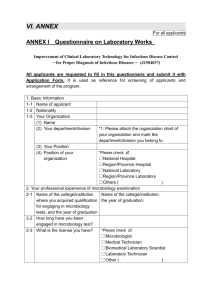
Molecular Diagnostic Tests Manual
advertisement

Policy # MI/MD/v50
Microbiology
Page 1 of 291
Department
Policy & Procedure Manual
Section: Molecular Diagnostic Tests Manual
Issued by: LABORATORY MANAGER
Approved by: Laboratory Director
Subject Title: Table of Contents
Original Date: June 08, 2007
Revision Date: October 26, 2015
Annual Review Date: June 15, 2015
MOLECULAR DIAGNOSTIC TESTS MANUAL
TABLE OF CONTENTS
Virology Accessioning Manual .................................................................................................................. 3
PCR Order Entry Chart .......................................................................................................................5
Adenovirus Qualitative Real-time PCR by Rotorgene ............................................................................. 14
BK Virus Quantitative PCR Bio-Rad CFX96 .......................................................................................... 23
BK Virus Quantitative PCR by Rotorgene ............................................................................................... 41
Chlamydia trachomatis and Neisseria gonorrhoeae PCR by Cobas® ..................................................... 53
Clostridium difficile toxin B gene PCR by Cepheid GeneXpert .............................................................. 64
Testing for C. difficile toxin from eSwab for Infection Control Purpose .......................................77
Cytomegalovirus Quantitative PCR by Cobas® Ampliprep/TaqMan ...................................................... 78
Cytomegalovirus Qualitative PCR by Rotorgene ..................................................................................... 84
Epstein Barr Virus Quantitative PCR by Rotorgene................................................................................. 94
Enterovirus RNA PCR by Lightcycler ................................................................................................... 106
Hepatitis B/Hepatitis C/HIV Donor Screen NAT PCR by Cobas® s201 Ampliprep/TaqMan ............. 116
Herpes simplex Virus/Varicella-Zoster Virus PCR by Rotorgene ......................................................... 127
Human Metapneumovirus RT-PCR by Rotorgene ................................................................................. 138
Human Metapneumovirus and Parainfluenza RT-PCR Bio-Rad CFX96............................................... 146
Human Papilloma Virus (HPV) PCR by Cobas® 4800 ........................................................................... 171
Influenza A/B & RSV PCR by Focus Diagnostics Simplexa™ ............................................................. 181
Parainfluenza RT-PCR by Rotorgene ..................................................................................................... 189
Parvovirus B19 PCR by Rotorgene ........................................................................................................ 197
West Nile Virus PCR by Rotorgene ......................................................................................................... 207
West Nile Virus Donor Screen NAT PCR by Cobas® s201 Ampliprep/TaqMan .................................... 217
APPENDIX I - Molecular Diagnostic Tests Schedule ........................................................................... 225
PROCEDURE MANUAL
UNIVERSITY HEALTH NETWORK / MOUNT SINAI HOSPITAL MICROBIOLOGY DEPARTMENT
NOTE: This is a CONTROLLED document. Any documents appearing in paper form that are not stamped in red "MASTER COPY" are not controlled and
should be checked against the document (titled as above) on the server prior to use
D:\106748206.doc
Policy # MI/MD/v50
Microbiology Department
Policy & Procedure Manual
Section: Molecular Diagnostic Tests Manual
Page 2 of
291
APPENDIX II - Nucleic Acid Extraction –Biomerieux NucliSENS easyMAG .................................... 226
APPENDIX III - Nucleic Acid Extraction for Whole Blood – Biomerieux NucliSENS easyMAG .... 234
APPENDIX IV – Influenza A, B and H1N1 Virus rPCR back up testing by RotorGene ...................... 242
APPENDIX V - Respiratory Synctial Virus (RSV) PCR backup testing by RotorGene ....................... 253
APPENDIX VI - General PCR Precautions and Decontamination Procedures......................................... 262
General PCR Precautions .................................................................................................................262
Decontamination Procedure .............................................................................................................263
WNV Decontamination Procedure ...................................................................................................263
Appendix VII: Creating Standard Curve for Quantitative PCRs............................................................... 265
Appendix VIII - Instructions for Pipetting by epMOTION ...................................................................... 267
Instructions for Pipetting One Test on epMOTION ......................................................................267
Instruction For Pipetting Two Or More Tests On Epmotion: ......................................................272
Appendix IX – RotorGene Worksheet ..................................................................................................... 280
Appendix X – RotorGene Calculations for Reports.................................................................................. 281
Appendix XI – Rotorgene Optical Temperature Verification (OTV) Procedure ....................................... 282
Appendix XII – WNV PCR Procedure Abbreviated * ............................................................................. 286
Record of Edited Revisions .................................................................................................................... 287
PROCEDURE MANUAL
UNIVERSITY HEALTH NETWORK / MOUNT SINAI HOSPITAL MICROBIOLOGY DEPARTMENT
NOTE: This is a CONTROLLED document. Any documents appearing in paper form that are not stamped in red "MASTER COPY" are not controlled and
should be checked against the document (titled as above) on the server prior to use
D:\106748206.doc
Page 3 of
291
Policy # MI/MD/v50
Microbiology Department
Policy & Procedure Manual
Section: Molecular Diagnostic Tests Manual
Virology Accessioning Manual
Respiratory specimen accessioning guide:
DF
A
Qiagen/
Light
Cycler
PCR
PCP
Entero
EasyMag – Altona Rotorgene PCR
Targets
Specimens
Resp Baby
WNV
Adeno
Alpha
HSV
+VZ
BKV
CMV
EBV
Parvo
Meta/
Para
Flu A/B
RSV
‘Virology’
If
requested
Resp (NP)
Adult
Simplexa
Requests/
Comment
If requested
If requested
Yes
‘Virology’
Yes
Resp (NP)
Adult
BAL
BAL
BAL/Spt
LIS CODE
PMH –
14A/14B/
14C/15A/
15B
(Regardless
of comment)
UHN Lung
Tx / Non-tx
Routine tx
“CMV”
PCP
Yes
If requested
If requested
Yes
Yes
Other
*Call ward if suspect virus
not indicated
-Add Multiplex testing:
order “resp virus
detection referred out”
-Label ‘NICU’ if sent
to PHL
-For NP MSH ICU add
Multiplex testing:
order “resp virus
detection referred out”
-MSH NP: 2 extra
aliquots for study
-Do not send NPs to
PHL for “multiplex”
despite comments.
Meta/Para done on
PMH wards NP only.
- Add media in Flu test
- multiplex/luminex or
other virus requests;
order “resp virus
detection ref out”
Yes
Yes
PCENT
PCWNV
PCADE
PCHZ
PCBKV
PCCMV
PCEBV
PCPAR
PCMET/
PCPIN
PROCEDURE MANUAL
UNIVERSITY HEALTH NETWORK / MOUNT SINAI HOSPITAL MICROBIOLOGY DEPARTMENT
NOTE: This is a CONTROLLED document. Any documents appearing in paper form that are not stamped in red "MASTER COPY" are not controlled and should be checked against the document (titled as above) on
the server prior to use
D:\106748206.doc
Page 4 of
291
Policy # MI/MD/v50
Microbiology Department
Policy & Procedure Manual
Section: Molecular Diagnostic Tests Manual
Virology specimen accessioning guide:
Qiagen/
Light
Cycler
PCR
EasyMag – Altona Rotorgene PCR
Targets
Entero
Specimens
Oral/Mouth
Urine
Skin
Genital
Eye
swab/Corneal
scraping
Vitreous/BX
Fetal specimen
Stool
EDTA plasma
WNV
Adeno
‘Virology’
‘Virology’
‘Virology’
‘Virology’
‘Virology’
‘Virology’
‘Virology’
‘Virology’
‘Virology’
CMV/EBV/BK
CSF
‘Virology’
Peritoneal,
Pleural,
Pericardial fluids
Esoph, colon Bx
Non-fetal
Tissue/ Fluid/bile
LIS CODE
‘Virology’
Simplexa
Requests/
Comment
Alpha
HSV
+VZ
BKV
CMV
If requested
If requested
EBV
Parvo
Flu A/B
RSV
Other
*Call ward if suspect virus not
indicated
Yes
PHL for EM
Yes
Yes
Yes
Yes
If requested
Yes
Yes
Yes
Yes
PHL
TGLN
(seasonal)
Yes
If requested
Tx pt only
WNV
(Seasonal)
Baby or Tx
Yes
Yes
Yes
Yes
Yes
PHL for EM
NML for CMV resistance,
HHV
Whole
Blood
Yes
Require
Approval
Require
Approval
PCEBV
PCPAR
NML for HHV-6,7 or JC
Yes
‘Virology’
‘Virology’
Yes
Yes
PCENT
Yes
PCWNV
PCADE
PCHZ
Yes
PCBKV
PCCMV
For processing instrcutions on specimens being sent out for testing see Send out Manual
PROCEDURE MANUAL
UNIVERSITY HEALTH NETWORK / MOUNT SINAI HOSPITAL MICROBIOLOGY DEPARTMENT
NOTE: This is a CONTROLLED document. Any documents appearing in paper form that are not stamped in red "MASTER COPY" are not controlled and should be checked against the document (titled as above) on
the server prior to use
D:\106748206.doc
Page 5 of
291
Policy # MI/MD/v50
Microbiology Department
Policy & Procedure Manual
Section: Molecular Diagnostic Tests Manual
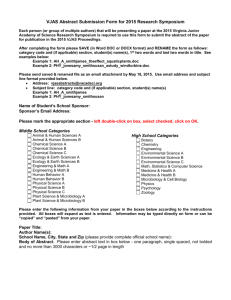
PCR Order Entry Chart
REQUSITIONS FROM
Bay and Algoma Health
Centre-Patients blood drawn
at LIFEA
Bluewater Health LaboratoryNorman Site
CML Healthcare Inc
(Canadian Medical
Laboratories)
Credit Valley Hospital
(Gamma) Dynacare
Laboratories London with
UHN MRN
(Gamma) Dynacare
Laboratories London
WITHOUT UHN MRN
USE UHN MRN
VISIT/WARD
Yes, if have UHN MRN
use UHN
visit/ward
NO, if no UHN MRN. Use
Last name first name
Yes, if have UHN MRN
LIFEA
use UHN
visit/ward
REPORTS TO
FIELD IN
ORDER
ENTRY
SORT
REQ TO
FILE
HOLDER
WHO GETS
REPORT
LIFEA
OTHER PCR
UHN (EPR) and
LIFEA
N
BHNS
OTHER PCR
UHN (EPR) and
BHNS
N
OTHER PCR
UHN (EPR) and
CMLL
Y
OTHER PCR
UHN (EPR) and
CVH
Y
NO, if no UHN MRN. Use
Last name first name
BHNS
Yes, use UHN MRN
use UHN visit
CMLL
Yes, if have UHN MRN
use UHN
visit/ward
CVH
NON
UHN/MSH
AUTOFAX
BUILT
Y/N
NO, if no UHN MRN. Use
Last name first name
CVH
Yes, use UHN MRN
use UHN visit
GDMLL
OTHER PCR
UHN (EPR) and
GDMLL
Y
NO, Last name first name
MRN
GDMLL
Leave Blank
OTHER PCR
GDMLL
Y
Leave Blank
PROCEDURE MANUAL
UNIVERSITY HEALTH NETWORK / MOUNT SINAI HOSPITAL MICROBIOLOGY DEPARTMENT
NOTE: This is a CONTROLLED document. Any documents appearing in paper form that are not stamped in red "MASTER COPY" are not controlled and should be checked against the document (titled as above) on
the server prior to use
D:\106748206.doc
Page 6 of
291
Policy # MI/MD/v50
Microbiology Department
Policy & Procedure Manual
Section: Molecular Diagnostic Tests Manual
REQUSITIONS FROM
(Gamma) Dynacare
Laboratories Main Lab
Brampton with UHN MRN
(Including Huronia Medical
Centre Midland, LaSalle
Community Health Care in
Windsor, 240 Old
Penetanguishene Rd.
(Tremble) and Highlands
Family Health or Dufferin
Area Family Health in
Orangeville (140 Rollinghills
Dr.))
(Gamma) Dynacare
Laboratories Main Lab
Brampton WITHOUT UHN
MRN
Georgian Bay General
Hospital Midland Site
Grand River Hospital
Grey Bruce Health ServicesMeaford Site
USE UHN MRN
VISIT/WARD
REPORTS TO
FIELD IN
ORDER
ENTRY
Yes, use UHN MRN
use UHN visit
DYNAC
OTHER PCR
UHN (EPR) and
DYNAC
Y
NO, Last name first name
MRN
DYNAC
Leave Blank
OTHER PCR
DYNAC
Y
Yes, use UHN MRN
use UHN visit
GBGHM
OTHER PCR
UHN (EPR) and
GBGHM
N
KWHC
Leave Blank
OTHER PCR
KWHC
N
use UHN visit
GBHSM
OTHER PCR
UHN (EPR) and
GBHSM
Y
NO, Last name first name
MRN
Yes, use UHN MRN
Put their lab# (found
under barcode) in site
NO, Use their MRN top
left of label
XXXX XX XX No spaces
in LIS
SORT
REQ TO
FILE
HOLDER
WHO GETS
REPORT
NON
UHN/MSH
AUTOFAX
BUILT
Y/N
PROCEDURE MANUAL
UNIVERSITY HEALTH NETWORK / MOUNT SINAI HOSPITAL MICROBIOLOGY DEPARTMENT
NOTE: This is a CONTROLLED document. Any documents appearing in paper form that are not stamped in red "MASTER COPY" are not controlled and should be checked against the document (titled as above) on
the server prior to use
D:\106748206.doc
Page 7 of
291
Policy # MI/MD/v50
Microbiology Department
Policy & Procedure Manual
Section: Molecular Diagnostic Tests Manual
REQUSITIONS FROM
USE UHN MRN
VISIT/WARD
REPORTS TO
FIELD IN
ORDER
ENTRY
SORT
REQ TO
FILE
HOLDER
WHO GETS
REPORT
use UHN visit
GBRHC
OTHER PCR
UHN (EPR) and
GBRHC
Y
OTMH
Leave Blank
OTHER PCR
OTMH
Y
NON
UHN/MSH
AUTOFAX
BUILT
Y/N
Halton Healthcare ServicesOakville
Yes, use UHN MRN
Put their lab# (found
under barcode) in site
NO, Use their MRN top
left of label
XXXX XX XX No spaces
in LIS
NO, Last name first name
MRN
Horizon Health Network
Yes, use UHN MRN
use UHN visit
DECRH
OTHER PCR
UHN (EPR) and
DECRH
H
Hospital in Common Lab
NO, Last name first name
MRN
HICLM
Leave Blank
OTHER PCR
HICLM
Y
Humber River Regional
Hospital (Church St Site)
NO, Last name first name
MRN
HRRH
Leave Blank
OTHER PCR
HRRH
Y
Humber River Regional
Hospital (Finch Ave Site)
NO, Last name first name
MRN
HRRHF
Leave Blank
OTHER PCR
HRRHF
N
Lakeridge Hospital
NO, Last name first name
MRN
LHC1
Leave Blank
OTHER PCR
LHC1
Y
NO, Use UNIT# as MRN
RTCH
LIFEA
LifeLabs box
LIFEA and
RTCH
Y
NO, Last name first name
MRN
LIFEA
HRRH
LifeLabs box
LIFEA and
HRRH
Y
Grey Bruce Regional Health
Services-Owen Sound Site
{GBHS-Owen Sound on req)
LifeLabs BUT 50 Charlton
Ave Hamilton: May say
Renal Transplant Clinic or
Nephrology Clinic or just
address
LifeLabs BUT Humber River
Regional Hospital at top.
(May also have Dr's name
here)
PROCEDURE MANUAL
UNIVERSITY HEALTH NETWORK / MOUNT SINAI HOSPITAL MICROBIOLOGY DEPARTMENT
NOTE: This is a CONTROLLED document. Any documents appearing in paper form that are not stamped in red "MASTER COPY" are not controlled and should be checked against the document (titled as above) on
the server prior to use
D:\106748206.doc
Page 8 of
291
Policy # MI/MD/v50
Microbiology Department
Policy & Procedure Manual
Section: Molecular Diagnostic Tests Manual
REQUSITIONS FROM
USE UHN MRN
VISIT/WARD
REPORTS TO
FIELD IN
ORDER
ENTRY
LifeLabs NON-TGH doctor
NO, Last name first name
MRN
LIFEA
Leave Blank
LifeLabs box
LIFEA
N
LifeLabs Orillia NON-TGH
doctor
NO, Last name first name
MRN
LIFEO
Leave Blank
LifeLabs box
LIFEO
N
LifeLabs Orillia requesting Tx
doctor (TGH doctor)
Yes, use UHN MRN
use UHN visit
LIFEO
LifeLabs box
UHN (EPR) and
LIFEO
N
LifeLabs requesting Tx doctor
(TGH doctor)
Yes, use UHN MRN
use UHN visit
LIFEA
LifeLabs box
UHN (EPR) and
LIFEA
Y
LHSCM
Leave Blank
OTHER PCR
LHSCM
Y
MSH
Leave Blank
OTHER PCR
MSH
N
Yes, use UHN MRN
use UHN visit
MLW
OTHER PCR
UHN (EPR) and
MLW
N
Yes, if have UHN MRN
use UHN
visit/ward
NFLDP
OTHER PCR
UHN (EPR) and
NFLDP
London Health Science
Centre Microbiology
Laboratory
Markham Stouffville Hospital
Medical Laboratories of
Windsor
Newfoundland Public Health
Laboratory
North Bay General Hospital.
If together with NBRHC
requisition use NBRHC in
Report to field.
Use their MRN top left of
label
XXXX XX XX No spaces
in LIS
Dr Code: JOHNM
Put their lab# (top right)
in site
NO, Last name first name
MRN
NO, if no UHN MRN. Use
Last name first name
Yes, if have UHN MRN
NO, if no UHN MRN. Use
Last name first name
NFLDP
use UHN
visit/ward
NBRHC
NBRHC
SORT
REQ TO
FILE
HOLDER
WHO GETS
REPORT
OTHER PCR
NON
UHN/MSH
AUTOFAX
BUILT
Y/N
N
UHN (EPR) and
NBCH
N
NBCH
PROCEDURE MANUAL
UNIVERSITY HEALTH NETWORK / MOUNT SINAI HOSPITAL MICROBIOLOGY DEPARTMENT
NOTE: This is a CONTROLLED document. Any documents appearing in paper form that are not stamped in red "MASTER COPY" are not controlled and should be checked against the document (titled as above) on
the server prior to use
D:\106748206.doc
Page 9 of
291
Policy # MI/MD/v50
Microbiology Department
Policy & Procedure Manual
Section: Molecular Diagnostic Tests Manual
REQUSITIONS FROM
North Bay Regional Health
Centre
North York General Hospital
USE UHN MRN
VISIT/WARD
Yes, if have UHN MRN
use UHN
visit/ward
NO, if no UHN MRN. Use
Last name first name
Yes, if have UHN MRN
NBRHC
use UHN
visit/ward
REPORTS TO
FIELD IN
ORDER
ENTRY
NBRHC
SORT
REQ TO
FILE
HOLDER
OTHER PCR
NYGCL
OTHER PCR
WHO GETS
REPORT
NON
UHN/MSH
AUTOFAX
BUILT
Y/N
UHN (EPR) and
NBRHC
N
NBRHC
UHN (EPR) and
NYGCL
NO, if no UHN MRN. Use
Last name first name
NYGCL
Notre Dame Hospital
Yes, use UHN MRN
use UHN visit
NDAM
OTHER PCR
Orillia Soldier's Memorial
Hospital Main Laborarory
Yes, if have UHN MRN
NO, if no UHN MRN. Use
Last name first name
use UHN
visit/wardOSMHO
OSMHOLeave
Blank
OTHER PCR
UHN (EPR) and
OSMHOOSMHO
N
Parry Sound (West Parry
Sound Health Centre)
Laboratory
Yes, use UHN MRN
use UHN visit
WPSHL
OTHER PCR
UHN (EPR) and
WPSHL
N
Pembroke Regional Hospital
Yes, use UHN MRN
use UHN visit
PRH -Pembroke
OTHER PCR
UHN (EPR) and
PRH
N
Peterborough Regional
Healthcare
Yes, use UHN MRN
use UHN visit
PRHC
OTHER PCR
UHN (EPR) and
PRHC
N
Queen Elizabeth Hospital,
PEI
NO, Last name first name
MRN
QEPEI
Leave Blank
OTHER PCR
QEPEI
Y
Leave Blank
Y
NYGCL
UHN (EPR) and
NDAM
N
PROCEDURE MANUAL
UNIVERSITY HEALTH NETWORK / MOUNT SINAI HOSPITAL MICROBIOLOGY DEPARTMENT
NOTE: This is a CONTROLLED document. Any documents appearing in paper form that are not stamped in red "MASTER COPY" are not controlled and should be checked against the document (titled as above) on
the server prior to use
D:\106748206.doc
Page 10 of
291
Policy # MI/MD/v50
Microbiology Department
Policy & Procedure Manual
Section: Molecular Diagnostic Tests Manual
REQUSITIONS FROM
USE UHN MRN
VISIT/WARD
REPORTS TO
FIELD IN
ORDER
ENTRY
Queen Elizabeth II Health
Science Centre, Halifax NS
NO, Last name first name
MRN
QE2HS
Leave Blank
OTHER PCR
QE2HS
Y
RVHB
OTHER PCR
UHN (EPR) and
RVHB
Y
SJRH
Leave Blank
OTHER PCR
SJRH
Y
SGHGC-CMV
PCR
SGHGC
SGHGC
Y
TSHBC
Y
Yes, if have UHN MRN
Royal Victoria Hospital Barrie
Saint John Regional Hospital,
Saint John NB
Scarborough General
Hospital-Birchmount
Campus (Grace)
The Scarborough Hospital
Birchmount Campus
Scarborough General
Hospital-General
CampusThe Scarborough
Hospital Main Campus
(x6075)
South Bruce Grey Health
Center WALKERTON
Laboratory
South West Health
NO, if no UHN MRN. Use
Last name first name
NO, Last name first name
MRN
Use Last name first name
Use Last name first name
Use their MRN
WKXXXXXX Dr code:
NEWK1
Put their lab# (under
barcode) in site
Yes, if have UHN MRN
NO, if no UHN MRN. Use
Last name first name
use UHN
visit/ward
SORT
REQ TO
FILE
HOLDER
WHO GETS
REPORT
NON
UHN/MSH
AUTOFAX
BUILT
Y/N
RVHB
OTHER PCR
TSHBC-VRESP
TSHBC
Leave Blank
SGH-CMV
PCRTSH-VRESP
SGHTSHLeave
Blank
OTHER PCR
SGHTSH
YY
SBGHW
Leave Blank
OTHER PCR
SBGWH
Y
SWH
OTHER PCR
UHN (EPR) and
SWH
Y
use UHN
visit/ward
SWH
PROCEDURE MANUAL
UNIVERSITY HEALTH NETWORK / MOUNT SINAI HOSPITAL MICROBIOLOGY DEPARTMENT
NOTE: This is a CONTROLLED document. Any documents appearing in paper form that are not stamped in red "MASTER COPY" are not controlled and should be checked against the document (titled as above) on
the server prior to use
D:\106748206.doc
Page 11 of
291
Policy # MI/MD/v50
Microbiology Department
Policy & Procedure Manual
Section: Molecular Diagnostic Tests Manual
REQUSITIONS FROM
USE UHN MRN
VISIT/WARD
REPORTS TO
FIELD IN
ORDER
ENTRY
Southlake Regional Health
Centre
NO, Last name first name
MRN
YCHN
Leave Blank
use UHN
visit/ward
SJRE
Yes, if have UHN MRN
St John's Rehab Hospital
Toronto (Part of Sunnybrook)
NO, if no UHN MRN. Use
Last name first name
Yes, if have UHN MRN
St Joseph's Hospital GuelphRehab
St Mary's General Hospital
Kitchener
St. Joseph's General
Hospital, Lab, Elliot Lake
Sunnybrook Health Science
Centre Study Dr Anita
Rachlis
Sunnybrook Health Science
Centre Microbiology
NO, if no UHN MRN. Use
Last name first name
Yes, use UHN MRN
Yes, use UHN MRN
SJRE
use UHN
visit/ward
SJHG
use UHN
visit/ward
use UHN
visit/ward
SORT
REQ TO
FILE
HOLDER
WHO GETS
REPORT
OTHER PCR
YCHN
N
OTHER PCR
UHN (EPR) and
SJRE
N
OTHER PCR
UHN (EPR) and
SJHG
N
Leave Blank
SJHG
Leave Blank
STMHK
OTHER PCR
SJGEL
OTHER PCR
UHN (EPR) and
STMHK
UHN (EPR) and
SJGEL
NON
UHN/MSH
AUTOFAX
BUILT
Y/N
N
N
NO, Last name first name
MRN
SHSCR
Leave Blank
OTHER PCR
SHSCR
N
NO, Last name first name
MRN
SHSC
Leave Blank
OTHER PCR
SHSC
Y
Sunnybrook Health Science
Centre/ ACCAPELA Study
NO, use last name:
ACCAPELA
SRCAC
Leave Blank
OTHER PCR
SRCAC
Y
Thunder Bay Regional
Hospital
Yes, use UHN MRN
TBRHS
OTHER PCR
UHN (EPR) and
TBRHS
Y
Toronto Rehab Institute
Yes, use UHN MRN
Leave Blank
OTHER PCR
TRI (EPR)
N (EPR)
use UHN
visit/ward
use UHN
visit/ward
PROCEDURE MANUAL
UNIVERSITY HEALTH NETWORK / MOUNT SINAI HOSPITAL MICROBIOLOGY DEPARTMENT
NOTE: This is a CONTROLLED document. Any documents appearing in paper form that are not stamped in red "MASTER COPY" are not controlled and should be checked against the document (titled as above) on
the server prior to use
D:\106748206.doc
Page 12 of
291
Policy # MI/MD/v50
Microbiology Department
Policy & Procedure Manual
Section: Molecular Diagnostic Tests Manual
REQUSITIONS FROM
USE UHN MRN
VISIT/WARD
REPORTS TO
FIELD IN
ORDER
ENTRY
Trillium Health Centre
NO, Last name first name
MRN
TRHC
Leave Blank
OTHER PCR
TRHC
Y
Yes, use UHN MRN
use UHN
visit/ward
WMRHN
OTHER PCR
UHN (EPR) and
WMRHN
N
WOHCB
Leave Blank
OTHER PCR
WOHCB
Y
WOHCE
Leave Blank
OTHER PCR
WOHCB
Y
WOHCB
use UHN
visit/ward
WRH
OTHER PCR
UHN (EPR) and
WRH
Western Memorial Regional
Hospital (Western Health)
William Osler Health CentreBrampton
William Osler Health CentreEtobicoke
NO, Last name first name
MRN
NO, Last name first name
MRN
Yes, if have UHN MRN
Windsor Regional Hospital
Laboratory
NO, if no UHN MRN. Use
Last name first name
WRH
Leave Blank
SORT
REQ TO
FILE
HOLDER
WHO GETS
REPORT
NON
UHN/MSH
AUTOFAX
BUILT
Y/N
N
PROCEDURE MANUAL
UNIVERSITY HEALTH NETWORK / MOUNT SINAI HOSPITAL MICROBIOLOGY DEPARTMENT
NOTE: This is a CONTROLLED document. Any documents appearing in paper form that are not stamped in red "MASTER COPY" are not controlled and should be checked against the document (titled as above) on
the server prior to use
D:\106748206.doc
Policy # MI/MD/v50
Microbiology Department
Policy & Procedure Manual
Section: Molecular Diagnostic Tests Manual
Page 13 of
291
Stool Preperation:
Stool specimens being processed in house for virology PCR should be processed in the following
manner:
1. Fill a clear small tube with 1.5ml VTM
2. Touch the tip of a wooden stick 3mm into the stool sample and inoculate in the VTM prepared.
3. Vortex the sample until well emulsified.
4. Centrifuge the sample in the Eppindorf 5417C at 10 000 rcf for 3 minutes.
5. Transfer the supernatant into a sample cryovial for extraction by easymag.
Sputolysin Procedure:
Sputolysin reagent is a concentrate of dithiothreitol (DTT) in phosphate buffer used in the isolation of
pathogens from mucoid sputum, BAL and other fluids.
1. Dilute 1ml of Sputolysin Reagent in a conical tube with 9ml of sterile dH20. This solution is
stable for up to 48hrs at 2-8°C
2. Suspend specimen with an equal volume of Sputolysin in a microcentrifuge tube by vortexing for
30 seconds.
3. Incubate at room temperature for 15 minutes.
4. Centrifuge at 5000rpm for 5 minutes and remove supernatant for use.
PROCEDURE MANUAL
UNIVERSITY HEALTH NETWORK / MOUNT SINAI HOSPITAL MICROBIOLOGY DEPARTMENT
NOTE: This is a CONTROLLED document. Any documents appearing in paper form that are not stamped in red "MASTER COPY" are not controlled and
should be checked against the document (titled as above) on the server prior to use
D:\106748206.doc
Policy # MI/MD/v50
Microbiology Department
Policy & Procedure Manual
Section: Molecular Diagnostic Tests Manual
Page 14 of
291
Adenovirus Qualitative Real-time PCR by Rotorgene
I.
Introduction
Adenovirus is a double stranded nonenveloped DNA virus in the family Adenoviridae first isolated in
1950 from adenoid tissue. Adenoviruses is classified into 7 species A to G with many serotypes; causing
a wide range of illnesses from colds, diarrhea, eye infections, to neurological diseases. Recently
Adenovirus has been seen to cause severe infections in transplant recipients resulting in graft loss.
Adenovirus PCR is a qualitative real-time PCR, used for thedetection of Adenovirus in sterile body
fluids, including plasma.
II.
Specimen Collection and Transport
Fluids collected in a sterile container, store at C after collection, if processed within 24 hours; store at
-20oC if processing >24 hours.
EDTA blood: plasma should be removed from red cells 4-6 hours after collection. Centrifuge EDTA
blood at ≥10,000 RCF (Relative Centrifugal Force), and remove plasma 4-6 hours after collection. Store
plasma at C if processed with 24 hours; store at -20oC if processing >24 hours.
III.
Specimen Processing
Please refer to Nucleic Acid Extraction – Biomerieux NucliSENS easyMAG
GENERAL PRECAUTIONS:
There must be separate PCR work areas:Clean room and Specimen preparation area
Powder-free Gloves should only be in use in PCR areas.
Change gloves frequently and keep tubes closed whenever possible.
Prepare Working 1% sodium hypochloride daily
Specimen Preparation Supplies and equipment must be dedicated to Specimen Preparation Area and
not used for other activities and never used in Clean Room.
Change lab coats and gloves between work areas.
Use only Aerosol Resistant Tips (ART)
Use only sterile RNase-free, DNAse-free microtubes
Thaw components thoroughly at room temperature.
PCR work areas (Clean Room and Specimen Preparation Area) benchtops and equipment after
each shift.
PROCEDURE MANUAL
UNIVERSITY HEALTH NETWORK / MOUNT SINAI HOSPITAL MICROBIOLOGY DEPARTMENT
NOTE: This is a CONTROLLED document. Any documents appearing in paper form that are not stamped in red "MASTER COPY" are not controlled and
should be checked against the document (titled as above) on the server prior to use
D:\106748206.doc
Policy # MI/MD/v50
Microbiology Department
Policy & Procedure Manual
Section: Molecular Diagnostic Tests Manual
Page 15 of
291
Materials, Equipments and Facilities:
Clean Room: Biosafety Cabinet (MIBCT3), freezer (MIFTG)
Specimen Preparation area: Biosafety Cabinet (MIBCT7 or MIBCT8)
Rotor-Gene 6000
Rotor-Gene 6000 Multiplexing System with experiment template: Adenovirus
72-Well Loading Block (pre-cooled to 4oC)
72-Well 6000 Series Rotor with Locking Ring
0.1 mL reaction microtubes Tubes and Caps
Variable volume Rainin pipettes: 1 to 20 uL, 10 to 200 uL, 100 to 1000 uL (assigned to designated
areas)
Reagent: Altona RealStar Adenovirus-PCR Kit 1.0: MasterA, MasterB, Internal Control, Adenovirus
Quantitative Standards 1, 2, 3, 4 (QS1, QS2, QS3, and QS4), PCR Grade Water
External Control: Adenovirus Positive, Adenovirus Negative, to be extracted and run in this order on
once amonth, or if QC failure occurs.
IV.
Procedure:
Prepare eluate samples in order according to the Adenovirus worksheet. Add the following Adenovirus
Quantitative Standard and NC Water to the worksheet in the following order: Adenovirus QS3,
Negative-Water.
PCR Set-up:
In the Clean Room: Change into dedicated clean room gown and gloves, work in Biological Safety
Cabinet. Remove from -20oC freezer to thaw at room temperature the required number of vials’ of
Adenovirus Master A, and Adenovirus Master B (12 reactions/vial) for your Adenovirus PCR run.
Prepare Adenovirus Master Mix in 1.5mL conical (sarstedt) microtube; to load on the Eppendorf
epMotion.
Prepare the Master Mix reactions required:
Number of Test Samples + 1 Standard (Adenovirus QS3&NC) + one
Mix gently, do not vortex. Make only enough master mix for the tests you are running. After
Master A has been added together to Master B it cannot be frozen again.
Number of Reactions
Adenovirus Master A
Adenovirus Master B
Volume of Master Mix
Sample/Control Volume
1
5
15
20
10
PROCEDURE MANUAL
UNIVERSITY HEALTH NETWORK / MOUNT SINAI HOSPITAL MICROBIOLOGY DEPARTMENT
NOTE: This is a CONTROLLED document. Any documents appearing in paper form that are not stamped in red "MASTER COPY" are not controlled and
should be checked against the document (titled as above) on the server prior to use
D:\106748206.doc
Policy # MI/MD/v50
Microbiology Department
Policy & Procedure Manual
Section: Molecular Diagnostic Tests Manual
Number of Test
reactions
1
2
3
4
5
6
7
8
9
10
11
12
Page 16 of
291
Adenovirus Master Mix
Adenovirus Master A
(µl)
5
10
15
20
25
30
35
40
45
50
55
60
Adenovirus Master B
(µl)
15
30
45
60
75
90
105
120
135
150
165
180
See Eppendorf epMotion Manual for further loading and programming instructions.
Manual Loading:
Load one reaction microtube (0.1mL) for each sample/control.
Pipette 20uL prepared Adenovirus Master Mix into each reaction microtube.
Pipette 1.0uL of internal control into each reaction microtube designated for the 1 Standards
(Adenovirus QS3 and NC water).
Specimen Processing Area:
Pipette 10uL of Sample/Standard into reaction microtube. Mix by pipetting 3x up and down into
the master mix. Cap each segment after pipetting is completed. Check reaction microtube
segments before loading into the rotor, ensure the liquid levels are at the same height, there are
no bubbles at the bottom of the microtubes, and the lid is tightly in place.
Load reaction microtubes in 72-Well blue rotor, fill empty rotor spaces with blank reaction
microtubes. Attach the Locking Ring. Load the rotor in the Rotor-gene 6000.
PROCEDURE MANUAL
UNIVERSITY HEALTH NETWORK / MOUNT SINAI HOSPITAL MICROBIOLOGY DEPARTMENT
NOTE: This is a CONTROLLED document. Any documents appearing in paper form that are not stamped in red "MASTER COPY" are not controlled and
should be checked against the document (titled as above) on the server prior to use
D:\106748206.doc
Policy # MI/MD/v50
Microbiology Department
Policy & Procedure Manual
Section: Molecular Diagnostic Tests Manual
Page 17 of
291
RotorGene Detection Area:
Switch ON computer, switch ON RotorGene.
FOR THE BLUE ROTORGENE ONLY. Select clinical icon; password “msh”. Enter.
Open “Rotor-Gene 6000 series software 1.7” icon
Wait for “Initializing machine…..”
New Run Window
Select Adenovirus PCR (or CMV this is the same pcr experiment template)
Select New
Select 72 Well Rotor (blue)
Check the box for “Locking Ring Attached”
Select “Next” button.
PROCEDURE MANUAL
UNIVERSITY HEALTH NETWORK / MOUNT SINAI HOSPITAL MICROBIOLOGY DEPARTMENT
NOTE: This is a CONTROLLED document. Any documents appearing in paper form that are not stamped in red "MASTER COPY" are not controlled and
should be checked against the document (titled as above) on the server prior to use
D:\106748206.doc
Policy # MI/MD/v50
Microbiology Department
Policy & Procedure Manual
Section: Molecular Diagnostic Tests Manual
Page 18 of
291
Enter operator intials.
In Notes enter RotorGene colour (i.e. Red or Blue) Reagent Lot Number. Make sure the reaction volume
is 30uL.
Select Next.
Temperature Profile window .Select Next.
Rotor must be loaded.
New Run Wizard window: Select Start Run. The RotorGene will start.
Save As window appears; the run filename is given with the default template. Save in: My Documents in
Adenovirus folder for the current year: e.g. Adenovirus 20150326(1) (assay name yyyymmdd run#)
Select Save.
RotorGene will start running.
Edit Samples window appears.
Enter sample numbers including Adenovirus QS3. Define the sample types according to the chart below.
Name
Sample Type
Samples
Adenovirus
QS3
NC Water
Unknown
Positive
Negative
“Finish”. Click on “Name On”.
PROCEDURE MANUAL
UNIVERSITY HEALTH NETWORK / MOUNT SINAI HOSPITAL MICROBIOLOGY DEPARTMENT
NOTE: This is a CONTROLLED document. Any documents appearing in paper form that are not stamped in red "MASTER COPY" are not controlled and
should be checked against the document (titled as above) on the server prior to use
D:\106748206.doc
P
r
e
s
s
Policy # MI/MD/v50
Microbiology Department
Policy & Procedure Manual
Section: Molecular Diagnostic Tests Manual
Page 19 of
291
Analysis
Profile Program reads: Run has completed.
Analyze raw data by clicking each channel one at a time: Green channel (Adenovirus) and
Yellow channel (IC).
Target
Channel
Report Dye
Adenovirus
Internal Control
Green
Yellow
FAM
JOE
Perform Raw Green (AdenovirusTarget) Channel. Select All Off.
Select sample water (NC) and Adenovirus QS3. Select Autoscale.
Compare each sample curve to the NC-water curve and the Adenovirus QS3 one at a time, then
proceeding to the next sample. A positive curve will have a sigmoidal shape. A negative result
will be a relatively flat line, like the water. Make a note of all positives on the worksheet.
Select Named On.
Select Analysis Icon
In Analysis window. Select Quantitation Tab. (This should be the default).
Two channel option: Cycling A Green and Cycling A Yellow
Select Cycling A. Green. Select Show.
Maximize the window: Quantitation Analysis Cycling A Green or Quantitation Analysis
Cycling A Yellow depending on what channel you are analyzing.
Select Slope Correct.
Select Ignore first: 5 Cycles. OK
Select Threshold Icon and adjust the threshold. The threshold can only cross a curve at one
point.
Select Reports. Select Cycling A Green or Quantitation Analysis Cycling A Yellow
depending on what channel you are analyzing.
Select Quantitation (Full Report)
Maximize report window. Check that only the positives that you have identified, from the raw
data analysis, are positive (i.e. have a crossing threshold ct value).
Print all pages for first channel. Print pages 2-5(or 4) for the second channel.
Close Report window.
Perform Raw Yellow (Internal Control) Channel. Select Name On.
PROCEDURE MANUAL
UNIVERSITY HEALTH NETWORK / MOUNT SINAI HOSPITAL MICROBIOLOGY DEPARTMENT
NOTE: This is a CONTROLLED document. Any documents appearing in paper form that are not stamped in red "MASTER COPY" are not controlled and
should be checked against the document (titled as above) on the server prior to use
D:\106748206.doc
Policy # MI/MD/v50
Microbiology Department
Policy & Procedure Manual
Section: Molecular Diagnostic Tests Manual
Page 20 of
291
All samples, including Adenovirus QS3, and NC water, should have a good amplification curve;
all should be positive in the Yellow IC Channel; with the exception of samples with high ct
values (ct <20.00) in the Adenovirus Target Green Channel.
Select Analysis Icon
In Analysis window. Select Quantitation Tab. (This should be the default).
Two channel option: Cycling A Green and Cycling A Yellow
Select Cycling A. Yellow. Select Show.
Maximize the window: Quantitation Analysis Cycling A Green or Quantitation Analysis
Cycling A Yellow depending on what channel you are analyzing.
Select Slope Correct.
Select Ignore first: 5 Cycles. OK
Select Threshold Icon and adjust the threshold. The threshold can only cross a curve at one
point.
Select Reports. Select Cycling A Green or Quantitation Analysis Cycling A Yellow
depending on what channel you are analyzing.
Select Quantitation (Full Report)
Print all pages for first channel. Print pages 2-5(or 4) for the second channel.
Close Report window.
Note: Cycling A. Yellow report: if there is message of “NEG (Multi Ct)” for any specimen, you
must adjust the threshold. This indicates the threshold has crossed the curve at multiple points.
The threshold can only cross a curve at one point.
Save changes to Adenovirus yyyy-mm-dd. Select Yes.
Shut down the computer, and switch off the Rotor-Gene.
PROCEDURE MANUAL
UNIVERSITY HEALTH NETWORK / MOUNT SINAI HOSPITAL MICROBIOLOGY DEPARTMENT
NOTE: This is a CONTROLLED document. Any documents appearing in paper form that are not stamped in red "MASTER COPY" are not controlled and
should be checked against the document (titled as above) on the server prior to use
D:\106748206.doc
Policy # MI/MD/v50
Microbiology Department
Policy & Procedure Manual
Section: Molecular Diagnostic Tests Manual
V.
Page 21 of
291
Reporting
Adenovirus Not detected: no ct value. Report in LIS using the keypads:
Virology Worklist > Viral PCR worklist > Select from the reporting keypads:
ADENegative for Adenovirus.
This is a research test.
RealStar Adenovirus Kit v1.0. Altona Diagnostics Inc.
Under media PCADE. F6 to enter the date tested.
Finalize the result (Ctrl+F)
Adenovirus Detected: with ct value.
Report Adenovirus as an isolate in the isolate window (F7).
Isolate #: 1 Org.ID. 21ade
Open the Isolate Comment window F8.
Go to the Virology keypad, type “V”.
Adenovirus Detected.
This is a research test.
RealStar Adenovirus Kit v1.0. Altona Diagnostics Inc.
Verify all in the Isolate window
Under media “PCADE” F6 to enter the date tested. And the ct value.
VI.
Quality Control
Reagent QCs:
An External Control (external to Altona Diagnostics) is used to monitor the isolation, amplification and
detection procedures beginning of every month. The result must correspond to expected value supplied
by the manufacturer.
Adenovirus Positive and Adenovirus Negative External controls should be extracted on the easyMag
once a month. Record external QC results in the T drive, Virology folder, QC folder.
Daily QCs: Every run:
Each patient specimen must have an Internal Control (IC) added to monitor both extraction and PCR
inhibition.
Adenovirus QS3 Standard is included and shows a positive reading in Green Channel. Quantitative
Standards must meet valid quantitative parameters.
PROCEDURE MANUAL
UNIVERSITY HEALTH NETWORK / MOUNT SINAI HOSPITAL MICROBIOLOGY DEPARTMENT
NOTE: This is a CONTROLLED document. Any documents appearing in paper form that are not stamped in red "MASTER COPY" are not controlled and
should be checked against the document (titled as above) on the server prior to use
D:\106748206.doc
Policy # MI/MD/v50
Microbiology Department
Policy & Procedure Manual
Section: Molecular Diagnostic Tests Manual
Page 22 of
291
A Negative Water Control is included and shows a negative reading in Green Channel
Report all failed QCs to senior/charge technologist.
Failed QC:
Test is invalid without satisfactory QC results.
Do not release results pending resolution of QC failure.
Inform charge/senior technologist.
Record in: Reagent Log Chart, Instrument Maintenance Log or Incident Report where appropriate.
If the QC failure was due to a simple matter of position reversal or misplacement, the run can be
released (positive QC material yielded positive result, negative yielded negative result).
If positive QC material yielded negative result, repeat the entire run.
If negative QC material yielded positive result, it may be due to cross-contamination from adjacent
positive sample within the run or carry-over contamination from previous runs via equipment or the
environment. Review procedure and equipment to establish and eliminate potential sources of
contamination.
The extent and nature of contamination can also be evaluated by comparing the positive rate of the run
with its expected positive rate.
If the contamination is extensive, it is necessary to quarantine/discard potentially contaminated reagents
and consumables and disinfect equipment and environment before repeating the run.
If a carry-over contamination is suspected (e.g. two or more runs with negative QC being positive or
patient samples have higher than expected positive rate and these samples are often non-repeatable
positives), it is necessary to have a thorough environmental disinfection followed by swabbing to
monitor.
Successful ending to a carry-over contamination may be indicated by QC results and patient positivity
rate falling back to the expected normal range and three negative environmental swabs
VII
References
Realstar Adenovirus PCR Kit v1.0 Instructions, Altona Diagnostics
PROCEDURE MANUAL
UNIVERSITY HEALTH NETWORK / MOUNT SINAI HOSPITAL MICROBIOLOGY DEPARTMENT
NOTE: This is a CONTROLLED document. Any documents appearing in paper form that are not stamped in red "MASTER COPY" are not controlled and
should be checked against the document (titled as above) on the server prior to use
D:\106748206.doc
Policy # MI/MD/v50
Microbiology Department
Policy & Procedure Manual
Section: Molecular Diagnostic Tests Manual
Page 23 of
291
BK Virus Quantitative PCR Bio-Rad CFX96
I. Introduction:
BK virus is a Polyomavirus, first isolated in 1970 from kidney transplant receipient. The virus is
commonly reactivated in immunocompromised transplant patients. BK virus in renal transplant
recipients is associated with nephropathy, in bone marrow transplant with haemorrhagic cystitis.
Monitoring and treatment of BK virus reactivation in transplant patients is vital graft survival
II. Collection and Transport
Urine collected in a sterile container, store at C after collection, if processed within 24 hours; store
at -20oC if processing >24 hours.
EDTA blood: plasma should be removed from red cells 4-6 hours after collection. Centrifuge EDTA
blood at ≥10,000 RCF (Relative Centrifugal Force), and remove plasma 4-6 hours after collection.
Store plasma at C if processed with 24 hours; store at -20oC if processing >24 hours.
III. Specimen Processing
Please refer to Nucleic Acid Extraction – Biomerieux NucliSENS easyMAG
GENERAL PRECAUTIONS:
There must be separate PCR work areas:
Clean room
Specimen preparation room
Powder-free Gloves should only be in use in PCR areas. Change gloves frequently and keep
tubes closed whenever possible.
Prepare Working 1% sodium hypochloride daily.
Specimen Preparation Supplies and equipment must be dedicated to Specimen Prep Area and
not used for other activities and never used in Clean Room.
Change lab coats and gloves between work areas.
Use only Aerosol Resistant Tips (ART)
Use only sterile RNase-free, DNAse-free microtubes
Thaw components thoroughly at room temperature.
PCR work areas (Clean Room and Specimen Preparation Area) benchtops and equipment
after each shift.
