injected. This simulates the maximum rate at which urine can be formed. After the injection of each 10-20 cc of contrast agent, pressures are measured in the renal pelvis and in the bladder. A differential pressure between the renal pelvis and the bladder of greater than 20 mm of mercury is diagnostic of an obstruction. Percutaneous Endoscopic Pyelotomy: In some patients, there can be a narrowing of the junction of the renal pelvis and the ureter (also called uretero-pelvic junction obstruction). One possible treatment for this disorder is the use of endoscopic methods. By accessing the renal pelvis (as described above for the use of a nephroscope), it is possible to make an incision in the strictured area using a knife that is passed through the nephroscope. Again, a double J stent must be placed across the stricture area once the procedure is complete in order to insure that the healing process occurs without leaving a residual stenosis. Complications: Unfortunately, complications (though usually uncommon) can occur with the abovedescribed interventional radiological techniques. Hemorrhage can occur, especially if a major artery is injured during the placement of the needle or catheter. This is the reason why the majority of these procedures are attempted through the avascular zone of the kidney posterolateral. Very frequently the urine in an obstructed kidney is infected. In order to gain access to the collecting system, needles and catheters (as described above) are inserted and these will ultimately traverse some of the blood vessels of the kidney. This can sometimes allow bacteria to gain access to the blood stream resulting in a bacteremia (which then can lead to urosepsis). For this reason, prophylactic antibiotics are given with these procedures. Therefore, a 2-hour observation period is necessary after performing a renal drainage procedure to insure that the patient does not become septic. Figures: 1 A patient with a malignant obstruction of the distal ureter resulting in hydronephrosis. A double J stent is passed through the obstruction to allow the passage of urine from the kidney into the bladder. 2 Nephrostolithotomy. A percutaneous placement of a guidewire in a patient with a staghorn calculus. References or Suggested Reading: 1. Handbook of Interventional Radiological Procedures: Kandarpa and Aruny, second edition, Little Brown & Company, 1996, pp. 201-214, 329, and 479. 2. Interventional Radiology in the Urinary Tract in Cancer Patients. Proceedings of the First International Endocurie/Hyperthermia Conference and Workshop: Rappoport AS. Endocurie/Hyperthermia Oncology. October 1987, Vol. 3, No. 4, pp. 209211. About the Author: Dr. Arnold S. Rappoport is a Board Certified Radiologist and is currently an active Interventional Radiologist at Memorial Medical Center in Long Beach, California. He is also an Associate Adjunct Professor for the Department of Radiological Sciences at the University of California, Irvine Medical Center. Dr. Rappoport is a Fellow of the American Board of Radiology and is a Fellow of the Royal College of Radiology. He is also a member of the Society for Cardiovascular Interventional Radiology and the Western Angiographic Society. He has published numerous articles in peer-review journals and has presented lectures regarding Interventional Radiology across the country and internationally. Examination: 1. Regarding urinary tract interventions, one anatomic fact regarding the blood supply of the kidney is important to know, which is the relatively avascular zone. As the main renal artery enters the kidney, it divides into A. three branches. B. ventral and dorsal branches. C. lateral and medial branches. D. right and left branches. E. none of the above. 2. The main indications for urinary tract intervention are A. bleeding B. hydronephrosis C. renal stones D. A & B above E. B & C above 3. Hydronephrosis by definition is the dilatation of the collecting system and ureter. The more common causes for the development of this disorder are A. a stone blocking the ureter B. a stricture of the ureter (which is either benign or malignant) C. a tumor in the retroperitoneum encasing the ureter D. a bladder tumor blocking the ureter E. all of the above 4. Regarding renal calculi (stones), the largest is known as a staghorn calculus. Other stones that often require intervention are large calculi within the collecting system that are refractory to A. shock lithotripsy B. pain medications C. cystoscopy D. nephroscopy E. none of the above 5. Which of the following statements is or are true? A. For antegrade pyelography, the patient is almost always under general anesthesia. B. For antegrade pyelography, infection is of little risk and therefore aseptic conditions are not generally performed. C. For antegrade pyelography, the skin is infiltrated with local anesthetic and a 22g needle is advanced into the renal pelvis under fluoroscopic guidance. D. For antegrade pyelography, the radiologist usually enters the renal pelvis from below through the bladder. E. All of the statements are true. 6. The basic technique for accessing the collecting system is as follows. Ideally, an access site is chosen in a lower pole calyx because this A. is below the costal margin B. C. D. E. is where most obstructions occur will usually cause the least amount of pain A & C above B & C above 7. The construction of the nephrostomy catheter is such that it has several holes at its distal end. There is a thread, which passes through the lumen of the catheter that exits one of the distal holes and is then fixed to the tip of the catheter. By pulling on the thread, the tip of the catheter is then approximated to the hole through which the thread exits and thereby forms A. a Whitaker loop B. a Kandarpa loop C. a Cope loop D. an Aruny loop E. none of the above 8. Generally in patients with a malignant stricture of the distal ureter or from a stricture of benign causes it is desirable to establish A. internal drainage B. external drainage C. peritoneal drainage D. shunt drainage E. none of the above 9. A double J stent catheter is not permanent and has to be changed every A. month B. six months C. three months D. six weeks E. three weeks 10. In most instances, urologists use a cystoscopic approach to place the double J stents and this is performed A. by ultrasound B. from below through the bladder C. by fluoroscopy D. A & B above E. A & C above 11. In order to perform nephrostolithotomy, the interventional radiologist inserts A. only one guidewire B. two guidewires C. three guidewires D. only a catheter with no guide wires E. none of the above 12. In performing nephrostolithotomy, the first wire is referred to as the working wire and it is used to dilate the nephrostomy tract to a size of A. B. C. D E. 1 cm diameter 1 inch diameter 1 mm diameter 2 mm diameter 2 cm diameter 13. In nephrostolithotomy, the stone is viewed with the use of a cystoscope or nephroscope through the introducing sheath. The stone is generally larger than the tract and therefore has to be broken up with A. an ultrasonic device B. a laser device C. an electrohydraulic device D. all of the above E. none of the above 14. A benign stricture of the ureter that is caused by ________________ can be treated using balloon dilation. A. fibrosis B. adhesions from a prior surgical procedure C. cancer of the cervix D. A & B above E. B & C above 15. When treating benign strictures of the ureter with balloon dilation, in order to insure that healing occurs in an expanded position, a double J stent is placed across the stricture site and it is generally left in position for A. three months B. three weeks C. one year D. six months E. six weeks 16. The Whitaker Test is a test that is generally utilized A. in the elderly B. in adults C. in children D. in the blind E. in newborns 17. In children, hydronephrosis may be due to ___________ and not obstruction. Therefore, urologists often perform pressure studies to determine the difference. A. reflux B. an infection C. cancer D. hemorrhage E. a tumor 18. In performing pressure studies, a differential pressure between the renal pelvis and the bladder of greater than _______________ is diagnostic of an obstruction. A. 60 mm of mercury B. 50 mm of mercury C. 40 mm of mercury D. 30 mm of mercury E. 20 mm of mercury 19. Unfortunately, complications (though usually uncommon) can occur with interventional radiological techniques. The two most common complications are A. infection and loss of a kidney B. hemorrhage and infection C. hemorrhage and tumor growth D. loss of a kidney and hemorrhage E. infection and death 20. A _____________ observation period is necessary after performing a renal drainage procedure to insure that the patient does not become septic. A. 1-day B. 1-hour C. 2-day D. 2-hour E. none of the above