Materials, Equipments and Facilities:
Clean Room: Biosafety Cabinet (MIBCT3), freezer (MIFTG)
Specimen Preparation area: Biosafety Cabinet (MIBCT7 or MIBCT8)
BIO-RAD CFX96 Deep WellTM Real-Time System
BIO-RAD Hard-Shel®PCR Plates 96-Well WHT/CLR
BIO-RAD Microseal ®‘B’ seal Seals
PROCEDURE MANUAL
UNIVERSITY HEALTH NETWORK / MOUNT SINAI HOSPITAL MICROBIOLOGY DEPARTMENT
NOTE: This is a CONTROLLED document. Any documents appearing in paper form that are not stamped in red "MASTER COPY" are not controlled and
should be checked against the document (titled as above) on the server prior to use
D:\106748206.doc
Policy # MI/MD/v50
Microbiology Department
Policy & Procedure Manual
Section: Molecular Diagnostic Tests Manual
Page 24 of
291
BIO-RAD Optical Flat 8-Cap Strips for 0.2ml tube strips
BIO-RAD Low-Profile PCR Tubes 8-tube strip, white
96-Well Loading Block (pre-cooled to -20°C)
Variable volume Rainin pipettes: 1 to 20 uL, 10 to 200 uL, 100 to 1000 uL
Reagent: Altona RealStar BKV-PCR Kit 1.0: MasterA, MasterB, Internal Control, BKV
Quantitative Standards 1, 2, 3, 4 (QS1, QS2, QS3, and QS4), PCR Grade Water
External Control: BKV High Positive, BKV Negative, BKV Low Positive, to be extracted and
run in this order on once a week, or if QC failure occurs.
IV. Procedure:
Prepare samples in the order according BKV worksheet. Add the following controls to the Worksheet:
BKV Quantitative Standards 1, 2, 3, 4 (QS1, QS2, QS3, and QS4), PCR Grade Water
PCR Set-up:
In the Clean Room: (Change into dedicated clean room gown and gloves, work in Biosafety Cabinet)
Remove the required vials of BKV Master A and Master B (12 reactions/ vial) from the freezer and
thaw them at room temperature
A. To be loaded by epMotion
Prepare BKV Master Mix in Sarstedt 1.5 mL conical microtube;
Prepare the number of Master Mix reactions required: Number of Test samples + 5 Controls +
extra one
Mix gently, do not vortex. Make only enough master mix for the tests you are running. After
Master A has been added to Master B it cannot be frozen again.
Number of Reactions
BKV Master A
BKV Master B
Volume of Master Mix
Sample/Control Volume
.
No. of Test
reactions
1
2
3
4
5
1
5
15
20
10
BKV Master Mix
BKV Master A (µl)
5
10
15
20
25
BKV Master B (µl)
15
30
45
60
75
PROCEDURE MANUAL
UNIVERSITY HEALTH NETWORK / MOUNT SINAI HOSPITAL MICROBIOLOGY DEPARTMENT
NOTE: This is a CONTROLLED document. Any documents appearing in paper form that are not stamped in red "MASTER COPY" are not controlled and
should be checked against the document (titled as above) on the server prior to use
D:\106748206.doc
Policy # MI/MD/v50
Microbiology Department
Policy & Procedure Manual
Section: Molecular Diagnostic Tests Manual
6
7
8
9
10
11
12
30
35
40
45
50
55
60
Page 25 of
291
90
105
120
135
150
165
180
See Eppendorf epMotion Manual for further loading and programming instructions.
B. To be loaded by manual:
Place 96-well plate onto pre-cooled block
Pipette 20 uL prepared BKV Master Mix into each reaction well;
Pipette 1.0 uL of internal control into the wells designated for the five BKV Controls (BKV
QS1,QS2,QS3,QS4), PCR Water Control NTC;
Pipette 10 uL PCR Water into the well designated for NTC.
In the Specimen Processing Area:
Pipette 10uL of each sample, QS, NTC into reaction wells. Mix by pipetting 3 times up and
down into the Master Mix.
Seal the plate after pipetting is completed.
Check reaction wells before loading into CFX96 Deep Well Real-Time System: ensure the
liquid levels are at the same height, and there are no bubble at the bottom of each reaction well.
Double click Bio-Rad CFX Manager icon
Startup Wizard window pops up
PROCEDURE MANUAL
UNIVERSITY HEALTH NETWORK / MOUNT SINAI HOSPITAL MICROBIOLOGY DEPARTMENT
NOTE: This is a CONTROLLED document. Any documents appearing in paper form that are not stamped in red "MASTER COPY" are not controlled and
should be checked against the document (titled as above) on the server prior to use
D:\106748206.doc
Policy # MI/MD/v50
Microbiology Department
Policy & Procedure Manual
Section: Molecular Diagnostic Tests Manual
Make sure CFX96 Deep Well is selected
Under Select run type, click User-defined button
Run Set up window pops up, including three tabs-Protocol, Plate, and Start Run
Click Open Lid button
Load sealed plate to the block
Click Close Lid button
WARNING! Do NOT manually close the motorized lid
Page 26 of
291
to open the lid
to close the lid
PROCEDURE MANUAL
UNIVERSITY HEALTH NETWORK / MOUNT SINAI HOSPITAL MICROBIOLOGY DEPARTMENT
NOTE: This is a CONTROLLED document. Any documents appearing in paper form that are not stamped in red "MASTER COPY" are not controlled and
should be checked against the document (titled as above) on the server prior to use
D:\106748206.doc
Policy # MI/MD/v50
Microbiology Department
Policy & Procedure Manual
Section: Molecular Diagnostic Tests Manual
Page 27 of
291
Under Protocol tab, select Altona DNA PCR.prcl from Express Load pull-down menu
Express
Load pulldown
menu
Open and
Close
Lid
button
Click Plate tab
on the top or click Next button
side to load the plate profile
Select BKV.pltd plate profile from the Express Load pull-down menu
on the bottom right
PROCEDURE MANUAL
UNIVERSITY HEALTH NETWORK / MOUNT SINAI HOSPITAL MICROBIOLOGY DEPARTMENT
NOTE: This is a CONTROLLED document. Any documents appearing in paper form that are not stamped in red "MASTER COPY" are not controlled and
should be checked against the document (titled as above) on the server prior to use
D:\106748206.doc
Policy # MI/MD/v50
Microbiology Department
Policy & Procedure Manual
Section: Molecular Diagnostic Tests Manual
Click Start Run tab
bottom right side
Confirm the following information:
Protocol: Altona DNA PCR.prcl
Plate: Altona BKV.pltd
Scan Mode: All Channels
If any information above needs to be edited, click Prev button
If all information is correct, click Start Run button
Save Optical Data File [CT014845] window pops up
Change “admin” to “BKV”
Save the file in the designated folder:
on the top or click Next button
Page 28 of
291
on the
T:Microbiology>Virology>Bio Rad CFX96 PCR>Save Run>DNA PCR 2015
Click Save button
PROCEDURE MANUAL
UNIVERSITY HEALTH NETWORK / MOUNT SINAI HOSPITAL MICROBIOLOGY DEPARTMENT
NOTE: This is a CONTROLLED document. Any documents appearing in paper form that are not stamped in red "MASTER COPY" are not controlled and
should be checked against the document (titled as above) on the server prior to use
D:\106748206.doc
Policy # MI/MD/v50
Microbiology Department
Policy & Procedure Manual
Section: Molecular Diagnostic Tests Manual
Page 29 of
291
Build Worklist
Open the worklist file according to the following path:
T:Microbiology>Virology>Bio Rad CFX96 PCR>Worklist Mastcopy>BKV Worklist
Password window pops up, click Read only button
Scan the samples’ information
File > Save as CSV at
T:Microbiology>Virology>Bio Rad CFX96 PCR>Import Worklist>DNA PCR Worklist
2015>BKV
File name: BKV yyyy.mm.dd.run No. eg. Metapara2015.04.07.1
Save as type: CSV (Comma delimited)
Note:Worklist can only be imported as CSV type
Click Save button
PROCEDURE MANUAL
UNIVERSITY HEALTH NETWORK / MOUNT SINAI HOSPITAL MICROBIOLOGY DEPARTMENT
NOTE: This is a CONTROLLED document. Any documents appearing in paper form that are not stamped in red "MASTER COPY" are not controlled and
should be checked against the document (titled as above) on the server prior to use
D:\106748206.doc
Page 30 of
291
Policy # MI/MD/v50
Microbiology Department
Policy & Procedure Manual
Section: Molecular Diagnostic Tests Manual
Click OK
The following window pops up, click Yes button
Close current excel file without any savings.
Import wordlist
Click Realtime Status tab
Select View/Edit Plate… from Plate Setup pull-down menu
Plate Setup
pull-down
menu
Plate Editor window pops up
Click Spreadsheet View/Importer button
PROCEDURE MANUAL
UNIVERSITY HEALTH NETWORK / MOUNT SINAI HOSPITAL MICROBIOLOGY DEPARTMENT
NOTE: This is a CONTROLLED document. Any documents appearing in paper form that are not stamped in red "MASTER COPY" are not controlled and
should be checked against the document (titled as above) on the server prior to use
D:\106748206.doc
Policy # MI/MD/v50
Microbiology Department
Policy & Procedure Manual
Section: Molecular Diagnostic Tests Manual
Plate Spreadsheet View window pops up
Select HEX from Fluors List pull-down menu
Click Import button
Page 31 of
291
PROCEDURE MANUAL
UNIVERSITY HEALTH NETWORK / MOUNT SINAI HOSPITAL MICROBIOLOGY DEPARTMENT
NOTE: This is a CONTROLLED document. Any documents appearing in paper form that are not stamped in red "MASTER COPY" are not controlled and
should be checked against the document (titled as above) on the server prior to use
D:\106748206.doc
Policy # MI/MD/v50
Microbiology Department
Policy & Procedure Manual
Section: Molecular Diagnostic Tests Manual
Page 32 of
291
Select Import File window pops up
T:Microbiology>Virology>Bio Rad CFX96 PCR>Import Worklist>DNA PCR Worklist 2015
Click top left
side corner to
select all
wells
Select appropriate worklist and click Open, all samples and controls information are imported
Click OK button
Select all wells by clicking top left side corner
Type IC as target Name for HEX channel
Hit Enter key on the key board
Click Well groups button
Type IC and
hit Enter key
PROCEDURE MANUAL
UNIVERSITY HEALTH NETWORK / MOUNT SINAI HOSPITAL MICROBIOLOGY DEPARTMENT
NOTE: This is a CONTROLLED document. Any documents appearing in paper form that are not stamped in red "MASTER COPY" are not controlled and
should be checked against the document (titled as above) on the server prior to use
D:\106748206.doc
Policy # MI/MD/v50
Microbiology Department
Policy & Procedure Manual
Section: Molecular Diagnostic Tests Manual
Page 33 of
291
Well Groups Manager window pops up
Click Add button
Select wells including control wells for BKV detection (selected wells should be highlight)
Change the name Group 1 to BKV
Click OK button
Click Ok button from Plate Editor window
PROCEDURE MANUAL
UNIVERSITY HEALTH NETWORK / MOUNT SINAI HOSPITAL MICROBIOLOGY DEPARTMENT
NOTE: This is a CONTROLLED document. Any documents appearing in paper form that are not stamped in red "MASTER COPY" are not controlled and
should be checked against the document (titled as above) on the server prior to use
D:\106748206.doc
Policy # MI/MD/v50
Microbiology Department
Policy & Procedure Manual
Section: Molecular Diagnostic Tests Manual
Click Yes button from the popping up window
Click Time Status tab
Page 34 of
291
from the Run Details window
PROCEDURE MANUAL
UNIVERSITY HEALTH NETWORK / MOUNT SINAI HOSPITAL MICROBIOLOGY DEPARTMENT
NOTE: This is a CONTROLLED document. Any documents appearing in paper form that are not stamped in red "MASTER COPY" are not controlled and
should be checked against the document (titled as above) on the server prior to use
D:\106748206.doc
Policy # MI/MD/v50
Microbiology Department
Policy & Procedure Manual
Section: Molecular Diagnostic Tests Manual
Page 35 of
291
Analyze results after the PCR is completed
Choose BKV from Well Groups pull-down menu
Change the channel names from Fluorophore to Target
Set the threshold line for each target channel
Check if the QC parameters meet requirement
Control Parameter
M Slope
PCR Efficiency
R square (R2)
Valid Values
-3.00 to -3.74
85% to 115%
>0.98
PROCEDURE MANUAL
UNIVERSITY HEALTH NETWORK / MOUNT SINAI HOSPITAL MICROBIOLOGY DEPARTMENT
NOTE: This is a CONTROLLED document. Any documents appearing in paper form that are not stamped in red "MASTER COPY" are not controlled and
should be checked against the document (titled as above) on the server prior to use
D:\106748206.doc
Policy # MI/MD/v50
Microbiology Department
Policy & Procedure Manual
Section: Molecular Diagnostic Tests Manual
Click Export
Select Custom Export…
Select Starting Quantity
Click Export button
Save as Window pops up
Change the File name according to the target and save in the following folder:
Click Save button
Page 36 of
291
PROCEDURE MANUAL
UNIVERSITY HEALTH NETWORK / MOUNT SINAI HOSPITAL MICROBIOLOGY DEPARTMENT
NOTE: This is a CONTROLLED document. Any documents appearing in paper form that are not stamped in red "MASTER COPY" are not controlled and
should be checked against the document (titled as above) on the server prior to use
D:\106748206.doc
Policy # MI/MD/v50
Microbiology Department
Policy & Procedure Manual
Section: Molecular Diagnostic Tests Manual
The final results with Ct values are exported in Excel sheet
Change Starting Quantity to Scientific Notation
Print the excel sheet and attach it to the BK worksheet
Close excel
Click OK button
Click Close button
Close CFX96 Deep Well Real-Time Systim
Shut down computer
Page 37 of
291
End of Shift Cleaning: Perform cleaning protocol as outlined below.
Clean Room: Wipe down with RNAse Away or NucleoClean on paper towel, followed by distilled
water, and then 70% alcohol
Biological Safety Cabinet
Pipettes
Bench tops
Specimen Preparation Area: Wipe down with Working 1% hypochloride (made daily), followed by
distilled water, and then 70% alcohol
Biological Safety Cabinet (BSC), pipettes, centrifuge, and bench top.
Seal and discard BSC waste
Wash racks.
EasyMAG , Lysis Rack, and BioHit Multi-channel Pipette: Wipe down surfaces with RNAse Away
or NucleoClean on KimWipe, followed by UltraPure water, and then 70% alcohol Wipe
Amplification Area: Wipe down surfaces with RNAse Away or NucleoClean on KimWipe, followed
by UltraPure water, and then 70% alcohol Wipe
Seal & discard reaction microtubes into biohazard waste after each run.
Perform the cleaning procedure according the daily maintenance sheet.
PROCEDURE MANUAL
UNIVERSITY HEALTH NETWORK / MOUNT SINAI HOSPITAL MICROBIOLOGY DEPARTMENT
NOTE: This is a CONTROLLED document. Any documents appearing in paper form that are not stamped in red "MASTER COPY" are not controlled and
should be checked against the document (titled as above) on the server prior to use
D:\106748206.doc
Policy # MI/MD/v50
Microbiology Department
Policy & Procedure Manual
Section: Molecular Diagnostic Tests Manual
Page 38 of
291
V. BKV Reporting:
BKV Not detected: Specimen has no ct value. Report in LIS using the keypads:
Virology Worklist > BK PCR worklist > Select from the reporting keypads:
>BKJC }BKNegative for BK virus DNA.
This is a research test.
BKV PCR Kit v1.0. Astra Diagnostics Inc.
Under media PCBKV. F6 to enter the date tested.
Finalize the result (Ctrl+F)
BKV Detected: Specimen with ct value. Report quantitation “copies of DNA/mL”
Report BKV as an isolate in the isolate window (F7).
Isolate #: 1
Org.ID. 62BKV
Open the Isolate Comment window F8.
Go to the Virology keypad, type “V”.
Greater than 10 copies (>10) of DNA/mL. Select the keypad: \BK+
Turn off the reporting keypad. Ctrl + A or Ctrl + K
Enter the copies, in scientific number format, in the space provided, remove extra spacing.
Example:
3.20E+04 copies of DNA/mL.
This is a research test.
BKV PCR Kit v1.0, Astra Diagnostics Inc.
Verify all in the Isolate window
Less than 10 copies (<10) of DNA/mL. Select: \BK10
Under media “PCBKV” F6 to enter the date tested.
If reporting Less than 10 copies (<10) of DNA/mL, enter the actual copy value.
Interim (Ctrl + L) the report.
Second technologist will check transcription in LIS and Finalize Ctrl + F the report.
PROCEDURE MANUAL
UNIVERSITY HEALTH NETWORK / MOUNT SINAI HOSPITAL MICROBIOLOGY DEPARTMENT
NOTE: This is a CONTROLLED document. Any documents appearing in paper form that are not stamped in red "MASTER COPY" are not controlled and
should be checked against the document (titled as above) on the server prior to use
D:\106748206.doc
Policy # MI/MD/v50
Microbiology Department
Policy & Procedure Manual
Section: Molecular Diagnostic Tests Manual
Page 39 of
291
VI. Quality Control
Reagent QCs:
An External Control (external to altona Diagnostics) is used to monitor the isolation,
amplification and detection procedures. The result must correspond to expected value supplied
by the manufacturer.
External control for hMPV A, hMPV B, PIV1/3, and PIV 2/4 should be extracted on the on the
easyMag and run once a month and/or with each new lot.
a.
b.
c.
d.
e.
f.
g.
h.
i.
j.
Daily QCs: Every Run
Each patient specimen must have an Internal Control (IC) added to monitor both isolation and
PCR inhibition.
A Positive Control is included and shows a positive reading in FAM channels (hMPV B and PIV
1/3) Channel or a positive reading in Cy5 Channels ( hMPV A and PIV 2/4)
A Negative Control is include and shows a negative reading in both FAM channels (hMPV B
and PIV 1/3) Channel and Cy5 Channels ( hMPV A and PIV 2/4)
Report all failed QCs to senior/charge technologist.
Failed QC:
Test is invalid without satisfactory QC results.
Do not release results pending resolution of QC failure.
Inform charge/senior technologist.
Record in Reagent Log Chart, Instrument Maintenance Log or Incident Report where
appropriate.
If the QC failure was due to a simple matter of position reversal or misplacement, the run can be
released (positive QC material yielded positive result, negative yielded negative result).
If positive QC material yielded negative result, repeat the entire run.
If negative QC material yielded positive result, it may be due to cross-contamination from
adjacent positive sample within the run or carry-over contamination from previous runs via
equipment or the environment. Review procedure and equipment to establish and eliminate
potential sources of contamination.
The extent and nature of contamination can also be evaluated by comparing the positive rate of
the run with its expected positive rate.
If the contamination is extensive, it is necessary to quarantine/discard potentially contaminated
reagents and consumables and disinfect equipment and environment before repeating the run.
If a carry-over contamination is suspected (e.g. two or more runs with negative QC being
positive or patient samples have higher than expected positive rate and these samples are often
non-repeatable positives), it is necessary to have a thorough environmental disinfection followed
by swabbing to monitor.
Successful ending to a carry-over contamination may be indicated by QC results and patient
positivity rate falling back to the expected normal range and three negative environmental swabs.
PROCEDURE MANUAL
UNIVERSITY HEALTH NETWORK / MOUNT SINAI HOSPITAL MICROBIOLOGY DEPARTMENT
NOTE: This is a CONTROLLED document. Any documents appearing in paper form that are not stamped in red "MASTER COPY" are not controlled and
should be checked against the document (titled as above) on the server prior to use
D:\106748206.doc
Policy # MI/MD/v50
Microbiology Department
Policy & Procedure Manual
Section: Molecular Diagnostic Tests Manual
VII.
Page 40 of
291
References:
RealStar hMPV RT-PCR Kit v1.0, altona Diagnostics
RealStar PIV RT-PCR Kit v1.0, altona Diagnostics
cdc.gov/Human Parainfluenza Viruses (HPIVs) (/parainfluenza/index.html
Emerging Infectious Disease Journal Volume 14, Number1-January 2008
PROCEDURE MANUAL
UNIVERSITY HEALTH NETWORK / MOUNT SINAI HOSPITAL MICROBIOLOGY DEPARTMENT
NOTE: This is a CONTROLLED document. Any documents appearing in paper form that are not stamped in red "MASTER COPY" are not controlled and
should be checked against the document (titled as above) on the server prior to use
D:\106748206.doc
Policy # MI/MD/v50
Microbiology Department
Policy & Procedure Manual
Section: Molecular Diagnostic Tests Manual
Page 41 of
291
BK Virus Quantitative PCR by Rotorgene
I.
Introduction
BK virus is a Polyomavirus, first isolated in 1970 from kidney transplant receipient. The virus is
commonly reactivated in immunocompromised transplant patients. BK virus in renal transplant
recipients is associated with nephropathy, in bone marrow transplant with haemorrhagic cystitis.
Monitoring and treatment of BK virus reactivation in transplant patients is vital graft survival
II.
Specimen Types
Urine collected in a sterile container, store at C after collection, if processed within 24 hours;
store at -20oC if processing >24 hours.
EDTA blood: plasma should be removed from red cells 4-6 hours after collection. Centrifuge
EDTA blood at ≥10,000 RCF (Relative Centrifugal Force), and remove plasma 4-6 hours after
collection. Store plasma at C if processed with 24 hours; store at -20oC if processing >24 hours.
III.
Specimen Processing
Please refer to Nucleic Acid Extraction – Biomerieux NucliSENS easyMAG
GENERAL PRECAUTIONS:
There must be separate PCR work areas:Clean room and Specimen preparation area
Powder-free Gloves should only be in use in PCR areas.
Change gloves frequently and keep tubes closed whenever possible.
Prepare Working 1% sodium hypochloride daily
Specimen Preparation Supplies and equipment must be dedicated to Specimen Preparation
Area and not used for other activities and never used in Clean Room.
Change lab coats and gloves between work areas.
Use only Aerosol Resistant Tips (ART)
Use only sterile RNase-free, DNAse-free microtubes
Thaw components thoroughly at room temperature.
PCR work areas (Clean Room and Specimen Preparation Area) benchtops and equipment
after each shift.
IV.
Materials, Equipments and Facilities:
Clean Room: Biosafety Cabinet (MIBCT3), freezer (MIFTG)
Specimen Preparation area: Biosafety Cabinet (MIBCT7 or MIBCT8)
Rotor-Gene 6000
Rotor-Gene 6000 Multiplexing System with experiment template: BK Virus
PROCEDURE MANUAL
UNIVERSITY HEALTH NETWORK / MOUNT SINAI HOSPITAL MICROBIOLOGY DEPARTMENT
NOTE: This is a CONTROLLED document. Any documents appearing in paper form that are not stamped in red "MASTER COPY" are not controlled and
should be checked against the document (titled as above) on the server prior to use
D:\106748206.doc
Policy # MI/MD/v50
Microbiology Department
Policy & Procedure Manual
Section: Molecular Diagnostic Tests Manual
Page 42 of
291
72-Well Loading Block (pre-cooled to 4oC)
72-Well 6000 Series Rotor with Locking Ring
0.1 mL reaction microtubes Tubes and Caps
Variable volume Rainin pipettes: 1 to 20 uL, 10 to 200 uL, 100 to 1000 uL (assigned to designated areas)
Reagent: Altona RealStar BKV-PCR Kit 1.0: MasterA, MasterB, Internal Control, BKV Quantitative
Standards 1, 2, 3, 4 (QS1, QS2, QS3, and QS4), PCR Grade Water
External Control: BKV High Positive, BKV Negative, BKV Low Positive, to be extracted and run in this
order on once a week, or if QC failure occurs.
V.
Procedure:
Prepare eluate samples in order according to the BKV worksheet. Add the following BKV
Quantitative Standards and NTC Water to the worksheet in the following order: BKV QS4,
BKV QS3, BKV QS2, BKV QS1, NTC (Non-Template Control) Water.
PCR Set-up:
In the Clean Room: Change into dedicated clean room gown and gloves, work in Biological
Safety Cabinet. Remove from -20oC freezer to thaw at room temperature the required number of
vials’ of BKV Master A, and BKV Master B (12 reactions/vial) for your BKV PCR run. Prepare
BKV Master Mix in 1.5mL conical (sarstedt) microtube; to load on the Eppendorf epMotion.
Prepare the Master Mix reactions required:
Number of Test Samples + 5 Standards (4QS&NTC) + one
Mix gently, do not vortex. Make only enough master mix for the tests you are running.
After Master A has been added together to Master B it cannot be frozen again.
Number of Reactions
BKV Master A
BKV Master B
Volume of Master Mix
Sample/Control Volume
1
5
15
20
10
PROCEDURE MANUAL
UNIVERSITY HEALTH NETWORK / MOUNT SINAI HOSPITAL MICROBIOLOGY DEPARTMENT
NOTE: This is a CONTROLLED document. Any documents appearing in paper form that are not stamped in red "MASTER COPY" are not controlled and
should be checked against the document (titled as above) on the server prior to use
D:\106748206.doc
Policy # MI/MD/v50
Microbiology Department
Policy & Procedure Manual
Section: Molecular Diagnostic Tests Manual
Number of Test
reactions
1
2
3
4
5
6
7
8
9
10
11
12
Page 43 of
291
BKV Master Mix
BKV Master A (µl)
5
10
15
20
25
30
35
40
45
50
55
60
BKV Master B (µl)
15
30
45
60
75
90
105
120
135
150
165
180
See Eppendorf epMotion Manual for further loading and programming instructions.
Manual Loading:
Load one reaction microtube (0.1mL) for each sample/control.
Pipette 20uL prepared BKV Master Mix into each reaction microtube.
Pipette 1.0uL of internal control into each reaction microtube designated for the 5 Standards
(BKV QS4, QS3, QS2, QS1, and NTC).
Specimen Processing Area:
Pipette 10uL of Sample/Standard into reaction microtube. Mix by pipetting 3x up and down into
the master mix. Cap each segment after pipetting is completed. Check reaction microtube
segments before loading into the rotor, ensure the liquid levels are at the same height, there are
no bubbles at the bottom of the microtubes, and the lid is tightly in place.
Load reaction microtubes in 72-Well blue rotor, fill empty rotor spaces with blank
reaction microtubes. Attach the Locking Ring. Load the rotor in the Rotor-gene 6000.
RotorGene Detection Area:
Switch ON computer, switch ON RotorGene.
FOR THE BLUE ROTOGENE ONLY. Select clinical icon; password “msh”. Enter.
Open “Rotor-Gene 6000 series software 1.7” icon
Wait for “Initializing machine…..”
PROCEDURE MANUAL
UNIVERSITY HEALTH NETWORK / MOUNT SINAI HOSPITAL MICROBIOLOGY DEPARTMENT
NOTE: This is a CONTROLLED document. Any documents appearing in paper form that are not stamped in red "MASTER COPY" are not controlled and
should be checked against the document (titled as above) on the server prior to use
D:\106748206.doc
Policy # MI/MD/v50
Microbiology Department
Policy & Procedure Manual
Section: Molecular Diagnostic Tests Manual
Page 44 of
291
New Run Window
Select BKV PCR
Select New
Select 72 Well Rotor (blue)
Check the box for “Locking Ring Attached”
Select “Next” button.
PROCEDURE MANUAL
UNIVERSITY HEALTH NETWORK / MOUNT SINAI HOSPITAL MICROBIOLOGY DEPARTMENT
NOTE: This is a CONTROLLED document. Any documents appearing in paper form that are not stamped in red "MASTER COPY" are not controlled and
should be checked against the document (titled as above) on the server prior to use
D:\106748206.doc
Policy # MI/MD/v50
Microbiology Department
Policy & Procedure Manual
Section: Molecular Diagnostic Tests Manual
Page 45 of
291
Enter operator intials.
In Notes enter RotorGene colour (i.e. Red or Blue) Reagent Lot Number. Make sure the reaction volume
is 30uL.
Select Next.
Temperature Profile window .Select Next.
Rotor must be loaded.
New Run Wizard window: Select Start Run. The RotorGene will start.
Save As window appears; the run filename is given with the default template. Save in: My Documents in
BK Virus folder for the current year: e.g. BK Virus 20150326(1) (assay name yyyymmdd run#)
Select Save.
RotorGene will start running.
Edit Samples window appears.
Enter sample numbers including Quantitative Standards (BKV QS4, QS3, QS2, QS1, NTC) and
concentrations. Define the sample types according to the chart below.
Name
Samples
BKV QS4
BKV QS3
BKV QS2
BKV QS1
NC Water
Sample Type
Given
concentration
Copies/uL
*Conversion
factor
x250
Enter Concentration
1.00E+01
1.00E+02
1.00E+03
1.00E+04
x250
x250
x250
x250
2.50E+03
2.50E+04
2.50E+05
2.50E+06
Copies/mL
Unknown
Standard
Standard
Standard
Standard
NTC
(No template
control)
*conversion factor is based on the extraction sample volume and eluate volume
*Result (copies of DNA/mL) = Result (copies/uL) x Elution volume (uL)
Sample volume (mL)
*Result (copies of DNA/mL) = Result (copies/uL) x 50(uL)
0.200 (mL)
Under Given Conc. Format: Select 1.23E+05 (2 decimal points expressed as an exponent).
Units: Select copies/mL
Press “Finish”. Click on “Name On”.
PROCEDURE MANUAL
UNIVERSITY HEALTH NETWORK / MOUNT SINAI HOSPITAL MICROBIOLOGY DEPARTMENT
NOTE: This is a CONTROLLED document. Any documents appearing in paper form that are not stamped in red "MASTER COPY" are not controlled and
should be checked against the document (titled as above) on the server prior to use
D:\106748206.doc
Policy # MI/MD/v50
Microbiology Department
Policy & Procedure Manual
Section: Molecular Diagnostic Tests Manual
Page 46 of
291
Analysis
Profile Program reads: Run has completed.
Analyze raw data by clicking each channel one at a time: Green channel (BKV) and Yellow
channel (IC).
Target
Channel
Report Dye
BKV
Internal Control
Green
Yellow
FAM
JOE
Perform Raw Green (BKV Target) Channel. Select All Off.
Select sample water (NTC) and BKV QS4, QS3, QS2, QS1. Select Autoscale.
Compare each sample curve to the NTC-water curve and the BKV QSs’ one at a time, then
proceeding to the next sample. A positive curve will have a sigmoidal shape. A negative result
will be a relatively flat line, like the water. Make a note of all positives on the worksheet.
Select Named On.
Select Analysis Icon
In Analysis window. Select Quantitation Tab. (This should be the default).
Two channel option: Cycling A Green and Cycling A Yellow
Select Cycling A. Green. Select Show.
Calculate Automatic Threshold. Select OK.
Maximize the window: Quantitation Analysis Cycling A Green or Quantitation Analysis
Cycling A Yellow depending on what channel you are analyzing.
Select Slope Correct.
Select Ignore first: 5 Cycles. OK
Select Threshold Icon and adjust the threshold. The threshold can only cross a curve at one
point.
Verify the Quantitative Standard Curve on the Green (FAM) Channel. The following parameters
must be met, this information can be found on page one of the Green Channel Quantitation –Full
Report or on the screen in the Green Channel Graph.
Control Parameter
M Slope
PCR Efficiency
R square (R2)
Valid Values
-3.00 to -3.74
85% to 115%
>0.98
PROCEDURE MANUAL
UNIVERSITY HEALTH NETWORK / MOUNT SINAI HOSPITAL MICROBIOLOGY DEPARTMENT
NOTE: This is a CONTROLLED document. Any documents appearing in paper form that are not stamped in red "MASTER COPY" are not controlled and
should be checked against the document (titled as above) on the server prior to use
D:\106748206.doc
Policy # MI/MD/v50
Microbiology Department
Policy & Procedure Manual
Section: Molecular Diagnostic Tests Manual
Page 47 of
291
If the quantitative parameters are not valid, it must be brought to the attention of the senior/and or
charge. External Controls must be valid, if not valid, it must be brought to the attention of the
senior/and or charge. Patients results must not be released.
PROCEDURE MANUAL
UNIVERSITY HEALTH NETWORK / MOUNT SINAI HOSPITAL MICROBIOLOGY DEPARTMENT
NOTE: This is a CONTROLLED document. Any documents appearing in paper form that are not stamped in red "MASTER COPY" are not controlled and
should be checked against the document (titled as above) on the server prior to use
D:\106748206.doc
Policy # MI/MD/v50
Microbiology Department
Policy & Procedure Manual
Section: Molecular Diagnostic Tests Manual
Page 48 of
291
Select Reports. Select Cycling A Green (Target) or Quantitation Analysis Cycling A Yellow
(Internal Control) depending on what channel you are analyzing.
Select Quantitation (Full Report)
Maximize report window. Check that only the positives that you have identified, from the raw
data analysis, are positive (i.e. have a crossing threshold ct value).
Print all pages for Green (Target-FAM) channel. Print pages 2-5(or 4) for the Yellow (Internal
Control-JOE) channel.
Close Report window.
Perform Raw Yellow (Internal Control) Channel. Select Name On.
All samples, including BKV QS1-4, and NTC water, should have a good amplification curve; all
should be positive in the Yellow IC Channel; with the exception of samples with high ct values
(ct <20.00) in the BKV Target Green Channel.
Select Analysis Icon
In Analysis window. Select Quantitation Tab. (This should be the default).
Two channel option: Cycling A Green and Cycling A Yellow
Select Cycling A. Yellow. Select Show.
Calculate Automatic Threshold. Select OK.
Maximize the window: Quantitation Analysis Cycling A Green or Quantitation Analysis
Cycling A Yellow depending on what channel you are analyzing.
Select Slope Correct.
Select Ignore first: 5 Cycles. OK
Select Threshold Icon and adjust the threshold. The threshold can only cross a curve at one
point.
Select Reports. Select Cycling A Green or Quantitation Analysis Cycling A Yellow
depending on what channel you are analyzing.
Select Quantitation (Full Report)
Print all pages for first channel. Print pages 2-5(or 4) for the Yellow IC channel.
Close Report window.
Note: Cycling A. Yellow report: if there is message of “NEG (Multi Ct)” for any specimen, you
must adjust the threshold. This indicates the threshold has crossed the curve at multiple points.
The threshold can only cross a curve at one point.
Save changes to BKV yyyy-mm-dd. Select Yes.
Shut down the computer, and switch off the Rotor-Gene.
PROCEDURE MANUAL
UNIVERSITY HEALTH NETWORK / MOUNT SINAI HOSPITAL MICROBIOLOGY DEPARTMENT
NOTE: This is a CONTROLLED document. Any documents appearing in paper form that are not stamped in red "MASTER COPY" are not controlled and
should be checked against the document (titled as above) on the server prior to use
D:\106748206.doc
Policy # MI/MD/v50
Microbiology Department
Policy & Procedure Manual
Section: Molecular Diagnostic Tests Manual
VI.
Page 49 of
291
Reporting
BKV Not detected: Specimen has no ct value. Report in LIS using the keypads:
Virology Worklist > BK PCR worklist > Select from the reporting keypads:
>BKJC }BKNegative for BK virus DNA.
This is a research test.
BKV PCR Kit v1.0. Astra Diagnostics Inc.
Under media PCBKV. F6 to enter the date tested.
Finalize the result (Ctrl+F)
BKV Detected: Specimen with ct value. Report quantitation “copies of DNA/mL”
Report BKV as an isolate in the isolate window (F7).
Isolate #: 1
Org.ID. 62BKV
Open the Isolate Comment window F8.
Go to the Virology keypad, type “V”.
Greater than 10 copies (>10) of DNA/mL. Select the keypad: \BK+
Turn off the reporting keypad. Ctrl + A or Ctrl + K
Enter the copies, in scientific number format, in the space provided, remove extra spacing.
Example:
3.20E+04 copies of DNA/mL.
This is a research test.
BKV PCR Kit v1.0, Astra Diagnostics Inc.
Verify all in the Isolate window
Less than 10 copies (<10) of DNA/mL. Select: \BK10
Under media “PCBKV” F6 to enter the date tested.
If reporting Less than 10 copies (<10) of DNA/mL, enter the actual copy value.
Interim (Ctrl + L) the report.
Second technologist will check transcription in LIS and Finalize Ctrl + F the report.
PROCEDURE MANUAL
UNIVERSITY HEALTH NETWORK / MOUNT SINAI HOSPITAL MICROBIOLOGY DEPARTMENT
NOTE: This is a CONTROLLED document. Any documents appearing in paper form that are not stamped in red "MASTER COPY" are not controlled and
should be checked against the document (titled as above) on the server prior to use
D:\106748206.doc
Policy # MI/MD/v50
Microbiology Department
Policy & Procedure Manual
Section: Molecular Diagnostic Tests Manual
VII.
Page 50 of
291
Quality Control
Reagent QCs:
An External Control (external to altona Diagnostics) is used to monitor the isolation,
amplification and detection procedures. The result must correspond to expected value supplied
by the manufacturer.
BKV High Positive and BKV Low Positive External controls should be extracted on the
easyMag once a week. Record external QC results in the T drive, Virology folder, QC folder.
Daily QCs: Every run:
Each patient specimen must have an Internal Control (IC) added to monitor both extraction and
PCR inhibition.
BKV QS1, QS2, QS3, QS4 Standard is included and shows a positive reading in Green Channel.
Quantitative Standards must meet valid quantitative parameters.
A Negative NTC (No template control) Control is included and shows a negative reading in
Green Channel
Report all failed QCs to senior/charge technologist.
Failed QC:
Test is invalid without satisfactory QC results.
Do not release results pending resolution of QC failure.
Inform charge/senior technologist.
Record in: Reagent Log Chart, Instrument Maintenance Log or Incident Report where
appropriate.
If the QC failure was due to a simple matter of position reversal or misplacement, the run can be
released (positive QC material yielded positive result, negative yielded negative result).
If positive QC material yielded negative result, repeat the entire run.
If negative QC material yielded positive result, it may be due to cross-contamination from
adjacent positive sample within the run or carry-over contamination from previous runs via
equipment or the environment. Review procedure and equipment to establish and eliminate
potential sources of contamination.
The extent
and nature of contamination can also be evaluated by comparing the positive rate of the run with
its expected positive rate.
If the contamination is extensive, it is necessary to quarantine/discard potentially contaminated
reagents and consumables and disinfect equipment and environment before repeating the run.
If a carry-over contamination is suspected (e.g. two or more runs with negative QC being
positive or patient samples have higher than expected positive rate and these samples are often
non-repeatable positives), it is necessary to have a thorough environmental disinfection followed
by swabbing to monitor.
Successful ending to a carry-over contamination may be indicated by QC results and patient
positivity rate falling back to the expected normal range and three negative environmental swabs
PROCEDURE MANUAL
UNIVERSITY HEALTH NETWORK / MOUNT SINAI HOSPITAL MICROBIOLOGY DEPARTMENT
NOTE: This is a CONTROLLED document. Any documents appearing in paper form that are not stamped in red "MASTER COPY" are not controlled and
should be checked against the document (titled as above) on the server prior to use
D:\106748206.doc
Page 51 of
291
Policy # MI/MD/v50
Microbiology Department
Policy & Procedure Manual
Section: Molecular Diagnostic Tests Manual
Summary Information: BKV PCR
Number of Reactions
BKV Master A
BKV Master B
Volume of Master Mix
Sample/Control Volume
Name
Sample Type
1
5
15
20
10
Given
concentration
Copies/uL
*Conversion
factor
x250
Enter Concentration
Copies/mL
Samples
Unknown
BKV QS4
Standard
1.00E+01
x250
2.50E+03
BKV QS3
Standard
1.00E+02
x250
2.50E+04
BKV QS2
Standard
1.00E+03
x250
2.50E+05
BKV QS1
Standard
1.00E+04
x250
2.50E+06
NC Water
NTC
(No template
control)
Control Parameter
M Slope
PCR Efficiency
R square (R2)
Valid Values
-3.00 to -3.74
85% to 115%
>0.98
PROCEDURE MANUAL
UNIVERSITY HEALTH NETWORK / MOUNT SINAI HOSPITAL MICROBIOLOGY DEPARTMENT
NOTE: This is a CONTROLLED document. Any documents appearing in paper form that are not stamped in red "MASTER COPY" are not controlled and
should be checked against the document (titled as above) on the server prior to use
D:\106748206.doc
Policy # MI/MD/v50
Microbiology Department
Policy & Procedure Manual
Section: Molecular Diagnostic Tests Manual
Page 52 of
291
VIII. References
RealStar BKV PCR Kit v1.0 Instructions, altona Diagnostics
PROCEDURE MANUAL
UNIVERSITY HEALTH NETWORK / MOUNT SINAI HOSPITAL MICROBIOLOGY DEPARTMENT
NOTE: This is a CONTROLLED document. Any documents appearing in paper form that are not stamped in red "MASTER COPY" are not controlled and
should be checked against the document (titled as above) on the server prior to use
D:\106748206.doc
Policy # MI/MD/v50
Microbiology Department
Policy & Procedure Manual
Section: Molecular Diagnostic Tests Manual
Page 53 of
291
Chlamydia trachomatis and Neisseria gonorrhoeae PCR by Cobas®
I.
Introduction
Chlamydia are gram-negative, non-motile bacteria consisting of four reported species.
Chlamydia trachomatis (CT) is the most frequently reported bacterial sexually
transmitted disease, and the second most leading cause of sexually transmitted disease
worldwide. CT can cause a variety of diseases in men and has severe consequences for
women if left untreated. It also can cause severe complications to pregnant women and
their child.
Neisseria gonorrhoeae are gram-negative diplococci and the causative agent of
gonorrhoeae. In women the primary site of infection is the endocervix, and can cause
conjunctivitis in infants with infected mothers.
The Cobas® 4800 CT/NG is an in vitro nucleic acid amplification test for the qualitative
detection of Chlamydia trachomatis (CT) and/or Neisseria gonorrhoeae (NG) in patient
specimens. The Cobas® 4800 CT/NG assay includes targets for all fifteen of the major
Chlamydia trachomatis serotypes, and both wild type and variant sequences of Neisseria
gonorrhoreae. The test utilizes amplification of target DNA be the Polymerase Chain
Reaction (PCR) followed by nucleic acid hybridization for the detection of CT and NG
DNA in a variety of specimens including, endocervical swabs, vaginal swabs, and urine
samples collected in Cobas® PCR media.
II.
Specimen Collection and Processing
a. Cobas® PCR Female Swab Kit
For endocervical, cervical and vaginal swab specimens
Transport at 2-30ºC. Endocervical specimens can be stored at 2-30ºC for up to 12
months, and cerivcal/vaginal swabs can be stored at 2-30ºC for 90 days once
samples have been stabilized in Cobas® PCR media.
Endocervical swab and vaginal swab specimens containing a SINGLE swab in the
cobas® PCR Media tube can be directly processed on the cobas® 4800 System.
A properly collected endocervical swab and vaginal swab specimen should have a
single swab with the shaft broken at the scoreline. Swab shafts which are broken
above the scoreline will appear longer than normal and may also be bent over to fit
into the cobas® PCR Media tube. This can produce an obstruction to the system
which may cause the loss of test results. In the event that a swab specimen has
an improperly broken shaft, remove the swab prior to sample processing on
the cobas x 480 instrument.
Do not process endocervical and vaginal swab specimens that appear bloody or
have a dark brown color. Compare the swab against 5% (v/v) whole blood standard.
PROCEDURE MANUAL
UNIVERSITY HEALTH NETWORK / MOUNT SINAI HOSPITAL MICROBIOLOGY DEPARTMENT
NOTE: This is a CONTROLLED document. Any documents appearing in paper form that are not stamped in red "MASTER COPY" are not controlled and
should be checked against the document (titled as above) on the server prior to use
D:\106748206.doc
Policy # MI/MD/v50
Microbiology Department
Policy & Procedure Manual
Section: Molecular Diagnostic Tests Manual
Page 54 of
291
b. Cobas® PCR Urine Sample Kit
Transport at 2-30ºC. Urine specimens can be stored at 2-30ºC for up to 12 months
once the specimens have been stabilized in Cobas® PCR media.
Do not process urine specimens that appear bloody or have a dark brown color.
Compare the urine against 0.35% (v/v) whole blood standard.
*Note: Specimens in Cobas® PCR media must be brought to room temperature for at
least 30 minutes before loading on to the cobas x 480 instrument.
III.
Procedure
Reagents:
a) Cobas® 4800 System Sample Preparation Kit - 240/960 test kits
Magnetic glass particles (MGP)
Elution buffer (EB)
b) Cobas® 4800 System Wash Buffer Kit – 240/960 test kits
Wash Buffer
c) Cobas® 4800 CT/NG Amplification/Detection Kit – 240/960 test kits
Master Mix (CT/NG MMX)
Manganese Solution (CT/NG Mn)
d) Cobas® 4800 System Control Diluent Kit
e) Cobas® 4800 CT/NG Controls Kit
Positive Control
Negative Control
Internal Control
f) Reagent Reservoirs – 50mL and 200 mL containers
g) CO-RE pipette tips
h) Plate carrier
i) Tip carrier
j) Sample and reagent racks
*Note: All reagents except CT/NG Master Mix and CT/NG Manganese solution must be
brought to room temperature before loading on the cobas x 480 instrument. CT/NG
Master Mix and CT/NG Manganese solutions must be removed from 2-8ºC just prior to
loading on the cobas x 480 instrument.
PROCEDURE MANUAL
UNIVERSITY HEALTH NETWORK / MOUNT SINAI HOSPITAL MICROBIOLOGY DEPARTMENT
NOTE: This is a CONTROLLED document. Any documents appearing in paper form that are not stamped in red "MASTER COPY" are not controlled and
should be checked against the document (titled as above) on the server prior to use
D:\106748206.doc
Policy # MI/MD/v50
Microbiology Department
Policy & Procedure Manual
Section: Molecular Diagnostic Tests Manual
Page 55 of
291
Sample Processing:
1. Turn on the system as the following sequence:
cobas z 480; Heater/Shaker unit ; cobas x 480 instrument
2. When the left orange light on the z 480 turns to solid green, turn on the computer
workstation.
3. Remove Cobas® Sample Preparation Kit and System Preparation Kit reagents
from fridge, and allow reagents to come to room temperature
4. Logon to the cobas 4800 software
User ID: LABOPERATOR
Password: 00labOPR
5. Perform instrument maintenance:
a. Select Overview tab and check maintenance status of the cobas x 480
instrument.
If weekly maintenance is due, click Run Weekly Maintenance.
If daily maintenance is due, click Run Daily Maintenance.
b. Follow the online instructions.
6. Start new run
a. After the completion of the maintenance, in the overview tab, click New Run
Tab on the right hand vertical bar
b. The following window pops up. Select test type: CT/NG workflow.
c.
d.
Type run name (optional).ie: CTNG 2012.05.29-1
Click OK.
PROCEDURE MANUAL
UNIVERSITY HEALTH NETWORK / MOUNT SINAI HOSPITAL MICROBIOLOGY DEPARTMENT
NOTE: This is a CONTROLLED document. Any documents appearing in paper form that are not stamped in red "MASTER COPY" are not controlled and
should be checked against the document (titled as above) on the server prior to use
D:\106748206.doc
Policy # MI/MD/v50
Microbiology Department
Policy & Procedure Manual
Section: Molecular Diagnostic Tests Manual
Page 56 of
291
7. Refer to the following figure while you are loading the deck:
E-plate
Holder
Tip Rack
Holder
Dynamic Loading
AD-plate
Holder
Plate Carrier
Track 1-6
Tip Rack
Holder
Tip Rack Carrier
Track 11-16
Sample Loading Area
Track 17-34
Tip Rack Carrier
Track 35-40
Reservoirs Reagent
Track
Track
48-50
51
8. Load samples
a. Decap samples.
b. Place samples on corresponding carrier.
c. Insert sample carriers on autoload tray when the LEDs for the designated track (1734) are flashing.
d. Click Load Samples
PROCEDURE MANUAL
UNIVERSITY HEALTH NETWORK / MOUNT SINAI HOSPITAL MICROBIOLOGY DEPARTMENT
NOTE: This is a CONTROLLED document. Any documents appearing in paper form that are not stamped in red "MASTER COPY" are not controlled and
should be checked against the document (titled as above) on the server prior to use
D:\106748206.doc
Policy # MI/MD/v50
Microbiology Department
Policy & Procedure Manual
Section: Molecular Diagnostic Tests Manual
Page 57 of
291
9. Load consumables
a) Place listed consumables on appropriate carriers.
Both tip carriers are fully filled and barcodes facing the right hand side
Ensure deepwell plate is loaded flatly and properly –barcode facing the right hand
side
Ensure microwell plate is loaded flat and properly (barcode facing away from you)
b) Insert carriers on autoload tray.
c) Click Load Consumables.
10. Load reagents
a) 200 mL reagent reservoir carrier
Load Wash Buffer on 200 mL reagent reservoir carrier as indicated in the wizard
(scan-scan-pour).
Insert carrier on autoload tray.
Click Load Reagents.
b) 50 mL reagent reservoir carrier
PROCEDURE MANUAL
UNIVERSITY HEALTH NETWORK / MOUNT SINAI HOSPITAL MICROBIOLOGY DEPARTMENT
NOTE: This is a CONTROLLED document. Any documents appearing in paper form that are not stamped in red "MASTER COPY" are not controlled and
should be checked against the document (titled as above) on the server prior to use
D:\106748206.doc
Policy # MI/MD/v50
Microbiology Department
Policy & Procedure Manual
Section: Molecular Diagnostic Tests Manual
Page 58 of
291
Load reagents on 50 mL reagent reservoir carrier as indicated in the wizard.(scan-scanpour).
vortex MGP for 10s prior to scan
Insert carrier on autoload tray.
Click Load Reagents.
c) Reagent carrier
Take out CT/NG MMX and CT/NG Mn from the clean room
Open reagent vials and load them on reagent carrier as indicated in the wizard.
Change gloves after uncapping positive control
Insert carrier on autoload tray.
Click Load Reagents.
11. Start sample preparation run
a) Click Start Run.
b) The sample preparation starts.
c) Check the timer in the wizard
PROCEDURE MANUAL
UNIVERSITY HEALTH NETWORK / MOUNT SINAI HOSPITAL MICROBIOLOGY DEPARTMENT
NOTE: This is a CONTROLLED document. Any documents appearing in paper form that are not stamped in red "MASTER COPY" are not controlled and
should be checked against the document (titled as above) on the server prior to use
D:\106748206.doc
Policy # MI/MD/v50
Microbiology Department
Policy & Procedure Manual
Section: Molecular Diagnostic Tests Manual
Page 59 of
291
12. Unload and seal micro plate.
a) Click Sample Prep Results to review the results of the sample preparation.
b) Click Unload.
c) Seal the micrwell oplate sealing foil applicator as indicated on screen.
Be sure not to touch the cover with your fingers as it may affect detection. Hold
the sides of the plate and use the smoothing applicator provided to properly seal.
The plate must be transferred from the cobas x 480 to the cobas z 480 within 90
minutes of completion
d) Click NEXT
13. Load mirowell plate on cobas z 480 analyzer.
a) Press load button on the cobas z 480 analyzer.
b) Place the sealed microwell plate into the extended loader.
PROCEDURE MANUAL
UNIVERSITY HEALTH NETWORK / MOUNT SINAI HOSPITAL MICROBIOLOGY DEPARTMENT
NOTE: This is a CONTROLLED document. Any documents appearing in paper form that are not stamped in red "MASTER COPY" are not controlled and
should be checked against the document (titled as above) on the server prior to use
D:\106748206.doc
Policy # MI/MD/v50
Microbiology Department
Policy & Procedure Manual
Section: Molecular Diagnostic Tests Manual
Page 60 of
291
c) Press load button again.
d) The amplification and detection run starts automatically.
e) Check the timer in the wizard.
14. Remove used reagents, samples, and deepwell plate from the cobas x 480 instrument.
15. Review and accept results.
a) Click Show Results.
b) Review and accept results in Results work area.
Do NOT accept FAILED results
c) Select results and click to print the results report.
16. Unload the cobas z 480 analyzer.
PROCEDURE MANUAL
UNIVERSITY HEALTH NETWORK / MOUNT SINAI HOSPITAL MICROBIOLOGY DEPARTMENT
NOTE: This is a CONTROLLED document. Any documents appearing in paper form that are not stamped in red "MASTER COPY" are not controlled and
should be checked against the document (titled as above) on the server prior to use
D:\106748206.doc
Policy # MI/MD/v50
Microbiology Department
Policy & Procedure Manual
Section: Molecular Diagnostic Tests Manual
Page 61 of
291
IV. Interpretation of Results
All assay and run validation is determined by the Cobas® 4800 software. Controls must be run
with each sample run and valid results must be obtained for both the positive and negative
control in order for sample results to be displayed.
Cobas® 4800 CT/NG Test
Interpretation
CT POS, NG POS
Specimen is positive for both CT and NG DNA
CT NEG, NG NEG
Neither CT or NG DNA could be detected
CT POS, NG NEG
or
CT NEG, NG POS
Specimen is positive for CT DNA
Invalid or Failed Results
V.
Specimen is positive for NG DNA
Do not accept the result from cobasX480. Refer to the trouble
shooting.
Troubleshooting
X3:
Error Clot Detected
1. Check the sample for clots.
2. If swab is present, votex 30 seconds and remove
swab from the sample.
3. Rerun the sample
X4:
Error Processing of the
sample was aborted due to
one or more pipetting error(s)
1. Make sure that the sample must have a minimum
volume of 1.0mL.
2. If swab is present, remove it.
Internal Control fails on ONE
specimen
Repeat specimen
Internal Control fails on a
specimen for the second time
Result specimen as: Invalid
In result comment: hit F5 to add comment “@SPIN”
“Likely due to specimen integrity, unable to obtain
valid test result after repeated attempts)”.
Verify result.
PROCEDURE MANUAL
UNIVERSITY HEALTH NETWORK / MOUNT SINAI HOSPITAL MICROBIOLOGY DEPARTMENT
NOTE: This is a CONTROLLED document. Any documents appearing in paper form that are not stamped in red "MASTER COPY" are not controlled and
should be checked against the document (titled as above) on the server prior to use
D:\106748206.doc
Policy # MI/MD/v50
Microbiology Department
Policy & Procedure Manual
Section: Molecular Diagnostic Tests Manual
VI.
Page 62 of
291
Reporting
Positive report:
* Chlamydia Detection – Urine
by Cobas 4800 CT/NG Assay
* N. gonorrhoeae Detection – Urine
by Cobas 4800 CT/NG Assay
Positive
* Chlamydia Detection – Urine
by Cobas 4800 CT/NG Assay
* N. gonorrhoeae Detection – Urine
by Cobas 4800 CT/NG Assay
Negative
* Chlamydia Detection – Cervical
by Cobas 4800 CT/NG Assay
* N. gonorrhoeae Detection – Cervical
by Cobas 4800 CT/NG Assay
Positive
Chlamydia Detection – Cervical
by Cobas 4800 CT/NG Assay
* N. gonorrhoeae Detection – Cervical
by Cobas 4800 CT/NG Assay
Negative
Chlamydia Detection – Semen
by Cobas 4800 CT/NG Assay
* N. gonorrhoeae Detection – Semen
by Cobas 4800 CT/NG Assay
Positive
Chlamydia Detection – Semen
by Cobas 4800 CT/NG Assay
* N. gonorrhoeae Detection – Semen
by Cobas 4800 CT/NG Assay
Negative
Negative report:
* Chlamydia Detection – Urine
by Cobas 4800 CT/NG Assay
* N. gonorrhoeae Detection – Urine
by Cobas 4800 CT/NG Assay
* Chlamydia Detection – Cervical
by Cobas 4800 CT/NG Assay
* N. gonorrhoeae Detection – Cervical
by Cobas 4800 CT/NG Assay
Negative
Positive
Negative
Positive
Negative
Positive
Negative
Negative
Negative
Negative
PROCEDURE MANUAL
UNIVERSITY HEALTH NETWORK / MOUNT SINAI HOSPITAL MICROBIOLOGY DEPARTMENT
NOTE: This is a CONTROLLED document. Any documents appearing in paper form that are not stamped in red "MASTER COPY" are not controlled and
should be checked against the document (titled as above) on the server prior to use
D:\106748206.doc
Policy # MI/MD/v50
Microbiology Department
Policy & Procedure Manual
Section: Molecular Diagnostic Tests Manual
* Chlamydia Detection – Semen
by Cobas 4800 CT/NG Assay
* N. gonorrhoeae Detection – Semen
by Cobas 4800 CT/NG Assay
VI.
Page 63 of
291
Negative
Negative
Quality Control
One Positive Control and one Negative Control must be included in each run.
Run external control (Accurun 341)) first week of each month and before a new reagent is put in
service and after the instrument is calibrated or services. Result filed in Reagent Lot Binder.
If any of these two controls fails, the test is invalid. Should inform Senior/Charge
technologists and repeat testing.
External proficiency testing is provided by CAP and QMP-LS.
Maintenance QC:
VII.
Reference
Package insert for Roche 4800 CT/NG Assay and Operators Manual
PROCEDURE MANUAL
UNIVERSITY HEALTH NETWORK / MOUNT SINAI HOSPITAL MICROBIOLOGY DEPARTMENT
NOTE: This is a CONTROLLED document. Any documents appearing in paper form that are not stamped in red "MASTER COPY" are not controlled and
should be checked against the document (titled as above) on the server prior to use
D:\106748206.doc
Policy # MI/MD/v50
Microbiology Department
Policy & Procedure Manual
Section: Molecular Diagnostic Tests Manual
Page 64 of
291
Clostridium difficile toxin B gene PCR by Cepheid GeneXpert
I. Introduction
The Cepheid Xpert C. difficile Assay, performed on the Cepheid GeneXpert® Dx System, is a
qualitative in vitro diagnostic test for rapid detection of toxin B gene sequences from unformed
(liquid or soft) stool specimens collected from patients suspected of having Clostridium difficile
infection (CDI). The test utilizes automated real-time polymerase chain reaction (PCR) to detect
toxin gene sequences associated with toxin producing C. difficile. The Xpert C. difficile Assay is
intended as an aid in the diagnosis of CDI. Concomitant culture is necessary only if further typing or
organism recovery is required.
II.
Specimen Collection and Processing
Collect unformed stool specimen in a clean Starplex container, and send to the Virology laboratory
as soon as possible. Stool collected in Enteric Transport Medium, or in SAF is not suitable for this
assay. The specimen is stable for up to 5 days when stored at 2–8°C. Alternatively, specimens can
be kept at room temperature (20 – 30 °C) for up to 24 hours.
Eswab rectal samples may be used for testing for Infection Control purposes upon request by
Infection Control Practioners.
III.
Materials & Equipment
GeneXpert Dx System
Vortex mixer
Dry swab for transfer of the specimen, such as the swab found in the Cepheid Sample
Collection Device 900-0370 (Copan Venturi Transystem® Culture) or the Copan Dual Swab and
Transport System.
Disposable transfer pipettes.
Xpert C. difficile kit – each kit contains 10 or 120 Xpert C. difficile cartridges and buffer
PROCEDURE MANUAL
UNIVERSITY HEALTH NETWORK / MOUNT SINAI HOSPITAL MICROBIOLOGY DEPARTMENT
NOTE: This is a CONTROLLED document. Any documents appearing in paper form that are not stamped in red "MASTER COPY" are not controlled and
should be checked against the document (titled as above) on the server prior to use
D:\106748206.doc
Policy # MI/MD/v50
Microbiology Department
Policy & Procedure Manual
Section: Molecular Diagnostic Tests Manual
Page 65 of
291
Each Xpert C. difficile Assay Cartridge with integrated reaction tubes contain:
Bead 1 (freeze-dried)
Polymerase
dNTPs
BSA (bovine serum albumin)
Probe
Bead 2 (freeze-dried)
Primers
Probes
BSA
Bead 3 (freeze-dried)
Sample Processing Control (SPC) non-infectious sample preparation
control spores
Reagent 1 (Sodium Hydroxide)
Reagent 2 (Tris Buffer, EDTA, surfactants)
Xpert C. difficile reagent pouch
Sample Reagent (Guanidinium thiocyanate, surfactants)
IV. Procedure
GeneXpert Dx System
i) GeneXpert Cartridge Preparation
1. The disposable single-use GeneXpert DX cartridge holds the samples and reagents that
you want to process in the GeneXpert DX System. Do not reuse spent cartridges.
2. Store new GeneXpert DX cartridge at 2 – 28 °C. The cartridge and reagents are stable for
up to 7 days after the package has been opened.
3. The test must be started within 30 minutes of adding reagents to the cartridge.
PROCEDURE MANUAL
UNIVERSITY HEALTH NETWORK / MOUNT SINAI HOSPITAL MICROBIOLOGY DEPARTMENT
NOTE: This is a CONTROLLED document. Any documents appearing in paper form that are not stamped in red "MASTER COPY" are not controlled and
should be checked against the document (titled as above) on the server prior to use
D:\106748206.doc
Policy # MI/MD/v50
Microbiology Department
Policy & Procedure Manual
Section: Molecular Diagnostic Tests Manual
Page 66 of
291
4. Use one cartridge and one sample reagent vial for each stool sample that needs to be
tested. Label the cartridge with the corresponding sample ID barcode. Do not hold the
cartridge from the reaction tube.
5. Place a dry swab which came with the Cepheid Sample Collection Device into the
unformed stool sample. The swab does not need to be completely saturated.
6. Insert the swab into the elution vial containing the Sample Reagent.
Note: Use sterile gauze to minimize the risk of contamination.
7. Hold the swab by the stem near the rim of the vial, lift the swab a few millimeters from
the bottom of the tube and push the stem against the edge of the vial to break it. Make
sure the swab is short enough to allow the cap to close tightly.
8. Close the lid and vortex at high speed for 10 seconds.
9. Open the cartridge lid. Using a clean transfer pipette, transfer the entire contents of the
Sample Reagent into the “S” chamber of the Xpert C. difficile Assay cartridge.
10. Close the cartridge lid.
Figure 1. Xpert C. difficile cartridge (top view)
ii)
Assay Method:
1. Turn on the computer, and then turn on the GeneXpert Dx instrument. Log into windows
using the password “cphd”.
2. On the Windows® desktop, double-click the GeneXpert Dx shortcut icon.
3. Log on to the GeneXpert Dx System software using your user name and password, for
example (User Name: admin1, Password: admin1).
PROCEDURE MANUAL
UNIVERSITY HEALTH NETWORK / MOUNT SINAI HOSPITAL MICROBIOLOGY DEPARTMENT
NOTE: This is a CONTROLLED document. Any documents appearing in paper form that are not stamped in red "MASTER COPY" are not controlled and
should be checked against the document (titled as above) on the server prior to use
D:\106748206.doc
Policy # MI/MD/v50
Microbiology Department
Policy & Procedure Manual
Section: Molecular Diagnostic Tests Manual
Page 67 of
291
4. The Database Management dialog box appears on top of the GeneXpert Dx System
window once the system starts up. Click “NO” in the Database Management dialog box
if you do not want to perform any database management tasks.
5. If a test archive is overdue, the Test Archive Reminder dialog box appears. If you do not
want to archive click “No” and if you do want to archive click “Yes”.
6. In the GeneXpert Dx System window, click Create Test. The Scan Sample ID Barcode
dialog box appears. Scan the Sample ID barcode using the barcode scanner or you can
manually enter the sample ID by clicking “Manual Entry”. Type in the Sample ID into
the Manually Patient ID Barcode Entry dialog box that appears.
7. Scan the barcode on the Xpert C. difficile Assay cartridge. The Create Test window
appears. Using the barcode information, the software automatically fills in the boxes for
the following fields: Select Assay, Reagent Lot ID, Cartridge SN, and Expiration Date.
8. Click Start Test. In the Create Test dialog box that appears. In the Check Status
Window, the selected instrument module progress changes to Waiting.
9. Open the instrument module door with the blinking green light and load the cartridge.
10. Close the door. The test starts and the green light stops blinking.
11. When the test is complete the instrument module door unlocks and the green light turns
off. Wait until the system releases the door lock before opening the module door and
removing the cartridge.
12. Dispose of the used cartridge in an appropriate specimen waste container.
13. Once testing is complete the report is automatically printed. To view the result, in the
GeneXpert DX System window, click View Results on the menu bar. The View Results
window appears.
14. Click View Test. The Select Test To Be Viewed dialog box appears. Select the test of
interest and click OK. The results of the selected test appear in the View Results
window.
15. The View Results window contains three tabs: Results, Errors, and Support. The
Results tab displays the information for a test such as the Patient ID, Sample ID, Assay
name and the test Result. The Errors tab list the errors encountered during the test
process.
PROCEDURE MANUAL
UNIVERSITY HEALTH NETWORK / MOUNT SINAI HOSPITAL MICROBIOLOGY DEPARTMENT
NOTE: This is a CONTROLLED document. Any documents appearing in paper form that are not stamped in red "MASTER COPY" are not controlled and
should be checked against the document (titled as above) on the server prior to use
D:\106748206.doc
Policy # MI/MD/v50
Microbiology Department
Policy & Procedure Manual
Section: Molecular Diagnostic Tests Manual
Page 68 of
291
16. Monthly Maintenance Procedure:
a. Disinfect the instrument surfaces
1. Dampen a paper towel with 10% bleach solution and wipe the instrument
surface thoroughly with the paper towel.
2. Wait 10 minutes
3. Dampen a paper towel with 70% alcohol solution and wipe the instrument
thoroughly with the paper towel.
b. Disinfect the cartridge bay interior
1. Dip a swab into 10% bleach solution. Press the swab against the inside
wall of the container to remove excess solution.
2. Open the instrument module door.
3. Wipe the surfaces inside the cartridge bay with the swab. Do not touch
the slit on the I-CORE module into which the cartridge reaction tube is
inserted.
4. Wait 10 minutes
5. Dip a new swab into 70% alcohol solution. Press the swab against the
wall of the container to remove excess solution.
6. Wipe the same surface with the new swab.
7. Repeat steps 5 and 6 two times.
8. Close the instrument module door.
c. Disinfecting the plunger rod
1. In the GeneXpert DX System window, click Maintenance on the menu
bar. The Maintenance window appears.
2. On the Maintenance menu, click Plunger Maintenance. The Plunger
Maintenance dialog box appears.
3. In the Module table, select the module you want to clean, and then click
Clean or select Clean All to clean all modules simultaneously. The
Plunger Cleaning dialog box then appears.
4. Follow the directions in the Plunger Cleaning dialog box, then click OK.
In the Plunger Maintenance dialog box, the Clean button changes to
Move Up (if you clicked Clean All button, it changes to Move Up All). In
the instrument, the plunger rod in the selected module (or all modules if
you clicked Clean All button) lowers into the cartridge bay.
5. Dip a number of swabs in the 10% bleach solution. Press the swabs
against the inside wall of the container to remove excess solution.
PROCEDURE MANUAL
UNIVERSITY HEALTH NETWORK / MOUNT SINAI HOSPITAL MICROBIOLOGY DEPARTMENT
NOTE: This is a CONTROLLED document. Any documents appearing in paper form that are not stamped in red "MASTER COPY" are not controlled and
should be checked against the document (titled as above) on the server prior to use
D:\106748206.doc
Policy # MI/MD/v50
Microbiology Department
Policy & Procedure Manual
Section: Molecular Diagnostic Tests Manual
Page 69 of
291
6. Wipe the plunger rods with the swabs. Use a fresh swab for each plunger
rod.
7. Wait 5 minutes
8. Dip a number of swabs into 70% alcohol solution. Press the swabs against
the inside wall of the container to remove excess solution.
9. Wipe the plunger rods with the swabs. Use a fresh swab for each plunger
rod.
10. Repeat steps 8 and 9 two times.
11. In the Plunger Maintenance dialog box, click Move Up (or Move Up All).
The plunger rod moves back into its resting position.
12. Click Close to dismiss the Plunger Maintenance dialog box.
d. Clean fan filters
17. The GeneXpert DX instrument needs to be recalibrated annually or after 2000 test per
instrument module, whichever comes first. The system monitors the number of tests
since last calibration. To check whether the system requires calibration:
1. In the Maintenance window, look at the ICORE Starts Since Cal
column. On the Maintenance menu, click Module Reports. The Module
Reports dialog box appears.
2. Check the calibration date. If calibration is required contact the Cepheid
Technical Support to schedule a calibration.
IV.
Assay validation
Each test includes a Sample Processing Control (SPC) and Probe Check Control (PCC):
1. Sample Processing Control (SPC) — ensures the sample was correctly processed. The
SPC contains spores of Bacillus globigii in the form of a dry spore cake that is included
in each cartridge to verify adequate processing of the sample bacteria. The SPC verifies
that lysis of C. difficile bacteria and a spore have occurred, if the organism is present, and
verifies that specimen processing is adequate. Additionally, this control detects specimenassociated inhibition of the real-time PCR assay. The SPC should be positive in a
negative sample and can be negative or positive in a positive sample. The SPC passes if it
meets the validated acceptance criteria.
PROCEDURE MANUAL
UNIVERSITY HEALTH NETWORK / MOUNT SINAI HOSPITAL MICROBIOLOGY DEPARTMENT
NOTE: This is a CONTROLLED document. Any documents appearing in paper form that are not stamped in red "MASTER COPY" are not controlled and
should be checked against the document (titled as above) on the server prior to use
D:\106748206.doc
Policy # MI/MD/v50
Microbiology Department
Policy & Procedure Manual
Section: Molecular Diagnostic Tests Manual
Page 70 of
291
2. Probe Check Control (PCC) — Before the start of the PCR reaction, the GeneXpert Dx
System measures the fluorescence signal from the probes to monitor bead rehydration,
reaction-tube filling, probe integrity and dye stability. Probe Check passes if it meets the
assigned acceptance criteria.
V.
Interpretation of Results
The results are interpolated by the GeneXpert Dx System from measured fluorescent signals
and embedded calculation algorithms and will be shown in the View Results window.
Possible results are:
1. Toxigenic C. difficile POSITIVE
Toxin producing C. difficile target DNA sequences are detected.
The toxin producing C. difficile target(s) have Cts within the valid range and endpoint
above the minimum setting.
SPC — NA (not applicable); SPC is ignored since C. difficile target amplification
may compete with this control
Probe Check – PASS; all probe check results pass.
2. Toxigenic C. difficile NEGATIVE with no Critical Threshold (ct) or Endpoint
C. difficile target DNA sequences are not detected.
Toxin producing C. difficile targets not detected.
SPC — PASS; SPC has a Ct within the valid range and endpoint above the endpoint
minimum setting.
Probe Check — PASS; all probe check results pass.
3. Toxigenic C. difficile NEGATIVE with Critical Threshold (ct) or Endpoint
(INDETERMINATE)
C. difficile target DNA sequences are detected but not sufficient to trigger a POS
result.
The GeneXpert test report gives a non-zero numeric value under ct or >10 under
EndPt for Toxin B yet the Analyte Result is NEG
LIS will trigger a ?END: SIG although test is “NEG” in the test result window to
notify of an indeterminate result.
All such stools should be frozen (7 vials)
PROCEDURE MANUAL
UNIVERSITY HEALTH NETWORK / MOUNT SINAI HOSPITAL MICROBIOLOGY DEPARTMENT
NOTE: This is a CONTROLLED document. Any documents appearing in paper form that are not stamped in red "MASTER COPY" are not controlled and
should be checked against the document (titled as above) on the server prior to use
D:\106748206.doc
Policy # MI/MD/v50
Microbiology Department
Policy & Procedure Manual
Section: Molecular Diagnostic Tests Manual
Page 71 of
291
4. INVALID
Presence or absence of C. difficile target DNA cannot be determined
SPC — FAIL; SPC target result is negative and the SPC Ct is not within valid range
and endpoint below minimum setting.
Probe Check — PASS; all probe check results pass.
The sample was not properly processed or PCR was inhibited.
Inform Virology Charge/ Senior and repeat the test according to the following
retesting procedure below.
5. ERROR
Presence or absence of C. difficile cannot be determined.
Toxin producing C. difficile targets — NO RESULT
Probe Check — FAIL*; one or more of the probe check results fail.
If the probe check passed, possible causes for the error include: the reaction tube was
filled improperly; a reagent probe integrity problem was detected; or the maximum
pressure limits exceeded the acceptable range.
Inform Virology Charge/ Senior and repeat the test according to the following
retesting procedure below.
6. NO RESULT
Indicated that insufficient data were collected, the presence or absence of C.difficile
cannot be determined.
Possible causes include the operator stopping the test will it was in progress.
Inform Virology Charge/ Senior and repeat the test according to the following
procedure below.
retesting
PROCEDURE MANUAL
UNIVERSITY HEALTH NETWORK / MOUNT SINAI HOSPITAL MICROBIOLOGY DEPARTMENT
NOTE: This is a CONTROLLED document. Any documents appearing in paper form that are not stamped in red "MASTER COPY" are not controlled and
should be checked against the document (titled as above) on the server prior to use
D:\106748206.doc
Policy # MI/MD/v50
Microbiology Department
Policy & Procedure Manual
Section: Molecular Diagnostic Tests Manual
Page 72 of
291
Retesting Procedure
The test should be repeated if an “INVALID”, “ERROR” or “NO RESULT” result was
obtained.
To repeat a test within 3 hours of an “INVALID/ERROR/NO RESULTS” result:
1. Transfer the remaining contents from the S Chamber of the current Xpert C. difficile
Assay cartridge to a new Sample Reagent Vial using a disposal transfer pipette.
2. Vortex and add the entire contents of the Sample Reagent to Chamber S of a new
Xpert C. difficile Assay cartridge.
3. Close the lid and start new test
4. Follow LIS Instructions below VI. Reporting for “INVALID”, “ERROR” or “NO
RESULT”
To repeat a test after 3 hours of an “INVALID” result:
1.
Repeat the test with a new swab sample.
PROCEDURE MANUAL
UNIVERSITY HEALTH NETWORK / MOUNT SINAI HOSPITAL MICROBIOLOGY DEPARTMENT
NOTE: This is a CONTROLLED document. Any documents appearing in paper form that are not stamped in red "MASTER COPY" are not controlled and
should be checked against the document (titled as above) on the server prior to use
D:\106748206.doc
Policy # MI/MD/v50
Microbiology Department
Policy & Procedure Manual
Section: Molecular Diagnostic Tests Manual
VI.
Page 73 of
291
Reporting
From Xpert C. difficile Assay
Result
LIS Codes
Result Comments
Negative
?END: NSG
?NAP1: NEGATIVE
?CLD: NEG
Positive
?END: SIG
?NAP1: SIG or NEG
?CLD: ?DETECTED
Auto resulting TEST Comment:
}NCTB Negative
“Negative - No Clostridium difficile toxin B
gene detected by Cepheid Xpert C.
difficile/Epi assay. This assay has a negative
likelihood ratio between 0.03-0.06. A second
test does NOT significantly increase the
sensitivity or change the negative likelihood
ratio. (Ref: Eur J Clin Microbiol Infect Dis.
2013 Jan;32(1):97-9)
ISOLATE Comment:
“Clostridium difficile toxin B gene
DETECTED by PCR using Cepheid Xpert
C.difficile/Epi assay.
Note: Strain designation is provided for
Infection control reasons only.
1. In test window, pick ‘P’ from
keypad
2. Chose ‘1’ or ‘D’ from keypad
- ‘1’ will generate: ~^clodn-;
(C.diff pos, nap-1 neg)
- ‘D’ will generate: ~^clodn+;
(C.diff pos, nap-1 pos)
3. Verify Isolate,
Accept “YES” Pop Up Comment
Clodn+/- - ~\GXPT
Clodn+/- - ~\Cdif
4. Verify, Finalize, View & Save
5. Notify ward/ICP,
6. Add media FRZ, freeze 4 vials
PROCEDURE MANUAL
UNIVERSITY HEALTH NETWORK / MOUNT SINAI HOSPITAL MICROBIOLOGY DEPARTMENT
NOTE: This is a CONTROLLED document. Any documents appearing in paper form that are not stamped in red "MASTER COPY" are not controlled and
should be checked against the document (titled as above) on the server prior to use
D:\106748206.doc
Policy # MI/MD/v50
Microbiology Department
Policy & Procedure Manual
Section: Molecular Diagnostic Tests Manual
Indeterminate
These will print out as NEG but have
a endpoint >10.
?END: SIG
?NAP1: NEGATIVE
?CLD: NEG
1. In test window, pick ‘P’ from
keypad.
2. Chose ‘I’ from keypad
Page 74 of
291
ISOLATE Comment:
“INDETERMINATE for C.difficile toxin B
gene by PCR using Cepheid Xpert
C.difficile/Epi Assay. This result indicates
either C. difficile toxin B gene at low
concentrations or a false positive result.
Clinical correlation is required. If you have
any questions, please contact the Medical
Microbiologist on call.
3. Accept “YES” Pop Up Comment
cloptb - ~\Ceph
cloptb - ~\Cptb
cloptb - ~\Cdif
“INVALID”,
“ERROR” or
“NO RESULT”
4. Verify, Finalize all tests, View &
Save
5. Notify ward/ICP, freeze 7 vials
?END: ERROR
?NAP1: ERROR
?CLD: ERROR
1. To add repeat test media, under the
CLD test, click in the CLDT media
and press “R” in the keypad. This will
drop “CLDRP” repeat media.
2 .DO NOT remove any significant
flags
in Test Tab OR any results
until you receive the repeat result.
3. Once the second result is available ,
Report accordingly
4. Should the repeat test give another
Errot/Invalid/No result, DO NOT
SET UP AGAIN; Report as:
M- Not processed }Due to interfering
Upon repeat, if the second result is:
NEGATIVE
1.Remove the significant flag so it will not be
posted as abnormal.
2.Under all tests, delete “ERROR”. In
?CLD Use keypad 1 }NCDB Negative.
3.Finalize all test ?END,?NAP1 and CLD.
POSITIVE
1.DO NOT remove the significant flag.
2.Follow POSITIVE reporting instructions.
3.Finalize all test ?END,?NAP1 and CLD.
INDETERMINATE
1.DO NOT remove the significant flag
2.Follow INDETERMINATE reporting
instructions
3.Finalize all test ?END,?NAP1 and CLD.
INVALID, ERROR, NO RESULT
1. Remove the significant flag.
2. Delete “ERROR” and use keypad M Not
Processed} DUE to interfering
3.Finalize all test ?END,?NAP1 and CLD.
PROCEDURE MANUAL
UNIVERSITY HEALTH NETWORK / MOUNT SINAI HOSPITAL MICROBIOLOGY DEPARTMENT
NOTE: This is a CONTROLLED document. Any documents appearing in paper form that are not stamped in red "MASTER COPY" are not controlled and
should be checked against the document (titled as above) on the server prior to use
D:\106748206.doc
Policy # MI/MD/v50
Microbiology Department
Policy & Procedure Manual
Section: Molecular Diagnostic Tests Manual
Page 75 of
291
*Any ?ERROR comment in the CLD test window will trigger a “significant” flag (even after
saving and finalizing result). Delete any ?ERROR left in the CLD test window before finalizing
result.
Phone positive result to ward (in-patient) or physician (Out-patient), and also phone to Infection
Control Practitioner as per Isolate Notification and Freezing Table QPCMI15003.
Referred Result
Previous Result
Negative within 7 days
LIS Code
}PNEG PrevNeg
TEST Comment
“This patient has tested negative for C. difficile toxin
B gene within the past week. This assay has a
negative likelihood ratio between 0.03-0.06.
A second test does NOT significantly increase the
sensitivity or change the negative likelihood ratio.
(Ref: Eur J Clin Microbiol Infect Dis. 2013
Jan;32(1):97-9)
If your patient has NEW, ONGOING or
WORSENING signs/symptoms since the last test that
suggest C difficile infection, please contact the
Microbiologist-on-call to arrange repeat testing.”
Positive within 15 days
}CLD+ PrevPos
Indeterminate within 7
days
}IND+ PrevIND+
“This patient has tested positive for C. difficile toxin
B gene within the past 15 days.
Do not repeat C. difficile toxin testing unless the
patient has received a full course of treatment (14
days) and has developed recurrent signs/symptoms
of C. difficile. Repeat C. difficile toxin testing is not
indicated in patients who have clinically responded to
treatment.”
“This patient has tested indeterminate for C.difficile
toxin B gene within the past week. Indeterminate
results indicate either detection of low levels of
C.difficile toxin B gene or a false positive result.
If your patient has signs/symptoms consistent with
C.difficile infection, an indeterminate result most
likely reflects a low level positive result and the
test does not need to be repeated.If you would like
repeat testing for another reason, please contact
the Microbiologist-on-call.”
PROCEDURE MANUAL
UNIVERSITY HEALTH NETWORK / MOUNT SINAI HOSPITAL MICROBIOLOGY DEPARTMENT
NOTE: This is a CONTROLLED document. Any documents appearing in paper form that are not stamped in red "MASTER COPY" are not controlled and
should be checked against the document (titled as above) on the server prior to use
D:\106748206.doc
Policy # MI/MD/v50
Microbiology Department
Policy & Procedure Manual
Section: Molecular Diagnostic Tests Manual
Page 76 of
291
Rejected Samples
VII.
Rejection Criteria
Formed stool received
LIS Code
Formed}FSTL
TEST Comment
“Not Processed. Formed stool received. Test
cancelled.”
Rectal swab received
Rectal}RECT
Duplicate Orders
received in the same day
Specimen received in
SAF transport media
}DUPL ICATE
Charcoal Swab received
}CHAR coal received
Specimen received in
enteric pathogen
transport medium
Patient’s Age is less
than 1 year old
}CDTX ETT received
“Not Processed. Rectal swab received; unsuitable for
testing.Please resubmit a stool sample.”
“This is a duplicate order. This test has been
cancelled.”
“Not Processed. Specimen received in SAF (fixative
for parasite) and is unsuitable for Clostridium
difficile toxin testing. If you have any question,
please call the Microbiology lab.”
“Not Processed. Charcoal swab received is unsuitable
for this test.If you have any question, please call the
Microbiology lab.”
“Not Processed. Specimen received in enteric
pathogen transport medium.Unsuitable for C.difficile
testing. Please repeat.”
“Test not performed on patients less than one year of
age.”
}SAF received
}<1y Age
Quality Control
Each test includes a Sample Processing Control (SPC) and Probe Check Control (PCC). Refer to a
senior technologist if control results are outside of limits or for any other problems with running or
reporting the assay.
Run external control (C. difficile Toxin from Positive C. difficile culture) with each new lot, QC and
instrument problems. Result filed in External Control Binder. If result is negative, the run is invalid.
Inform Charge/senior technologist, and repeat testing.
CAP provides external proficiency testing.
VIII.
Reference
Xpert C.difficile PCR Assay package insert
PROCEDURE MANUAL
UNIVERSITY HEALTH NETWORK / MOUNT SINAI HOSPITAL MICROBIOLOGY DEPARTMENT
NOTE: This is a CONTROLLED document. Any documents appearing in paper form that are not stamped in red "MASTER COPY" are not controlled and
should be checked against the document (titled as above) on the server prior to use
D:\106748206.doc
Policy # MI/MD/v50
Microbiology Department
Policy & Procedure Manual
Section: Molecular Diagnostic Tests Manual
Page 77 of
291
Testing for C. difficile toxin from eSwab for Infection Control Purpose
Infection Control Practioners may request C. difficile on specimens collected in eSwab during
admission screening to rule out C. difficile infection prior to admission.
1. From a previously collected eSwab culture, place a new order in the LIS and order the C.
difficile toxin test
2. use the Cepheid instrument by the VRE bench so that automated results through the interface do
not occur
3. use 100 uL of eSwab liquid transport media for testing and follow the Procedure above
4. Report results as above with additional Comment:
“Note: This specimen type is not appropriate for C. difficile testing but has been tested for
infection control purposes only.”
PROCEDURE MANUAL
UNIVERSITY HEALTH NETWORK / MOUNT SINAI HOSPITAL MICROBIOLOGY DEPARTMENT
NOTE: This is a CONTROLLED document. Any documents appearing in paper form that are not stamped in red "MASTER COPY" are not controlled and
should be checked against the document (titled as above) on the server prior to use
D:\106748206.doc
Policy # MI/MD/v50
Microbiology Department
Policy & Procedure Manual
Section: Molecular Diagnostic Tests Manual
Page 78 of
291
Cytomegalovirus Quantitative PCR by Cobas® Ampliprep/TaqMan
I.
Introduction
Human cytomegalovirus (CMV) can cause severe, life threatening disease in immunocompromised
patients such as transplant patients, patients with HIV, and developing fetus. In conjunction with
clinical presentation and other lab markers, the quantitative CMV test can indicate clinical prognosis,
be used to monitor anti-viral treatment and manage CMV infection in patients at risk.
The quantitative CMV test is not intended for use as a screening test for CMV in blood, as a
diagnostic test to confirm the presence of CMV infection or in specimens other than human plasma.
®
®
The COBAS AmpliPrep/TaqMan CMV test is an in vitro nucleic acid amplification test for the
quantitation of CMV DNA in EDTA plasma using the AmpliPrep instrument for automated DNA
®
extraction and the TaqMan analyzer for automated amplification and detection. The test can
quantitate CMV DNA over the range of 150 - 10,000,000 copies/mL. One copy of CMV DNA (as
®
defined by TaqMan ) is equivalent to 0.91 International Unit (IU) [1.1 cp/IU] on the WHO Standard).
Below the lower limit of quantitation of 150 cp/mL, CMV DNA can be detected but its quantitation
cannot be accurately calculated.
The CMV QS, a non-infectious DNA construct, is added to each specimen at a known copy number to
compensate effects of inhibition, allowing a more accurate quantitation of CMV DNA in each
specimen The TaqMan Analyzer calculates the CMV DNA concentration in the test specimens by
comparing the CMV signal to the CMV QS signal for each specimen.
II.
Specimen Collection and Processing
Five to 10 mL of blood is collected in a sterile lavender top (EDTA) tube and is transported at 2-25oC
to the lab within 6 hours of collection.
In the lab, samples are centrifuged at 800-1600 g (3000 rpm in centrifuge MICT36) for 20 minutes.
Plasma is separated within 6 hours of collection into two storage tubes and put in CMV DNA’ box in –
20oC freezer.
Plasma specimens may be stored at 2-8°C for up to 7 days. Plasma specimens are stable for 6 weeks if
frozen at ≤-20°C. Plasma specimens may be frozen and thawed up to 3 times without a significant loss
of CMV DNA.
III. Materials and Instruementation:
Instruments:
Cobas Ampliprep Instruement
Cobas Taqman 48 Analyzer
Reagent Kit: Cobas Ampliprep/Cobas TaqMan CMV Test
PROCEDURE MANUAL
UNIVERSITY HEALTH NETWORK / MOUNT SINAI HOSPITAL MICROBIOLOGY DEPARTMENT
NOTE: This is a CONTROLLED document. Any documents appearing in paper form that are not stamped in red "MASTER COPY" are not controlled and
should be checked against the document (titled as above) on the server prior to use
D:\106748206.doc
Policy # MI/MD/v50
Microbiology Department
Policy & Procedure Manual
Section: Molecular Diagnostic Tests Manual
Page 79 of
291
Disposables:
Sample processing units: SPUs
Sample input tubes (S-tubes) with barcode clips
Racks of K-tips
Racks of K-tubes
Other materials:
Sample Rack (SK 24 rack)
Reagent Rack
SPU Rack
K-Carrier
K-Carrier Transporter
K-Carrier rack
IV. Procedure:
Start –up
1.
Turn Compter ON.
2.
Control-Alt-Delete
3.
To log onto Windows
a.
User name: aluser
b.
Password : aluser
4.
Click Amplilink icon
5.
To log onto amplilink
a.
User name: MSH (case sensitive)
b.
Password: Msh12345 (case sensitive)
6.
Check Wash Reagent Reservoir.
7.
Empty Waste container.
8.
Perform all maintenance in the “Service Due” tab and as listed below
9.
Clean glass cover of instrument.
10. Clean as per figure 1: Work surfaces of Ampliprep
11. Clean figure 2 and 3 on both heads
12. Clean Reagent tips on both heads
13. Clean loading panel
14. Clean Taqman
15. Taqman on
16. Record maintenance on maintenance worksheet.
PROCEDURE MANUAL
UNIVERSITY HEALTH NETWORK / MOUNT SINAI HOSPITAL MICROBIOLOGY DEPARTMENT
NOTE: This is a CONTROLLED document. Any documents appearing in paper form that are not stamped in red "MASTER COPY" are not controlled and
should be checked against the document (titled as above) on the server prior to use
D:\106748206.doc
Policy # MI/MD/v50
Microbiology Department
Policy & Procedure Manual
Section: Molecular Diagnostic Tests Manual
Page 80 of
291
Load Reagents
1.
Remove reagents from refrigerator
2.
Load CS1 on one Rack and insert into position A
If doing multiple assays, load enough CS1
cassettes for all runs. Be careful not to smudge the barcodes.
3.
Load Cassettes CS2, CS3 and CS4 onto another rack
and insert into positions B-E.
All reagents cassettes should be removed for the refrigerator and loaded immediately on to the
Ampliprep and allowed to come to room temperature on the instrument for at least 30 min. before the
first specimen is processed. Do not let the cassettes come to room temperature outside the instrument as
condensation may form on the barcode labels. Do not wipe off condensation if it appears on the barcode
labels.
Load Consumables
One sample processing unit (SPU), one Input sample tube (s-tube), one K-tip and one K-tube is needed
for each specimen and control.
1.
2.
3.
4.
Load SPU’s on positions J,K,L.
Check seating in rack; do not push on top of (S-tips)- only on sides
Load K-tips into positions M-P.
Place control Barcode clips on sample rack
1. HPC , 2. LPC ,3. Neg
Place new Barcode clips on sample rack for each sample being tested.
Create Order
1.
Click the orders button
2.
Select the Sample-Rack tab and click NEW
3.
Type the Sample rack ID in the Sample Rack ID box.
4.
Put the worklist # in the Batch ID box.
5.
Click the test button (CMVCAP48 for CMV).
6.
To identify the controls highlight then click the “S” in the sample type (T) column to select the
control types: CMV (-)C, CMV L(+)C and CMV H(+)C
7.
Highlight Sample ID on line 4
8.
Scan or enter Sample ID
9.
Repeat 7 and 8 for all samples
10.
Click save when finished.
PROCEDURE MANUAL
UNIVERSITY HEALTH NETWORK / MOUNT SINAI HOSPITAL MICROBIOLOGY DEPARTMENT
NOTE: This is a CONTROLLED document. Any documents appearing in paper form that are not stamped in red "MASTER COPY" are not controlled and
should be checked against the document (titled as above) on the server prior to use
D:\106748206.doc
Policy # MI/MD/v50
Microbiology Department
Policy & Procedure Manual
Section: Molecular Diagnostic Tests Manual
Page 81 of
291
Prepare Specimens
1.
Transfer 500 uL into an S-tube for each specimen and control. Close cap of S-tube finger tight.
Avoid contaminating the upper part of the S-tube with specimens or controls.
2.
Place K-tubes on Sample rack for each specimen.
3.
Check seating of Clips and S-tubes.
4.
Load Sample rack onto positions F, G or H.
Load K-Carrier
1.
Click the System button
2.
Select the Cobas Ampliprep instrument using the instrument Selection box.
3.
Click the Samples tab to display the Samples folder.
*Steps 4 and 5 must be completed within 5 seconds.
4.
Using the handheld barcode scanner, scan the K-carrier rack barcode.
5.
Scan the K-carrier barcode.
6.
Load the K-carrier rack containing the K-carrier in position O and P.
Start Ampliprep
1.
Check Status of Cassettes, Specimens and System by clicking on each tab
2.
Press start.
3.
Note the time when the run is completed on the worksheet.
End of Run
1.
Click the Messages button and examine for any error messages.
2.
Click the Systems button
3.
Examine the Samples folder – successfully processed samples are green
4.
Open the load panel
5.
Remove the K-carrier rack containing the processed samples.
Note: All processed specimens and controls should not be exposed to light.
Note: The K-carrier must be loaded into the Taqman within 2 hours of processing on the Ampliprep
Start Cobas TaqMan 48 Analyzer
1.
Select the Cobas TaqMan 48 Analyzer using the instrument Selection box.
2.
Select the System tab.
3.
Click Open for the thermal cycler to be loaded.
4.
Open the thermal cycler lid.
Balance the K-carrier if necessary.
5.
Using the K-carrier transporter, place the K-carrier in the thermal cylcer.
6.
Close the lid
7.
Choose Start.
8.
Store reagents for the Ampliprep in the refrigerator.
PROCEDURE MANUAL
UNIVERSITY HEALTH NETWORK / MOUNT SINAI HOSPITAL MICROBIOLOGY DEPARTMENT
NOTE: This is a CONTROLLED document. Any documents appearing in paper form that are not stamped in red "MASTER COPY" are not controlled and
should be checked against the document (titled as above) on the server prior to use
D:\106748206.doc
Policy # MI/MD/v50
Microbiology Department
Policy & Procedure Manual
Section: Molecular Diagnostic Tests Manual
Page 82 of
291
Remove instrument waste
1.
Remove used SPUs and S-tubes put in autoclave bag and seal it.
2.
Remove empty K-tip racks
3.
Remove Sample racks and dispose used bar-code clips
4.
Discard used K-tubes
Results interpretation
1.
Click Results button
2.
Select the Review tab
3.
Select the desired worklist under the batch ID column
4.
Examine the results
Double-click the results line to display detail
Check for flags and error messages
Click Measurement Details to view graph
Print graph of any _Q_QS_ INVALID, _S_Drift_High or any other unusual flag
and consult Senior Tech or Charge Tech.
5. Click Accept.
The K-carrier must be removed from the Taqman before results can be accepted.
6. Print Results Report
V. Reporting
Titre Result
Target Not Detected
<1.37E+02 IU/mL
Interpretation
No CMV DNA detected
CMV DETECTED, <137 IU/mL
>=1.37E+02 IU/mL
and <=9.10E+06 IU/mL
>9.10E+06 IU/mL
CMV, (# value) IU/mL
CMV, >9.10E+06 IU/mL
The conversion factor between CMV DNA copies/mL (as defined by COBAS® Ampliprep/
COBAS® Taqman ® CMV test) is 1.1cp/IU [0.91 IU/cp].
Note: Specimens that produce an invalid result with a flag “QS_INVALID” review the graph.
Repeat testing.
Once the results have been finalized a report is faxed to the BMT clinic using the LIS :
-Lab-Reports-Verified ResultsReports;
(remove checks from all items under print flags)
PROCEDURE MANUAL
UNIVERSITY HEALTH NETWORK / MOUNT SINAI HOSPITAL MICROBIOLOGY DEPARTMENT
NOTE: This is a CONTROLLED document. Any documents appearing in paper form that are not stamped in red "MASTER COPY" are not controlled and
should be checked against the document (titled as above) on the server prior to use
D:\106748206.doc
Policy # MI/MD/v50
Microbiology Department
Policy & Procedure Manual
Section: Molecular Diagnostic Tests Manual
Page 83 of
291
-put in date in Verification Date field
-in Ward field put “BMTCL”
-in the Test ID field put in “8CMVP”
-fax to BMT
VI. Quality Controls
One CMV (-)C, CMV L(+)C and CMV H(+)C
is included with each run. Each result must be within the set value for each Lot #, otherwise the
run is invalid.
Record these results on-line in the T-Drive under “Microbiology/Virology/CMV QC… Active”.
The results should be within mean ± 2.S.D., otherwise withhold reports and inform charge/senior
technologist for further review.
External QC:
Run external control with each new reagent lot and at least once a month. May also need to run
external QC after equipment / QC failures, consult charge/senior technologist.
Record these results on-line in the T-Drive under “Microbiology/Virology/CM QC… Active”.
The results should be within ± 2.S.D., otherwise withhold reports and inform charge/senior
technologist for further review.
External proficiency testing : Provided by National Microbiology Lab (NML).
Alternatively, send 2 samples to PHL for parallel testing (January and July).
Reference
Roche Diagnostics, Ampliprep Software Version 3.2, Application Manual Version 1.
PROCEDURE MANUAL
UNIVERSITY HEALTH NETWORK / MOUNT SINAI HOSPITAL MICROBIOLOGY DEPARTMENT
NOTE: This is a CONTROLLED document. Any documents appearing in paper form that are not stamped in red "MASTER COPY" are not controlled and
should be checked against the document (titled as above) on the server prior to use
D:\106748206.doc
Policy # MI/MD/v50
Microbiology Department
Policy & Procedure Manual
Section: Molecular Diagnostic Tests Manual
Page 84 of
291
Cytomegalovirus Qualitative PCR by Rotorgene
I.
Introduction
Human cytomegalovirus (CMV) can cause severe, life threatening disease in
immunocompromised patients such as transplant patients, patients with HIV, and developing
fetus. Quantitative CMV can be used to monitor the course of CMV infection during and after
treatment.
II.
Specimen Collection and Processing
Please refer to Nucleic Acid Extraction – Biomerieux NucliSENS easyMAG
III.
Materials, Equipments
Clean Room: dedicated Biosafety Cabinet (MIBCT4),
Designated clean room gowns and powder-free gloves
Designated Clean room Variable volume pipettes: 1 to 20 uL
10 to 200 uL
100 to 1000 uL
o
36 microtube Loading block pre-cooled to 4 C
72 microtube Loading block pre-cooled to 4oC
0.2mL microtubes/ or 0.1mL microtubes and Caps
Aersol Resistant Tips (ART)
Altona CMV PCR Kit 1.0, (stored at -20o C in clean room):
Master A (12 tests per vial)
Master B (12 tests per vial)
Internal Control (IC)
Water (PCR grade)
Specimen Preparation area: Variable volume pipettes: 1 to 20 uL
10 to 200 uL
100 to 1000 uL
o
Altona CMV PCR Kit 1.0, (stored at -20 C in clean room):
QS1 (10^4 Copies/µL)
QS2 (10^3 Copies/µL)
QS3 (10^2 Copies/µL)
QS4 (10^1 Copies/µL)
External Control: To be run when a new lot is used, during training or if QC failure
occurs.
PROCEDURE MANUAL
UNIVERSITY HEALTH NETWORK / MOUNT SINAI HOSPITAL MICROBIOLOGY DEPARTMENT
NOTE: This is a CONTROLLED document. Any documents appearing in paper form that are not stamped in red "MASTER COPY" are not controlled and
should be checked against the document (titled as above) on the server prior to use
D:\106748206.doc
Policy # MI/MD/v50
Microbiology Department
Policy & Procedure Manual
Section: Molecular Diagnostic Tests Manual
Page 85 of
291
Detection Area: Rotorgene 6000 Multiplexing System programmed with ALTONA CMV PCR
36-Well Rotor with Locking Ring/ or 72-Well Rotor with Locking Ring
GENERAL PRECAUTIONS:
There must be designated separate PCR work areas: 1. Clean Room
2. Specimen preparation area
3. Detection (Amplification) Area
Supplies and equipment must be dedicated to each PCR work area.
Use only aerosol resistant tips (ART).
Work with powder-free gloves; change gloves frequently.
Follow cleaning instructions outlined on daily maintenance schedules.
IV.
DETECTION SET UP:
Organize CMV eluates and store at 4oC until ready to load.
Clean Room: (Change into dedicated clean room gown and gloves, work in Biosafety Cabinet)
a. Take out the necessary number of CMV Master Mix A and B vials (12 tests per vial) from
the -20C freezer, quickly and thoroughly thaw inside the Biosafety Cabinet. Prepare
CMV Master Mix (number of samples + controls + 1 extra test) required according to
the chart. Mix gently, do not vortex.
PROCEDURE MANUAL
UNIVERSITY HEALTH NETWORK / MOUNT SINAI HOSPITAL MICROBIOLOGY DEPARTMENT
NOTE: This is a CONTROLLED document. Any documents appearing in paper form that are not stamped in red "MASTER COPY" are not controlled and
should be checked against the document (titled as above) on the server prior to use
D:\106748206.doc
Policy # MI/MD/v50
Microbiology Department
Policy & Procedure Manual
Section: Molecular Diagnostic Tests Manual
No. of samples
1
2
3
4
5
6
7
8
9
10
11
12
Page 86 of
291
Preparation of Master Mix
Master A (µl)
5
10
15
20
25
30
35
40
45
50
55
60
Master B (µl)
15
30
45
60
75
90
105
120
135
150
165
180
b. Place proper number of microtubes for each sample, Controls (Positive and Negative) into
the Cooling Block (pre-cooled to 4oC).
c. Pipette 20 uL prepared CMV Master Mix (A+B) into each microtubes. Lightly cap
sample microtubes.
d. Pipette 1.0 uL of internal control into the microtubes designated for the Positive control
(CMV QS3) and the Negative control.
e. Pipette 10uL water (PCR grade) into the negative control microtube and cap tightly.
Number microtube lids.
f. Changed out of dedicated clean room gown.
Specimen Processing Area:
a. Carefully pipette 10uL of each sample eluate, and Positive Control (CMV QS3), into designated
numbered microtube containing CMV Master Mix. Gently mix by pipetting up and down. Close
the lid tightly.
PROCEDURE MANUAL
UNIVERSITY HEALTH NETWORK / MOUNT SINAI HOSPITAL MICROBIOLOGY DEPARTMENT
NOTE: This is a CONTROLLED document. Any documents appearing in paper form that are not stamped in red "MASTER COPY" are not controlled and
should be checked against the document (titled as above) on the server prior to use
D:\106748206.doc
Policy # MI/MD/v50
Microbiology Department
Policy & Procedure Manual
Section: Molecular Diagnostic Tests Manual
Page 87 of
291
b. Visually check that each microtube is tightly closed and that all microtubes have the same liquid
level 30ul, before loading. Make sure there are no bubbles at the bottom of the microtubes.
Detection (RotorGene) Area:
a. Turn ON the RotorGene and computer.
b. FOR THE BLUE ROTORGENE ONLY. Choose clinical icon; pass word “msh”; press “→”
button;
c. Double click (left on the mouse) “Rotor-Gene 6000 series software 1.7” icon. Wait for
“Initializing machine…..”
d. Load microtubes into proper rotor (eg. 36 well/or 72-well). Load sample #1 into rotor position
#1, sample #2 into rotor position #2, and so on.
e. Fill the empty positions of the rotor using empty microtubes and snap in the locking ring. Load
the rotor in the RotorGene 6000.
f. Highlight CMV assay;
g. Press “New” button;
h. Highlighting the correct rotor in use: Red 36-well Rotor
Blue 72-well Rotor
i. Click the box “Locking Ring Attached”
j. Press “Next” button.
k. Enter initials in Operator space. Enter kit lot number and the Rotor-Gene Colour (ie.Red/Blue) in
the Notes box. Verify the Reaction Volume is 30ul.
l. Press “Next”
m. Temperature Profile window pops up; press “Next”.
n. Summary window appears; press “Start Run”. The RotorGene will start.
o. Save as window appears; go to My documents -Open–select CMV result folder- Open Press
Save -CMV yyyy-mm-dd (run no.)
p. Edit Samples window. Go to format select 1.23E+05. Under Units select copies/ul.
q. Enter sample LIS numbers using the barcode reader, enter CMV Positive (CMV QS3), and
water.
PROCEDURE MANUAL
UNIVERSITY HEALTH NETWORK / MOUNT SINAI HOSPITAL MICROBIOLOGY DEPARTMENT
NOTE: This is a CONTROLLED document. Any documents appearing in paper form that are not stamped in red "MASTER COPY" are not controlled and
should be checked against the document (titled as above) on the server prior to use
D:\106748206.doc
Policy # MI/MD/v50
Microbiology Department
Policy & Procedure Manual
Section: Molecular Diagnostic Tests Manual
Name
Sample Number
QS3 CMV
Water
Type
Unknown
Standard
NTC(no template control)
Given conc.
1.00E+02
Page 88 of
291
Select
Yes
Yes
Yes
r. Press “Finish”. Click on “Name On”
To analyze and print CMV report after a run has finished:
1. The run is done when Profile Program reads: Run has completed.
2. Analyze raw data by clicking each channel one at a time: Green channel (CMV) and Yellow
channel (IC).These tabs are found on the second menu bar from the top, on the left hand side.
3. In the Green Channel. Click “All Off” (bottom right). Select sample “water (NTC)” and “cmv
QS3 (Standard)”. Click on Autoscale (bottom left).
Compare each specimen curve to the water curve and the cmv QS3 curve one at a time (by clicking
each sample on and off then proceeding to the next sample). A positive curve will have a sigmoidal
shape. A negative result will be a relatively flat line, like the water. Make a note of all positives on
the worklist.
4. Click on “Named On”.
5. Perform curve Analysis (Get report): Click “Analysis” on the top tool bar.
6. Analysis floating window pops up.
7. Click Quantitation Analysis.
8. Quantitation window is brought up to the front. There are should be two channels (Green/Yellow).
9. Highlight Cycling A. Green option and press Show.
10. Maximize the cycling green channel graph (or the channel you are working on).
11. Press “Import Curve” button on the right side of the screen.
12. Press “From other run” button.
13. Go to My Document -STD curves folder, press “Open”
PROCEDURE MANUAL
UNIVERSITY HEALTH NETWORK / MOUNT SINAI HOSPITAL MICROBIOLOGY DEPARTMENT
NOTE: This is a CONTROLLED document. Any documents appearing in paper form that are not stamped in red "MASTER COPY" are not controlled and
should be checked against the document (titled as above) on the server prior to use
D:\106748206.doc
Policy # MI/MD/v50
Microbiology Department
Policy & Procedure Manual
Section: Molecular Diagnostic Tests Manual
Page 89 of
291
14. Choose the latest CMV standard curve (Note: standard curves should changed every 6 months
unless instructed by Charge/Microbiologist), “Open”
15. Highlight green channel, press “Import” button.
16. Adjust if only ONE Standard used (Note: Do NOT adjust if ALL Std used)
17. Press button “Slope Correct” on the top.
18. Press button “Ignore first” on the top, and type “5”, press OK.
19. Check curve quality, adjust the Threshold.
20. To Print Reports: Press “Reports”.
21. Choose Cycling A.Green (Page 1)
22. Highlight Quantitation full report, press “Show” Maximize the report window, check that only
the positives that you have identified from the raw data are positive (i.e. have a crosspoint)
23. Print pages 1-4 for the green channel; pages 2-4 for the yellow channel.
Close the report window.
24. Yellow channel Analysis. Go to the floating Analysis window: Quantitation tab,
Select Cycling A. Yellow -the internal control (IC), select Show.
Maximize the graph Quantitation Analysis –Cycling A. Yellow.
Select Slope Correct. Select Ignore first and type “5” press OK (this will ignore the readings in
the first 5 cycles of the run).
Set the threshold (right-hand side middle) at 0.05. A threshold line will appear on your graph
screen. Move the threshold line to above the noise.
Press Reports. Select Cycling A.Yellow. Select Quantitation (Full report). Select Show.
All samples should have a positive IC curve, and a cycle number in the Ct column.
Print pages 2-4.
(For Cycling A. Yellow report, if there is message of “NEG (Multi Ct)” for any specimen, you have
to go back to check Raw Data of cycling A.Yellow. If all specimens are amplified, adjust the
threshold in Quantitation Analysis for Cycling A.Yellow, so that all samples have one Ct.
Adjust the threshold line so that the threshold line crosses the curve at only one point.)
25. Close the outer most window.
“Save changes to CMV yyyy-mm-dd?” Select Yes.
Shut down the computer, and switch off the Rotor-Gene.
PROCEDURE MANUAL
UNIVERSITY HEALTH NETWORK / MOUNT SINAI HOSPITAL MICROBIOLOGY DEPARTMENT
NOTE: This is a CONTROLLED document. Any documents appearing in paper form that are not stamped in red "MASTER COPY" are not controlled and
should be checked against the document (titled as above) on the server prior to use
D:\106748206.doc
Policy # MI/MD/v50
Microbiology Department
Policy & Procedure Manual
Section: Molecular Diagnostic Tests Manual
Page 90 of
291
V.
Calculations:
Perform calculations on CMV PCR blood (CMVB) specimens only. CMV PCR blood (CMVB)
specimens should be reported quantitatively; all CMV PCR non-blood (CMVNB) specimens are
reported qualitatively (CMV DNA detected/ No CMV DNA detected).
Result (copies of DNA/mL) = Result (copies/uL) x Elution volume (uL)
Sample volume (mL)
Result (copies of DNA/mL) = Result (copies/uL) x 50(uL)
0.200 (mL)
These calculations can also be performed using PCR bench Math excel file.
VI.
Reporting:
CMV PCR blood (CMVB) specimens should be reported quantitatively; all CMV PCR non-blood
(CMVNB) specimens are reported qualitatively (ie. CMV DNA detected/ No CMV DNA detected).
PCR Positives from sterile sites: CSF, eye specimens, biopsy, tissues; should be repeated a second
time. Re-extract the sample on the easyMAG and repeat the PCR. Release a preliminary report.
CMV PCR Blood (CMVB) Specimens:
CMV PCR negative (has no Ct value) report on the LIS test window, use keypad:
No CMV DNA detected.
This is a research test.
CMV PCR Kit 1.0, Altona Diagnostics Inc.
Under media “PCCMV” F6 to enter the date tested.
Finalize the result (Ctrl+F)
CMV PCR positive, with value in copies of DNA/mL (ie.After calculation has been performed). Report
CMV as an isolate in the isolate window (F7).
Isolate #: 1 Org.ID. 13cmv
Open the Isolate Comment window F8.
Go to the Virology keypad, type “V”.
From the keypad select: >CMV+ this will take you to CMV resulting keypads.
If result is <100 copies of DNA/mL select: <100\cmv1
If copies are to be reported select: \CMV+ Type in the copies, in scientific format, in the space
provided.
Grave (`) the result.
Under media “PCCMV” F6 to enter the date tested. If reporting <100 cp/mL enter the actual copy
value.
Interim the result (Ctrl + L).
PROCEDURE MANUAL
UNIVERSITY HEALTH NETWORK / MOUNT SINAI HOSPITAL MICROBIOLOGY DEPARTMENT
NOTE: This is a CONTROLLED document. Any documents appearing in paper form that are not stamped in red "MASTER COPY" are not controlled and
should be checked against the document (titled as above) on the server prior to use
D:\106748206.doc
Policy # MI/MD/v50
Microbiology Department
Policy & Procedure Manual
Section: Molecular Diagnostic Tests Manual
Page 91 of
291
CMV PCR Non-Blood (CMVNB) Specimens: Report qualitatively only.
CMV PCR negative, no Ct value. Report on the front of LIS workcard, use keypad:
No CMV DNA detected.
This is a research test.
CMV PCR Kit 1.0, Altona Diagnostics Inc.
Under media “PCCMV” F6 to enter the date tested.
Finalize the result (Ctrl+F)
CMV PCR positive (Ct value present), no calculations are performed. Report CMV as an isolate
window F7.
Isolate #: 1 Org.ID. 13cmv
Open the Isolate Comment window F8.
Go to the Virology keypad, type “V”.
Select: >CMV+
Select: \CMV+ Type: DETECTED and delete the “copies of DNA/mL” phrase.
Isolate Comment window F8 should appear as:
DETECTED.
This is a research test.
CMV PCR Kit 1.0, Altona Diagnostics Inc.
Grave (`) the result.
Under media “PCCMV” F6 to enter the date tested.
Interim the result (Ctrl+ L).
Calling Results:
BMT: Call all CMV PCR blood (CMVB) results to the Bone Marrow Transplant Clinic when tested;
CMV PCR positives and negative results.
PMH: Call Positive CMV PCR blood (CMVB) results
TGH: Call Positive CMV PCR blood (CMVB) results, if patients’ have not had CMV detected in their
blood in more than 2 months. If patients’ have had CMV detected in their blood within the last 2 months
no calling is necessary.
Outside clients: Call Positive CMV PCR blood (CMVB) and fax results.
Call all Positive CMV PCR Non-blood (CMVNB).
PROCEDURE MANUAL
UNIVERSITY HEALTH NETWORK / MOUNT SINAI HOSPITAL MICROBIOLOGY DEPARTMENT
NOTE: This is a CONTROLLED document. Any documents appearing in paper form that are not stamped in red "MASTER COPY" are not controlled and
should be checked against the document (titled as above) on the server prior to use
D:\106748206.doc
Policy # MI/MD/v50
Microbiology Department
Policy & Procedure Manual
Section: Molecular Diagnostic Tests Manual
VII.
Page 92 of
291
Testing Schedule: CMV PCR blood (CMVB)
PMH patients will be tested as requested.
TGH patients: CMV PCR blood (CMVB) Positive no CMV PCR Blood (CMVB) will be tested for 5
days. Result as: Previous CMV PCR Positive, please resubmit a specimen for testing after 5 days.
VIII. Quality Control
Reagent QCs:
An External Control (external to Altona Diagnostics) is used to monitor the isolation,
amplification and detection procedures. The result must correspond to expected value
supplied by the manufacturer.
CMV High Positive and CMV Low Positive External controls should be extracted on the
easyMag daily and run daily. Record external QC results in the T drive, Virology folder, QC
folder.
Daily QCs:
Every run:
Each patient specimen must have an Internal Control (IC) added to monitor both extraction
and PCR inhibition.
CMV QS3 Standard is included and shows a positive reading in Green Channel
A Negative Control is included and shows a negative reading in Green Channel
Report all failed QCs to senior/charge technologist.
a.
b.
c.
d.
e.
f.
g.
Failed QC:
Test is invalid without satisfactory QC results.
Do not release results pending resolution of QC failure.
Inform charge/senior technologist.
Record in Reagent Log Chart, Instrument Maintenance Log or Incident Report where
appropriate.
If the QC failure was due to a simple matter of position reversal or misplacement, the run can be
released (positive QC material yielded positive result, negative yielded negative result).
If positive QC material yielded negative result, repeat the entire run.
If negative QC material yielded positive result, it may be due to cross-contamination from
adjacent positive sample within the run or carry-over contamination from previous runs via
equipment or the environment. Review procedure and equipment to establish and eliminate
potential sources of contamination.
The extent and nature of contamination can also be evaluated by comparing the positive rate of
the run with its expected positive rate.
PROCEDURE MANUAL
UNIVERSITY HEALTH NETWORK / MOUNT SINAI HOSPITAL MICROBIOLOGY DEPARTMENT
NOTE: This is a CONTROLLED document. Any documents appearing in paper form that are not stamped in red "MASTER COPY" are not controlled and
should be checked against the document (titled as above) on the server prior to use
D:\106748206.doc
Policy # MI/MD/v50
Microbiology Department
Policy & Procedure Manual
Section: Molecular Diagnostic Tests Manual
Page 93 of
291
h. If the contamination is extensive, it is necessary to quarantine/discard potentially contaminated
reagents and consumables and disinfect equipment and environment before repeating the run.
i. If a carry-over contamination is suspected (e.g. two or more runs with negative QC being
positive or patient samples have higher than expected positive rate and these samples are often
non-repeatable positives), it is necessary to have a thorough environmental disinfection followed
by swabbing to monitor.
j. Successful ending to a carry-over contamination may be indicated by QC results and patient
positivity rate falling back to the expected normal range and three negative environmental swabs.
IX.
References
CMV PCR Kit 1.0, Altona Diagnostics
PROCEDURE MANUAL
UNIVERSITY HEALTH NETWORK / MOUNT SINAI HOSPITAL MICROBIOLOGY DEPARTMENT
NOTE: This is a CONTROLLED document. Any documents appearing in paper form that are not stamped in red "MASTER COPY" are not controlled and
should be checked against the document (titled as above) on the server prior to use
D:\106748206.doc
Policy # MI/MD/v50
Microbiology Department
Policy & Procedure Manual
Section: Molecular Diagnostic Tests Manual
Page 94 of
291
Epstein Barr Virus Quantitative PCR by Rotorgene
I.
Introduction
Epstein-Barr Virus is a double stranded DNA virus, in the family Herpesviridae. An
asymptomatic infection most commonly during childhood; EBV has been associated with some
cancers, including Burkett’s lymphoma and nasopharyngeal carcinoma. EBV PCR is most
commonly used for transplant recipients for monitoring post-transplant. EBV PCR is a real time
PCR, for the detection and quantitation of EBV from whole blood.
II.
Specimen Collection and Transport
EDTA whole blood stored at C if processed with 24 hours; processing >24 hours aliquot and
freeze whole blood at -20oC.
Sterile body fluids (CSF, plasma) for EBV PCR testing require Medical Microbiologist consent
before testing.
III.
Specimen Processing:
Whole blood processing refer to:
Nucleic Acid Extraction for Whole Blood – Biomerieux NucliSENS easyMAG
Sterile body processing refer to:
Nucleic Acid Extraction – Biomerieux NucliSENS easyMAG
GENERAL PRECAUTIONS:
There must be separate PCR work areas:Clean room and Specimen preparation area
Powder-free Gloves should only be in use in PCR areas.
Change gloves frequently and keep tubes closed whenever possible.
Prepare Working 1% sodium hypochloride daily
Specimen Preparation Supplies and equipment must be dedicated to Specimen Preparation
Area and not used for other activities and never used in Clean Room.
Change lab coats and gloves between work areas.
Use only Aerosol Resistant Tips (ART)
Use only sterile RNase-free, DNAse-free microtubes
Thaw components thoroughly at room temperature.
PCR work areas (Clean Room and Specimen Preparation Area) benchtops and equipment
after each shift.
PROCEDURE MANUAL
UNIVERSITY HEALTH NETWORK / MOUNT SINAI HOSPITAL MICROBIOLOGY DEPARTMENT
NOTE: This is a CONTROLLED document. Any documents appearing in paper form that are not stamped in red "MASTER COPY" are not controlled and
should be checked against the document (titled as above) on the server prior to use
D:\106748206.doc
Policy # MI/MD/v50
Microbiology Department
Policy & Procedure Manual
Section: Molecular Diagnostic Tests Manual
IV.
Page 95 of
291
Materials, Equipments
Clean Room: Biosafety Cabinet (MIBCT3), freezer (MIFTG)
Specimen Preparation area: Biosafety Cabinet (MIBCT7 or MIBCT8)
Rotor-Gene 6000
Rotor-Gene 6000 Multiplexing System with experiment template: EBV
72-Well Loading Block (pre-cooled to 4oC)
72-Well 6000 Series Rotor with Locking Ring
0.1 mL reaction microtubes Tubes and Caps
Variable volume Rainin pipettes: 1 to 20 uL, 10 to 200 uL, 100 to 1000 uL (assigned to
designated areas)
Reagent: Altona RealStar EBV-PCR Kit 1.0: MasterA, MasterB, Internal Control, EBV
Quantitative Standards 1, 2, 3, 4 (QS1, QS2, QS3, and QS4), PCR Grade Water
External Control: EBV High Positive, EBV Negative, EBV Low Positive, to be extracted and
run in this order on once a week, or if QC failure occurs.
V.
Procedure:
Prepare eluate samples in order according to the EBV worksheet. Add the following EBV
Quantitative Standards and NTC Water to the worksheet in the following order: EBV QS4,
EBV QS3, EBV QS2, EBV QS1, NTC (Non-Template Control) Water.
PCR Set-up:
In the Clean Room: Change into dedicated clean room gown and gloves, work in Biological
Safety Cabinet. Remove from -20oC freezer to thaw at room temperature the required number of
vials’ of EBV Master A, and EBV Master B (12 reactions/vial) for your EBV PCR run. Prepare
EBV Master Mix in 1.5mL conical (sarstedt) microtube; to load on the Eppendorf epMotion.
Prepare the Master Mix reactions required:
Number of Test Samples + 5 Standards (4QS&NTC) + one
Mix gently, do not vortex. Make only enough master mix for the tests you are running.
After Master A has been added together to Master B it cannot be frozen again.
Number of Reactions
EBV Master A
EBV Master B
Volume of Master Mix
Sample/Control Volume
1
5
15
20
10
PROCEDURE MANUAL
UNIVERSITY HEALTH NETWORK / MOUNT SINAI HOSPITAL MICROBIOLOGY DEPARTMENT
NOTE: This is a CONTROLLED document. Any documents appearing in paper form that are not stamped in red "MASTER COPY" are not controlled and
should be checked against the document (titled as above) on the server prior to use
D:\106748206.doc
Policy # MI/MD/v50
Microbiology Department
Policy & Procedure Manual
Section: Molecular Diagnostic Tests Manual
No. of samples
1
2
3
4
5
6
7
8
9
10
11
12
Page 96 of
291
EBV Master Mix
Master A (µl)
5
10
15
20
25
30
35
40
45
50
55
60
Master B (µl)
15
30
45
60
75
90
105
120
135
150
165
180
See Eppendorf epMotion Manual for further loading and programming instructions.
Manual Loading:
Load one reaction microtube (0.1mL) for each sample/control.
Pipette 20uL prepared EBV Master Mix into each reaction microtube.
Pipette 1.0uL of internal control into each reaction microtube designated for the 5 Standards
(EBV QS4, QS3, QS2, QS1, and NTC).
Specimen Processing Area:
Pipette 10uL of Sample/Standard into reaction microtube. Mix by pipetting 3x up and down into
the master mix. Cap each segment after pipetting is completed. Check reaction microtube
segments before loading into the rotor, ensure the liquid levels are at the same height, there are
no bubbles at the bottom of the microtubes, and the lid is tightly in place.
Load reaction microtubes in 72-Well blue rotor, fill empty rotor spaces with blank reaction
microtubes. Attach the Locking Ring. Load the rotor in the Rotor-gene 6000.
PROCEDURE MANUAL
UNIVERSITY HEALTH NETWORK / MOUNT SINAI HOSPITAL MICROBIOLOGY DEPARTMENT
NOTE: This is a CONTROLLED document. Any documents appearing in paper form that are not stamped in red "MASTER COPY" are not controlled and
should be checked against the document (titled as above) on the server prior to use
D:\106748206.doc
Policy # MI/MD/v50
Microbiology Department
Policy & Procedure Manual
Section: Molecular Diagnostic Tests Manual
Page 97 of
291
Detection (RotorGene) Area:
Switch ON computer, switch ON RotorGene.
FOR THE BLUE ROTOGENE ONLY. Select clinical icon; password “msh”. Enter.
Open “Rotor-Gene 6000 series software 1.7” icon
Wait for “Initializing machine…..”
New Run Window
Select EBV PCR
Select New
Select 72 Well Rotor (blue)
Check the box for “Locking Ring Attached”
Select “Next” button
PROCEDURE MANUAL
UNIVERSITY HEALTH NETWORK / MOUNT SINAI HOSPITAL MICROBIOLOGY DEPARTMENT
NOTE: This is a CONTROLLED document. Any documents appearing in paper form that are not stamped in red "MASTER COPY" are not controlled and
should be checked against the document (titled as above) on the server prior to use
D:\106748206.doc
Policy # MI/MD/v50
Microbiology Department
Policy & Procedure Manual
Section: Molecular Diagnostic Tests Manual
Page 98 of
291
Enter operator intials.
In Notes enter RotorGene colour (i.e. Red or Blue) Reagent Lot Number. Make sure the reaction
volume is 30uL.
Select Next.
Temperature Profile window .Select Next.
Rotor must be loaded.
New Run Wizard window: Select Start Run. The RotorGene will start.
Save As window appears; the run filename is given with the default template. Save in: My
Documents in EBV Virus folder for the current year: e.g. EBV Virus 20150326(1) (assay name
yyyymmdd run#)
PROCEDURE MANUAL
UNIVERSITY HEALTH NETWORK / MOUNT SINAI HOSPITAL MICROBIOLOGY DEPARTMENT
NOTE: This is a CONTROLLED document. Any documents appearing in paper form that are not stamped in red "MASTER COPY" are not controlled and
should be checked against the document (titled as above) on the server prior to use
D:\106748206.doc
Page 99 of
291
Policy # MI/MD/v50
Microbiology Department
Policy & Procedure Manual
Section: Molecular Diagnostic Tests Manual
Select Save.
RotorGene will start running.
Edit Samples window appears.
Enter sample numbers including Quantitative Standards (EBV QS4, QS3, QS2, QS1, NTC) and
concentrations. Define the sample types according to the chart below.
Name
Sample Type
Samples
EBV QS4
EBV QS3
EBV QS2
EBV QS1
NC Water
Unknown
Given
concentration
IU/uL
*Conversion
factor
x250
Enter Concentration
IU/mL
1.00E+01
1.00E+02
1.00E+03
1.00E+04
x250
x250
x250
x250
2.50E+03
2.50E+04
2.50E+05
2.50E+06
Standard
Standard
Standard
Standard
NTC
(No template
control)
*conversion factor is based on the extraction sample volume and eluate volume
*Result (copies of DNA/mL) = Result (copies/uL) x Elution volume (uL)
Sample volume (mL)
*Result (copies of DNA/mL) = Result (copies/uL) x 50(uL)
0.200 (mL)
Under Given Conc. Format: Select 1.23E+05 (2 decimal points expressed as an exponent).
Units: Select copies/mL
Press “Finish”. Click on “Name On”.
Analysis
Profile Program reads: Run has completed.
Analyze raw data by clicking each channel one at a time: Green channel (EBV) and Yellow
channel (IC).
Target
Channel
Report Dye
EBV
Internal Control
Green
Yellow
FAM
JOE
PROCEDURE MANUAL
UNIVERSITY HEALTH NETWORK / MOUNT SINAI HOSPITAL MICROBIOLOGY DEPARTMENT
NOTE: This is a CONTROLLED document. Any documents appearing in paper form that are not stamped in red "MASTER COPY" are not controlled and
should be checked against the document (titled as above) on the server prior to use
D:\106748206.doc
Policy # MI/MD/v50
Microbiology Department
Policy & Procedure Manual
Section: Molecular Diagnostic Tests Manual
Page 100 of
291
Perform Raw Green (EBV Target) Channel. Select All Off.
Select sample water (NTC) and EBV QS4, QS3, QS2, QS1. Select Autoscale.
Compare each sample curve to the NTC-water curve and the EBV QSs’ one at a time, then
proceeding to the next sample. A positive curve will have a sigmoidal shape. A negative result
will be a relatively flat line, like the water. Make a note of all positives on the worksheet.
Select Named On.
Select Analysis Icon
In Analysis window. Select Quantitation Tab. (This should be the default).
Two channel option: Cycling A Green and Cycling A Yellow
Select Cycling A. Green. Select Show.
Calculate Automatic Threshold. Select OK.
Maximize the window: Quantitation Analysis Cycling A Green or Quantitation Analysis
Cycling A Yellow depending on what channel you are analyzing.
Select Slope Correct.
Select Ignore first: 5 Cycles. OK
Select Threshold Icon and adjust the threshold. The threshold can only cross a curve at one
point.
Verify the Quantitative Standard Curve on the Green (FAM) Channel. The following parameters
must be met, this information can be found on page one of the Green Channel Quantitation –Full
Report or on the screen in the Green Channel Graph.
Control Parameter
M Slope
PCR Efficiency
R square (R2)
Valid Values
-3.00 to -3.74
85% to 115%
>0.98
PROCEDURE MANUAL
UNIVERSITY HEALTH NETWORK / MOUNT SINAI HOSPITAL MICROBIOLOGY DEPARTMENT
NOTE: This is a CONTROLLED document. Any documents appearing in paper form that are not stamped in red "MASTER COPY" are not controlled and
should be checked against the document (titled as above) on the server prior to use
D:\106748206.doc
Policy # MI/MD/v50
Microbiology Department
Policy & Procedure Manual
Section: Molecular Diagnostic Tests Manual
Page 101 of
291
If the quantitative parameters are not valid, it must be brought to the attention of the senior/and or
charge. External Controls must be valid, if not valid, it must be brought to the attention of the
senior/and or charge. Patients results must not be released.
Select Reports. Select Cycling A Green (Target) or Quantitation Analysis Cycling A Yellow
(Internal Control) depending on what channel you are analyzing.
Select Quantitation (Full Report)
Maximize report window. Check that only the positives that you have identified, from the raw
data analysis, are positive (i.e. have a crossing threshold ct value).
Print all pages for Green (Target-FAM) channel. Print pages 2-5(or 4) for the Yellow (Internal
Control-JOE) channel.
PROCEDURE MANUAL
UNIVERSITY HEALTH NETWORK / MOUNT SINAI HOSPITAL MICROBIOLOGY DEPARTMENT
NOTE: This is a CONTROLLED document. Any documents appearing in paper form that are not stamped in red "MASTER COPY" are not controlled and
should be checked against the document (titled as above) on the server prior to use
D:\106748206.doc
Policy # MI/MD/v50
Microbiology Department
Policy & Procedure Manual
Section: Molecular Diagnostic Tests Manual
Page 102 of
291
Close Report window.
Perform Raw Yellow (Internal Control) Channel. Select Name On.
All samples, including EBV QS1-4, and NTC water, should have a good amplification curve; all
should be positive in the Yellow IC Channel; with the exception of samples with high ct values
(ct <20.00) in the EBV Target Green Channel.
Select Analysis Icon
In Analysis window. Select Quantitation Tab. (This should be the default).
Two channel option: Cycling A Green and Cycling A Yellow
Select Cycling A. Yellow. Select Show.
Calculate Automatic Threshold. Select OK.
Maximize the window: Quantitation Analysis Cycling A Green or Quantitation Analysis
Cycling A Yellow depending on what channel you are analyzing.
Select Slope Correct.
Select Ignore first: 5 Cycles. OK
Select Threshold Icon and adjust the threshold. The threshold can only cross a curve at one
point.
Select Reports. Select Cycling A Green or Quantitation Analysis Cycling A Yellow
depending on what channel you are analyzing.
Select Quantitation (Full Report)
Print all pages for first channel. Print pages 2-5(or 4) for the Yellow IC channel.
Close Report window.
Note: Cycling A. Yellow report: if there is message of “NEG (Multi Ct)” for any specimen, you
must adjust the threshold. This indicates the threshold has crossed the curve at multiple points.
The threshold can only cross a curve at one point.
Save changes to EBV yyyy-mm-dd. Select Yes.
Shut down the computer, and switch off the Rotor-Gene.
PROCEDURE MANUAL
UNIVERSITY HEALTH NETWORK / MOUNT SINAI HOSPITAL MICROBIOLOGY DEPARTMENT
NOTE: This is a CONTROLLED document. Any documents appearing in paper form that are not stamped in red "MASTER COPY" are not controlled and
should be checked against the document (titled as above) on the server prior to use
D:\106748206.doc
Policy # MI/MD/v50
Microbiology Department
Policy & Procedure Manual
Section: Molecular Diagnostic Tests Manual
VI.
Page 103 of
291
Reporting
EBV Not detected: Specimen has no ct value. Report in LIS using the keypads:
Virology Worklist > EBV PCR worklist > Select from the reporting keypads: }EBVNegative for EBV virus DNA.
This is a research test.
EBV PCR Kit v1.0. Astra Diagnostics Inc.
Under media PCEBV. F6 to enter the date tested.
Finalize the result (Ctrl+F)
EBV Detected: Specimen with ct value. Report quantitation “IU/mL”
Report EBV as an isolate in the isolate window (F7).
Isolate #: 1
Org.ID. 65ebv
Open the Isolate Comment window F8.
Go to the Virology keypad, type “V”.
Greater than 600 IU/mL. Select the keypad: \EBV+
Turn off the reporting keypad. Ctrl + A or Ctrl + K
Enter the IU/mL, in scientific number format, in the space provided, remove extra spacing.
Example:
3.20E+04 IU/mL.
This is a research test.
EBV PCR Kit v1.0, Astra Diagnostics Inc.
Verify all in the Isolate window
Less than 600 (<600) of IU/mL. Select: \E600
Under media “PCEBV” F6 to enter the date tested.
If reporting Less than 600 IU/mL, enter the actual IU/mL.
Interim (Ctrl + L) the report.
Second technologist will check transcription in LIS and Finalize (Ctrl + F) the report.
PROCEDURE MANUAL
UNIVERSITY HEALTH NETWORK / MOUNT SINAI HOSPITAL MICROBIOLOGY DEPARTMENT
NOTE: This is a CONTROLLED document. Any documents appearing in paper form that are not stamped in red "MASTER COPY" are not controlled and
should be checked against the document (titled as above) on the server prior to use
D:\106748206.doc
Policy # MI/MD/v50
Microbiology Department
Policy & Procedure Manual
Section: Molecular Diagnostic Tests Manual
VII.
Page 104 of
291
Quality Control
Reagent QCs:
An External Control (external to altona Diagnostics) is used to monitor the isolation, amplification and
detection procedures. The result must correspond to expected value supplied by the manufacturer.
EBV High Positive and EBV Low Positive External controls should be extracted on the easyMag once
a week. Record external QC results in the T drive, Virology folder, QC folder.
Daily QCs: Every run:
Each patient specimen must have an Internal Control (IC) added to monitor both extraction and PCR
inhibition.
EBV QS1, QS2, QS3, QS4 Standard is included and shows a positive reading in Green Channel.
Quantitative Standards must meet valid quantitative parameters.
A Negative NTC (No template control) Control is included and shows a negative reading in Green
Channel
Report all failed QCs to senior/charge technologist.
Failed QC:
Test is invalid without satisfactory QC results.
Do not release results pending resolution of QC failure.
Inform charge/senior technologist.
Record in: Reagent Log Chart, Instrument Maintenance Log or Incident Report where appropriate.
If the QC failure was due to a simple matter of position reversal or misplacement, the run can be
released (positive QC material yielded positive result, negative yielded negative result).
If positive QC material yielded negative result, repeat the entire run.
If negative QC material yielded positive result, it may be due to cross-contamination from adjacent
positive sample within the run or carry-over contamination from previous runs via equipment or the
environment. Review procedure and equipment to establish and eliminate potential sources of
contamination.
The extent and nature of contamination can also be evaluated by comparing the positive rate of the run
with its expected positive rate.
If the contamination is extensive, it is necessary to quarantine/discard potentially contaminated reagents
and consumables and disinfect equipment and environment before repeating the run.
If a carry-over contamination is suspected (e.g. two or more runs with negative QC being positive or
patient samples have higher than expected positive rate and these samples are often non-repeatable
positives), it is necessary to have a thorough environmental disinfection followed by swabbing to
monitor.
Successful ending to a carry-over contamination may be indicated by QC results and patient positivity
rate falling back to the expected normal range and three negative environmental swabs
PROCEDURE MANUAL
UNIVERSITY HEALTH NETWORK / MOUNT SINAI HOSPITAL MICROBIOLOGY DEPARTMENT
NOTE: This is a CONTROLLED document. Any documents appearing in paper form that are not stamped in red "MASTER COPY" are not controlled and
should be checked against the document (titled as above) on the server prior to use
D:\106748206.doc
Page 105 of
291
Policy # MI/MD/v50
Microbiology Department
Policy & Procedure Manual
Section: Molecular Diagnostic Tests Manual
Summary Information: EBV PCR
Number of Reactions
EBV Master A
EBV Master B
Volume of Master Mix
Sample/Control Volume
Name
Sample Type
1
5
15
20
10
Given
concentration
IU/uL
*Conversion
factor
x250
Enter Concentration
IU/mL
Samples
Unknown
EBV QS4
Standard
1.00E+01
x250
2.50E+03
EBV QS3
Standard
1.00E+02
x250
2.50E+04
EBV QS2
Standard
1.00E+03
x250
2.50E+05
EBV QS1
Standard
1.00E+04
x250
2.50E+06
NC Water
NTC
(No template
control)
Control Parameter
M Slope
PCR Efficiency
R square (R2)
Valid Values
-3.00 to -3.74
85% to 115%
>0.98
VIII. References
Altona EBV PCR Kit v1.0 Instructions, Altona Diagnostics
PROCEDURE MANUAL
UNIVERSITY HEALTH NETWORK / MOUNT SINAI HOSPITAL MICROBIOLOGY DEPARTMENT
NOTE: This is a CONTROLLED document. Any documents appearing in paper form that are not stamped in red "MASTER COPY" are not controlled and
should be checked against the document (titled as above) on the server prior to use
D:\106748206.doc
Policy # MI/MD/v50
Microbiology Department
Policy & Procedure Manual
Section: Molecular Diagnostic Tests Manual
Page 106 of
291
Enterovirus RNA PCR by Lightcycler
I.
Introduction
Enterovirus belongs to the family Picornaviridae including over 70 distinct serotypes(coxsackie
A and B, echoviruses, polioviruses, and enteroviruses 68-73). They infect a wide variety of
mammals and are associated with a board spectrum of diseases. There are 68 viruses within the
Enterovirus genus that are known to infect humans. Enteroviruses are transmitted primarily by
the fecal-oral route but respiratory spread is possible. Non-polio enteroviruses most commonly
cause rashes, upper respiratory infections. Enteroviruses infections account for a substantial
number of ascetic meningitis and encephalitis cases in summer and fall.
II.
Collection and Transport
Blood samples for enterovirus PCR should be collected in EDTA (purple top vacutainer tube).
CSF specimens should be collected in a clean, sterile container and sent to the laboratory as soon
as possible. If specimens cannot be transported immediately, they should be kept at 4oC. If a
delay of more than 6 hours is anticipated, the CSF specimen should be frozen at –70oC. The
EDTA samples should be processed within 6 hours of collection (plasma separated and
refrigerated; frozen if delay is more than 6 hours). Allow only one freeze-thaw cycle.
NOTE: Repeated freezing-thawing will reduce test sensitivity and cryoprecipitates may
accumulate in the plasma.
III.
Procedure
A. Worklist Preparation:
a. log on to Softmic,
b. Go to PCR Worklist
i. Worklist : 1VPCR VIROL PCR
ii. Enter
iii. F12
c. Pending samples (plasma, serum or CSF) will appear on Worklist.
d. Mark received samples using the F5 key, that require Enterovirus PCR
e. Type "`" to print Worklist.
B. LIS Label Printing (if needed for the RNA eluate):
a. While still in the Worklist, press Enter to go to the Test Screen
b. Press F1 to move curser to Demographic field
c. Press: / (to Order/Entry)
d. Press: No (to confirm editing)
e. Press: F9
f. Press: \ (Print Labels)
g. Press: No (modify record)
h. Select label printer for the LIS label
PROCEDURE MANUAL
UNIVERSITY HEALTH NETWORK / MOUNT SINAI HOSPITAL MICROBIOLOGY DEPARTMENT
NOTE: This is a CONTROLLED document. Any documents appearing in paper form that are not stamped in red "MASTER COPY" are not controlled and
should be checked against the document (titled as above) on the server prior to use
D:\106748206.doc
Policy # MI/MD/v50
Microbiology Department
Policy & Procedure Manual
Section: Molecular Diagnostic Tests Manual
Page 107 of
291
C. Specimens Processing:
Specimens should be processed as soon as possible after arriving in virology laboratory.
CSF:
An aliquot (0.2-2 mL) of the CSF should be frozen unless PCR can be performed
immediately
After processing, an aliquot of the left-over specimens should be stored frozen at-70C.
E. Materials, Equipments and Facilities:
Clean Room with dedicated Biosafety Cabinet (MIBCT4), freezer (MIFTG), gowns and
gloves
Specimen Preparation area with Biosafety Cabinet and microcentrifuge
Detection Room for LightCycler
Roche LightCycler programmed for Artus Enterovirus RT-PCR
Microcentrifuge (MICT14)
Vortex
1.5 mL microcentrifuge tubes
Cooling Block with capillary adaptors pre-cooled to 4oC
Variable volume pipettes:
1 to 20 uL
10 to 200 uL
100 to 1000 uL
ART-Aersol Resistant Tips for pipettes
From Qiagen QIAampR Viral RNA Mini Kit:
Collection Tubes
Lysis Buffer AVL
Carrier RNA (poly A)-add 310 uL Elution Buffer -AVE to lyophilized carrier RNA
(310 ug) dissolve thoroughly and aliquot into 5.6 uL and 30 uL screw-cap microtubes,
and store at -20C in the clean room. DO NOT freeze-thaw the carrier RNA aliquots
more than 3 times
Spin Columns
Wash Buffer 1 (Buffer AW1) – add 125 mL ethanol before use
Wash Buffer 2 (Buffer AW2) – add 160 mL ethanol before use
Elution Buffer (Buffer AVE)
PROCEDURE MANUAL
UNIVERSITY HEALTH NETWORK / MOUNT SINAI HOSPITAL MICROBIOLOGY DEPARTMENT
NOTE: This is a CONTROLLED document. Any documents appearing in paper form that are not stamped in red "MASTER COPY" are not controlled and
should be checked against the document (titled as above) on the server prior to use
D:\106748206.doc
Policy # MI/MD/v50
Microbiology Department
Policy & Procedure Manual
Section: Molecular Diagnostic Tests Manual
Page 108 of
291
From: artusTM Enterovirus LC RT-PCR Kit (stored at -20o C in clean room):
Quantification Standards (QS). When a new kit is opened, the QS must be
moved to a freezer in the specimen preparation area.
Internal Control (IC)
Master Mix (12 tests)
Water (PCR grade)
Ethanol, anhydrous, reagent grade, 96 - 100%
External Control: To be run when a new lot (Qiagen or RealArt) is used, during training
or if QC failure occurs.
GENERAL PRECAUTIONS:
There must be separate PCR work areas:
1. Clean room
2. Specimen preparation room
3. Amplification room
Supplies and equipment must be dedicated to each PCR area and not used for other
activities or moved between areas.
Change gloves between work areas. Only blue gowns are to be worn in the clean
room.
Use only filtered pipette tips
Use only sterile RNase, Dnase-free microcentrifuge tubes
Use sterile, disposable polypropylene tubes throughout the procedure
Always wear powder-free gloves when handling reagents
Change gloves frequently and keep tubes closed whenever possible
Prepare and store reagents (lysis buffer, RNA carrier, elution buffer, AW1, AW2 and
ethanol) in the clean room. Keep only working aliquots in the specimen preparation
area.
Keep the Quantitation Standards and specimens in the specimen preparation area.
Thaw components thoroughly at room temperature
Mix components and centrifuge briefly
Work quickly in the cooling block
Use 1% sodium hypochloride or Eliminase to disinfect equipment and surfaces and
then rinse with 70% alcohol or water.
PROCEDURE MANUAL
UNIVERSITY HEALTH NETWORK / MOUNT SINAI HOSPITAL MICROBIOLOGY DEPARTMENT
NOTE: This is a CONTROLLED document. Any documents appearing in paper form that are not stamped in red "MASTER COPY" are not controlled and
should be checked against the document (titled as above) on the server prior to use
D:\106748206.doc
Policy # MI/MD/v50
Microbiology Department
Policy & Procedure Manual
Section: Molecular Diagnostic Tests Manual
Page 109 of
291
Clean Room
In the Clean Room prepare the Working Lysis Buffer AVL; determine the number of tests to be
extracted and prepare the appropriate volume of Working Lysis Buffer AVL required according to
the chart. Mix gently, invert 10 times to mix. Do not vortex.
Volume
Lysis
Buffer No. of
AVL
samples (mL)
1
0.56
2
1.12
3
1.68
4
2.24
5
2.80
6
3.36
7
3.92
8
4.48
9
5.04
10
5.60
11
6.16
12
6.72
Volume
Carrier
RNA-in
Elution
buffer AVE (uL)
5.6
11.2
16.8
22.4
28.0
33.6
39.2
44.8
50.4
56.0
61.6
67.2
DO NOT freeze-thaw the carrier RNA aliquots more than 3 times.
Working Lysis Buffer AVL is stable for 48 hrs at 2-8C. Solution may precipitate at 2-8C; redisolve
by warming on the bench, DO NOT MICROWAVE.
Lysis and Purification:
a. Use Specimen Preparation area; work in cabinet with gown. Use only ART tips. Change
gloves frequently.
b. For each Specimen and External Control, prepare and label two 1.5 mL microcentrifuge
tubes (sterilized, RNase-free) with the corresponding number in the Worklist. Put the
specimens first on the worklist, followed by the external control (if using one). Label one of
them with the lab number (LIS label). This microcentrifuge tube will store the eluted RNA;
the other will be used for processing and will be discarded. Also, label one QIAamp Spin
Column (Qiagen) with the number on the Worklist. Arrange the 2 microcentrifuge tubes and
Columns into 3 rows.
PROCEDURE MANUAL
UNIVERSITY HEALTH NETWORK / MOUNT SINAI HOSPITAL MICROBIOLOGY DEPARTMENT
NOTE: This is a CONTROLLED document. Any documents appearing in paper form that are not stamped in red "MASTER COPY" are not controlled and
should be checked against the document (titled as above) on the server prior to use
D:\106748206.doc
Policy # MI/MD/v50
Microbiology Department
Policy & Procedure Manual
Section: Molecular Diagnostic Tests Manual
Page 110 of
291
c. Add 560 uL Working Lysis Buffer (AVL with RNA carrier) into each of the microcentrifuge
tubes in one row (these will contain the waste).
d. Add 140 uL Specimen to the Working Lysis Buffer (Buffer AVL with RNA carrier), vortex
for 15 seconds.
e. Incubate at Room Temperature (15-25oC) for 10 minutes.
f. Centrifuge for 10 seconds at 3000 rpm (2000 g) to remove drops from the lids.
g. Add 5 uL Enterovirus Internal Control to each of the microcentrifuge tubes with Buffer
AVL.
h. Add 560 uL ethanol (96-100%) to the samples, vortex for 15 seconds. Centrifuge for 10
seconds at 3000rpm (2000 g) to remove drops from the lids.
i. Pipette 630 uL (half the volume) of the mixture (specimen-lysis buffer-ethanol) to the
QIAamp spin column (in a 2 mL collection tube), close the cap and centrifuge at 8000 rpm
(6000 g) for 1 minute. Place the QIAamp spin column into a clean 2 mL collection tube and
discard the collection tube containing the filtrate.
j. Repeat Step (h) by pipeting the remaining 630 uL of the mixture to the QIAamp spin column
(in a 2 mL collection tube), close the cap and centrifuge at 8000rpm (6000 g) for 1 minute.
Place the QIAamp spin column into a clean 2 mL collection tube and discard the collection
tube containing the filtrate.
k. Open the spin column and add 500 uL of Buffer AW1. Close the cap and centrifuge at 8,000
rpm (6,000 g) for 1 minute.
l. Place the QIAamp spin column into a clean 2 mL collection tube and discard the collection
tube containing the filtrate.
m. Open the spin column and add 500 uL of Buffer AW2. Close the cap and centrifuge at full
speed 14,000 rpm (20,000g) for 3 minutes.
b. Place the spin column into a clean 2 mL collection tube and discard the collection tube
containing the filtrate. Centrifuge at 14,000 rpm (20,000g) for 3 minutes.
Elution Steps:
a. Place the spin column in the second clean 1.5 mL microcentrifuge tube with the LIS
specimen label. Discard the collection tube containing the filtrate. Open the spin column
and add 50 uL of Elution Buffer (Buffer AVE). Close the caps and incubate at room
temperature for 1 minute.
PROCEDURE MANUAL
UNIVERSITY HEALTH NETWORK / MOUNT SINAI HOSPITAL MICROBIOLOGY DEPARTMENT
NOTE: This is a CONTROLLED document. Any documents appearing in paper form that are not stamped in red "MASTER COPY" are not controlled and
should be checked against the document (titled as above) on the server prior to use
D:\106748206.doc
Policy # MI/MD/v50
Microbiology Department
Policy & Procedure Manual
Section: Molecular Diagnostic Tests Manual
Page 111 of
291
b. Centrifuge at 8000rpm (6000 g) for 1 min. Discard the spin column. Store the eluate at -20oC
or –70oC if not able to proceed immediately.
PCR Amplification and Detection Procedures:
In the Clean Room:
Change into dedicated clean room gown and gloves, work in Biosafety Cabinet. Use only ART tips.
a.
Take out the necessary number of Enterovirus Master Mix vials (12 tests per vial) from the
freezer and thoroughly thaw inside the Biosafety Cabinet.
b.
Place a capillary for each purified sample, QS, external QC and Negative control (H2O) into the
capillary adaptor of the Cooling Block (pre-cooled to 4oC).
a.
Pipette 15 uL Master Mix into the reservoir of each capillary.
b.
Pipette 0.5 uL of internal control into the capillaries designated for the QS and the Negative
control.
c.
Pipette 5 uL PCR grade water into the negative control capillary and cap.
d.
Changed out of dedicated clean room gown
In the Specimen Processing Room: Changed into specimen room gown.
a.
Using ART tips, carefully pipette 5 uL each of purified sample, and QS4, (and external QC, if
using) directly into the capillary tube. Immediately close the capillary with a lid.
b.
Load capillary tubes into LightCycler (LC) sample carousel and centrifuge at 3000 rpm for 15
seconds in LC centrifuge. Load the LC sample carousel into the LC instrument.
The LightCycler (LC) Instrument:
a.
Turn LightCycler on first and then the computer.
b.
Enter your user name and password and click OK.
c.
Click on the LightCycler icon and push ENTER.
d.
Wait for the “Self-test box” to appear.
e.
Perform "selftest". “Skip selftest” if performed within 24 hr.
f.
Choose OK when the self-test passes.
PROCEDURE MANUAL
UNIVERSITY HEALTH NETWORK / MOUNT SINAI HOSPITAL MICROBIOLOGY DEPARTMENT
NOTE: This is a CONTROLLED document. Any documents appearing in paper form that are not stamped in red "MASTER COPY" are not controlled and
should be checked against the document (titled as above) on the server prior to use
D:\106748206.doc
Policy # MI/MD/v50
Microbiology Department
Policy & Procedure Manual
Section: Molecular Diagnostic Tests Manual
Page 112 of
291
g.
Record that you did the self-test in the log book.
h.
Select: "Open Experimental File"
“Enterovirus protocol"; choose “Open”
“Run”
i.
Type in file name “enterovir-year-month-day- run number” e.g. enterovir -2004-02-01. Choose
“save”.
j.
Type in the number of samples to run including QS, Negative Control, and External Control (if
using one) in the “maximum position” field.
k.
Select “Enter Samples Later”. LightCycler will begin protocol.
l.
Select “Edit Samples” (bottom right of screen).
m.
Select “Clear Sample List”. OK
n.
Type in the lab numbers; QS; ext. QC (if any) and Negative control.
o.
On the QS row, click the arrow-down button to change its description from “Unknown” to
“STD” and enter the number of copies/uL (eg. QS3=100)
p.
Press “Done”
Remember to freeze the end product and patient samples.
To Print Results, go to:
“FLUORESCENCE” and click
F1
Quantification
Print Window
To Print Internal Control, go to:
“FLUORESCENCE” and click:
F3/BACK- F1
Print Window
PROCEDURE MANUAL
UNIVERSITY HEALTH NETWORK / MOUNT SINAI HOSPITAL MICROBIOLOGY DEPARTMENT
NOTE: This is a CONTROLLED document. Any documents appearing in paper form that are not stamped in red "MASTER COPY" are not controlled and
should be checked against the document (titled as above) on the server prior to use
D:\106748206.doc
Policy # MI/MD/v50
Microbiology Department
Policy & Procedure Manual
Section: Molecular Diagnostic Tests Manual
Page 113 of
291
At the end of the day, follow the cleaning protocol below using 1% hypochorite or Eliminase followed
by 70% alcohol:
Clean Room:
Clean Biological Safety Cabinet and turn on UV light for a least ½ hour but not overnight.
Clean Pipettors
Specimen Preparation Room:
Seal and discard waste bag
Clean Biological Safety Cabinet thoroughly
Wipe all pipettors, centrifuge, and bench top.
Wash racks.
Amplification Room:
Discard capillaries into a sharps container and put the cap the back onto the sharps container
If a capillary breaks in the carousel, use the small brush supplied to clean the holes with 1%
hypochorite and then alcohol.
IV.
Reporting:
Fluorimeter
Channel F1
(Target)
Fluorimeter
Channel F3 back- F1
(IC amplicon)
Interpretations
-
-
Possible PCR inhibition-Repeat assay.
If still -ve on both Fluorimeter Channels,
report: Indeterminate
-
+
+
-
+
+
Sample has no detectable Enterovirus RNA
Report: Negative
Review the F1 graph.
Sample contains Enterovirus RNA.
May need to be repeated. Inform
charge/senior.
Report: POSITIVE
Review the F1 graph.
Sample contains Enterovirus RNA.
May need to be repeated. Inform
charge/senior.
Report: POSITIVE
PROCEDURE MANUAL
UNIVERSITY HEALTH NETWORK / MOUNT SINAI HOSPITAL MICROBIOLOGY DEPARTMENT
NOTE: This is a CONTROLLED document. Any documents appearing in paper form that are not stamped in red "MASTER COPY" are not controlled and
should be checked against the document (titled as above) on the server prior to use
D:\106748206.doc
Policy # MI/MD/v50
Microbiology Department
Policy & Procedure Manual
Section: Molecular Diagnostic Tests Manual
Page 114 of
291
Positive results for the Enterovirus amplicon (Channel F1) will have the cycle number printed under
the Cross Point Column in the chart and the Specimen Cross point (Ct) will be less than the
Enterovirus QS4 (60 copies/uL).Review the curve, it will be rising exponentially and levels off to a
plateau. Internal Control amplicon need not be positive. Inform Charge of positive specimen, sample
may need to be repeated.
Indeterminate results may be those with a positive signal for the Enterovirus (F1 channel) cycle
number printed under the Cross Point Column, the Specimen Cross point (Ct) is less than the
Enterovirus QS4 (60 copies/uL). Review the curve. Inform Charge of Indeterminate specimen, sample
may need to be repeated.
Indeterminate results may also be those with no signal for the Enterovirus (F1) and also no signal for
the IC amplicon (Channel F3/Back-F1), indicating possible PCR inhibition. Report Indeterminate
specimens to Charge, repeat testing may be required.
Negative results for the Enterovirus amplicon (Channel F1) will be blank under the Cross Point
Column in the chart and the curve will be rather flat. The IC amplicon (Channel F3 back F1) must be
positive to be valid.
Negative Report:
Negative by RT-PCR.
This is a research test performed by using artus Enterovirus LC RT-PCR
assay, Artus Biotech Inc.
Indeterminate Report: Indeterminate by RT-PCR
This is a research test performed by using artus Enterovirus LC RT-PCR
assay, Artus Biotech Inc.
Positive Report:
POSITIVE by RT-PCR
This is a research test performed by using artus Enterovirus LC RT-PCR
assay, Artus Biotech Inc.
Inform Charge technologist of Positive and Indeterminate results. Record isolate in LIS in F7
Isolate window as 39ent Enterovirus, and call Positive results.
PROCEDURE MANUAL
UNIVERSITY HEALTH NETWORK / MOUNT SINAI HOSPITAL MICROBIOLOGY DEPARTMENT
NOTE: This is a CONTROLLED document. Any documents appearing in paper form that are not stamped in red "MASTER COPY" are not controlled and
should be checked against the document (titled as above) on the server prior to use
D:\106748206.doc
Policy # MI/MD/v50
Microbiology Department
Policy & Procedure Manual
Section: Molecular Diagnostic Tests Manual
V.
Page 115 of
291
Quality Control
Colour Compensation (to compensate interference between different fluorochromes) should be
run to update the Colour Compensation File.
Reagent QCs:
Before every lot change of isolation and/or master mix kit:
An External Control (external to Artus Biotech) is used to monitor the isolation, amplification
and detection procedures. The result must correspond to expected value supplied by the
manufacturer.
Before every lot change of master mix kit:
All four Quantification Standards (QS 1, 2, 3, and 4) must be run.
Daily QCs:
Every run:
Each patient specimen must have an Internal Control (IC) added to monitor extraction
and PCR inhibition. The sample must show a positive reading in either fluorimeter
Channel F1 or fluorimeter Channel F3 back-F1 (IC amplicon) to be valid (no PCR
inhibition).
A Positive Control (e.g.QS4) is included and shows a positive reading in fluorimeter
Channel F1
A Negative Control (e.g. H2O spiked with IC) is include and shows a negative reading in
fluorimeter Channel F1 and a positive reading in fluorimeter Channel F3 back F1 (IC
amplicon).
Report all failed QCs to senior/charge technologist
VI.
References:
QIAamp Viral RNA Mini Kit Handbook Dec. 2005, Qiagen
ArtusTM Enterovirus LC RT-PCR Kit User Manual March 2006, Artus
LightCycler, Roche Diagnostics
PROCEDURE MANUAL
UNIVERSITY HEALTH NETWORK / MOUNT SINAI HOSPITAL MICROBIOLOGY DEPARTMENT
NOTE: This is a CONTROLLED document. Any documents appearing in paper form that are not stamped in red "MASTER COPY" are not controlled and
should be checked against the document (titled as above) on the server prior to use
D:\106748206.doc
Policy # MI/MD/v50
Microbiology Department
Policy & Procedure Manual
Section: Molecular Diagnostic Tests Manual
Page 116 of
291
Hepatitis B/Hepatitis C/HIV Donor Screen NAT PCR by Cobas® s201 Ampliprep/TaqMan
I.
Introduction
A major concern surrounding tissue and blood donations from live or cadaveric donors involves
the potential of viral infection transmission including that of Human Immunodeficiency Virus
(HIV-1) and Type 2 (HIV-2), Hepatitis C Virus (HCV) and Hepatitis B Virus (HBV). These
agents are primarily transmitted by exposure to contaminated blood or blood products, exposure
to certain body tissues or fluids, by sexual contact or by an infected mother to the newborn child.
The cobas® TaqScreen MPX Test, v2.0 is a qualitative multiplex test that enables the
simultaneous detection and discrimination of HIV RNA, HCV RNA and HBV DNA and the
internal Control in a single test of an infected pool or individual plasma donation. The cobas®
TaqScreen MPX Test, v2.0 uses a generic nucleic acid preparation technique on the cobas®
Ampliprep Instrument. HIV RNA (HIV-1 Group M and O RNA, , HIV-2 RNA). HCV RNA and
HBV DNA are amplified, detected and discriminated using automated, real time PCR on the
cobas® TaqMan® Analyzer. The test does not discriminate between HIV-1 Group M, HIV-1
Group O and HIV-2. The test also incorporates an Internal Control for monitoring test
performance in each individual test as well as the AmpErase enzyme to reduce potential
contamination by previously amplified material (amlicon). Discriminatory tests for HIV-1 Group
O and HIV-2 are not available from Roche
II.
Specimen Collection and Storage
Living donor specimen:
Blood collected in EDTA tube(s) may be stored for up to 48 hours at 2-25 oC and up to 72
hours at 2-8oC
Following separation from cells, plasma may be stored at 2-8 oC for up to 7 days, and up
to 30 days at <-18 oC with 3 freeze/thaw cycles.
Cadaveric blood specimen-EDTA plasma or serum may be used
Specimens from cadaveric donors displaying a straw to pink color are classified as
Moderately Hemolyzed and specimens displaying a red to dard-red or brown color are
classified as Highly Hemolyzed specimens.
Cadaveric blood collected in EDTA or serum tube(s) may be stored for up to 24 hours at
2-30 oC followed by up to 24 hours at 2-25 oC prior to plasma or serum separation from
red blood cells. For storage longer than 48 hours, separate the plasma or serum from the
red blood cells by centrifugation and remove the separated plasma or serum from the red
blood cells prior to storage. Following removal, plasma or serum may be stored at 2-8oC
for an additional 8 days. Alternatively, plasma or serum may be stored at ≤-18 oC for up
to 30 days after removal from red blood cells with 3 freeze/thaw cycles.
Cadaveric Plasma or serum is tested at 1:5 dilution for each MPX and/or WNV
PROCEDURE MANUAL
UNIVERSITY HEALTH NETWORK / MOUNT SINAI HOSPITAL MICROBIOLOGY DEPARTMENT
NOTE: This is a CONTROLLED document. Any documents appearing in paper form that are not stamped in red "MASTER COPY" are not controlled and
should be checked against the document (titled as above) on the server prior to use
D:\106748206.doc
Policy # MI/MD/v50
Microbiology Department
Policy & Procedure Manual
Section: Molecular Diagnostic Tests Manual
Page 117 of
291
Do NOT freeze whole blood.
Heparin Plasma is NOT acceptable
Donor Serology and Molecular Testing Specimen Storage
III.
Materials, Equipments and Facilities
Reagents:
1. Cobas® TaqScreen MPX Test (CS1-CS4) stored at 2-8 oC
magnetic glass particles reagent cassette
lysis reagent cassette
Multi-reagent cassette
Test-specific reagent cassette
2. Cobas® TaqScreen MPX/WNV Control Kit stored at 2-8 oC
HIV-1M positive control
HIV-1 O positive control
HIV-2 positive control
HCV positive control
HBV positive control
TaqScreen negative control
3. Cobas® TaqScreen Wash Reagent stored at 15-30 oC
4. Cobas® TaqScreen Cadaveric Specimen Diluents:
unopened CADV SPEC DIL is stable until the expiration date.
Once opened, this reagent is stable for 30 days at 2-8 oC or until the expiration date,
whichever comes first.
Equipment:
Hamilton MICROLAB STAR/STARlet IVD Pipettor
Cobas® Ampliprep Instrument
Cobas® Taqman Analyzer
Pooling, AMPLILINK and Data Management Workstation, Data Station
Pipette tips (high volume CO-RE tips (1000mL), filter
Waste bags
Sample Input tubes (S-tubes) and barcode clips
24 and 32 test tube sample carrier
Plate carrier
Tip carrier
Sample Racks (SK24)
SK24 Rack Carrier
SPUs
PROCEDURE MANUAL
UNIVERSITY HEALTH NETWORK / MOUNT SINAI HOSPITAL MICROBIOLOGY DEPARTMENT
NOTE: This is a CONTROLLED document. Any documents appearing in paper form that are not stamped in red "MASTER COPY" are not controlled and
should be checked against the document (titled as above) on the server prior to use
D:\106748206.doc
Policy # MI/MD/v50
Microbiology Department
Policy & Procedure Manual
Section: Molecular Diagnostic Tests Manual
IV.
Page 118 of
291
SPU racks
Reagent Racks
Racks of K-tips
K-tubes
BD Vacutainer
Procedure
1. Take out MPX reagent kits and controls from the fridge, and leave at room temperature.
2. If Hamilton STAR was off during the weekend, turn on Hamilton STAR at least 1 minute
before turn on the computer!
3. Re-start computers for Pooling Manager, and Data Manager every week day.
4. Perform daily maintenance procedures for HAMILTON and AMPLIPREP.
5. Use Pooling Manager Terminal for the maintenance of Hamilton:
a. Click Wizard icon
b. Click Maintenance Tab
c. Click Daily Maintenance
d. Click Start
e. Follow instructions to finish daily maintenance procedure
Perform weekly maintenance every Tuesday.
!Push Back Up tape into driver every Tuesday morning after the weekly maintenance
Turn off Hamilton STAR and computer at the end of the Friday!
* Do not touch the red scanner
* Clean inside of HAMILTON with de-ionized water and 70%alcohol
* Clean the pipette ejector ledge with alcohol
5. Loading of reagents and disposables in AmpliPrep
a. Loading of Reagent Cassettes in AmpliPrep
Place all CS1 for 8MPX onto a same reagent cassette
Place CS2, CS3, CS4 for MPX onto to a separate reagent cassettes
Load the reagent cassette containing all CS1 onto position A of the AmpliPrep
Load the reagent cassettes containing CS2, CS3, CS4 onto position B,C,D or E of the
AMPLIPREP
b. Loading of Disposables in AmpliPrep
Load enough SPUs in the SPU rack(s) and load the rack(s) onto position J, K or L of the
AmpliPrep.
PROCEDURE MANUAL
UNIVERSITY HEALTH NETWORK / MOUNT SINAI HOSPITAL MICROBIOLOGY DEPARTMENT
NOTE: This is a CONTROLLED document. Any documents appearing in paper form that are not stamped in red "MASTER COPY" are not controlled and
should be checked against the document (titled as above) on the server prior to use
D:\106748206.doc
Policy # MI/MD/v50
Microbiology Department
Policy & Procedure Manual
Section: Molecular Diagnostic Tests Manual
Page 119 of
291
Load enough K-tubes onto position M-N of the AmpliPrep.
Load enough K-tips onto position O-P of the AmpliPrep.
! Do NOT unload any partial rack of K-tube or K-tips even the LEDs are green
! Position M-N are designated for K-tubes, position O-P are designated for K-tips.
6. Prepare Sample rack and S-tube rack
a. Using the Work list, match labels of sample tube with the 6mL BD Vacutainer tube
b. Add 1200ul plasma of Living Donor samples to the empty 6mL BD Vacutainer tubes
c. Add 300ul plasma/serum Cadaveric samples to the 6mL BD Vacutainer tube with 1200
uL Cadaveric diluent
d. Centrifuge at 3000 rpm for 10 minutes
! Make sure the sample tube is free of bubbles, clots and flocculates.
e. De-cap and place 6mL BD Vacutainer tubes onto 32 test tube sample carrier
f. Take out enough clips and S-tubes (4 controls plus the sample number)
g. Slightly bend the clip before place it onto the S-tubes rack starting position#1
h. Place S-tubes into clips
i. Place S-tube rack onto SK24 Rack Carrier
j. De-cap S-tubes
7. Set up MPX NEGATIVE CONTROL and POSITIVE CONTROL racks
!!!Mix controls by inversion at least 3 times, avoiding the creation of bubbles, as
specified below:
Inversion each time is defined as turning the control upside down and right side
up again
Within inversion each time, hold the control for at least 2 seconds in each
orientation (i.e. turn the control upside down, and hold for at least 2 seconds.
Then, turn the control right side up again, and hold for at least 2 seconds
a. Place clean Kleenex paper on Control Working Area
b. Remove positive control lids and leave on Kleenex paper.
c. Load positive controls in Positive Control Rack Position #1, 2, and 3 with barcode labels
visible.
Yellow cap positive control is in position#1
Orange cap positive control is in position#2
Red cap positive control is in position#3
CHANGE GLOVES AFTER SETTING UP POSITIVE CONTROL RACK
d. Load negative control in negative Control Rack Position #1 with barcode label visible.
! Pop bubbles from control tubes by lightly tapping with control tube cover
! Return Control boxes back to fridge after finish loading.
8. Pooling Manager Terminal
a. Click Wizard Icon
PROCEDURE MANUAL
UNIVERSITY HEALTH NETWORK / MOUNT SINAI HOSPITAL MICROBIOLOGY DEPARTMENT
NOTE: This is a CONTROLLED document. Any documents appearing in paper form that are not stamped in red "MASTER COPY" are not controlled and
should be checked against the document (titled as above) on the server prior to use
D:\106748206.doc
Policy # MI/MD/v50
Microbiology Department
Policy & Procedure Manual
Section: Molecular Diagnostic Tests Manual
Page 120 of
291
b. Make sure Batch Run is selected
c. Click Assay/Start
b.
c.
d.
e.
f.
g.
h.
i.
Choose MPX v2.0
Click Next
Click Pools of 1
Follow the instruction to load sample rack
Click Done button after all samples are loaded
All required quantities of S-Tubes,SK24 racks,tips, RMEC (roche manufactured
external controls) are calculated
PROCEDURE MANUAL
UNIVERSITY HEALTH NETWORK / MOUNT SINAI HOSPITAL MICROBIOLOGY DEPARTMENT
NOTE: This is a CONTROLLED document. Any documents appearing in paper form that are not stamped in red "MASTER COPY" are not controlled and
should be checked against the document (titled as above) on the server prior to use
D:\106748206.doc
Policy # MI/MD/v50
Microbiology Department
Policy & Procedure Manual
Section: Molecular Diagnostic Tests Manual
Page 121 of
291
f.
h.
j. Follow instructions to load S-tube rack, control racks, and pipette tip rack.
PROCEDURE MANUAL
UNIVERSITY HEALTH NETWORK / MOUNT SINAI HOSPITAL MICROBIOLOGY DEPARTMENT
NOTE: This is a CONTROLLED document. Any documents appearing in paper form that are not stamped in red "MASTER COPY" are not controlled and
should be checked against the document (titled as above) on the server prior to use
D:\106748206.doc
Policy # MI/MD/v50
Microbiology Department
Policy & Procedure Manual
Section: Molecular Diagnostic Tests Manual
Page 122 of
291
i.
k.
l.
m.
n.
After tips are loaded, pipetting is automatically started
All racks are automatically unloaded after the pooling procedure is finished
Re-cap the S-tubes .Double check that caps are not so tight and properly placed
Press the ‘ctrl’ on the keyboard + the ‘logoff’ button on the lower right corner of
the pooling wizard to exit the pooling wizard
o. To start a new pooling run, click pooling wizard and click tab Batch Run
p. If window is freeze, press Ctrl key and Logoff icon at the same time to active the
windows
9. Extraction/Amplification/Detection
AMPLIPREP USER ID: MSH
PASSWORD: Msh12345
Load in AMPLIPREP – AMPLIPREP Terminal
PROCEDURE MANUAL
UNIVERSITY HEALTH NETWORK / MOUNT SINAI HOSPITAL MICROBIOLOGY DEPARTMENT
NOTE: This is a CONTROLLED document. Any documents appearing in paper form that are not stamped in red "MASTER COPY" are not controlled and
should be checked against the document (titled as above) on the server prior to use
D:\106748206.doc
Policy # MI/MD/v50
Microbiology Department
Policy & Procedure Manual
Section: Molecular Diagnostic Tests Manual
Page 123 of
291
!NO order needs to be manually created. The order is automatically
transmitted from Pooling manager to Ampliprep
a. In the Amplilink computer, click order icon to check if the order is send to Amliprep.
If the order is not sent over, proceed the procedure of Synchronize Hamilton with
Amliprep
b. Remove S-tube rack from carrier. Load S- tube rack in AMPLIPREP
(Start with Track F), check the End time (Time to transfer k-tubes to Taqman)
c. Load only FULL K-tube / K-tip rack when required.
d. When the run is complete, the indicator light on the Cobas® Ampliprep will be
orange, and SK24 racks may be removed.
10. Load the SK24 racks directly to the Cobas® TaqMan.
11. If the Amplification and detection run does not start automatically, click Start
12. Check finished time.
13. When testing is finished in Cobas® TaqMan , the results are automatically transmitted to
Data Manager.
!DO NOT NEED TO MANULLY ACCEPT RESULTS FROM Cobas® TaqMan
14. Print Results from Data Manager (follow instructions) Print Donor Result Report only
a. DMS
b. Query Tab
c. Today
d. Search
e. Highlight batch, Next
f. Confirm any information in Alarm Review
g. Donor Review Tab,
h. Print
If all sample tests are negative, only check Donor Result Report
If there is positive result for patient’s sample, check both PCR Batch Report
and Donor Result Report
15. Report results in LIS manually.
16. Clean Up and Shutdown Procedures
a. Check number of reagents left and write in CS1 then cover with parafilm and store in
fridge.
b. Discard used SPU tubes and save clean ones.
PROCEDURE MANUAL
UNIVERSITY HEALTH NETWORK / MOUNT SINAI HOSPITAL MICROBIOLOGY DEPARTMENT
NOTE: This is a CONTROLLED document. Any documents appearing in paper form that are not stamped in red "MASTER COPY" are not controlled and
should be checked against the document (titled as above) on the server prior to use
D:\106748206.doc
Page 124 of
291
Policy # MI/MD/v50
Microbiology Department
Policy & Procedure Manual
Section: Molecular Diagnostic Tests Manual
V.
Synchronize Hamilton with Ampliprep
VI.
Click Pooling icon
Click Amplilink Status tab
Under Amplilink workstation, click PCR-LAB-W1-220
Under Current Batches, click the Rack ID
Click Synchronize button
Assay Validation
All controls have to be valid before specimen results are released.
All result data are stored in main frame computer HPR 300XR in Rm 1438.
VII.
Interpretatiion of Results
If all controls are valid;
Non Reactive: reported as Negative
Reactive: reported as Positive.
Invalid: repeat once. If still invalid, reported as Indeterminate
VIII. Reporting
For Negative Result
Result
NonReactive
NonReactive
CT Values
HIV│HBV│HCV│IC
─│─│ ─ │###
─│─│ ─ │─
Internal
Control
Valid
Invalid
Report
Comment
8MPX:Negative@RMPx
Verify 8MPX
If there is enough sample for
repeating, repeat the test
Order 8COM to record initial
invalid result
After repeating, if the IC is
still invalid, result as
following:
8MPX: Indeterminate@RMPx
Verify 8MPX
In the
comment for
8COM, record
the 2nd result
Verify 8COM
If there is not enough sample
for repeating, result as
following:
8MPX: Indeterminate@RMPx
In the comment for 8MPX,
type:
Not Sufficient Quantity for
repeating
Verify 8MPX
Verify 8COM
PROCEDURE MANUAL
UNIVERSITY HEALTH NETWORK / MOUNT SINAI HOSPITAL MICROBIOLOGY DEPARTMENT
NOTE: This is a CONTROLLED document. Any documents appearing in paper form that are not stamped in red "MASTER COPY" are not controlled and
should be checked against the document (titled as above) on the server prior to use
D:\106748206.doc
Policy # MI/MD/v50
Microbiology Department
Policy & Procedure Manual
Section: Molecular Diagnostic Tests Manual
Page 125 of
291
For Positive Result
Result
HBV
Reactive
HIV
Reactive
HCV
Reactive
CT Values
HIV│HBV│HCV│IC
─│###│ ─ │###
###│─│ ─ │###
Internal
Control
Valid
Valid
Valid
─│─│ ###│###
Architect Result
8HAGX:Negative
8HBC:Positive
Or
8HAGX:Positive
8HBC:Positive
Or
8HAGX:Positive
8HBC:Negative
Repeat in
Duplicate
No
8HAGX:Negative
8HBC:Negative
Or
No serology
results available
Yes
8TSC:@MOH+
8TSC: Positive
No
Report
1. 8MPX: Positive@RMPx
HBV DNA Detected
2. Order 8COM in LIS and record HBV CT
a. 8MPX: Positive@RMPx
HBV DNA Detected
b. Order 8COM in LIS and record HBV CT
Enough Volume for repeating:
a. 2/3 Positive8MPX :Positive@RMPx
HBV DNA Repeatedly
Detected
Order 8COM in LIS and record all HBV CT
b. 2/3 Negative8MPX: Negative@RMPx
Order 8COM in LIS and record all results
NSQ for repeating
8MPX :Positive@RMPx
HBV DNA Detected, not sufficient sample for
repeating
a. 8MPX:Positive@RMPx
HIV RNA Detected
b. Order 8COM in LIS and record HIV CT
8TSC:Negative
Or
No serology result
availalbe
Yes
Enough Volume for repeating:
a. 2/3 Positive8MPX:Positive@RMPx
HIV RNA Repeatedly Detected
Order 8COM in LIS and record all HIV CT
b. 2/3 Negative8MPX: Negative@RMPx
Order 8COM in LIS and record all results
8HCA: Positive
Or
8HCA:@MOH+
No
NSQ for repeating
8MPX :Positive@RMPx
HIV RNA Detected, not sufficient sample for
repeating
8MPX: Positive@RMPx
HCV RNA Detected
8HCA:Negative
Or
No serology result
available
Yes
Enough Volume for repeating:
a. 2/3 Positive8MPX:Positive@RMPx
HCV RNA Repeatedly
Detected
Order 8COM in LIS and record all HCV CT
b. 2/3 Negative8MPX: Negative@RMPx
Order 8COM in LIS and record all results
NSQ for repeating
8MPX :Positive@RMPx
HCV RNA Detected, not sufficient sample for
repeating
PROCEDURE MANUAL
UNIVERSITY HEALTH NETWORK / MOUNT SINAI HOSPITAL MICROBIOLOGY DEPARTMENT
NOTE: This is a CONTROLLED document. Any documents appearing in paper form that are not stamped in red "MASTER COPY" are not controlled and
should be checked against the document (titled as above) on the server prior to use
D:\106748206.doc
Policy # MI/MD/v50
Microbiology Department
Policy & Procedure Manual
Section: Molecular Diagnostic Tests Manual
IX.
Trouble Shooting:
Problem
Internal Control fails
on ONE specimen
Internal Control fails
on a specimen for the
second time
Pooling manager
computer is frozen
while loading
specimen
X.
Page 126 of
291
Solutions
Repeat specimen
Result specimen as: Invalid
In result comment: hit F5 to add comment “@SPIN”
“Likely due to specimen integrity, unable to obtain
valid test result after repeated attempts)”.
Verify result.
1. Press Ctrl key and Logoff icon at the same time to
active the windows
2. If computer is still frozen, press Ctrl+Alt+Del to
restart the pooling manager computer
3. If the computer is still frozen, turned off the Hamilton
STAR and computer
4. Manually unload the specimens from the Hamilton
STAR
5. Wait for couple of minutes, turn back the Hamilton
STAR at least 1 minute before turn on the computer
6. Wait for the log on screen before pressing
Ctrl+Alt+Del to log in
7. Restart the pooling procedure
Quality Control :
Run External Positive and negative control (previously tested CAP proficiency samples)
monthly.
XI.
CAP and NML provide external proficiency testing.
Reference:
Roche cobas s 201 System
Hardware and Software reference Manual, P/N 05575982190-01.
PDM Software Software Guide,P/N 05575974190-01.
Operator’s Manual for Use with small Pools(Pools of 1 and 6) P/N 05576008190-01
Roche Hot Line Tel# 877-273-3433
michael.salem@roche.com
xinyu.song@roche.com
PROCEDURE MANUAL
UNIVERSITY HEALTH NETWORK / MOUNT SINAI HOSPITAL MICROBIOLOGY DEPARTMENT
NOTE: This is a CONTROLLED document. Any documents appearing in paper form that are not stamped in red "MASTER COPY" are not controlled and
should be checked against the document (titled as above) on the server prior to use
D:\106748206.doc
Policy # MI/MD/v50
Microbiology Department
Policy & Procedure Manual
Section: Molecular Diagnostic Tests Manual
Page 127 of
291
Herpes simplex Virus/Varicella-Zoster Virus PCR by Rotorgene
I.
Introduction
Herpes simplex virus (HSV) and Varicella zoster virus (VZV) are doube stranded DNA virus in
the family Herpesviridae. HSV and VZV remain in the host as a latent lifelong infection in the
peripheral nervous system, and can reactivate in the host, causing serious complications in
immunocompromised patients.
The RealStar alpha Herpesvirus PCR Kit is a real-time PCR, for the qualitative detection and
differentiation of Herpes simlex virus type 1, type 2, and Varicella zoster virus in a single PCR
reaction.
II.
Collection and Transport
Sterile body fluids, swabs in viral transport media.
Store collected specimens at 4oC, process specimens as soon as possible.
III. Specimen Processing
Please refer to Nucleic Acid Extraction – Biomerieux NucliSENS easyMAG
IV. Materials, Equipments and Facilities:
Clean Room with dedicated Biosafety Cabinet (MIBCT3), freezer (MIFTG), gowns and gloves
Specimen Preparation area with Biosafety Cabinet (MIBCT7 or MIBCT8)
and microcentrifuge(MICT17)
Vortex
Detection Area for Rotor-Gene 6000
Rotor-Gene 6000 Multiplexing System programmed for ALTONA HSV & VZV
36-Well Loading Block (pre-cooled to 4oC)
36-Well 6000 Series Rotor & Locking Ring
72-Well Loading Block (pre-cooled to 4oC)
72-Well 6000 Series Rotor & Locking Ring
0.1 mL Strip Tubes and Caps
0.2mL microtubes
Aerosol Resistant Tips (ART)
Variable volume pipettes:
1 to 20 uL
10 to 200 uL
100 to 1000 uL
RealStar alpha Herpes PCR Kit v1.0: stored at -20C until needed
PROCEDURE MANUAL
UNIVERSITY HEALTH NETWORK / MOUNT SINAI HOSPITAL MICROBIOLOGY DEPARTMENT
NOTE: This is a CONTROLLED document. Any documents appearing in paper form that are not stamped in red "MASTER COPY" are not controlled and
should be checked against the document (titled as above) on the server prior to use
D:\106748206.doc
Policy # MI/MD/v50
Microbiology Department
Policy & Procedure Manual
Section: Molecular Diagnostic Tests Manual
Page 128 of
291
Component Master A
Component Master B
HSV-1 Positive Control
HSV-2 Positive Control
VZV Positive Control
PCR Water
alpha Herpes Internal Control
External Control: To be run when a new lot is used, during training or if QC failure occurs.
GENERAL PRECAUTIONS:
V.
There must be separate PCR work areas:
o Clean room
o Specimen preparation room
Amplification room Supplies and equipment must be dedicated to each PCR
area and not used for other activities or moved between areas.
Change lab coats and gloves between work areas. Only blue gowns are to be
worn in the clean room.
Use only filtered pipette tips
Use only sterile RNase, Dnase-free microcentrifuge tubes
Use sterile, disposable polypropylene tubes throughout the procedure
Always wear powder-free gloves when handling reagents
Change gloves frequently and keep tubes closed whenever possible
Thaw components thoroughly at room temperature
Mix components and centrifuge briefly
Work quickly in the cooling block
Use 1% sodium hypochloride or Eliminase to disinfect equipment and
surfaces and then rinse with 70% alcohol or water.
Detection Set-up:
Organize eluates and controls according to worklist.
In the Clean Room:
(Change into dedicated clean room gown and gloves, work in Biosafety Cabinet)
Take out the necessary number of alpha Herpes Components Master A and Master B vials (12 tests per
vial) from the freezer and thoroughly thaw inside the Biosafety Cabinet.
Prepare alpha Herpes Master Mix (number of test samples + controls + 1 extra test) required
according to the chart.
Work quickly. Protect Master A and Master B from light.
PROCEDURE MANUAL
UNIVERSITY HEALTH NETWORK / MOUNT SINAI HOSPITAL MICROBIOLOGY DEPARTMENT
NOTE: This is a CONTROLLED document. Any documents appearing in paper form that are not stamped in red "MASTER COPY" are not controlled and
should be checked against the document (titled as above) on the server prior to use
D:\106748206.doc
Policy # MI/MD/v50
Microbiology Department
Policy & Procedure Manual
Section: Molecular Diagnostic Tests Manual
Page 129 of
291
Mix gently, DO NOT VORTEX.
Avoid repeated thawing and freezing of Master A and Master B (maximum twice).
After Master A has been mixed to Master B it cannot be frozen again.
No. of samples
1
2
3
4
5
6
7
8
9
10
11
12
Preparation of Master Mix
Master A (µl)
5
10
15
20
25
30
35
40
45
50
55
60
Master B (µl)
15
30
45
60
75
90
105
120
135
150
165
180
a.
Place microtubes into the Cooling Block (pre-cooled to 4oC).
b.
Pipette 20 uL alpha Herpes Master Mix (A+B) into each microtubes
a.
Pipette 1.0 uL of internal control (IC) into the microtubes designated for the Positive controls
(HSV-1, HSV-2, VZV) and water (PCR grade).
b.
Pipette 10uL water (PCR grade) into the negative control micro tube. Mix up and down 3X and
cap tightly. Label each microtubes 1,2,3…. before leaving clean room.
c.
Changed out of dedicated clean room gown.
Specimen Processing Area: (Changed into specimen area lab coat)
Carefully pipette 10 uL each of eluate sample, Positive controls (HSV-1, HSV-2, and VZV), and
external QC (if using) directly into the microtubes containg alpha Herpes Master Mix. Pipette up
and down three times (3X) into the Master Mix to mix sample with Master Mix. Close the cap
tightly.
PROCEDURE MANUAL
UNIVERSITY HEALTH NETWORK / MOUNT SINAI HOSPITAL MICROBIOLOGY DEPARTMENT
NOTE: This is a CONTROLLED document. Any documents appearing in paper form that are not stamped in red "MASTER COPY" are not controlled and
should be checked against the document (titled as above) on the server prior to use
D:\106748206.doc
Policy # MI/MD/v50
Microbiology Department
Policy & Procedure Manual
Section: Molecular Diagnostic Tests Manual
Page 130 of
291
Detection Area:
Check each microtube before loading. Make sure the microtube is capped tightly and
there is no bubble at the bottom of the microtube.
Load microtubes into rotor (e.g. 72 Rotor or 36 Rotor) and secure the locking ring.
Fill the empty position of the rotor using empty microtubes.
Place Rotor in to the Rotor-Gene 6000.
On the Rotor-Gene 6000:
a. Turn on computer, turn on Rotorgene;
b. FOR THE BLUE ROTORGENE ONLY. Choose clinical icon; pass word “msh”; press “→”
button;
c. Double click(left on the mouse) “Rotor-Gene 6000 series software 1.7” icon
d. Wait for “Initializing machine…..”
e. Highlight “ALTONA HSV & VZV ” assay;
f. Press “New” button;
g. Highlighting the correct Rotor type you are using
h. 72-well Rotor (Blue)
i. 36-well Rotor (Red)
j. Click the “Locking Ring Attached” option, to confirm Locking Ring is in place.
k. Press “Next” button
l. Enter initials in Operator space. Enter kit lot number and the Rotor-Gene Colour (ie.Red/Blue) in
the Notes box. Verify the Reaction Volume is 30ul.
m. Press “Next” button.
n. Temperature Profile window pops up; press “Next”.
o. Summary window appears; press “Start Run”. The RotorGene will start.
p. Save as window appears; go to My documents -Open–select hsv & vzv result folder- Open
Press Save –HSV VZV yyyy-mm-dd (run no.)
q. Edit Samples window. Enter sample LIS numbers using barcode scanner. Enter HSV-1, HSV-2,
VZV as Positive Controls, and water as negative Control.
Name
Type
Select
Sample
Unknown
Yes
Positive Controls HSV-1, HSV-2, VZV
Positive Control
Yes
Water
Negative Control
Yes
r. Once finishing all samples, press Finish button.
s. Once cycling screen comes on, click “Named On” button.
PROCEDURE MANUAL
UNIVERSITY HEALTH NETWORK / MOUNT SINAI HOSPITAL MICROBIOLOGY DEPARTMENT
NOTE: This is a CONTROLLED document. Any documents appearing in paper form that are not stamped in red "MASTER COPY" are not controlled and
should be checked against the document (titled as above) on the server prior to use
D:\106748206.doc
Policy # MI/MD/v50
Microbiology Department
Policy & Procedure Manual
Section: Molecular Diagnostic Tests Manual
Page 131 of
291
To analyze and print HSV and VZV report after a run is finished:
The run is done when Profile Program reads: Run has completed.
Analyze raw data by clicking on the each of these channels (one at a time).
Green channel (VZV), Red channel (HSV-2), Orange channel (HSV-1) and Yellow channel (IC).
These tabs are found on the second menu bar from the top, on the left hand side.
Select the Green Channel (VZV). Click “All Off” (bottom right). Select sample “water
Negative Control” and “VZV Positive Control”. Click on Autoscale (bottom left).
Compare each specimen curve to the water curve and the VZV Positive Control one at a time (by
clicking each sample on and off then proceeding to the next sample). A positive curve will have
a sigmoidal shape. A negative result will be a relatively flat line, like the water. Make a note of
all positives on the worklist.
Select the Orange Channel (HSV-1). Click “All Off”. Select sample “water Negative
Control” and “HSV-1 Positive Control”. Click on Autoscale (bottom left).
Compare each specimen curve to the water curve and the HSV-1 Positive Control one at a time
(by clicking each sample on and off then proceeding to the next sample). A positive curve will
have a sigmoidal shape. A negative result will be a relatively flat line, like the water. Make a
note of all positives on the worklist.
Select the Red Channel (HSV-2). Click “All Off”. Select sample “water Negative Control”
and “HSV-2 Positive Control”. Click on Autoscale (bottom left).
Compare each specimen curve to the water curve and the HSV-2 Positive Control one at a time
(by clicking each sample on and off then proceeding to the next sample). A positive curve will
have a sigmoidal shape. A negative result will be a relatively flat line, like the water. Make a
note of all positives on the worklist.
a.
b.
c.
d.
e.
Click on “Named On”
Perform curve Analysis (Get report): Click “Analysis” on the top tool bar.
Analysis floating window pops up;
Click Quantitation Analysis.
Quantitation window is brought up to the front. There should be four channels: Green (VZV),
Orange (HSV-1), Red (HSV-2) and Yellow (IC).
f.
g.
h.
i.
j.
k.
l.
Highlight Cycling A. Green (VZV) option and press Show.
Maximize cycling green window (or the channel you are working on)
Press button “Slope Correct” on the top.
Press button “Ignore first” on the top, and type “5”, press OK.
Set threshold at 0.05. A threshold line will appear on the screen.
Move threshold line to above the noise (i.e. Negative specimens)
To Print reports: Press “Reports”.
PROCEDURE MANUAL
UNIVERSITY HEALTH NETWORK / MOUNT SINAI HOSPITAL MICROBIOLOGY DEPARTMENT
NOTE: This is a CONTROLLED document. Any documents appearing in paper form that are not stamped in red "MASTER COPY" are not controlled and
should be checked against the document (titled as above) on the server prior to use
D:\106748206.doc
Policy # MI/MD/v50
Microbiology Department
Policy & Procedure Manual
Section: Molecular Diagnostic Tests Manual
m.
n.
o.
p.
q.
r.
s.
t.
Page 132 of
291
Report Browser window pops up.
Choose Cycling A. Green (Page 1).
Highlight Quantitation full report, press “Show”.
Maximize the report window, check that only the positives that you have identified from the raw
data review are positive and have a crosspoint (ct value).
Print pages 1-4 for the green channel; pages 2-4 for all the other channels: orange, red.
Repeat the steps above 3-15 for Cycling A. Orange(HSV-1), Cycling A. Red (HSV-2).
Yellow channel Analysis. Go to the floating Analysis window: Quantitation tab, select Cycling
A. Yellow -the internal control (IC), select Show.
Maximize the graph Quantitation Analysis –Cycling A. Yellow.
Select Slope Correct. Select Ignore first and type “5” press OK (this will ignore the readings in
the first 5 cycles of the run).
Set the threshold (right-hand side middle) at 0.05. A threshold line will appear on your graph
screen. Move the threshold line to above the noise.
Press Reports. Select Cycling A.Yellow. Select Quantitation (Full report). Select Show.
All samples should have a positive IC curve, and a cycle number in the Ct column.
Print pages 2-4.
(For Cycling A. Yellow report, if there is message of “NEG (Multi Ct)” for any specimen, you
have to go back to check Raw Data of cycling A.Yellow. If all specimens are amplified, adjust
the threshold in Quantitation Analysis for Cycling A.Yellow, so that all samples have one Ct.
Adjust the threshold line so that the threshold line crosses the curve at only one point.)
Close the outer most window.
“Save changes to Altona HSV & VZV yyyy-mm-dd?” Select Yes.
Shut down the computer, and switch off the Rotor-Gene.
At the end of the day, follow the cleaning protocol below using 1% hypochorite followed by 70%
alcohol:
Clean Room:
Clean Biological Safety Cabinet, pipettors, and bench tops
Specimen Preparation Area:
Clean Biological Safety Cabinet, pipettors, centrifuge, and bench top.
Cap discard container.
Wash racks.
Amplification Area:
Discard microtubes into a disposal bag and tight the bag.
Discard the bag into biohazard waster container.
Perform the cleaning procedure according the daily maintenance sheet.
PROCEDURE MANUAL
UNIVERSITY HEALTH NETWORK / MOUNT SINAI HOSPITAL MICROBIOLOGY DEPARTMENT
NOTE: This is a CONTROLLED document. Any documents appearing in paper form that are not stamped in red "MASTER COPY" are not controlled and
should be checked against the document (titled as above) on the server prior to use
D:\106748206.doc
Policy # MI/MD/v50
Microbiology Department
Policy & Procedure Manual
Section: Molecular Diagnostic Tests Manual
VI.
Page 133 of
291
Interpretation:
Green
Channel
(VZV)
Orange
Channel
(HSV-1)
+
-
-
+
-
-
Red
Channel
(HSV-2)
-
Yellow
Channel
(IC)
Interpretations
+/-
Positive for VZV
-*
+/-
Positive for HSV-1
-
+
+/-
Positive for HSV-2
-
-
+
-
-
-
Negative for HSV and VZV
INVALID: internal control failed to
amplify. Dilute sample 1:4 and re-extract
and test.
* Cross-talk: Samples and controls that are strong positives in the Orange HSV-1 Channel, can be
observed to exhibit a diminished weak curve in the Red HSV-2 Channel (y-axis fluorescence is very
weak); these samples and controls are not HSV-2 positive.
PCR Positives from sterile sites: CSF, eye specimens, biopsy, tissues; should be repeated a second
time. Re-extract the sample on the easyMAG and repeat the PCR. Release a preliminary report,
see below “Reporting”.
VI.
Reporting:
Report HSV and VZV results for sterile body fluids, tissues, eye swabs, and skin/lesion specimens only.
Report HSV results only on oral swabs/washings, and BALs.
Negative for HSV and VZV.
Under media on the back of the LIS workcard. PCHZ: F6 to add run date
Report on the front of the LIS workcard from the keypad select: }HVZ}HVZ-
Negative for Herpes simplex virus.
Negative for Varicella zoster virus.
This is a research test.
PROCEDURE MANUAL
UNIVERSITY HEALTH NETWORK / MOUNT SINAI HOSPITAL MICROBIOLOGY DEPARTMENT
NOTE: This is a CONTROLLED document. Any documents appearing in paper form that are not stamped in red "MASTER COPY" are not controlled and
should be checked against the document (titled as above) on the server prior to use
D:\106748206.doc
Policy # MI/MD/v50
Microbiology Department
Policy & Procedure Manual
Section: Molecular Diagnostic Tests Manual
Page 134 of
291
Alpha Herpes Virus PCR Kit v1.0.
Altona Diagnostics Inc.
Ctrl-F to finalize the report.
Sterile sites: PRELIMINARY Positive for HSV-1, or HSV-2, or VZV.
Date the media on the back of the LIS workcard. PCHZ: F6 to add run date
Enter on the media line the cross point (ct) value: Ct=
Report the virus as an isolate in the F7 window.
Isolate #: 1
Org. ID: 15hsv1 for HSV-1
15hsv2 for HSV-2
18vzv for VZV
Open the Isolate Comment window F8.
Go to the Virology keypad, type “V”. Ctrl D. Select from the keypad: \HSV+ to add the comment
phrase:
\HSV+
DETECTED by PCR, confirmation to follow.
This is a research test.
Alpha Herpes Virus PCR Kit v1.0.
Altona Diagnostics Inc.
Grave (`) the result.
Ctrl-P to prelim the report. Call reports to ward/doctor.
Sterile sites: CONFIRMED Positive for HSV-1, or HSV-2, or VZV.
Date the media on the back of the LIS workcard. PCHZ: F6 to add run date
Enter on the media line the cross point (ct) value: Ct=
Report the virus as an isolate in the F7 window.
Isolate #: 1
Org. ID: 15hsv1 for HSV-1
15hsv2 for HSV-2
18vzv for VZV
Open the Isolate Comment window F8.
Go to the Virology keypad, type “V”. Ctrl D. Select from the keypad: \HSV+ to add the comment
phrase:
\HSV+
DETECTED by PCR, confirmed.
This is a research test.
Alpha Herpes Virus PCR Kit v1.0.
PROCEDURE MANUAL
UNIVERSITY HEALTH NETWORK / MOUNT SINAI HOSPITAL MICROBIOLOGY DEPARTMENT
NOTE: This is a CONTROLLED document. Any documents appearing in paper form that are not stamped in red "MASTER COPY" are not controlled and
should be checked against the document (titled as above) on the server prior to use
D:\106748206.doc
Policy # MI/MD/v50
Microbiology Department
Policy & Procedure Manual
Section: Molecular Diagnostic Tests Manual
Page 135 of
291
Altona Diagnostics Inc.
Grave (`) the result.
Ctrl-F to finalize the report.
Sterile sites: NOT CONFIRMED for HSV-1, or HSV-2, or VZV.
Date the media on the back of the LIS workcard. PCHZ: F6 to add run date
Isolate #: 1 must be suppressed, change to an alphabet
Front of the LIS workcard type the following:
UPDATED REPORT: Previously reported Herpes simplex virus type 1/ Herpes simplex
virus type 2/ or Varicella zoster virus not confirmed.
Report on the front of the LIS workcard (manually type):
This is a research test.
Alpha Herpes Virus PCR Kit v1.0.
Altona Diagnostics Inc.
Ctrl-F to finalize the report. Call Updated reports to ward/doctor.
Positive for HSV-1, or HSV-2, or VZV.
Date the media on the back of the LIS workcard. PCHZ: F6 to add run date
Enter on the media line the cross point (ct) value: Ct=
Report the virus as an isolate in the F7 window.
Isolate #: 1
Org. ID: 15hsv1 for HSV-1
15hsv2 for HSV-2
18vzv for VZV
Open the Isolate Comment window F8.
Go to the Virology keypad, type “V”. Ctrl D. Select from the keypad: \HSV+ to add the comment
phrase:
\HSV+
DETECTED by PCR.
This is a research test.
Alpha Herpes Virus PCR Kit v1.0.
Altona Diagnostics Inc.
Grave (`) the result.
Ctrl-F to finalize the report.
PROCEDURE MANUAL
UNIVERSITY HEALTH NETWORK / MOUNT SINAI HOSPITAL MICROBIOLOGY DEPARTMENT
NOTE: This is a CONTROLLED document. Any documents appearing in paper form that are not stamped in red "MASTER COPY" are not controlled and
should be checked against the document (titled as above) on the server prior to use
D:\106748206.doc
Policy # MI/MD/v50
Microbiology Department
Policy & Procedure Manual
Section: Molecular Diagnostic Tests Manual
Page 136 of
291
Calling Results:
HSV-1, HSV-2, and VZV DETECTED from sterile body fluids, tissues, and eye fluids/swabs should
be called to ward and/or doctor.
HSV-1, HSV-2, and VZV DETECTED from CSF must be faxed and phoned to the Medical Officer of
Health (MOH).
VZV DETECTED from skin/lesion specimens must be phoned to the ward and/or doctor and the
Infection Control Practitioner (ICP) must be notified.
IX.
Quality Control
Reagent QCs:
An External Control (external to Altona Diagnostics) is used to monitor the isolation,
amplification and detection procedures. The result must correspond to expected value supplied
by the manufacturer.
External control for VZV, HSV-1, and HSV-2 should be extracted on the on the easyMag and
run once a month and/or with each new lot.
Daily QCs:
Every run:
Each patient specimen must have an Internal Control (IC) added to monitor both extraction
and PCR inhibition.
A Positive Control is included and shows either a positive reading in Green Channel
(VZV) or a positive reading in Orange Channel (HSV-1), or a positive reading in Red
Channel (HSV-2)
A Negative Control is included and shows a negative reading in Green Channel (VZV),
Orange Channel (HSV-1), and Red Channel (HSV-2)
Report all failed QCs to senior/charge technologist.
Failed QC:
Test is invalid without satisfactory QC results.
a. Do not release results pending resolution of QC failure.
b. Inform charge/senior technologist.
c. Record in Reagent Log Chart, Instrument Maintenance Log or Incident Report where
appropriate.
d. If the QC failure was due to a simple matter of position reversal or misplacement, the run can be
released (positive QC material yielded positive result, negative yielded negative result).
PROCEDURE MANUAL
UNIVERSITY HEALTH NETWORK / MOUNT SINAI HOSPITAL MICROBIOLOGY DEPARTMENT
NOTE: This is a CONTROLLED document. Any documents appearing in paper form that are not stamped in red "MASTER COPY" are not controlled and
should be checked against the document (titled as above) on the server prior to use
D:\106748206.doc
Policy # MI/MD/v50
Microbiology Department
Policy & Procedure Manual
Section: Molecular Diagnostic Tests Manual
Page 137 of
291
e. If positive QC material yielded negative result, repeat the entire run.
f. If negative QC material yielded positive result, it may be due to cross-contamination from
adjacent positive sample within the run or carry-over contamination from previous runs via
equipment or the environment. Review procedure and equipment to establish and eliminate
potential sources of contamination.
g. The extent and nature of contamination can also be evaluated by comparing the positive rate of
the run with its expected positive rate.
h. If the contamination is extensive, it is necessary to quarantine/discard potentially contaminated
reagents and consumables and disinfect equipment and environment before repeating the run.
i. If a carry-over contamination is suspected (e.g. two or more runs with negative QC being
positive or patient samples have higher than expected positive rate and these samples are often
non-repeatable positives), it is necessary to have a thorough environmental disinfection followed
by swabbing to monitor.
j. Successful ending to a carry-over contamination may be indicated by QC results and patient
positivity rate falling back to the expected normal range and three negative environmental swabs.
X.
References:
Altona alpha Herpes Virus PCR Kit v1.0 Instructions, Altona Diagnostics
PROCEDURE MANUAL
UNIVERSITY HEALTH NETWORK / MOUNT SINAI HOSPITAL MICROBIOLOGY DEPARTMENT
NOTE: This is a CONTROLLED document. Any documents appearing in paper form that are not stamped in red "MASTER COPY" are not controlled and
should be checked against the document (titled as above) on the server prior to use
D:\106748206.doc
Policy # MI/MD/v50
Microbiology Department
Policy & Procedure Manual
Section: Molecular Diagnostic Tests Manual
Page 138 of
291
Human Metapneumovirus RT-PCR by Rotorgene
I. Introduction:
Human metapneumovirus (hMPV) is a Paramyxovirus first isolated 2001. hMPV infections may
resemble RSV, causing mild upper respiratory tract infections to severe lower respiratory tract
infections. hMPV is most frequently seen during winter months. All ages may be affected, but children
and people with compromised immune systems are most at risk.
RealStar hMPV RT-PCR Kit 1.0 is a real time PCR test for the qualitative detection of hMPV RNA;
differentiating between hMPVsubtype A and hMPV subtypeB.
II. Collection and Transport
Nasopharyngeal swabs collected in Viral Transport Media (VTM), store at 4C. Vortexed swabs on high
for 10 seconds; aliquot off the VTM and store at 4C, extract on the easyMag as soon as possible.
BAL specimens if mucoid treat with working sputolysin. Remove red blood cells and large particulate
matter by micro-centrifuging sample for 5minutes at 3000 rpm in the Eppendroff 5415 C Microcentrifuge. Aliquot supernatant and store at 4C, extract on the easyMag as soon as possible.
III. Specimen Processing
Please refer to Nucleic Acid Extraction –Biomerieux NucliSENS easyMAG
GENERAL PRECAUTIONS:
There must be separate PCR work areas:
Clean room
Specimen preparation room
Powder-free Gloves should only be in use in PCR areas. Change gloves frequently and keep
tubes closed whenever possible.
Prepare Working 1% sodium hypochloride daily.
Specimen Preparation Supplies and equipment must be dedicated to Specimen Prep Area and
not used for other activities and never used in Clean Room.
Change lab coats and gloves between work areas.
Use only Aerosol Resistant Tips (ART)
Use only sterile RNase-free, DNAse-free microtubes
Thaw components thoroughly at room temperature.
PCR work areas (Clean Room and Specimen Preparation Area) benchtops and equipment
after each shift.
Materials, Equipments and Facilities:
Clean Room: Biosafety Cabinet (MIBCT3), freezer (MIFTG)
Specimen Preparation area: Biosafety Cabinet (MIBCT7 or MIBCT8)
Rotor-Gene 6000
PROCEDURE MANUAL
UNIVERSITY HEALTH NETWORK / MOUNT SINAI HOSPITAL MICROBIOLOGY DEPARTMENT
NOTE: This is a CONTROLLED document. Any documents appearing in paper form that are not stamped in red "MASTER COPY" are not controlled and
should be checked against the document (titled as above) on the server prior to use
D:\106748206.doc
Policy # MI/MD/v50
Microbiology Department
Policy & Procedure Manual
Section: Molecular Diagnostic Tests Manual
Page 139 of
291
Rotor-Gene 6000 Multiplexing System with experiment template: Altona RealStar PIV & hMeta
72-Well Loading Block (pre-cooled to 4oC)
72-Well 6000 Series Rotor
72-Well Rotor Locking Ring
0.1 mL reaction microtubes Tubes and Caps
Variable volume Rainin pipettes: 1 to 20 uL, 10 to 200 uL, 100 to 1000 uL
Reagent: Altona RealStar hMPV RT-PCR Kit 1.0: MasterA, MasterB, Internal Control, hMPV A
Positive Control, hMPV B Positive Control, PCR Grade Water
External Control: To be run first week of the month/ or with every new lot; run during training or if QC
failure occurs.
IV. Procedure:
Prepare samples in order according to hMetapneumovirus (hMPV) worksheet. Add the following
controls to the hMetapneumovirus Worksheet:
hMPV A Positive control, hMPV B Positive Control, Negative Control (PCR grade Water).
PCR Set-up:
In the Clean Room: (Change into dedicated clean room gown and gloves, work in Biosafety Cabinet)
Remove to thaw at room temperature the required vial’s hMPV Master A and Master B (12 reactions/
vial) from the freezer.
Prepare hMPV Master Mix in Sarstedt 1.5 mL conical microtube; to load on the Eppendorf epMotion.
Prepare the number of Master Mix reactions required: Number of Test samples + 3 Controls + one
Mix gently, do not vortex. Make only enough master mix for the tests you are running. After
Master A has been added to Master B it cannot be frozen again.
Number of Reactions
hMPV Master A
hMPV Master B
Volume of Master Mix
Sample/Control Volume
1
5
10
15
10
PROCEDURE MANUAL
UNIVERSITY HEALTH NETWORK / MOUNT SINAI HOSPITAL MICROBIOLOGY DEPARTMENT
NOTE: This is a CONTROLLED document. Any documents appearing in paper form that are not stamped in red "MASTER COPY" are not controlled and
should be checked against the document (titled as above) on the server prior to use
D:\106748206.doc
Policy # MI/MD/v50
Microbiology Department
Policy & Procedure Manual
Section: Molecular Diagnostic Tests Manual
No. of Test
reactions
1
2
3
4
5
6
7
8
9
10
11
12
Page 140 of
291
hMPV Master Mix
hMPV Master A (µl)
5
10
15
20
25
30
35
40
45
50
55
60
hMPV Master B (µl)
10
20
30
40
50
60
70
80
90
100
110
120
See Eppendorf epMotion Manual for further loading and programming instructions.
Manual Loading:
Load one reaction microtube (0.1 mL) for each sample/control.
Pipette 15 uL prepared hMPV Master Mix into each reaction microtube.
Pipette 1.0 uL of internal control into the reaction microtubes designated for the 3 hMPV Controls
(hMPV A Positive Control, hMPV B Positive Control, Negative PCR Water Control .
In the Specimen Processing Area:
Pipette 10uL each of Sample/Control into reaction microtubes. Mix by pipetting 3x up and down into
the Master Mix. Cap each segment, after pipetting is completed. Check reaction microtubes before
loading into the rotor ensure the liquid levels are at the same height, and there are no bubble at the
bottom of the reaction microtube.
Load reaction microtubes into 72-Well Blue rotor, fill empty rotor spaces with blank reaction
microtubes, attach the Locking Ring. Load the rotor in Rotor-Gene 6000.
In the Rotorgene Detection Area:
a. Switch ON computer, switch ON Rotorgene;
b. FOR BLUE ROTORGENE ONLY. Choose clinical icon; pass word “msh”; press “→”
button;
c. Open “Rotor-Gene 6000 series software 1.7” icon
d. Wait for “Initializing machine…..”
e. Highlight “Altona RealStar PIV & hMeta” experiment
f. Select “New” button;
g. Highlighting the correct Rotor type you are using
h. 72-well Rotor (Blue)
PROCEDURE MANUAL
UNIVERSITY HEALTH NETWORK / MOUNT SINAI HOSPITAL MICROBIOLOGY DEPARTMENT
NOTE: This is a CONTROLLED document. Any documents appearing in paper form that are not stamped in red "MASTER COPY" are not controlled and
should be checked against the document (titled as above) on the server prior to use
D:\106748206.doc
Policy # MI/MD/v50
Microbiology Department
Policy & Procedure Manual
Section: Molecular Diagnostic Tests Manual
Page 141 of
291
i. Check the box for “Locking Ring Attached” option
j. Select “Next” button
k. Enter operator initials. In Notes enter RotorGene Colour (i.e. RED or BLUE) Reagent Lot
number. Make sure the Reaction Volume is “25µl”;
l. Select “Next” button
Temperature profile window appears, select “Next” button
m. Rotor must be loaded.
n. Summary window appears, select “Start Run” button;
o. Save As window appears; the run is given a filename with a default template. Save in My
documents in PIV & hMeta folder for the current year: e.g. Altona Realstar PIV & hMeta
20150101(1) (e.g. assay name-year-month-date-numerical run#);
a. Note: PIV & hMeta results are stored in \desktop\My Document\Altona RealStar PIV & hMeta
p. Select Save button;
q. Machine starts and Edit Samples window appears.
r. Enter sample numbers including positive and negative controls. Define the type of samples
according to the chart:
Name
Sample
hMPV A Positive
Control
hMPV B Positive
Control
PCR Grade Water
Type
Unknown
Select
Yes
Positive Control
Yes
Positive Control
Yes
Negative Control
Yes
s. Select Finish button.
t. Once cycling screen appears select “Named On” button.
To analyze and print PIV report after a run is finished:
a. The run is done when Profile Program reads: Run has completed.
b. Analyze Raw data by selecting each channel, one at a time: Green hMPV B Channel, Red
hMPV A Channel and Yellow channel Internal Control (IC).
Target
Channel
hMPV B RNA Green
hMPV A RNA Red
Internal Control Yellow
Report
Dye
FAM
Cy5
JOE
c. Select Autoscale.
Select “All Off”.
Select Negative (water) Control.
PROCEDURE MANUAL
UNIVERSITY HEALTH NETWORK / MOUNT SINAI HOSPITAL MICROBIOLOGY DEPARTMENT
NOTE: This is a CONTROLLED document. Any documents appearing in paper form that are not stamped in red "MASTER COPY" are not controlled and
should be checked against the document (titled as above) on the server prior to use
D:\106748206.doc
Policy # MI/MD/v50
Microbiology Department
Policy & Procedure Manual
Section: Molecular Diagnostic Tests Manual
d.
e.
f.
g.
h.
i.
j.
k.
l.
m.
n.
o.
p.
q.
r.
s.
t.
u.
v.
Page 142 of
291
Compare the specimen and control curves to the water one at a time.
A positive curve will have a sigmoidal shape. A negative result will be a relatively flat line, like
the water. Make a note of the positives on the hMPV Worksheet.
Select on “Named On”
Select Analysis.
Analysis floating window pops up
Select “Quantitation” Tab.
Quantitation window is brought up to the front. There should be three channels: Green hMPV
B, Red hMPV A, and Yellow (IC).
Highlight Cycling A. Green hMPV B. Select Show.
Maximize Target (Green/Red/Yellow) graph window
Select slope correct
Select Ignore first… 5 cycles
Select Threshold icon, and set threshold.
Move threshold to remove noise.(i.e. Negative specimens)
Print reports: Select Reports.
Report Browser window pops up.
Choose Cycling A. Green hMPV B. Under templates box, choose “Quantitation full report”.
Select Show button
Maximize the report window, check that only the positives that you have identified from your
raw data analysis are positive (i.e. have a crosspoint).
Choose print report. (red and yellow channels print only pages 2-4).
Once finished printing, close the report window
Analysis, perform analysis on remaining channels: Red hMPV A Channel, Yellow IC Channel.
Shut down computer:
Exit from software. “Save changes”. Select “yes”.
Select “start” button. Select “Turn off computer”.
Switch off Rotorgene
End of Shift Cleaning: Perform cleaning protocol as outlined below.
Clean Room: Wipe down with RNAse Away or NucleoClean on paper towel, followed by distilled
water, and then 70% alcohol
Biological Safety Cabinet
Pipettes
Bench tops
Specimen Preparation Area: Wipe down with Working 1% hypochloride (made daily), followed by
distilled water, and then 70% alcohol
Biological Safety Cabinet (BSC), pipettes, centrifuge, and bench top.
Seal and discard BSC waste
PROCEDURE MANUAL
UNIVERSITY HEALTH NETWORK / MOUNT SINAI HOSPITAL MICROBIOLOGY DEPARTMENT
NOTE: This is a CONTROLLED document. Any documents appearing in paper form that are not stamped in red "MASTER COPY" are not controlled and
should be checked against the document (titled as above) on the server prior to use
D:\106748206.doc
Policy # MI/MD/v50
Microbiology Department
Policy & Procedure Manual
Section: Molecular Diagnostic Tests Manual
Page 143 of
291
Wash racks.
EasyMAG , Lysis Rack, and BioHit Multi-channel Pipette: Wipe down surfaces with RNAse Away
or NucleoClean on KimWipe, followed by UltraPure water, and then 70% alcohol Wipe
Amplification Area: Wipe down surfaces with RNAse Away or NucleoClean on KimWipe, followed
by UltraPure water, and then 70% alcohol Wipe
Seal & discard reaction microtubes into biohazard waste after each run.
Perform the cleaning procedure according the daily maintenance sheet.
IV.
Interpretation and Reporting:
Red
Channel
hMPV A
Yellow Channel
(IC specific)
Interpretations
+
-
+/-
hMPV B DETECTED
-
+
+/-
hMPV A DETECTED
+
+
+/-
hMPV B DETECTED.
hMPV A DETECTED.
(ask charge/senior for confirmation)
-
-
+
hMPV NOT DETECTED
-
-
-
INVALID
Respiratory sample needs to be diluted 1:4 with
VTM and re-extracted and RT-PCR repeated.
Green
Channel
hMPV B
VTM=Viral Transport Media
hMPV B DETECTED. or hMPV A DETECTED
Report as an isolate in the (F7) Isolate Window.
Date the media on the back of the LIS workcard PCMET: F6 to add the date tested.
In the media PCMET enter crosspoint (ct) value : ct=
Report the virus as an isolate in the F7 window.
Isolate #: 1, or next available isolate number.
Org. ID: 25mpvA
Metapneumovirus A DETECTED
25mpvB
Metapneumovirus B DETECTED
PROCEDURE MANUAL
UNIVERSITY HEALTH NETWORK / MOUNT SINAI HOSPITAL MICROBIOLOGY DEPARTMENT
NOTE: This is a CONTROLLED document. Any documents appearing in paper form that are not stamped in red "MASTER COPY" are not controlled and
should be checked against the document (titled as above) on the server prior to use
D:\106748206.doc
Policy # MI/MD/v50
Microbiology Department
Policy & Procedure Manual
Section: Molecular Diagnostic Tests Manual
Page 144 of
291
The reporting isolate comment is attached to the Organism ID.
Verify All in the isolate window.
Review report entry: media, and isolates.
Finalize the report.
Call all positives to ward/doctor and Infection Control Practitioner (ICP). Document calls and emails
in the media CALL.
hMPV NOT DETECTED
Date the media on the back of the workcard. PCMET: F6 to add run date.
On the front of the workcard, select from the keypad: }MET}MET-
Negative for metapneumovirus
by RealStar hMPV RT-PCR, Altona Diagnostics.
Review report entry.
Finalize the report.
hMPV INDETERMINATE
Internal control has failed twice to amplify in a sample.
Date the media on the back of the LIS workcard. PCMET: F6 to add run date.
Select from the keypad “Failed single”, type “IC no amplification”, select >FAIL
Select from keypad ^PRMET
Under this media ^PRMET report the 1:4 dilution test result type “IC no amplification”.
Report: select from the keypad: }METChange “Negative” to INDETERMINATE; final report should appear as:
INDETERMINATE for metapneumovirus
by RealStar hMPV RT-PCR, Altona Diagnostics.
Review report entry.
Finalize the report.
V.
Quality Control
Reagent QCs:
An External Control (external to altona Diagnostics) is used to monitor the isolation,
amplification and detection procedures. The result must correspond to expected value supplied
by the manufacturer.
PROCEDURE MANUAL
UNIVERSITY HEALTH NETWORK / MOUNT SINAI HOSPITAL MICROBIOLOGY DEPARTMENT
NOTE: This is a CONTROLLED document. Any documents appearing in paper form that are not stamped in red "MASTER COPY" are not controlled and
should be checked against the document (titled as above) on the server prior to use
D:\106748206.doc
Policy # MI/MD/v50
Microbiology Department
Policy & Procedure Manual
Section: Molecular Diagnostic Tests Manual
a.
b.
c.
d.
e.
f.
g.
h.
i.
j.
Page 145 of
291
External control for hMPV A, and hMPV B should be extracted on the on the easyMag and run
once a month and/or with each new lot.
Daily QCs: Every Run
Each patient specimen must have an Internal Control (IC) added to monitor both isolation and
PCR inhibition.
A Positive Control is included and shows a positive reading in
Green hMPV B Channel or a positive reading in Red hMPV A Channel
A Negative Control is include and shows a negative reading in both Green hMPV B Channel or a
negative reading in Red hMPV A Channel
Report all failed QCs to senior/charge technologist.
Failed QC:
Test is invalid without satisfactory QC results.
Do not release results pending resolution of QC failure.
Inform charge/senior technologist.
Record in Reagent Log Chart, Instrument Maintenance Log or Incident Report where
appropriate.
If the QC failure was due to a simple matter of position reversal or misplacement, the run can be
released (positive QC material yielded positive result, negative yielded negative result).
If positive QC material yielded negative result, repeat the entire run.
If negative QC material yielded positive result, it may be due to cross-contamination from
adjacent positive sample within the run or carry-over contamination from previous runs via
equipment or the environment. Review procedure and equipment to establish and eliminate
potential sources of contamination.
The extent and nature of contamination can also be evaluated by comparing the positive rate of
the run with its expected positive rate.
If the contamination is extensive, it is necessary to quarantine/discard potentially contaminated
reagents and consumables and disinfect equipment and environment before repeating the run.
If a carry-over contamination is suspected (e.g. two or more runs with negative QC being
positive or patient samples have higher than expected positive rate and these samples are often
non-repeatable positives), it is necessary to have a thorough environmental disinfection followed
by swabbing to monitor.
Successful ending to a carry-over contamination may be indicated by QC results and patient
positivity rate falling back to the expected normal range and three negative environmental swabs.
V. References:
RealStar hMPV RT-PCR Kit v1.0, altona Diagnostics
Emerging Infectious Disease Journal Volume 14, Number1-January 2008
PROCEDURE MANUAL
UNIVERSITY HEALTH NETWORK / MOUNT SINAI HOSPITAL MICROBIOLOGY DEPARTMENT
NOTE: This is a CONTROLLED document. Any documents appearing in paper form that are not stamped in red "MASTER COPY" are not controlled and
should be checked against the document (titled as above) on the server prior to use
D:\106748206.doc
Policy # MI/MD/v50
Microbiology Department
Policy & Procedure Manual
Section: Molecular Diagnostic Tests Manual
Page 146 of
291
Human Metapneumovirus and Parainfluenza RT-PCR Bio-Rad CFX96
VIII. Introduction:
Human metapneumovirus (hMPV) is a Paramyxovirus first isolated 2001. hMPV infections may
resemble RSV, causing mild upper respiratory tract infections to severe lower respiratory tract
infections. hMPV is most frequently seen during winter months. All ages may be affected, but children
and people with compromised immune systems are most at risk.
RealStar hMPV RT-PCR Kit 1.0 is a real time PCR test for the qualitative detection of hMPV RNA;
differentiating between hMPVsubtype A and hMPV subtypeB.
Parainfluenza viruses (PIV) can cause upper and lower respiratory tract infections. Commonly seen in
children, but may occur at any age group causing severe disease in older adults, and people with
compromised immune systems. PIV-1 and PIV -2 often causes cold-like symptoms, and croup in
children. PIV-3 is often associated with bronchiolitis, bronchitis, and pneumonia. PIV-4 may cause mild
to severe respiratory tract infections.
RealStar PIV RT-PCR is a real time PCR for the qualitative detection of human PIV RNA;
differentiating PIV-1and 3, and PIV-2 and 4.
IX. Collection and Transport
Nasopharyngeal swabs collected in Viral Transport Media (VTM), store at 4C. Vortexed swabs on high
for 10 seconds; aliquot off the VTM and store at 4C, extract on the easyMag as soon as possible.
BAL specimens if mucoid treat with working sputolysin. Remove red blood cells and large particulate
matter by micro-centrifuging sample for 5minutes at 3000 rpm in the Eppendroff 5415 C Microcentrifuge. Aliquot supernatant and store at 4C, extract on the easyMag as soon as possible.
X. Specimen Processing
Please refer to Nucleic Acid Extraction –Biomerieux NucliSENS easyMAG
GENERAL PRECAUTIONS:
There must be separate PCR work areas:
Clean room
Specimen preparation room
Powder-free Gloves should only be in use in PCR areas. Change gloves frequently and keep
tubes closed whenever possible.
Prepare Working 1% sodium hypochloride daily.
Specimen Preparation Supplies and equipment must be dedicated to Specimen Prep Area and
not used for other activities and never used in Clean Room.
Change lab coats and gloves between work areas.
PROCEDURE MANUAL
UNIVERSITY HEALTH NETWORK / MOUNT SINAI HOSPITAL MICROBIOLOGY DEPARTMENT
NOTE: This is a CONTROLLED document. Any documents appearing in paper form that are not stamped in red "MASTER COPY" are not controlled and
should be checked against the document (titled as above) on the server prior to use
D:\106748206.doc
Policy # MI/MD/v50
Microbiology Department
Policy & Procedure Manual
Section: Molecular Diagnostic Tests Manual
Page 147 of
291
Use only Aerosol Resistant Tips (ART)
Use only sterile RNase-free, DNAse-free microtubes
Thaw components thoroughly at room temperature.
PCR work areas (Clean Room and Specimen Preparation Area) benchtops and equipment
after each shift.
XI. Materials, Equipments and Facilities:
Clean Room: Biosafety Cabinet (MIBCT3), freezer (MIFTG)
Specimen Preparation area: Biosafety Cabinet (MIBCT7 or MIBCT8)
BIO-RAD CFX96 Deep WellTM Real-Time System
BIO-RAD Hard-Shel®PCR Plates 96-Well WHT/CLR
BIO-RAD Microseal ®‘B’ seal Seals
BIO-RAD Optical Flat 8-Cap Strips for 0.2ml tube strips
BIO-RAD Low-Profile PCR Tubes 8-tube strip, white
96-Well Loading Block (pre-cooled to -20°C)
Variable volume Rainin pipettes: 1 to 20 uL, 10 to 200 uL, 100 to 1000 uL
Reagent: Altona RealStar hMPV RT-PCR Kit 1.0: MasterA, MasterB, Internal Control;
Altona RealStar PIV RT-PCR Kit 1.0: MasterA, MasterB, Internal Control;
hMPV A Positive Control, hMPV B Positive Control
PIV-1 Positive Control, PIV-2 Positive Control, PIV-3 Positive Control, PIV-4 Positive
Control
PCR Grade Water
External Control: To be run first week of the month/ or with every new lot; run during training or if
QC failure occurs.
XII.
Procedure:
Prepare samples in the order according to hMetapneumovirus and Parainfluenza viruses (hMPV and
PIV) worksheet. Add the following controls to the Worksheet:
hMPV A Positive control, hMPV B Positive Control, Negative Control (PCR grade Water);
PIV1/3 Positive control, PIV2/4 Positive control, Negative Control(PCR grade Water).
PCR Set-up:
In the Clean Room: (Change into dedicated clean room gown and gloves, work in Biosafety Cabinet)
Remove the required vials of hMPV Master A and Master B (12 reactions/ vial) from the freezer and
thaw them at room temperature
C. To be loaded by epMotion
Prepare hMPV Master Mix in Sarstedt 1.5 mL conical microtube;
Prepare the number of Master Mix reactions required: Number of Test samples + 3 Controls +
extra one
PROCEDURE MANUAL
UNIVERSITY HEALTH NETWORK / MOUNT SINAI HOSPITAL MICROBIOLOGY DEPARTMENT
NOTE: This is a CONTROLLED document. Any documents appearing in paper form that are not stamped in red "MASTER COPY" are not controlled and
should be checked against the document (titled as above) on the server prior to use
D:\106748206.doc
Policy # MI/MD/v50
Microbiology Department
Policy & Procedure Manual
Section: Molecular Diagnostic Tests Manual
Page 148 of
291
Mix gently, do not vortex. Make only enough master mix for the tests you are running. After
Master A has been added to Master B it cannot be frozen again.
Number of Reactions
hMPV Master A
hMPV Master B
Volume of Master Mix
Sample/Control Volume
No. of Test
reactions
1
2
3
4
5
6
7
8
9
10
11
12
1
5
10
15
10
hMPV Master Mix
hMPV Master A (µl)
5
10
15
20
25
30
35
40
45
50
55
60
hMPV Master B (µl)
10
20
30
40
50
60
70
80
90
100
110
120
See Eppendorf epMotion Manual for further loading and programming instructions.
D. To be loaded by manual:
Place 96-well plate onto pre-cooled block
Pipette 15 uL prepared hMPV Master Mix into each reaction well;
Pipette 1.0 uL of internal control into the wells designated for the 3 hMPV Controls (hMPV A
Positive Control, hMPV B Positive Control, Negative PCR Water Control;
Pipette 10 uL PCR Water into the well designated for Negative Control.
In the Specimen Processing Area:
Prepare working P1/P3 and P2/P4 positive controls:
Prepare Working aliquot P1/P3 Positive Control and P2/P4 Positive. Prepare as needed, use
aliquot until finished, and then prepare a new aliquot.
In a 1.5mL conical microtube pipette 180 uL PCR grade water add 20uL PIV-1 Positive
Control and add 20uL PIV-3 Positive Control; label as P1/P3 Positive Control with date.
PROCEDURE MANUAL
UNIVERSITY HEALTH NETWORK / MOUNT SINAI HOSPITAL MICROBIOLOGY DEPARTMENT
NOTE: This is a CONTROLLED document. Any documents appearing in paper form that are not stamped in red "MASTER COPY" are not controlled and
should be checked against the document (titled as above) on the server prior to use
D:\106748206.doc
Policy # MI/MD/v50
Microbiology Department
Policy & Procedure Manual
Section: Molecular Diagnostic Tests Manual
Page 149 of
291
In a 1.5mL conical microtube pipette 180 uL PCR grade water add 20uL PIV-2 Positive Control
and add 20uL PIV-4 Positive Control; label as P2/P4 Positive Control with date.
Working Positive Control PCR Grade Water
PIV Control
180uL
20uL PIV-1 Positive Control
P1/P3 Positive Control
20uL PIV-3 Positive Control
180uL
20uL PIV-2 Positive Control
P2/P4 Positive Control
20uL PIV-4a Positive Control
20uL PIV-4b Positive Control
Pipette 10uL each of Sample/Control into reaction wells. Mix by pipetting 3 times up and down
into the Master Mix.
Seal the plate after pipetting is completed.
Check reaction wells before loading into CFX96 Deep Well Real-Time System: ensure the
liquid levels are at the same height, and there are no bubble at the bottom of each reaction well.
Double click Bio-Rad CFX Manager icon
Startup Wizard window pops up
Make sure CFX96 Deep Well is selected
Under Select run type, click User-defined button
PROCEDURE MANUAL
UNIVERSITY HEALTH NETWORK / MOUNT SINAI HOSPITAL MICROBIOLOGY DEPARTMENT
NOTE: This is a CONTROLLED document. Any documents appearing in paper form that are not stamped in red "MASTER COPY" are not controlled and
should be checked against the document (titled as above) on the server prior to use
D:\106748206.doc
Page 150 of
291
Policy # MI/MD/v50
Microbiology Department
Policy & Procedure Manual
Section: Molecular Diagnostic Tests Manual
Run Set up window pops up, including three tabs-Protocol, Plate, and Start Run
Click Open Lid button
Load sealed plate to the block
Click Close Lid button
WARNING! Do NOT manually close the motorized lid
Under Protocol tab, select Altona PIV RT-PCR.prcl from Express Load pull-down menu
to open the lid
to close the lid
Express
Load pulldown
menu
Open and
Close
Lid
button
Click Plate tab
on the top or click Next button
side to load the plate profile
on the bottom right
PROCEDURE MANUAL
UNIVERSITY HEALTH NETWORK / MOUNT SINAI HOSPITAL MICROBIOLOGY DEPARTMENT
NOTE: This is a CONTROLLED document. Any documents appearing in paper form that are not stamped in red "MASTER COPY" are not controlled and
should be checked against the document (titled as above) on the server prior to use
D:\106748206.doc
Policy # MI/MD/v50
Microbiology Department
Policy & Procedure Manual
Section: Molecular Diagnostic Tests Manual
Select hMPV and PIV.pltd plate profile from the Express Load pull-down menu
Click Start Run tab
bottom right side
on the top or click Next button
Page 151 of
291
on the
PROCEDURE MANUAL
UNIVERSITY HEALTH NETWORK / MOUNT SINAI HOSPITAL MICROBIOLOGY DEPARTMENT
NOTE: This is a CONTROLLED document. Any documents appearing in paper form that are not stamped in red "MASTER COPY" are not controlled and
should be checked against the document (titled as above) on the server prior to use
D:\106748206.doc
Policy # MI/MD/v50
Microbiology Department
Policy & Procedure Manual
Section: Molecular Diagnostic Tests Manual
Confirm the following information:
Protocol: Altona PIV RT-PCR.prcl
Plate: hMPV and PIV.pltd
Scan Mode: All Channels
If any information above needs to be edited, click Prev button
If all information is correct, click Start Run button
Save Optical Data File [CT014845] window pops up
Name and save the file in the designated folder:
Page 152 of
291
T:Microbiology>Virology>Bio Rad CFX96 PCR>Save Run>Respiratory PCR 2015
Click Save button
PROCEDURE MANUAL
UNIVERSITY HEALTH NETWORK / MOUNT SINAI HOSPITAL MICROBIOLOGY DEPARTMENT
NOTE: This is a CONTROLLED document. Any documents appearing in paper form that are not stamped in red "MASTER COPY" are not controlled and
should be checked against the document (titled as above) on the server prior to use
D:\106748206.doc
Policy # MI/MD/v50
Microbiology Department
Policy & Procedure Manual
Section: Molecular Diagnostic Tests Manual
Page 153 of
291
Build Worklist
Open the worklist file according to the following path:
T:Microbiology>Virology>Bio Rad CFX96 PCR>Worklist Mastcopy>Metapara Worklist-excel
Password window pops up, click Read only button
Scan the samples’ information
Row A to Row D are designated for hMeta detection
Row E to Row H are designated for PIV detection
File>Save as
PROCEDURE MANUAL
UNIVERSITY HEALTH NETWORK / MOUNT SINAI HOSPITAL MICROBIOLOGY DEPARTMENT
NOTE: This is a CONTROLLED document. Any documents appearing in paper form that are not stamped in red "MASTER COPY" are not controlled and
should be checked against the document (titled as above) on the server prior to use
D:\106748206.doc
Policy # MI/MD/v50
Microbiology Department
Policy & Procedure Manual
Section: Molecular Diagnostic Tests Manual
Page 154 of
291
Save the worklist at
T:Microbiology>Virology>Bio Rad CFX96 PCR>Import Worklist>Respiratory
Worklist2015
File name: Metapara yyyy.mm.dd.run No. eg. Metapara2015.04.07.1
Save as type: CSV (Comma delimited)
Note:Worklist can only be imported as CSV type
Click Save button
Click OK
The following window pops up, click Yes button
Close current excel file without any savings.
PROCEDURE MANUAL
UNIVERSITY HEALTH NETWORK / MOUNT SINAI HOSPITAL MICROBIOLOGY DEPARTMENT
NOTE: This is a CONTROLLED document. Any documents appearing in paper form that are not stamped in red "MASTER COPY" are not controlled and
should be checked against the document (titled as above) on the server prior to use
D:\106748206.doc
Policy # MI/MD/v50
Microbiology Department
Policy & Procedure Manual
Section: Molecular Diagnostic Tests Manual
Page 155 of
291
Import wordlist
Click Realtime Status tab
Select View/Edit Plate… from Plate Setup pull-down menu
Plate Setup
pull-down
menu
Plate Editor window pops up
PROCEDURE MANUAL
UNIVERSITY HEALTH NETWORK / MOUNT SINAI HOSPITAL MICROBIOLOGY DEPARTMENT
NOTE: This is a CONTROLLED document. Any documents appearing in paper form that are not stamped in red "MASTER COPY" are not controlled and
should be checked against the document (titled as above) on the server prior to use
D:\106748206.doc
Policy # MI/MD/v50
Microbiology Department
Policy & Procedure Manual
Section: Molecular Diagnostic Tests Manual
Click Spreadsheet View/Importer button
Plate Spreadsheet View window pops up
Select HEX from Fluors List pull-down menu
Click Import button
Page 156 of
291
PROCEDURE MANUAL
UNIVERSITY HEALTH NETWORK / MOUNT SINAI HOSPITAL MICROBIOLOGY DEPARTMENT
NOTE: This is a CONTROLLED document. Any documents appearing in paper form that are not stamped in red "MASTER COPY" are not controlled and
should be checked against the document (titled as above) on the server prior to use
D:\106748206.doc
Policy # MI/MD/v50
Microbiology Department
Policy & Procedure Manual
Section: Molecular Diagnostic Tests Manual
Page 157 of
291
Select Import File window pops up
T:Microbiology>Virology>Bio Rad CFX96 PCR>Import Worklist>Respiratory
Worklist2015
Select appropriate worklist and click Open, all samples and controls information are imported
Click OK button
Select all wells by clicking top left side corner
Type IC as target Name for HEX channel
Hit Enter key on the key board
Click Well groups button
PROCEDURE MANUAL
UNIVERSITY HEALTH NETWORK / MOUNT SINAI HOSPITAL MICROBIOLOGY DEPARTMENT
NOTE: This is a CONTROLLED document. Any documents appearing in paper form that are not stamped in red "MASTER COPY" are not controlled and
should be checked against the document (titled as above) on the server prior to use
D:\106748206.doc
Policy # MI/MD/v50
Microbiology Department
Policy & Procedure Manual
Section: Molecular Diagnostic Tests Manual
Click top left
side corner to
select all
wells
Page 158 of
291
Type IC and
hit Enter key
Well Groups Manager window pops up
Click Add button
PROCEDURE MANUAL
UNIVERSITY HEALTH NETWORK / MOUNT SINAI HOSPITAL MICROBIOLOGY DEPARTMENT
NOTE: This is a CONTROLLED document. Any documents appearing in paper form that are not stamped in red "MASTER COPY" are not controlled and
should be checked against the document (titled as above) on the server prior to use
D:\106748206.doc
Policy # MI/MD/v50
Microbiology Department
Policy & Procedure Manual
Section: Molecular Diagnostic Tests Manual
Page 159 of
291
Select wells including control wells for Meta detection (selected wells should be highlight)
Change the name Group 1 to meta
Click Add button
Group 2 shows up
Select wells including control wells for Para detection (selected wells should be highlight)
Change group 2 to para
PROCEDURE MANUAL
UNIVERSITY HEALTH NETWORK / MOUNT SINAI HOSPITAL MICROBIOLOGY DEPARTMENT
NOTE: This is a CONTROLLED document. Any documents appearing in paper form that are not stamped in red "MASTER COPY" are not controlled and
should be checked against the document (titled as above) on the server prior to use
D:\106748206.doc
Policy # MI/MD/v50
Microbiology Department
Policy & Procedure Manual
Section: Molecular Diagnostic Tests Manual
Click OK button
Click Ok button from Plate Editor window
Click Yes button from the popping up window
Page 160 of
291
PROCEDURE MANUAL
UNIVERSITY HEALTH NETWORK / MOUNT SINAI HOSPITAL MICROBIOLOGY DEPARTMENT
NOTE: This is a CONTROLLED document. Any documents appearing in paper form that are not stamped in red "MASTER COPY" are not controlled and
should be checked against the document (titled as above) on the server prior to use
D:\106748206.doc
Policy # MI/MD/v50
Microbiology Department
Policy & Procedure Manual
Section: Molecular Diagnostic Tests Manual
Click Time Status tab
Page 161 of
291
from the Run Details window
PROCEDURE MANUAL
UNIVERSITY HEALTH NETWORK / MOUNT SINAI HOSPITAL MICROBIOLOGY DEPARTMENT
NOTE: This is a CONTROLLED document. Any documents appearing in paper form that are not stamped in red "MASTER COPY" are not controlled and
should be checked against the document (titled as above) on the server prior to use
D:\106748206.doc
Policy # MI/MD/v50
Microbiology Department
Policy & Procedure Manual
Section: Molecular Diagnostic Tests Manual
Page 162 of
291
Analyze results after the PCR is completed
Export and Print Hmpv result
Choose meta from Well Groups pull-down menu
Change the channel names from Fluorophore to Target
Set the threshold line for each target channel
Click Export
PROCEDURE MANUAL
UNIVERSITY HEALTH NETWORK / MOUNT SINAI HOSPITAL MICROBIOLOGY DEPARTMENT
NOTE: This is a CONTROLLED document. Any documents appearing in paper form that are not stamped in red "MASTER COPY" are not controlled and
should be checked against the document (titled as above) on the server prior to use
D:\106748206.doc
Policy # MI/MD/v50
Microbiology Department
Policy & Procedure Manual
Section: Molecular Diagnostic Tests Manual
Select Custom Export…
Click Export button
Save as Window pops up
Change the File name according to the target and save in the following folder:
Page 163 of
291
T:\Microbiology\Virology\Bio Rad CFX96 PCR\Exported Excel Results
Click Save button
PROCEDURE MANUAL
UNIVERSITY HEALTH NETWORK / MOUNT SINAI HOSPITAL MICROBIOLOGY DEPARTMENT
NOTE: This is a CONTROLLED document. Any documents appearing in paper form that are not stamped in red "MASTER COPY" are not controlled and
should be checked against the document (titled as above) on the server prior to use
D:\106748206.doc
Policy # MI/MD/v50
Microbiology Department
Policy & Procedure Manual
Section: Molecular Diagnostic Tests Manual
Once Export completed, Click OK button
The final results with Ct values are exported in Excel sheet
Print the excel sheet and attach it to the hMPV worksheet
Close excel
Page 164 of
291
Export and Print PIV result
Choose para from Well Groups pull-down menu
Change the channel names from Fluorophore to Target
Set the threshold line for each target channel
Click Export
Save as Window pops up
Change the File name according to the target and save in the following folder:
T:\Microbiology\Virology\Bio Rad CFX96 PCR\Exported Excel Results
Click OK button
PROCEDURE MANUAL
UNIVERSITY HEALTH NETWORK / MOUNT SINAI HOSPITAL MICROBIOLOGY DEPARTMENT
NOTE: This is a CONTROLLED document. Any documents appearing in paper form that are not stamped in red "MASTER COPY" are not controlled and
should be checked against the document (titled as above) on the server prior to use
D:\106748206.doc
Policy # MI/MD/v50
Microbiology Department
Policy & Procedure Manual
Section: Molecular Diagnostic Tests Manual
Click Close button
Print the excel sheet and attach it to the hMPV worksheet
Close excel
Close CFX96 Deep Well Real-Time Systim
Shut down computer
Page 165 of
291
End of Shift Cleaning:.
Clean Room: Wipe down with RNAse Away or NucleoClean on paper towel, followed by distilled
water, and then 70% alcohol
Biological Safety Cabinet
Pipettes
Bench tops
Specimen Preparation Area: Wipe down with Working 1% hypochloride (made daily), followed by
distilled water, and then 70% alcohol
Biological Safety Cabinet (BSC), pipettes, centrifuge, and bench top.
Seal and discard BSC waste
Wash racks.
EasyMAG , Lysis Rack, and BioHit Multi-channel Pipette: Wipe down surfaces with RNAse Away
or NucleoClean on KimWipe, followed by UltraPure water, and then 70% alcohol Wipe
Amplification Area: Wipe down surfaces with RNAse Away or NucleoClean on KimWipe, followed
by UltraPure water, and then 70% alcohol Wipe
Seal & discard reaction microtubes into biohazard waste after each run.
Perform the cleaning procedure according the daily maintenance sheet.
PROCEDURE MANUAL
UNIVERSITY HEALTH NETWORK / MOUNT SINAI HOSPITAL MICROBIOLOGY DEPARTMENT
NOTE: This is a CONTROLLED document. Any documents appearing in paper form that are not stamped in red "MASTER COPY" are not controlled and
should be checked against the document (titled as above) on the server prior to use
D:\106748206.doc
Policy # MI/MD/v50
Microbiology Department
Policy & Procedure Manual
Section: Molecular Diagnostic Tests Manual
Page 166 of
291
XIII. hMPV Interpretation and Reporting:
Cy5
Channel
hMPV A
HEX Channel
(IC specific)
Interpretations
+
-
+/-
hMPV B DETECTED
-
+
+/-
hMPV A DETECTED
FAM
Channel
hMPV B
+
+
+/-
hMPV B DETECTED.
hMPV A DETECTED.
(ask charge/senior for confirmation)
-
-
+
hMPV NOT DETECTED
-
INVALID
Respiratory sample needs to be diluted 1:4 with
VTM and re-extracted and RT-PCR repeated.
-
-
VTM=Viral Transport Media
hMPV B DETECTED or hMPV A DETECTED
Report as an isolate in the (F7) Isolate Window.
Date the media on the back of the LIS workcard PCMET: F6 to add the date tested.
In the media PCMET enter crosspoint (ct) value : ct=
Report the virus as an isolate in the F7 window.
Isolate #: 1, or next available isolate number.
Org. ID: 25mpvA
Metapneumovirus A DETECTED
25mpvB
Metapneumovirus B DETECTED
The reporting isolate comment is attached to the Organism ID.
Verify All in the isolate window.
Review report entry: media, and isolates.
Finalize the report.
Call all positives to ward/doctor and Infection Control Practitioner (ICP). Document calls and emails
in the media CALL.
PROCEDURE MANUAL
UNIVERSITY HEALTH NETWORK / MOUNT SINAI HOSPITAL MICROBIOLOGY DEPARTMENT
NOTE: This is a CONTROLLED document. Any documents appearing in paper form that are not stamped in red "MASTER COPY" are not controlled and
should be checked against the document (titled as above) on the server prior to use
D:\106748206.doc
Policy # MI/MD/v50
Microbiology Department
Policy & Procedure Manual
Section: Molecular Diagnostic Tests Manual
Page 167 of
291
hMPV NOT DETECTED
Date the media on the back of the workcard. PCMET: F6 to add run date.
On the front of the workcard, select from the keypad: }MET}MET-
Negative for metapneumovirus
by RealStar hMPV RT-PCR, Altona Diagnostics.
Review report entry.
Finalize the report.
hMPV INDETERMINATE
Internal control has failed twice to amplify in a sample.
Date the media on the back of the LIS workcard. PCMET: F6 to add run date.
Select from the keypad “Failed single”, type “IC no amplification”, select >FAIL
Select from keypad ^PRMET
Under this media ^PRMET report the 1:4 dilution test result type “IC no amplification”.
Report: select from the keypad: }METChange “Negative” to INDETERMINATE; final report should appear as:
INDETERMINATE for metapneumovirus
by RealStar hMPV RT-PCR, Altona Diagnostics.
Review report entry.
Finalize the report.
PROCEDURE MANUAL
UNIVERSITY HEALTH NETWORK / MOUNT SINAI HOSPITAL MICROBIOLOGY DEPARTMENT
NOTE: This is a CONTROLLED document. Any documents appearing in paper form that are not stamped in red "MASTER COPY" are not controlled and
should be checked against the document (titled as above) on the server prior to use
D:\106748206.doc
Policy # MI/MD/v50
Microbiology Department
Policy & Procedure Manual
Section: Molecular Diagnostic Tests Manual
Page 168 of
291
XIV. PIV Interpretation and Reporting:
FAM
Channel
PIV1/3
Cy5
Channel
PIV2/4
HEX Channel
(IC specific)
Interpretations
+
-
+/-
PIV-1/3 DETECTED
-
+
+/-
PIV-2/4 DETECTED
+
+
+/-
PIV-1/3 DETECTED.
PIV-2/4 DETECTED.
(ask charge/senior for confirmation)
-
-
+
PIV NOT DETECTED
-
INVALID
Respiratory sample needs to be diluted 1:4
with VTM and re-extracted and RT-PCR
repeated.
-
-
VTM=Viral Transport Media
PIV-1/3 DETECTED. or PIV-2/4 DETECTED
Report as an isolate in the (F7) Isolate Window.
Date the media on the back of the LIS workcard PCPIN: F6 to add the date tested.
In the media PCPIN enter crosspoint (ct) value : ct=
Report the virus as an isolate in the F7 window.
Isolate #: 1, or next available isolate number.
Org. ID: 24par13
Parainfluenza virus 1 and/or 3
24par24
Parainfluenza virus 2 and/or 4
The reporting isolate comment is attached to the Organism ID.
Verify All in the isolate window.
Review report entry: media, isolate.
Finalize the report.
Call all positives to ward/doctor and Infection Control Practitioner (ICP). Document calls and emails
in the media CALL.
PROCEDURE MANUAL
UNIVERSITY HEALTH NETWORK / MOUNT SINAI HOSPITAL MICROBIOLOGY DEPARTMENT
NOTE: This is a CONTROLLED document. Any documents appearing in paper form that are not stamped in red "MASTER COPY" are not controlled and
should be checked against the document (titled as above) on the server prior to use
D:\106748206.doc
Policy # MI/MD/v50
Microbiology Department
Policy & Procedure Manual
Section: Molecular Diagnostic Tests Manual
Page 169 of
291
PIV-1/3 NOT DETECTED. or PIV-2/4 NOT DETECTED
Date the media on the back of the workcard. PCPIN: F6 to add run date.
On the front of the workcard, select from the keypad: }PI}PI-
Negative for parainfluenza virus by RealStar
PIV RT-PCR, Altona Diagnostics.
Review report entry.
Finalize the report.
PIV INDETERMINATE
Internal control has failed twice to amplify in a sample.
Date the media on the back of the LIS workcard. PCPIN: F6 to add run date.
Select from the keypad “Failed single”, type “IC no amplification”, select >FAIL
Select from keypad ^PRPIN
Under this media ^PRPIN report the 1:4 dilution test result type “IC no amplification”.
Report: select from the keypad: }PIChange “Negative” to INDETERMINATE; final report should appear as:
INDETERMINATE for parainfluenza virus by RealStar
PIV RT-PCR, Altona Diagnostics.
Review report entry.
Finalize the report.
XV.
Quality Control
Reagent QCs:
An External Control (external to altona Diagnostics) is used to monitor the isolation,
amplification and detection procedures. The result must correspond to expected value supplied
by the manufacturer.
External control for hMPV A, hMPV B, PIV1/3, and PIV 2/4 should be extracted on the on the
easyMag and run once a month and/or with each new lot.
Daily QCs: Every Run
Each patient specimen must have an Internal Control (IC) added to monitor both isolation and
PCR inhibition.
A Positive Control is included and shows a positive reading in FAM channels (hMPV B and PIV
1/3) Channel or a positive reading in Cy5 Channels ( hMPV A and PIV 2/4)
A Negative Control is include and shows a negative reading in both FAM channels (hMPV B
and PIV 1/3) Channel and Cy5 Channels ( hMPV A and PIV 2/4)
Report all failed QCs to senior/charge technologist.
PROCEDURE MANUAL
UNIVERSITY HEALTH NETWORK / MOUNT SINAI HOSPITAL MICROBIOLOGY DEPARTMENT
NOTE: This is a CONTROLLED document. Any documents appearing in paper form that are not stamped in red "MASTER COPY" are not controlled and
should be checked against the document (titled as above) on the server prior to use
D:\106748206.doc
Policy # MI/MD/v50
Microbiology Department
Policy & Procedure Manual
Section: Molecular Diagnostic Tests Manual
a.
b.
c.
d.
e.
f.
g.
h.
i.
j.
Page 170 of
291
Failed QC:
Test is invalid without satisfactory QC results.
Do not release results pending resolution of QC failure.
Inform charge/senior technologist.
Record in Reagent Log Chart, Instrument Maintenance Log or Incident Report where
appropriate.
If the QC failure was due to a simple matter of position reversal or misplacement, the run can be
released (positive QC material yielded positive result, negative yielded negative result).
If positive QC material yielded negative result, repeat the entire run.
If negative QC material yielded positive result, it may be due to cross-contamination from
adjacent positive sample within the run or carry-over contamination from previous runs via
equipment or the environment. Review procedure and equipment to establish and eliminate
potential sources of contamination.
The extent and nature of contamination can also be evaluated by comparing the positive rate of
the run with its expected positive rate.
If the contamination is extensive, it is necessary to quarantine/discard potentially contaminated
reagents and consumables and disinfect equipment and environment before repeating the run.
If a carry-over contamination is suspected (e.g. two or more runs with negative QC being
positive or patient samples have higher than expected positive rate and these samples are often
non-repeatable positives), it is necessary to have a thorough environmental disinfection followed
by swabbing to monitor.
Successful ending to a carry-over contamination may be indicated by QC results and patient
positivity rate falling back to the expected normal range and three negative environmental swabs.
XVI. References:
RealStar hMPV RT-PCR Kit v1.0, altona Diagnostics
RealStar PIV RT-PCR Kit v1.0, altona Diagnostics
cdc.gov/Human Parainfluenza Viruses (HPIVs) (/parainfluenza/index.html
Emerging Infectious Disease Journal Volume 14, Number1-January 2008
PROCEDURE MANUAL
UNIVERSITY HEALTH NETWORK / MOUNT SINAI HOSPITAL MICROBIOLOGY DEPARTMENT
NOTE: This is a CONTROLLED document. Any documents appearing in paper form that are not stamped in red "MASTER COPY" are not controlled and
should be checked against the document (titled as above) on the server prior to use
D:\106748206.doc
Policy # MI/MD/v50
Microbiology Department
Policy & Procedure Manual
Section: Molecular Diagnostic Tests Manual
Page 171 of
291
Human Papilloma Virus (HPV) PCR by Cobas® 4800
I. Introduction
The cobas® 4800 HPV Test is for the qualitative in vitro detection of Human Paillomavirus in patients
specimens using PCR. There are 118 types of HPV, and approximately 40 different HPVs that can infect
the human anogenital mucosa. The cobas® 4800 HPV test specifically identifies types HPV 16 and
HPV 18, and also detects high risk types (31, 33, 39, 45, 51, 52, 56, 58, 59, 66, and 68).
HPV is a small, non-enveloped, double stranded DNA virus with a genome of approximately 8000
nucleotides. The presence of HPV has been found in 99% of cervical cancers, with types 13 to 18 is
considered high-risk for the development of cervical cancer, and its precursor lesions.
II. Specimen Collection/Transport/Storage
Cervical specimens collected in primary container: PreservCyt Solution, cobas® PCR Cell Collection
Media, and SurePath Preservative Fluid. Minimum volume in primary container should be 3.0 mL.
Primary containers for PreservCyt Solution, and cobas® PCR Cell Collection Media should be vortex
prior to loading on the cobas® x480.
Cervical specimens in PreservCyt Solution, cobas® PCR Cell Collection Media, and SurePath
Preservative Fluid can be transported at 2-30°C. Cervical specimens collected in SurePath Preservative
Fluid should be refrigerated 24 hour after collection.
Cervical specimens collected in PreservCyt Solution, cobas® PCR Cell Collection Media, may be stored
at 2-30°C for up to 6 months after collection date. Cervical samples collected in SurePath Preservative
Fluid may be stored at 2-8°C for up to 4 weeks after collection.
III. Reagents and Materials
a) cobas® 4800 System Liquid Cytology Preparation Kit – 240 tests (stored at 2-8°C)
PK- Proteinase K
SDS- 4800 System SDS Reagent
LYS- 4800 Lysis Buffer
b) cobas® 4800 System Sample Preparation Kit – 240 test (stored at 2-8°C)
MGP-Magnetic glass particles
EB-Elution buffer
c) cobas® 4800 System Wash Buffer Kit – 240 test kits (stored at 15-25°C)
WB-Wash Buffer
d) cobas® 4800 HPV Amplification/Detection Kit – 240 test (stored in Clean Room at 2-8°C)
HPV MMX-Master Mix
HPV Mg/Mn-Magnesium/Magnesium
e) cobas® 4800 HPV Controls Kit (stored at 2-8°C)
HPV (+) C - Positive Control
PROCEDURE MANUAL
UNIVERSITY HEALTH NETWORK / MOUNT SINAI HOSPITAL MICROBIOLOGY DEPARTMENT
NOTE: This is a CONTROLLED document. Any documents appearing in paper form that are not stamped in red "MASTER COPY" are not controlled and
should be checked against the document (titled as above) on the server prior to use
D:\106748206.doc
Policy # MI/MD/v50
Microbiology Department
Policy & Procedure Manual
Section: Molecular Diagnostic Tests Manual
f)
g)
h)
i)
j)
k)
l)
Page 172 of
291
HPV (-) C - Negative Control
Reagent Reservoirs – 50mL and 200 mL containers
cobas® 4800 System Extraction (deep well) Plate
cobas® 4800 AD (microwell) Plate
CO-RE pipette tips (1000 uL) rack of 96
Plate carrier
Tip carrier
Sample and reagent racks
IV. Instrumentation and Software
cobas® x 480 Instrument
cobas® z 480 Analyzer
Heater/Shaker Unit
cobas® 4800 System Control Unit
V. Procedure
NOTE: All reagents must be at except HPV Amplification/Detection Kit should be at room
temperature before loading on the cobas® x480. HPV MMX and HPV Mg/Mn can be loaded
directly on cobas® x480 from 2-8°C.
Specimens in PreservCyt Solution, cobas® PCR Cell Collection Media, and SurePath Preservative
Fluid must be at room temperature before loading on the cobas® x480.
1. Turn on the system as the following sequence:
1. cobas® z 480 2. Heater/Shaker unit 3. cobas® x 480 instrument
2. When the left orange light on the cobas® z 480 turns to solid green, turn on the computer
workstation.
3. Remove one set of reagents from cobas® 4800 System Liquid Cytology Preparation Kit, one set of
reagents from cobas® System Sample Preparation Kit from fridge, and allow reagents to come to
room temperature
4. Logon to the cobas 4800 software
User ID: LABOPERATOR
Password: 00labOPR
5. Perform instrument maintenance: follow the online window dialogue boxes
1) Select Overview tab and check maintenance status of the cobas x 480 instrument.
If weekly maintenance is due, click Run Weekly Maintenance.
If daily maintenance is due, click Run Daily Maintenance.
2) Follow the online instructions.
6. Start New Run
a. After the completion of the maintenance, in the overview tab, select New Run icon.
PROCEDURE MANUAL
UNIVERSITY HEALTH NETWORK / MOUNT SINAI HOSPITAL MICROBIOLOGY DEPARTMENT
NOTE: This is a CONTROLLED document. Any documents appearing in paper form that are not stamped in red "MASTER COPY" are not controlled and
should be checked against the document (titled as above) on the server prior to use
D:\106748206.doc
Policy # MI/MD/v50
Microbiology Department
Policy & Procedure Manual
Section: Molecular Diagnostic Tests Manual
Page 173 of
291
on the right hand vertical bar
b.
The following window pops up. Select test type: HPV workflow.
c. Type run name ie: HPV 2012.05.29-1
d. Click OK.
7. Refer to the following figure while you are loading the deck:
E-plate
Holder
Tip Rack
Holder
Dynamic Loading
AD-plate
Holder
Plate Carrier
Track 1-6
Tip Rack
Holder
Tip Rack Carrier
Track 11-16
Sample Loading Area
Track 17-34
Tip Rack Carrier
Track 35-40
Reservoirs Reagent
Track
Track
48-50
51
8. Load samples
Vortex the primary PreservCyt Solution samples prior to loading on the cobas® x480.
PROCEDURE MANUAL
UNIVERSITY HEALTH NETWORK / MOUNT SINAI HOSPITAL MICROBIOLOGY DEPARTMENT
NOTE: This is a CONTROLLED document. Any documents appearing in paper form that are not stamped in red "MASTER COPY" are not controlled and
should be checked against the document (titled as above) on the server prior to use
D:\106748206.doc
Policy # MI/MD/v50
Microbiology Department
Policy & Procedure Manual
Section: Molecular Diagnostic Tests Manual
Page 174 of
291
Un-cap samples.
Place samples on corresponding carrier.
Insert sample carriers on autoload tray when the LEDs for the designated track(17-34) are flashing.
Select Load Samples
9.
Load consumables
Place listed consumables on appropriate carriers.
Both tip carriers are fully filled and barcodes facing the right hand side
Ensure deepwell plate is loaded flatly and properly –barcode facing the right hand side
Ensure microwell plate is loaded flat and properly (barcode facing away from you)
Insert carriers on autoload tray.
Select Load Consumables.
PROCEDURE MANUAL
UNIVERSITY HEALTH NETWORK / MOUNT SINAI HOSPITAL MICROBIOLOGY DEPARTMENT
NOTE: This is a CONTROLLED document. Any documents appearing in paper form that are not stamped in red "MASTER COPY" are not controlled and
should be checked against the document (titled as above) on the server prior to use
D:\106748206.doc
Policy # MI/MD/v50
Microbiology Department
Policy & Procedure Manual
Section: Molecular Diagnostic Tests Manual
Page 175 of
291
10. Load reagents
200 mL reagent reservoir carrier
Load Wash Buffer (WB) on 200 mL reagent reservoir carrier as indicated in the wizard
(scan-scan-pour).
Insert carrier on autoload tray.
Click Load Reagents.
Note: Once the Wash Buffer is scanned you have one hour to complete the loading process and
Press Start button.
50 mL reagent reservoir carrier
Load reagents on 50 mL reagent reservoir carrier as indicated in the wizard.(scan-scan-pour).
Elution Buffer (EB), SDS Reagent (SDS), Lysis Buffer (LYS)
vortex MGP for 10s prior to scanning and loading
Insert carrier on autoload tray.
Click Load Reagents.
Reagent carrier
Take out HPV MMX and HPV Mg/Mn from the clean room
Open reagent vials and load them on reagent carrier as indicated in the wizard.
Change gloves after uncapping positive control
Insert carrier on autoload tray.
Click Load Reagents.
PROCEDURE MANUAL
UNIVERSITY HEALTH NETWORK / MOUNT SINAI HOSPITAL MICROBIOLOGY DEPARTMENT
NOTE: This is a CONTROLLED document. Any documents appearing in paper form that are not stamped in red "MASTER COPY" are not controlled and
should be checked against the document (titled as above) on the server prior to use
D:\106748206.doc
Policy # MI/MD/v50
Microbiology Department
Policy & Procedure Manual
Section: Molecular Diagnostic Tests Manual
11.
Page 176 of
291
Start sample preparation run
Select Start Run.
The sample preparation starts.
Check the timer in the wizard; timer should count down.
12.
Unload AD (microwell) Plate. Seal AD plate.
Select Sample Prep Results to review the results of the sample preparation.
Select Unload.
PROCEDURE MANUAL
UNIVERSITY HEALTH NETWORK / MOUNT SINAI HOSPITAL MICROBIOLOGY DEPARTMENT
NOTE: This is a CONTROLLED document. Any documents appearing in paper form that are not stamped in red "MASTER COPY" are not controlled and
should be checked against the document (titled as above) on the server prior to use
D:\106748206.doc
Policy # MI/MD/v50
Microbiology Department
Policy & Procedure Manual
Section: Molecular Diagnostic Tests Manual
Page 177 of
291
Seal AD (microwell) plate with Sealing Film and applicator as indicated on screen.
Be sure not to touch the seal with your fingers as it may affect detection. Hold the sides of the
plate and use the smoothing applicator provided to properly seal.
The plate must be transferred from the cobas x 480 to the cobas z 480 within 90 minutes of
completion
Select NEXT
13.
Load mirowell plate on cobas® z 480 analyzer.
Press load button on the cobas z 480 analyzer.
Place the sealed AD (microwell) plate into the extended loader.
Select load button again.
The amplification and detection run starts automatically.
Check the timer in the wizard; timer should be counting down.
14.
Remove used reagents, reservoirs, samples, and deepwell plate from the cobas x 480 instrument.
Discard waste appropriately, used reagents should be disposed of properly.
(Some reagents may contain Guanidine HCl and should be disposed of properly.) PCR waste should
put in sealed waste bags into the biohazard boxes.
PROCEDURE MANUAL
UNIVERSITY HEALTH NETWORK / MOUNT SINAI HOSPITAL MICROBIOLOGY DEPARTMENT
NOTE: This is a CONTROLLED document. Any documents appearing in paper form that are not stamped in red "MASTER COPY" are not controlled and
should be checked against the document (titled as above) on the server prior to use
D:\106748206.doc
Policy # MI/MD/v50
Microbiology Department
Policy & Procedure Manual
Section: Molecular Diagnostic Tests Manual
15.
Page 178 of
291
Detection is completed in the cobas® z 480. Run is finished.
Select Show Results.
Review and accept results in Results.
●DO NOT ACCEPT FAILED or INVALID results●
Select results and select printer icon ; to print the results report.
Select results to Export.
16.
Unload the AD (microwell) plate from the cobas® z 480. Discard the AD plate in a sealed waste
bag into the biohazard box.
Log-off and Exit from the cobas® 4800 program. Shutdown the PC. Switch-off the cobas® z 480,
switch-off the cobas® x 480, and switch-off the heater.
VI.
Interpretation of Results
All assay and run validation is determined by the Cobas® 4800 software. Controls must be run with
each sample run and valid results must be obtained for both the positive and negative control in
order for sample results to be displayed.
PROCEDURE MANUAL
UNIVERSITY HEALTH NETWORK / MOUNT SINAI HOSPITAL MICROBIOLOGY DEPARTMENT
NOTE: This is a CONTROLLED document. Any documents appearing in paper form that are not stamped in red "MASTER COPY" are not controlled and
should be checked against the document (titled as above) on the server prior to use
D:\106748206.doc
Policy # MI/MD/v50
Microbiology Department
Policy & Procedure Manual
Section: Molecular Diagnostic Tests Manual
VII.
Page 179 of
291
Result Reporting and Interpretation
Cobas® 4800 HPV Test
Interpretation
Other HR HPV NEG, HPV16 NEG,
HPV18 NEG
Specimen is negative for Other High Risk HPV, Negative for HPV16,
Negative for HPV18
Other HR HPV POS, HPV16 NEG,
HPV18 NEG
Specimen is POSITIVE for Other High Risk HPV, Negative for
HPV16, Negative for HPV18
Other HR HPV POS, HPV16 POS,
HPV18 NEG
Specimen is Negative for Other High Risk HPV, POSITIVE for
HPV16, Negative for HPV18
Other HR HPV NEG, HPV16 NEG,
HPV18 POS
Specimen is Negative for Other High Risk HPV, Negative for HPV16,
POSITIVE for HPV18
INVALID or FAILED
SAMPLE RESULTS
NO NOT ACCEPT the results in the results field. These results should
not be exported. Review Details.
Refer to trouble shooting guidelines.
Trouble Shooting
INVALID
X3:
Error Clot Detected
Re-test the original specimen.
Vortex 30s to break-up excessive mucous. Re-test.
X4:
Check for excessive mucous. Vortex 30s to break-up
Error Processing of the sample was aborted excessive mucous. Re-test.
due to one or more pipetting error(s)
PROCEDURE MANUAL
UNIVERSITY HEALTH NETWORK / MOUNT SINAI HOSPITAL MICROBIOLOGY DEPARTMENT
NOTE: This is a CONTROLLED document. Any documents appearing in paper form that are not stamped in red "MASTER COPY" are not controlled and
should be checked against the document (titled as above) on the server prior to use
D:\106748206.doc
Policy # MI/MD/v50
Microbiology Department
Policy & Procedure Manual
Section: Molecular Diagnostic Tests Manual
VIII.
Page 180 of
291
Quality Control
Each HPV run includes a set of HPV Positive and Negative Controls. The HPV controls must be
valid, before specimens results are displayed, in the cobas 4800 HPV result field.
Each sample has an internal control, ß-globin, to monitor cell adequacy, extraction and amplification;
internal control must be valid for specimen test to be valid.
CAP provides external proficiency testing.
All invalid failed runs should be brought to the attention of Charge/seniors for trouble shooting, and
resolution.
IX.
Reference
cobas® 4800 HPV Test 2010, Roche Molecular Systems, Inc.
PROCEDURE MANUAL
UNIVERSITY HEALTH NETWORK / MOUNT SINAI HOSPITAL MICROBIOLOGY DEPARTMENT
NOTE: This is a CONTROLLED document. Any documents appearing in paper form that are not stamped in red "MASTER COPY" are not controlled and
should be checked against the document (titled as above) on the server prior to use
D:\106748206.doc
Policy # MI/MD/v50
Microbiology Department
Policy & Procedure Manual
Section: Molecular Diagnostic Tests Manual
Page 181 of
291
Influenza A/B & RSV PCR by Focus Diagnostics Simplexa™
I.
Introduction
The Simplexa™ Flu A/B & RSV Direct assay system is a real-time RT-PCR system that
enables the direct amplification, detection and differentiation of human influenza A virus
RNA, human influenza B virus RNA and respiratory syncytial virus (RSV) RNA from
unprocessed nasopharyngeal swabs (NPS) that have not undergone an extraction process.
The system consists of the Simplexa™ Flu A/B & RSV Direct assay, the 3M Integrated
Cycler (with Integrated Cycler Studio Software), the Direct Amplification Disc and
associated accessories
In the Simplexa™ Flu A/B & RSV Direct assay, bi-functional fluorescent probe-primers
are used together with corresponding reverse primers to amplify Flu A, Flu B, RSV and
internal control RNA. The assay provides three results; conserved regions of influenza A
viruses (matrix gene), influenza B viruses (matrix gene) and RSV (M gene) are targeted
to identify these viruses in the specimen. An RNA internal control is used to detect RTPCR failure and/or inhibition.
II.
Specimen Collection and Transport
Nasopharyngeal swabs collected in Viral Transport Media (VTM) are stored at 4oC. Vortex
swabs on high for 10 seconds, aliquot the VTM into freezer vials and store at 4oC.
If BAL specimens are mucoid, treat with working sputolysin. Remove red blood cells and large
particulate matter by micro-centrifuging sample for 5 minutes at 3000 rpm in the Eppendorf
5415 C Micro-centrifuge. Aliquot supernatant and store at 4oC.
III.
Materials and Equipments
3M Integrated Cycler (with Integrated Cycler Studio Software v4.1 or higher)
Simplexa™ Flu A/B & RSV Direct assay (MOL2650) 24 tests
i) Direct Amplification Discs-24 tests stored at room temperature
ii) Simplexa ™ Flu A/B & RSV Reaction Mix (RM) – 24 tests stored in Clean Room
freezer (-10 to -30°C) Yse within 30 minutes after thawing
Variable volume Ranin Pipitte: 10 to 200 uL
Aerosol Resistant Tips (ART)
Powder free gloves
Biological Safety Cabinet
PROCEDURE MANUAL
UNIVERSITY HEALTH NETWORK / MOUNT SINAI HOSPITAL MICROBIOLOGY DEPARTMENT
NOTE: This is a CONTROLLED document. Any documents appearing in paper form that are not stamped in red "MASTER COPY" are not controlled and
should be checked against the document (titled as above) on the server prior to use
D:\106748206.doc
Policy # MI/MD/v50
Microbiology Department
Policy & Procedure Manual
Section: Molecular Diagnostic Tests Manual
IV.
Page 182 of
291
Procedure:
NOTE: Do not wear gloves when using the computer and Cycler.
Perform daily maintenance. Slightly dampen KimWipe with 70% alcohol, wipe external surfaces
of the 3M Cyclers, and laptop keyboards. Wipe benchtop with 70% alcohol.
Cautionary notes: Avoid creating aerosols. Use only ART tips. Change gloves frequently. Dispose
of waste properly, in sealed discard bags. Do not open foil wedges or pierce foil of post amplified
tests. Avoid cross contamination.
1. Switch ON 3M Cycler -first
Then switch on lap top computer –second.
Windows… User name: MSH
Password: MSH12345
Enter
2. Select and open: Integrated Cycler Studio Icon on desktop.
User name: MSH
Password: MSH12345
LogOn
3. In the Clean Room freezer remove Simplexa™ Flu A/B & RSV Reacion Mix (RM) vials.
Please check lot numbers; ensure you are using the current “in use Reagent lot”. Only one
Reagent Mix (RM) Lot can be used in specimen testing batch. DO NOT MIX LOTS.
One Reagent Mix (RM) is required for every specimen. Thaw thoroughly before use, 3 minutes.
DO NOT VORTEX. Spin down reagent mix.
Reagent Mix must be used within 30 minutes.
4. New Reagent Lot ONLY.
Menu bar at the top Select: Tools
Select: Scan Assay Barcode
Dialogue window appears: Please scan the Assay barcode(s) now.
Scan the Simplexa Reagent Lot card (provided with each kit), the square barcode. See diagram
below.
Dialogue window appears: “Import assay parameters… Select: OK
PROCEDURE MANUAL
UNIVERSITY HEALTH NETWORK / MOUNT SINAI HOSPITAL MICROBIOLOGY DEPARTMENT
NOTE: This is a CONTROLLED document. Any documents appearing in paper form that are not stamped in red "MASTER COPY" are not controlled and
should be checked against the document (titled as above) on the server prior to use
D:\106748206.doc
Policy # MI/MD/v50
Microbiology Department
Policy & Procedure Manual
Section: Molecular Diagnostic Tests Manual
Page 183 of
291
<<<Scan Large Data Barcode for NEW
Reagent lots Only.
5. Remove Direct Amplification Disc (8 tests per disc) from the foil package.
Note: Partially used discs are remembered in the machine they were first run on. Ensure
the right disc is used and the available spaces on the disc corresponds to what is shown in
the computer
6. Load specimens in Specimen processing area Biological Safety Cabinet.
Load one test at a time. Opening one foil wedge at a time.
Lift the foil from the wedge to be loaded. DO NOT CREATE AEROSOLS.
Pipette 50 uL of the Reagent Mix (RM) into the well marked R.
Pipette 50 uL of the specimen into the well marked SAMPLE.
Re-seal the wedge with foil firmly and tear off the perforated tab edge.
Open the lid of the 3M Cycler with glove-free hand, load the Amplification Disc into 3M Cycler.
Close the lid.
NOTE: Different Reagent Mix (RM) lots cannot be mixed on a disc.
Only one Reagent Mix (RM) Lot can be used with each specimen testing batch on
a disc.
PROCEDURE MANUAL
UNIVERSITY HEALTH NETWORK / MOUNT SINAI HOSPITAL MICROBIOLOGY DEPARTMENT
NOTE: This is a CONTROLLED document. Any documents appearing in paper form that are not stamped in red "MASTER COPY" are not controlled and
should be checked against the document (titled as above) on the server prior to use
D:\106748206.doc
Policy # MI/MD/v50
Microbiology Department
Policy & Procedure Manual
Section: Molecular Diagnostic Tests Manual
Page 184 of
291
7. Left-hand toolbar Configure Runs.
Select: Simplexa FluA_B & RSV Direct 5.
Running window appears. A run is automatically generated under Run name, add your initials to
the end of the run file; example: Run 11-11-2012 At 0900 lws. This will identify you as operator.
8. In Reagent Lot:
Scan reagent barcode on Reagent Mix RM) Vial used to load your batch of samples.
If your reagent lot is new, the program will prompt you and require you to scan the data bar
code. See New Reagent Lot (above).
NOTE: Different Reagent Mix (RM) lots cannot be mixed on a disc. Only one Reagent Mix
(RM) Lot can be used with each specimen testing batch on a disc.
In Disc ID:
Scan the barcode, located on the side of the Direct Amplication Disc.
9. Under Sample ID: Scan the sample(s) barecodes(s).
Ensure specimens are loaded in the correct wedge identified.
Create VRESP Worklist
Select: Save
10. Select: Run.
Select Run. Run time is 64 minutes. Run status window allows you to monitor the whole run.
11. Run complete. Select Print. Print report window appears Select: include CT values and print
with graph.
12. If Direct Amplification disc can still be used; test wedges still available, leave on 3M Cycler. If
the Direct Amplification disc is finished, no test wedges available, seal the used disc in a bag,
and discard into biohazard waste.
13. Shutdown lap top computer –first. Then Switch-off the 3M Cycler.
PROCEDURE MANUAL
UNIVERSITY HEALTH NETWORK / MOUNT SINAI HOSPITAL MICROBIOLOGY DEPARTMENT
NOTE: This is a CONTROLLED document. Any documents appearing in paper form that are not stamped in red "MASTER COPY" are not controlled and
should be checked against the document (titled as above) on the server prior to use
D:\106748206.doc
Page 185 of
291
Policy # MI/MD/v50
Microbiology Department
Policy & Procedure Manual
Section: Molecular Diagnostic Tests Manual
V.
Interpretation of Results
Upon completion of the run, the software automatically interprets and displays results.
For each Specimen entered, software displays a result (“Detected”, “Not Detected” or “Invalid”) for Flu
A, Flu B and RSV.
Flu A (FAM)
Flu B (JOE)
RSV (CFR610)
Not detected
Not detected
Not detected
Internal Control
–IC (Q670)
Detected
Detected
Not Detected
Not Detected
Detected
Not Detected
Detected
Not Detected
Detected
Not Detected
Not Detected
Detected
Detected
Invalid
Invalid
Invalid
Invalid
Interpretation
Flu A/B RNA and RSV
RNA not detected.
Influenza A RNA
Detected
Influenza B RNA
Detected
RSV RNA Detected
Invalid. Review trouble
shooting guidelines.
Invalid Results Troubleshooting:
Internal Control (IC) failure: Dilute sample 1: 10 with Viral Transport Media (VTM); pipette 50uL
specimen to 450ul VTM for a 1:10 dilution, and retest the specimen. In LIS order media PRABR, when
repeating Simplexa testing.
If repeat test is still Invalid, report as INDETERMINATE.
EC500 error code result points to a data quality error for the particular viral analyte(s). The software
was unable to determine a valid amplification for that analyte(s). Dilute sample 1: 10 with Viral
Transport Media (VTM); pipette 50uL specimen to 450ul VTM for a 1:10 dilution, and retest the
specimen. In LIS order media PRABR, when repeating Simplexa testing.
If repeat test is still Invalid, report as INDETERMINATE.
Insufficient Specimen Volume; may be due sample integrity, air bubble was introduce during
pipetting, pipetting to quickly, or R reagent was not thawed completely. Dilute sample 1: 10 with Viral
Transport Media (VTM); pipette 50uL specimen to 450ul VTM for a 1:10 dilution, and retest the
specimen. In LIS order media PRABR, when repeating Simplexa testing.
If repeat test is still Invalid, report as INDETERMINATE.
Unresolved problems should be brought to the attention of senior/charge technologist and/or contact
Focus Diagnostics Technical Services department.
PROCEDURE MANUAL
UNIVERSITY HEALTH NETWORK / MOUNT SINAI HOSPITAL MICROBIOLOGY DEPARTMENT
NOTE: This is a CONTROLLED document. Any documents appearing in paper form that are not stamped in red "MASTER COPY" are not controlled and
should be checked against the document (titled as above) on the server prior to use
D:\106748206.doc
Policy # MI/MD/v50
Microbiology Department
Policy & Procedure Manual
Section: Molecular Diagnostic Tests Manual
Page 186 of
291
VI. Reporting
Result influenza samples using the Virology Worklist “Respiratory PCR”
Negative Report:
In the Respiratory Viral Detection test comment:
Select: }SIMNegative for Influenza A , Influenza B, and Respiratory syncytial virus by Simplexa™ Flu A/B & RSV
Direct kit. Focus Diagnostics.
In the media PCABR add date tested (F6).
Finalize all negative reports.
EXCEPTION: Interim reports originating from NP swasb from PMH wards 14A/14B/14C/15A/15B
waiting for results on parainfluenza and metapneumovirus.
MULTIPLEX REQUESTS: For negative samples requesting multiplex testing, under test “Respiratory
viral detection referred out” select keypad option }PHLV. Enter “multiplex testing” in the comment.
Enter a date in the media as the day sent to PHL and interim test. Print a PHL requisition using instant
report MIC10. Affix a “Respiratory Multiplex testing” and “Negative for FluA, FluB and RSV by Focus
Simplexa” label under test requested on the requisition. Package 0.5mL of samples with the requisition
to be sent to PHOL.
Positive Report:
Record date tested (F6) and positive ct value in media PCABR
Report as a numbered Isolate in the isolate window.
Influenza A Positive. Select: \SIMA for send
DETECTED.
By Simplexa™ Flu A/B & RSV Direct kit. Focus Diagnostics Inc.”
This isolate has been forwarded to PHL
(Public Health Laboratory) for subtyping. Results are to follow.
Add date to media PHL when sample is sent to PHL.
PROCEDURE MANUAL
UNIVERSITY HEALTH NETWORK / MOUNT SINAI HOSPITAL MICROBIOLOGY DEPARTMENT
NOTE: This is a CONTROLLED document. Any documents appearing in paper form that are not stamped in red "MASTER COPY" are not controlled and
should be checked against the document (titled as above) on the server prior to use
D:\106748206.doc
Policy # MI/MD/v50
Microbiology Department
Policy & Procedure Manual
Section: Molecular Diagnostic Tests Manual
Page 187 of
291
Phone all positive results to ward / physician, and notify Infection Control Practitioner as per Isolate
Notification and Freezing Table QPCMI15003
Notify Medical Officer of Health (MOH) for Influenza A, and Influenza B.
*All Influenza A isolates should be forwarded to Toronto Public Health (PHL) for subtyping.
Use instant report MIC10 to print a PHL requisition. Affix a TIBDN Flu A subtyping label under test
requested. Make a 0.5mL aliquot to send out. Keep samples and PHL requisition in order and package
for send out at the end of the shift.
MULTIPLEX REQUESTS: Samples testing positive in house for a respiratory virus will not be sent out
for multiplex testing at PHOL. For positive samples requesting multiplex testing, under test “Respiratory
viral detection referred out” select keypad option }REFV and finalize test.
Influenza B and RSV Positive. Select: \SIM+
DETECTED.
By Simplexa™ Flu A/B & RSV Direct kit. Focus Diagnostics Inc.”
Phone all positive results to ward/physician, and notify Infection Control Practitioner as per Isolate
Notification and Freezing Table QPCMI15003
Notify Medical Officer of Health (MOH) for Influenza A, and Influenza B.
All positive Reports should be finalized by reporting technologist.
EXCEPTION: Interim reports originating from NP swasb from PMH wards 14A/14B/14C/15A/15B
waiting for results on parainfluenza and metapneumovirus.
MULTIPLEX REQUESTS: Samples testing positive in house for a respiratory virus will not be sent out
for multiplex testing at PHOL. For positive samples requesting multiplex testing, under test “Respiratory
viral detection referred out” select keypad option }REFV and finalize test.
Indeterminate Report:
Select: }SIMi
Indeterminate for Influenza A, Influenza B, and Respiratory syncytial virus by Simplexa™ Flu A/B &
RSV Direct kit. Focus Diagnostics.
Finalize all Indeterminate reports.
EXCEPTION: Interim reports originating from NP swasb from PMH wards 14A/14B/14C/15A/15B
waiting for results on parainfluenza and metapneumovirus.
PROCEDURE MANUAL
UNIVERSITY HEALTH NETWORK / MOUNT SINAI HOSPITAL MICROBIOLOGY DEPARTMENT
NOTE: This is a CONTROLLED document. Any documents appearing in paper form that are not stamped in red "MASTER COPY" are not controlled and
should be checked against the document (titled as above) on the server prior to use
D:\106748206.doc
Policy # MI/MD/v50
Microbiology Department
Policy & Procedure Manual
Section: Molecular Diagnostic Tests Manual
VII.
Page 188 of
291
Quality Control
a. All In-house External control materials: FluA, FluB, and RSV should be run first week of
each month on both 3M Cyclers for non flu season.
VIII. Troubleshooting
Follow the instructions in “Troubleshooting” folder on desktop.
IX.
Clean Up & Maintenance
Start-up. Perform daily maintenance. Slightly dampen KimWipe with 70% alcohol, wipe external
surfaces of the 3M Cyclers, and laptop keyboards. Wipe benchtop with 70% alcohol.
End of day. Clean Biological Safety Cabinet (BSC) by wiping surfaces with a 1% working solution
hypo chloride (made daily), followed by wiping surfaces with 70% alcohol. Clean pipette with slightly
dampened Kimwipe with a 1% working solution hypo chloride, followed by slightly dampened
KimWipe with 70% alcohol.
Dispose of PCR waste in sealed discard waste bags into the biohazard boxes.
Once a week, every Monday, perform Database Backup on both Analyzers.
At the Menu bar, Select Tools > Database Tools > Backup Database > Create backup
X.
Reference
1.
Simplexa Flu A/B & RSV Assay package insert.
2.
On line: http://www.cdc.gov/rsv/clinical/description.html
and http://www.cdc.gov/Features/dsRSV/
PROCEDURE MANUAL
UNIVERSITY HEALTH NETWORK / MOUNT SINAI HOSPITAL MICROBIOLOGY DEPARTMENT
NOTE: This is a CONTROLLED document. Any documents appearing in paper form that are not stamped in red "MASTER COPY" are not controlled and
should be checked against the document (titled as above) on the server prior to use
D:\106748206.doc
Policy # MI/MD/v50
Microbiology Department
Policy & Procedure Manual
Section: Molecular Diagnostic Tests Manual
Page 189 of
291
Parainfluenza RT-PCR by Rotorgene
I. Introduction:
Parainfluenza viruses (PIV) can cause upper and lower respiratory tract infections. Commonly seen in children,
but may occur at any age group causing severe disease in older adults, and people with compromised immune
systems. PIV-1 and PIV -2 often causes cold-like symptoms, and croup in children. PIV-3 is often associated with
bronchiolitis, bronchitis, and pneumonia. PIV-4 may cause mild to severe respiratory tract infections.
RealStar PIV RT-PCR is a real time PCR for the qualitative detection of human PIV RNA; differentiating PIV1and 3, and PIV-2 and 4.
II. Collection and Transport
Nasopharyngeal swabs collected in Viral Transport Media (VTM), store at 4C. Vortexed swabs on high
for 10 seconds; aliquot off the VTM and store at 4C, extract on the easyMag as soon as possible.
BAL specimens if mucoid treat with working sputolysin. Remove red blood cells and large particulate
matter by micro-centrifuging sample for 5minutes at 3000 rpm in the Eppendroff 5415 C Microcentrifuge. Aliquot supernatant and store at 4C, extract on the easyMag as soon as possible.
III. Specimen Processing
Please refer to Nucleic Acid Extraction –Biomerieux NucliSENS easyMAG
GENERAL PRECAUTIONS:
There must be separate PCR work areas:
Clean room
Specimen preparation room
Powder-free Gloves should only be in use in PCR areas. Change gloves frequently and keep
tubes closed whenever possible.
Prepare Working 1% sodium hypochloride daily.
Specimen Preparation Supplies and equipment must be dedicated to Specimen Prep Area and
not used for other activities and never used in Clean Room.
Change lab coats and gloves between work areas.
Use only Aerosol Resistant Tips (ART)
Use only sterile RNase-free, DNAse-free microtubes
Thaw components thoroughly at room temperature.
PCR work areas (Clean Room and Specimen Preparation Area) benchtops and equipment
after each shift.
Materials, Equipments and Facilities:
Clean Room: Biosafety Cabinet (MIBCT3), freezer (MIFTG)
Specimen Preparation area: Biosafety Cabinet (MIBCT7 or MIBCT8)
Rotor-Gene 6000
Rotor-Gene 6000 Multiplexing System with experiment template: Altona RealStar PIV & hMeta
PROCEDURE MANUAL
UNIVERSITY HEALTH NETWORK / MOUNT SINAI HOSPITAL MICROBIOLOGY DEPARTMENT
NOTE: This is a CONTROLLED document. Any documents appearing in paper form that are not stamped in red "MASTER COPY" are not controlled and
should be checked against the document (titled as above) on the server prior to use
D:\106748206.doc
Policy # MI/MD/v50
Microbiology Department
Policy & Procedure Manual
Section: Molecular Diagnostic Tests Manual
Page 190 of
291
72-Well Loading Block (pre-cooled to 4oC)
72-Well 6000 Series Rotor
72-Well Rotor Locking Ring
0.1 mL reaction microtubes Tubes and Caps
Variable volume Rainin pipettes: 1 to 20 uL, 10 to 200 uL, 100 to 1000 uL
Reagent: Altona RealStar PIV RT-PCR Kit 1.0: MasterA, MasterB, Internal Control, PIV-1 Positive
Control, PIV-2 Positive Control, PIV-3 Positive Control, PIV-4 Positive Control, PCR Grade Water
External Control: To be run first week of the month/ or with every new lot; run during training or if QC
failure occurs.
IV. Procedure:
Prepare samples in order according to PIV worksheet. Add the following controls to the PIV Worksheet:
P1/P3 Positive control, P2/P4 Positive Control, Negative Control (PCR grade Water).
PCR Set-up:
In the Clean Room: (Change into dedicated clean room gown and gloves, work in Biosafety Cabinet)
Remove to thaw at room temperature the required vial’s PIV Master A and Master B (12 reactions/ vial)
from the freezer.
Prepare PIV Master Mix in Sarstedt 1.5 mL conical microtube; to load on the Eppendorf epMotion.
Prepare the number of Master Mix reactions required: Number of Test samples + 3 Controls + one
Mix gently, do not vortex. Make only enough master mix for the tests you are running. After
Master A has been added to Master B it cannot be frozen again.
Number of Reactions
PIV Master A
PIV Master B
Volume of Master Mix
Sample/Control Volume
No. of Test
reactions
1
2
3
4
5
6
1
5
10
15
10
PIV Master Mix
PIV Master A (µl)
5
10
15
20
25
30
PIV Master B (µl)
10
20
30
40
50
60
PROCEDURE MANUAL
UNIVERSITY HEALTH NETWORK / MOUNT SINAI HOSPITAL MICROBIOLOGY DEPARTMENT
NOTE: This is a CONTROLLED document. Any documents appearing in paper form that are not stamped in red "MASTER COPY" are not controlled and
should be checked against the document (titled as above) on the server prior to use
D:\106748206.doc
Policy # MI/MD/v50
Microbiology Department
Policy & Procedure Manual
Section: Molecular Diagnostic Tests Manual
Page 191 of
291
7
35
70
8
40
80
9
45
90
10
50
100
11
55
110
12
60
120
See Eppendorf epMotion Manual for further loading and programming instructions.
Manual Loading:
Load one reaction microtube (0.1 mL) for each sample/control.
Pipette 15 uL prepared PIV Master Mix into each reaction microtube.
Pipette 1.0 uL of internal control into the reaction microtubes designated for the 3 PIV Controls (P1/P3
Positive Control, P2/P4 Positive Control, Negative PCR Water Control .
In the Specimen Processing Area:
Prepare Working aliquot P1/P3 Positive Control and P2/P4 Positive. Prepare as needed, use aliquot until
finished, and then prepare a new aliquot.
In a 1.5mL conical microtube pipette 180 uL PCR grade water add 20uL PIV-1 Positive Control and
add 20uL PIV-3 Positive Control; label as P1/P3 Positive Control with date.
In a 1.5mL conical microtube pipette 180 uL PCR grade water add 20uL PIV-2 Positive Control and
add 20uL PIV-4 Positive Control; label as P2/P4 Positive Control with date.
Working Positive Control PCR Grade Water
PIV Control
180uL
20uL
PIV-1
Positive Control
P1/P3 Positive Control
20uL PIV-3 Positive Control
180uL
20uL PIV-2 Positive Control
P2/P4 Positive Control
20uL PIV-4a Positive Control
20uL PIV-4b Positive Control
Pipette 10 uL each of Sample/Control into reaction microtubes. Mix by pipetting 3x up and down into
the Master Mix. Cap each segment, after pipetting is completed. Check reaction microtubes before
loading into the rotor ensure the liquid levels are at the same height, and there are no bubble at the
bottom of the reaction microtube.
Load reaction microtubes into 72-Well Blue rotor, fill empty rotor spaces with blank reaction
microtubes, attach the Locking Ring. Load the rotor in Rotor-Gene 6000.
In the Rotorgene Detection Area:
u. Switch ON computer, switch ON Rotorgene;
v. FOR BLUE ROTORGENE ONLY. Choose clinical icon; pass word “msh”; press “→”
button;
w. Open “Rotor-Gene 6000 series software 1.7” icon
x. Wait for “Initializing machine…..”
y. Highlight “Altona RealStar PIV & hMeta” experiment
PROCEDURE MANUAL
UNIVERSITY HEALTH NETWORK / MOUNT SINAI HOSPITAL MICROBIOLOGY DEPARTMENT
NOTE: This is a CONTROLLED document. Any documents appearing in paper form that are not stamped in red "MASTER COPY" are not controlled and
should be checked against the document (titled as above) on the server prior to use
D:\106748206.doc
Policy # MI/MD/v50
Microbiology Department
Policy & Procedure Manual
Section: Molecular Diagnostic Tests Manual
Page 192 of
291
z. Select “New” button;
aa. Highlighting the correct Rotor type you are using
bb. 72-well Rotor (Blue)
cc. Check the box for “Locking Ring Attached” option
dd. Select “Next” button
ee. Enter operator initials. In Notes enter RotorGene Colour (i.e. RED or BLUE) Reagent Lot
number. Make sure the Reaction Volume is “25µl”;
ff. Select “Next” button
Temperature profile window appears, select “Next” button
gg. Rotor must be loaded.
hh. Summary window appears, select “Start Run” button;
ii. Save As window appears; the run is given a filename with a default template. Save in My
documents in PIV &hMeta folder for the current year: e.g. Altona Realstar PIV & hMeta
20150101(1) (e.g. assay name-year-month-date-numerical run#);
a. Note: PIV & hMeta results are stored in \desktop\My Doucument\Altona RealStar PIV & hMeta
jj. Select Save button;
kk. Machine starts and Edit Samples window appears.
ll. Enter sample numbers including positive and negative controls. Define the type of samples
according to the chart:
Name
Sample
P1/P3 Positive Control
P2/P4 Positive Control
PCR Grade Water
Type
Unknown
Positive Control
Positive Control
Negative Control
Select
Yes
Yes
Yes
Yes
mm.
Select Finish button.
nn. Once cycling screen appears, select “Named On” button.
To analyze and print PIV report after a run is finished:
w. The run is done when Profile Program reads: Run has completed.
x. Analyze raw data by selecting each channel, one at a time: Green channel PIV-1 and PIV3, Red channel PIV-2 and PIV-4 and Yellow channel Internal Control (IC).
Target
Channel
PIV-1 and PIV-3 RNA Green
PIV-2 and PIV-4a/b
Red
Internal Control
Yellow
Report
Dye
FAM
Cy5
JOE
y. Select autoscale (bottom left). Click “All Off” (bottom right). Click “water” on. Compare the
specimen and control curves to the water one at a time (by selecting each sample on and then off,
PROCEDURE MANUAL
UNIVERSITY HEALTH NETWORK / MOUNT SINAI HOSPITAL MICROBIOLOGY DEPARTMENT
NOTE: This is a CONTROLLED document. Any documents appearing in paper form that are not stamped in red "MASTER COPY" are not controlled and
should be checked against the document (titled as above) on the server prior to use
D:\106748206.doc
Policy # MI/MD/v50
Microbiology Department
Policy & Procedure Manual
Section: Molecular Diagnostic Tests Manual
Page 193 of
291
then proceeding to the next sample). A positive curve will have a sigmoidal shape. A negative
result will be a relatively flat line, like the water. Make a note of the positives on the PIV
Worksheet.
z. Select on “Named On”
aa. Perform curve analysis: Select Analysis on the top tool bar.
bb. Analysis floating window pops up
cc. Select “Quantitation” tab.
dd. Quantitation window is brought up to the front. There should be three channels: Green PIV-1/3,
Red PIV-2/4 and Yellow (IC).
ee. Highlight Cycling A. Green PIV-1/3 option and select Show button.
ff. Maximize Target (Green/Red/Yellow)window
gg. Select slope correct
hh. Select Ignore first… 5 cycles
ii. Set threshold at 0.05. A threshold line will appear on the screen.
jj. Move threshold line to above the noise (i.e. Negative specimens)
kk. To Print reports: Select Reports button on the top toolbar.
ll. Report Browser window pops up.
mm.
Choose Cycling A. Green PIV-1/3 . Under templates box, choose
“Quantitation full report”.
nn. Select Show button
oo. Maximize the report window, check that only the positives that you have identified from your
raw data analysis are positive (i.e. have a crosspoint).
pp. Choose print report. (red and yellow channels print only pages 2-4).
qq. Once finished printing, close the report window
rr. Go to the floating Analysis window;
ss. Repeat the step from “e” to “t” for Cycling A. Red PIV-2/4 and Cycling A. Yellow Internal
control
Shut down computer:
Exit from software. “save changes”. Select “yes”.
Select“start” button. Select “Turn off computer”.
Turn off Rotorgene
End of Shift Cleaning: Perform cleaning protocol as outlined below.
Clean Room: Wipe down with RNAse Away or NucleoClean on paper towel, followed by distilled
water, and then 70% alcohol
Biological Safety Cabinet
Pipettes
Bench tops
PROCEDURE MANUAL
UNIVERSITY HEALTH NETWORK / MOUNT SINAI HOSPITAL MICROBIOLOGY DEPARTMENT
NOTE: This is a CONTROLLED document. Any documents appearing in paper form that are not stamped in red "MASTER COPY" are not controlled and
should be checked against the document (titled as above) on the server prior to use
D:\106748206.doc
Policy # MI/MD/v50
Microbiology Department
Policy & Procedure Manual
Section: Molecular Diagnostic Tests Manual
Page 194 of
291
Specimen Preparation Area: Wipe down with Working 1% hypochloride (made daily), followed by
distilled water, and then 70% alcohol
Biological Safety Cabinet (BSC), pipettes, centrifuge, and bench top.
Seal and discard BSC waste
Wash racks.
EasyMAG , Lysis Rack, and BioHit Multi-channel Pipette: Wipe down surfaces with RNAse Away
or NucleoClean on KimWipe, followed by UltraPure water, and then 70% alcohol Wipe
Amplification Area: Wipe down surfaces with RNAse Away or NucleoClean on KimWipe, followed
by UltraPure water, and then 70% alcohol Wipe
Seal & discard reaction microtubes into biohazard waste after each run.
Perform the cleaning procedure according the daily maintenance sheet.
IV.
Interpretation and Reporting:
Green
Channel
PIV1/3
Red
Channel
PIV2/4
Yellow Channel
(IC specific)
Interpretations
+
-
+/-
PIV-1/3 DETECTED
-
+
+/-
PIV-2/4 DETECTED
+
+
+/-
PIV-1/3 DETECTED.
PIV-2/4 DETECTED.
(ask charge/senior for confirmation)
-
-
+
PIV NOT DETECTED
-
-
-
INVALID
Respiratory sample needs to be diluted 1:4 with
VTM and re-extracted and RT-PCR repeated.
VTM=Viral Transport Media
PIV-1/3 DETECTED. or PIV-2/4 DETECTED
Report as an isolate in the (F7) Isolate Window.
Date the media on the back of the LIS workcard PCPIN: F6 to add the date tested.
In the media PCPIN enter crosspoint (ct) value : ct=
Report the virus as an isolate in the F7 window.
PROCEDURE MANUAL
UNIVERSITY HEALTH NETWORK / MOUNT SINAI HOSPITAL MICROBIOLOGY DEPARTMENT
NOTE: This is a CONTROLLED document. Any documents appearing in paper form that are not stamped in red "MASTER COPY" are not controlled and
should be checked against the document (titled as above) on the server prior to use
D:\106748206.doc
Policy # MI/MD/v50
Microbiology Department
Policy & Procedure Manual
Section: Molecular Diagnostic Tests Manual
Page 195 of
291
Isolate #: 1, or next available isolate number.
Org. ID: 24par13
Parainfluenza virus 1 and/or 3
24par24
Parainfluenza virus 2 and/or 4
The reporting isolate comment is attached to the Organism ID.
Verify All in the isolate window.
Review report entry: media, isolate.
Finalize the report.
Call all positives to ward/doctor and Infection Control Practitioner (ICP). Document calls and emails
in the media CALL.
PIV-1/3 NOT DETECTED. or PIV-2/4 NOT DETECTED
Date the media on the back of the workcard. PCPIN: F6 to add run date.
On the front of the workcard, select from the keypad: }PI}PI-
Negative for parainfluenza virus by RealStar
PIV RT-PCR, Altona Diagnostics.
Review report entry.
Finalize the report.
PIV INDETERMINATE
Internal control has failed twice to amplify in a sample.
Date the media on the back of the LIS workcard. PCPIN: F6 to add run date.
Select from the keypad “Failed single”, type “IC no amplification”, select >FAIL
Select from keypad ^PRPIN
Under this media ^PRPIN report the 1:4 dilution test result type “IC no amplification”.
Report: select from the keypad: }PIChange “Negative” to INDETERMINATE; final report should appear as:
INDETERMINATE for parainfluenza virus by RealStar
PIV RT-PCR, Altona Diagnostics.
Review report entry.
Finalize the report.
V.
Quality Control
Reagent QCs:
An External Control (external to Altona Diagnostics) is used to monitor the isolation,
amplification and detection procedures. The result must correspond to expected value supplied
by the manufacturer.
PROCEDURE MANUAL
UNIVERSITY HEALTH NETWORK / MOUNT SINAI HOSPITAL MICROBIOLOGY DEPARTMENT
NOTE: This is a CONTROLLED document. Any documents appearing in paper form that are not stamped in red "MASTER COPY" are not controlled and
should be checked against the document (titled as above) on the server prior to use
D:\106748206.doc
Policy # MI/MD/v50
Microbiology Department
Policy & Procedure Manual
Section: Molecular Diagnostic Tests Manual
a.
b.
c.
d.
e.
f.
g.
h.
i.
j.
Page 196 of
291
External control for PIV-1/3, and PIV-2/4 should be extracted on the on the easyMag and run
once a month and/or with each new lot.
Daily QCs: Every Run
Each patient specimen must have an Internal Control (IC) added to monitor both isolation and
PCR inhibition.
A Positive Control is included and shows a positive reading in
Green PIV-1/3 Channel or a positive reading in Red PIV-2/4 Channel
A Negative Control is include and shows a negative reading in both Green PIV-1/3 Channel or a
negative reading in Red PIV-2/4 Channel
Report all failed QCs to senior/charge technologist.
Failed QC:
Test is invalid without satisfactory QC results.
Do not release results pending resolution of QC failure.
Inform charge/senior technologist.
Record in Reagent Log Chart, Instrument Maintenance Log or Incident Report where
appropriate.
If the QC failure was due to a simple matter of position reversal or misplacement, the run can be
released (positive QC material yielded positive result, negative yielded negative result).
If positive QC material yielded negative result, repeat the entire run.
If negative QC material yielded positive result, it may be due to cross-contamination from
adjacent positive sample within the run or carry-over contamination from previous runs via
equipment or the environment. Review procedure and equipment to establish and eliminate
potential sources of contamination.
The extent and nature of contamination can also be evaluated by comparing the positive rate of
the run with its expected positive rate.
If the contamination is extensive, it is necessary to quarantine/discard potentially contaminated
reagents and consumables and disinfect equipment and environment before repeating the run.
If a carry-over contamination is suspected (e.g. two or more runs with negative QC being
positive or patient samples have higher than expected positive rate and these samples are often
non-repeatable positives), it is necessary to have a thorough environmental disinfection followed
by swabbing to monitor.
Successful ending to a carry-over contamination may be indicated by QC results and patient
positivity rate falling back to the expected normal range and three negative environmental swabs.
V. References:
RealStar PIV RT-PCR Kit v1.0, altona Diagnostics
cdc.gov/Human Parainfluenza Viruses (HPIVs) (/parainfluenza/index.html
PROCEDURE MANUAL
UNIVERSITY HEALTH NETWORK / MOUNT SINAI HOSPITAL MICROBIOLOGY DEPARTMENT
NOTE: This is a CONTROLLED document. Any documents appearing in paper form that are not stamped in red "MASTER COPY" are not controlled and
should be checked against the document (titled as above) on the server prior to use
D:\106748206.doc
Policy # MI/MD/v50
Microbiology Department
Policy & Procedure Manual
Section: Molecular Diagnostic Tests Manual
Page 197 of
291
Parvovirus B19 PCR by Rotorgene
I.
Introduction
Parvovirus B19 belongs to the DNA virus family Parvoviridae and the genus Erythrovirus.
Infection with B19 may result in an asymptomatic infection or produce a wide range of disease;
ranging from erythema infections in children (slapped cheek syndrome or fifth disease) to severe
anemia (the cause of aplastic crisis in hemolytic anemias and in sickle-cell disease), and systemic
disease involving the central nervous system, heart, liver depending on the immune competence
of the host. In pregnant women, Parvovirus B19 may cause hydrops fetalis, congenital anemia,
fetal death, or spontaneous abortion.
II.
Collection and Transport
Amniotic fluid stored at 4C and extract on the BioMerieux EasyMag as soon as possible. EDTA
plasma; EDTA blood is spun at 3000 rpm for 10 minutes and the plasma is separated and extract
on the BioMerieux EasyMag as soon as possible.
III.
Specimen Processing
Please refer to Nucleic Acid Extraction – Biomerieux NucliSENS easyMAG
GENERAL PRECAUTIONS:
There must be separate PCR work areas:
Clean room
Specimen preparation room
Amplification room
Supplies and equipment must be dedicated to each PCR area and not used for other activities
or moved between areas.
Change lab coats and gloves between work areas. Only blue gowns are to be worn in the
clean room.
Use only filtered pipette tips
Use only sterile RNase, Dnase-free microcentrifuge tubes
Use sterile, disposable polypropylene tubes throughout the procedure
Always wear powder-free gloves when handling reagents
Change gloves frequently and keep tubes closed whenever possible
Keep the Quantitation Standards and specimens in the specimen preparation area.
Thaw components thoroughly at room temperature
Mix components and centrifuge briefly
Work quickly in the cooling block
Use 1% sodium hypochloride or RNAse Away to disinfect equipment and surfaces and then
rinse with 70% alcohol or water.
PROCEDURE MANUAL
UNIVERSITY HEALTH NETWORK / MOUNT SINAI HOSPITAL MICROBIOLOGY DEPARTMENT
NOTE: This is a CONTROLLED document. Any documents appearing in paper form that are not stamped in red "MASTER COPY" are not controlled and
should be checked against the document (titled as above) on the server prior to use
D:\106748206.doc
Policy # MI/MD/v50
Microbiology Department
Policy & Procedure Manual
Section: Molecular Diagnostic Tests Manual
Page 198 of
291
Materials, Equipments and Facilities:
Clean Room with dedicated Biosafety Cabinet (MIBCT4), freezer (MIFTG), gowns and gloves
Specimen Preparation area with Biosafety Cabinet and microcentrifuge
Detection Room for Rotor-Gene 6000
Rotor-Gene 6000 Multiplexing System programmed for ALTONA VZ PCR
72-Well Loading Block (pre-cooled to 4oC)
72-Well 6000 Series Rotor
72-Well Rotor Locking Ring
0.1 mL Strip Tubes and Caps
36-Well Loading Block (pre-cooled to 4oC)
36-Well Rotor Locking Ring
0.2mL Tubes
Variable volume pipettes: 1 to 20 uL
10 to 200 uL
100 to 1000 uL
From: Altona Parvovirus B19 PCR Kit 1.0, (stored at -20o C in clean room):
QS1 (10^4 Copies/µL)
QS2 (10^3 Copies/µL)
QS3 (10^2 Copies/µL)
QS4 (10^1 Copies/µL)
Master A (12 tests per vial)
Master B (12 tests per vial)
Internal Control (IC)
Water (PCR grade)
External Control: To be run when a new lot is used, during training or if QC failure occurs.
IV.
Procedure:
Prepare Parvovirus B19 Worklist and arrange eluates in order according to the worklist store at
4C until it is time to add sample to the master mix.
Remove the Parvo B19 QS3 from -20C freezer and place at 4C until ready to load.
In the Clean Room: (Change into dedicated clean room gown and gloves, work in Biosafety
Cabinet)
a. Take out the necessary number of Parvovirus B19 Master Mix A and B vials (12 tests per
vial) from the freezer and thoroughly thaw inside the Biosafety Cabinet. Determine the
PROCEDURE MANUAL
UNIVERSITY HEALTH NETWORK / MOUNT SINAI HOSPITAL MICROBIOLOGY DEPARTMENT
NOTE: This is a CONTROLLED document. Any documents appearing in paper form that are not stamped in red "MASTER COPY" are not controlled and
should be checked against the document (titled as above) on the server prior to use
D:\106748206.doc
Policy # MI/MD/v50
Microbiology Department
Policy & Procedure Manual
Section: Molecular Diagnostic Tests Manual
Page 199 of
291
number of tests and prepare the appropriate volume of Master Mix required according to the
chart. Mix gently, do not vortex.
No. of samples
1
2
3
4
5
6
7
8
9
10
11
12
Preparation of Master Mix
Master A (µl)
5
10
15
20
25
30
35
40
45
50
55
60
Master B (µl)
15
30
45
60
75
90
105
120
135
150
165
180
b. Place proper micro tubes for each purified sample, Positive controls, external QC and
Negative control (H2O) into the Cooling Block (pre-cooled to 4oC).
c. Pipette 20 uL prepared Master Mix (A+B) into each micro tubes.
d. Pipette 1.0 uL of internal control into the micro tubes designated for the Positive control
(Parvo B19 QS3 100 cp/uL) and the Negative control.
e. Pipette 10uL water (PCR grade) into the negative control micro tube and cap tightly.
f. Place the cooling block in to a clean biohazard bag.
g. Changed out of dedicated clean room gown.
In the Specimen Processing Area: (Changed into specimen room gown)
a. Using a separate filter tip each time, carefully pipette 10 uL each of purified sample, Positive
controls (QS3), and external QC (if using) directly into the micro tubes. Mix by pipetting up
and down. Close the lid tightly.
b. Check that each micro tube is closed tightly before loading. Make sure there are no bubbles
at the bottom of the micro tubes.
In the RotorGene room:
a. Turn on computer, turn on rotorGene.
b. FOR THE BLUE ROTORGENE ONLY. Choose clinical icon; pass word “msh”; press
“→” button
PROCEDURE MANUAL
UNIVERSITY HEALTH NETWORK / MOUNT SINAI HOSPITAL MICROBIOLOGY DEPARTMENT
NOTE: This is a CONTROLLED document. Any documents appearing in paper form that are not stamped in red "MASTER COPY" are not controlled and
should be checked against the document (titled as above) on the server prior to use
D:\106748206.doc
Policy # MI/MD/v50
Microbiology Department
Policy & Procedure Manual
Section: Molecular Diagnostic Tests Manual
c.
d.
e.
f.
g.
h.
i.
j.
k.
l.
m.
n.
o.
p.
q.
r.
s.
Page 200 of
291
Double click(left on the mouse) “Rotor-Gene 6000 series software 1.7” icon
Wait for “Initializing machine…..”
Load micro tubes into a proper rotor (eg. 36-well or 72-well).
Fill up the empty positions of the rotor using empty microtubes and snap close the locking
ring. Load the rotor in Rotor-Gene 6000.
Highlight Parvo B19 assay;
Press “New” button;
Highlighting the correct Rotor type you are using
72-well Rotor (Blue)
36-well Rotor (Red)
Tick the “Locking Ring Attached” option
Press “Next” button
Enter initials at Operator space and make sure the Reaction Volume is “30µl”; enter lot no. in
the Notes section.
Press “Next” button
Temperature profile window pops up, press “Next” button.
Make sure your ring has been loaded in the Rotorgene.
Summary window pops up, press “Start Run” button. The RotorGene will start.
Save as window appears; go to My documents -Open–select Parvo result folder- Open
Press Save –Parvo yyyy-mm-dd (run no.)
Press Save button.
Machine is starting and Edit Samples window pops up
Enter sample LIS# including positive and negative controls. Define the type of samples
according to the chart:
Name
Sample Number
QS3 Parvo B19
Water
Type
Given conc.
Select
Unknown
Yes
Positive Control
Yes
Negative Control
Yes
t. Once finishing all samples, press Finish button.
u. Once cycling screen cmes on, click “Named On” button.
To analyze and print Parvo B19 report after a run has finished:
The run is done when Profile Program reads: Run has completed.
Analyze raw data by clicking on the each of these channels (one at a time).
PROCEDURE MANUAL
UNIVERSITY HEALTH NETWORK / MOUNT SINAI HOSPITAL MICROBIOLOGY DEPARTMENT
NOTE: This is a CONTROLLED document. Any documents appearing in paper form that are not stamped in red "MASTER COPY" are not controlled and
should be checked against the document (titled as above) on the server prior to use
D:\106748206.doc
Policy # MI/MD/v50
Microbiology Department
Policy & Procedure Manual
Section: Molecular Diagnostic Tests Manual
Page 201 of
291
Green channel (Parvo B19), and Yellow channel (IC). These tabs are found on the second menu
bar from the top, on the left hand side.
Select the Green Channel (Parvo B19). Click “All Off” (bottom right). Select sample “water
Negative Control” and “QS3 Parvo B19 Positive Control”. Click on Autoscale (bottom left).
Compare each specimen curve to the water curve and the QS3 Parvo B19 Positive Control one at
a time (by clicking each sample on and off then proceeding to the next sample). A positive curve
will have a sigmoidal shape. A negative result will be a relatively flat line, like the water. Make a
note of all positives on the worklist.
a.
b.
c.
d.
e.
Click on “Named On”
Perform curve Analysis (Get report): Click “Analysis” on the top tool bar.
Analysis floating window pops up;
Click Quantitation Analysis.
Quantitation window is brought up to the front. There should be four channels: Green
(Parvo B19), and Yellow (IC).
f.
g.
h.
i.
j.
k.
l.
m.
n.
Highlight Cycling A. Green (Parvo B19) option and press Show.
Maximize cycling green window (or the channel you are working on)
Press button “Slope Correct” on the top.
Press button “Ignore first” on the top, and type “5”, press OK.
Set threshold at 0.05. A threshold line will appear on the screen.
Move threshold line to above the noise (i.e. Negative specimens)
To Print reports: Press “Reports”.
Report Browser window pops up.
Choose Cycling A. Green (Page 1).
Highlight Quantitation full report, press “Show”.
Maximize the report window, check that only the positives that you have identified from the
raw data review are positive and have a crosspoint (ct value).
o. Print pages 1-4 for the green channel; pages 2-4 for all the other channels.
p. Yellow channel Analysis. Go to the floating Analysis window: Quantitation tab, select
Cycling A. Yellow -the internal control (IC), select Show.
Maximize the graph Quantitation Analysis –Cycling A. Yellow.
Select Slope Correct. Select Ignore first and type “5” press OK (this will ignore the
readings in the first 5 cycles of the run).
Set the threshold (right-hand side middle) at 0.05. A threshold line will appear on your graph
screen. Move the threshold line to above the noise.
q. Press Reports. Select Cycling A.Yellow. Select Quantitation (Full report). Select Show.
All samples should have a positive IC curve, and a cycle number in the Ct column.
Print pages 2-4.
(For Cycling A. Yellow report, if there is message of “NEG (Multi Ct)” for any specimen,
you have to go back to check Raw Data of cycling A.Yellow. If all specimens are
PROCEDURE MANUAL
UNIVERSITY HEALTH NETWORK / MOUNT SINAI HOSPITAL MICROBIOLOGY DEPARTMENT
NOTE: This is a CONTROLLED document. Any documents appearing in paper form that are not stamped in red "MASTER COPY" are not controlled and
should be checked against the document (titled as above) on the server prior to use
D:\106748206.doc
Policy # MI/MD/v50
Microbiology Department
Policy & Procedure Manual
Section: Molecular Diagnostic Tests Manual
Page 202 of
291
amplified, adjust the threshold in Quantitation Analysis for Cycling A.Yellow, so that all
samples have one Ct.
Adjust the threshold line so that the threshold line crosses the curve at only one point.)
r. Close the outer most window.
“Save changes to Altona Parvo B19 yyyy-mm-dd?” Select Yes.
Shut down the computer, and switch off the RotorGene.
At the end of the day, follow the cleaning protocol below using 1% hypochorite followed by 70%
alcohol:
Clean Room:
Clean Biological Safety Cabinet, pipettors, and bench tops
Specimen Preparation Area:
Clean Biological Safety Cabinet, pipettors, centrifuge, and bench top.
Bag and securely close off bag and discard waste
Wash racks.
Clean the easyMag according to the daily maintenance sheet
Amplification Area:
Discard microtubes into a disposal bag and tight the bag.
Discard the bag into biohazard waster container.
Perform the cleaning procedure according the daily maintenance sheet: clean the rotor and
cooling blocks with RNase Away, followed by double distilled water, and finally 70% alcohol
PROCEDURE MANUAL
UNIVERSITY HEALTH NETWORK / MOUNT SINAI HOSPITAL MICROBIOLOGY DEPARTMENT
NOTE: This is a CONTROLLED document. Any documents appearing in paper form that are not stamped in red "MASTER COPY" are not controlled and
should be checked against the document (titled as above) on the server prior to use
D:\106748206.doc
Policy # MI/MD/v50
Microbiology Department
Policy & Procedure Manual
Section: Molecular Diagnostic Tests Manual
Page 203 of
291
Interpretation:
Green Channel
Parvo B19 target
Yellow Channel
Internal Control
Interpretation
-
+
Report: Negative for Parvo B19 DNA by PCR.
+
+
+
-
-
-
Preliminary report: Positive
Repeat extraction & Parvo B19 PCR to confirm.
Parvovirus B19 DETECTED, confirmation to
follow.
Notify senior or Charge.
Preliminary report: Positive
Repeat extraction & Parvo B19 PCR to confirm.
Parvovirus B19 DETECTED, confirmation to
follow.
Notify senior or Charge.
Possible PCR inhibition.
Repeat extraction & PCR.
If still negative on Yellow IC Channel, report:
INDETERMINATE for Parvo B19.
PCR Positives from sterile sites: CSF, eye specimens, biopsy, tissues; should be
repeated a second time. Re-extract the sample on the easyMAG and repeat the PCR.
Release a preliminary report, see below “Reporting”.
VII.
Reporting:
Negative for Parvovirus B19.
Under media on the back of the LIS workcard. PCPAR: F6 to add run date
Report on the front of the LIS workcard from the keypad select: }PAR}PAR-
Negative for Parovirus B19.
This is a research test.
Parvo B19 PCR Kit v1.0.
Altona Diagnostics Inc.
Ctrl-F to finalize the report.
PROCEDURE MANUAL
UNIVERSITY HEALTH NETWORK / MOUNT SINAI HOSPITAL MICROBIOLOGY DEPARTMENT
NOTE: This is a CONTROLLED document. Any documents appearing in paper form that are not stamped in red "MASTER COPY" are not controlled and
should be checked against the document (titled as above) on the server prior to use
D:\106748206.doc
Policy # MI/MD/v50
Microbiology Department
Policy & Procedure Manual
Section: Molecular Diagnostic Tests Manual
Page 204 of
291
Sterile sites: PRELIMINARY Positive for Parvovirus B19.
Date the media on the back of the LIS workcard. PCPAR: F6 to add run date
Enter on the media line the cross point (ct) value: Ct=
Order a repeat Parvo PCR test, on the back of the workcard. >FAIL, Ctrl D, select from keypad
^PRPAR Enter.
Report the virus as an isolate in the F7 window.
Isolate #: 1
Org. ID: 63parB
Parvovirus B19
Open the Isolate Comment window F8.
Go to the Virology keypad, type “V”. Ctrl D. Select from the keypad: \B19+ to add the comment
phrase.
\B19+
DETECTED by PCR, confirmation to follow.
This is a research test.
PARVO B19 PCR Kit v1.0, Altona Diagnostics Inc.
Manually type the phrase “confirmation to follow.”
Grave (`) the result.
Ctrl-P to prelim the report. Call reports to ward/doctor.
Sterile sites: CONFIRMED Positive for Parvovirus B19.
Date the media on the back of the LIS workcard. ^PRPAR : F6 to add run date
Enter on the media line the cross point (ct) value: Ct=
Open the Isolate (F7) Comment window (F8)
Isolate #: 1
Org. ID: 63parB
Parvovirus B19
Open the Isolate Comment window F8.
Delete the phrase “confirmation to follow”. Manually type: CONFIRMED
The final reporting phrase should appear as below:
\B19+
DETECTED by PCR, CONFIRMED.
This is a research test.
PARVO B19 PCR Kit v1.0, Altona Diagnostics Inc.
Grave (`) the result.
Ctrl-F to finalize the report.
PROCEDURE MANUAL
UNIVERSITY HEALTH NETWORK / MOUNT SINAI HOSPITAL MICROBIOLOGY DEPARTMENT
NOTE: This is a CONTROLLED document. Any documents appearing in paper form that are not stamped in red "MASTER COPY" are not controlled and
should be checked against the document (titled as above) on the server prior to use
D:\106748206.doc
Policy # MI/MD/v50
Microbiology Department
Policy & Procedure Manual
Section: Molecular Diagnostic Tests Manual
Page 205 of
291
Sterile sites: NOT CONFIRMED for Parvovirus B19.
Date the media on the back of the LIS workcard. ^PRPAR: F6 to add run date
Isolate #: 1 must be suppressed, change to an alphabet
Front of the LIS workcard type the following:
UPDATED REPORT: Previously reported Parvovirus B19 NOT CONFIRMED.
Report on the front of the LIS workcard (manually type):
This is a research test.
This is a research test.
PARVO B19 PCR Kit v1.0, Altona Diagnostics Inc.
Ctrl-F to finalize the report. Call Updated reports to ward/doctor.
V.
Quality Control
Reagent QCs:
An External Control (external to Altona Diagnostics) is used to monitor the isolation,
amplification and detection procedures. The result must correspond to expected value supplied
by the manufacturer.
External control for Parvo B19 should be extracted on the on the easyMag and run once a month
and/or with each new lot.
Daily QCs:
Every run:
Each patient specimen must have an Internal Control (IC) added to monitor both extraction and
PCR inhibition.
A Positive Control is included and shows either a positive reading in Green Channel (QS3 Parvo
B19)
A Negative PCR Water Control is included and shows a negative reading in Green Channel
(QS3 Parvo B19)
Report all failed QCs to senior/charge technologist.
Failed QC:
Test is invalid without satisfactory QC results.
PROCEDURE MANUAL
UNIVERSITY HEALTH NETWORK / MOUNT SINAI HOSPITAL MICROBIOLOGY DEPARTMENT
NOTE: This is a CONTROLLED document. Any documents appearing in paper form that are not stamped in red "MASTER COPY" are not controlled and
should be checked against the document (titled as above) on the server prior to use
D:\106748206.doc
Policy # MI/MD/v50
Microbiology Department
Policy & Procedure Manual
Section: Molecular Diagnostic Tests Manual
Page 206 of
291
a. Do not release results pending resolution of QC failure.
b. Inform charge/senior technologist.
c. Record in Reagent Log Chart, Instrument Maintenance Log or Incident Report where
appropriate.
d. If the QC failure was due to a simple matter of position reversal or misplacement, the run can be
released (positive QC material yielded positive result, negative yielded negative result).
e. If positive QC material yielded negative result, repeat the entire run.
f. If negative QC material yielded positive result, it may be due to cross-contamination from
adjacent positive sample within the run or carry-over contamination from previous runs via
equipment or the environment. Review procedure and equipment to establish and eliminate
potential sources of contamination.
g. The extent and nature of contamination can also be evaluated by comparing the positive rate of
the run with its expected positive rate.
h. If the contamination is extensive, it is necessary to quarantine/discard potentially contaminated
reagents and consumables and disinfect equipment and environment before repeating the run.
i. If a carry-over contamination is suspected (e.g. two or more runs with negative QC being
positive or patient samples have higher than expected positive rate and these samples are often
non-repeatable positives), it is necessary to have a thorough environmental disinfection followed
by swabbing to monitor.
j. Successful ending to a carry-over contamination may be indicated by QC results and patient
positivity rate falling back to the expected normal range and three negative environmental swabs.
Report all failed QCs to senior/charge technologist
VI.
References:
Parvo B19 PCR kit v1.0, Altona Diagnostics Inc.
PROCEDURE MANUAL
UNIVERSITY HEALTH NETWORK / MOUNT SINAI HOSPITAL MICROBIOLOGY DEPARTMENT
NOTE: This is a CONTROLLED document. Any documents appearing in paper form that are not stamped in red "MASTER COPY" are not controlled and
should be checked against the document (titled as above) on the server prior to use
D:\106748206.doc
Policy # MI/MD/v50
Microbiology Department
Policy & Procedure Manual
Section: Molecular Diagnostic Tests Manual
Page 207 of
291
West Nile Virus PCR by Rotorgene
I.
Introduction
West Nile virus (WNV) is a flavivirus belonging to the Japanese Encephalitis group. The
primary host is wild birds and the virus is usually transmitted to humans via mosquitoes.
Transplants and blood transfusions have also been implicated in its transmission.
This assay involves isolating the viral RNA using the Qiagen Viral RNA Kit and amplifying it
by Altona (previously known as Altona) RealStarTM WNV Reverse-Transcription (RT)-PCR Kit.
The amplification and detection take place simultaneously, continually and in real time in the
Rotor-GeneTM.
In real-time PCR, fluorescent dyes are linked to oligonucleotide probes, which bind specifically
to the amplified product. Monitoring the level of fluorescence allows the detection of the
amplicon. In the RealStarTM WNV assay, two fluorescent dyes are incorporated in the master
mix to detect two amplified products: One for the WNV amplicon; and the other for the Internal
Control (IC). The IC is added to each specimen in the initial step to both control the isolation
procedure and to check for PCR inhibition. The Rotor-Gene TM simultaneously monitors the two
different amplicons using two fluorimeter channels.
II.
Collection and Transport
Blood samples for WNV PCR should be collected in EDTA (purple top vacutainer tube). CSF
specimens should be collected in a clean, sterile container and sent to the laboratory as soon as
possible. If specimens cannot be transported immediately, they should be kept at 4oC. If a delay
of more than 6 hours is anticipated, the CSF specimen should be frozen at –70oC. The EDTA
samples should be processed within 6 hours of collection (plasma separated and refrigerated;
frozen if delay is more than 6 hours). Allow only one freeze-thaw cycle.
NOTE: Repeated freezing-thawing will reduce test sensitivity and cryoprecipitates may
accumulate in the plasma.
III.
Materials, Equipments and Facilities:
Clean Room with dedicated Biosafety Cabinet (MIBCT3), freezer (MIFTG), gowns and gloves
Specimen Preparation area with Biosafety Cabinet (MIBCT7 or MIBCT8) and microcentrifuge
(MICT17)
Vortex
Detection Room for Rotor-Gene 6000
Rotor-Gene 6000 Multiplexing System programmed for ALTONA WNV RT PCR
PROCEDURE MANUAL
UNIVERSITY HEALTH NETWORK / MOUNT SINAI HOSPITAL MICROBIOLOGY DEPARTMENT
NOTE: This is a CONTROLLED document. Any documents appearing in paper form that are not stamped in red "MASTER COPY" are not controlled and
should be checked against the document (titled as above) on the server prior to use
D:\106748206.doc
Policy # MI/MD/v50
Microbiology Department
Policy & Procedure Manual
Section: Molecular Diagnostic Tests Manual
Page 208 of
291
36-Well High Profile Rotor
36-Well Rotor Locking Ring
0.2 mL Tubes
1.5 mL microcentrifuge tubes
Variable volume pipettes:
1 to 20 uL
10 to 200 uL
100 to 1000 uL
From Qiagen Viral Isolation Kit:
Collection Tubes
Dissolve the lyophilized carrier RNA with 320uL of Elution Buffer. Individually
pipette 5.6 uL into microcentrifuge tubes, freeze at – 20oC.
Spin Columns
Wash Buffer 1 (Buffer AW1) – add 125 mL ethanol before use
Wash Buffer 2 (Buffer AW2) – add 160 mL ethanol before use
Elution Buffer (Buffer AVE)
From: Altona WNV RT-PCR Kit 1.0, (stored at -20o C in clean room):
WNV Positive Control
Master A (12 tests per vial)
Master B (12 tests per vial)
Internal Control (IC)
Water (PCR grade)
External Control: To be run when a new lot is used, during training or if QC failure occurs.
IV.
General Precautions:
There must be separate PCR work areas:
a. Clean room
b. Specimen preparation room
Amplification room Supplies and equipment must be dedicated to each PCR area
and not used for other activities or moved between areas.
Change lab coats and gloves between work areas. Only blue gowns are to be worn
in the clean room.
Use only filtered pipette tips
Use only sterile RNase, Dnase-free microcentrifuge tubes
Use sterile, disposable polypropylene tubes throughout the procedure
Always wear powder-free gloves when handling reagents
Change gloves frequently and keep tubes closed whenever possible
Thaw components thoroughly at room temperature
PROCEDURE MANUAL
UNIVERSITY HEALTH NETWORK / MOUNT SINAI HOSPITAL MICROBIOLOGY DEPARTMENT
NOTE: This is a CONTROLLED document. Any documents appearing in paper form that are not stamped in red "MASTER COPY" are not controlled and
should be checked against the document (titled as above) on the server prior to use
D:\106748206.doc
Policy # MI/MD/v50
Microbiology Department
Policy & Procedure Manual
Section: Molecular Diagnostic Tests Manual
V.
Page 209 of
291
Mix components and centrifuge briefly
Work quickly in the cooling block
Use 1% sodium hypochloride or Eliminase to disinfect equipment and surfaces
and then rinse with 70% alcohol or water.
Procedure
Sample Preparation:
Lysis and Purification Steps:
a. For each specimen and External Control, prepare and label one 1.5 mL microcentrifuge tubes
(sterilized, RNase-free) with the corresponding number in the Worklist. Put the specimens
first on the worklist, followed by the external control (if using one). Label one of them with
the lab number (LIS label). This microcentrifuge tube will store the eluted RNA, the other
will be used for processing and will be discarded. Also, label one QIAamp Spin Column
(Qiagen) with the number on the Worklist. Arrange the microcentrifuge tube and Columns
into 3 rows.
b. Add 560 uL Lysis Buffer into 5.6 uL cRNA microcentrifuge tubes.
c. Add 140 uL specimen to the Lysis Buffer (Buffer AVL with RNA carrier), vortex for 15
seconds.
d. Incubate at Room Temperature (15-25oC) for 10 minutes.
e. Centrifuge for 10 seconds at 3000 rpm (2000 g) to remove drops from the lids.
f. Add 6 uL WNV Internal Control to each of the microcentrifuge tubes with Buffer AVL.
g. Add 560 uL ethanol (96-100%) to the samples, vortex for 15 seconds. Centrifuge for 10
seconds at 3000rpm (2000 g) to remove drops from the lids.
h. Pipette 630 uL (half the volume) of the mixture (specimen-lysis buffer-ethanol) to the
QIAamp spin column (in a 2 mL collection tube), close the cap and centrifuge at 8000 rpm
(6000 g) for 1 minute. Place the QIAamp spin column into a clean 2 mL collection tube and
discard the collection tube containing the filtrate.
i. Repeat Step (h) by pipeting the remaining 630 uL of the mixture to the QIAamp spin column
(in a 2 mL collection tube), close the cap and centrifuge at 8000rpm (6000 g) for 1 minute.
Place the QIAamp spin column into a clean 2 mL collection tube and discard the collection
tube containing the filtrate.
PROCEDURE MANUAL
UNIVERSITY HEALTH NETWORK / MOUNT SINAI HOSPITAL MICROBIOLOGY DEPARTMENT
NOTE: This is a CONTROLLED document. Any documents appearing in paper form that are not stamped in red "MASTER COPY" are not controlled and
should be checked against the document (titled as above) on the server prior to use
D:\106748206.doc
Policy # MI/MD/v50
Microbiology Department
Policy & Procedure Manual
Section: Molecular Diagnostic Tests Manual
Page 210 of
291
j. Open the spin column and add 500 uL of Buffer AW1. Close the cap and centrifuge at 8,000
rpm (6,000 g) for 1 minute.
k. Place the QIAamp spin column into a clean 2 mL collection tube and discard the collection
tube containing the filtrate.
l. Open the spin column and add 500 uL of Buffer AW2. Close the cap and centrifuge at full
speed 14,000 rpm (20,000g) for 3 minutes.
m. Place the spin column into a clean 2 mL collection tube and discard the collection tube
containing the filtrate. Centrifuge at 14,000 rpm (20,000g) for 3 min.
Elution Steps:
a. Place the spin column in the clean 1.5 mL microcentrifuge tube with the LIS specimen label.
Discard the collection tube containing the filtrate. Open the spin column and add 60 uL of
Elution Buffer (Buffer AVE). Close the caps and incubate at room temperature for 1 minute.
b. Centrifuge at 8000rpm (6000 g) for 1 min. Discard the spin column. Store the eluate at -20oC
or –70oC if not able to proceed immediately.
PROCEDURE MANUAL
UNIVERSITY HEALTH NETWORK / MOUNT SINAI HOSPITAL MICROBIOLOGY DEPARTMENT
NOTE: This is a CONTROLLED document. Any documents appearing in paper form that are not stamped in red "MASTER COPY" are not controlled and
should be checked against the document (titled as above) on the server prior to use
D:\106748206.doc
Policy # MI/MD/v50
Microbiology Department
Policy & Procedure Manual
Section: Molecular Diagnostic Tests Manual
Page 211 of
291
PCR Amplification and Detection Procedures:
PCR Set-up:
In the Clean Room: (Change into dedicated clean room gown and gloves, work in Biosafety Cabinet)
a. Take out the necessary number of WNV Master Mix A and B vials (24 tests per vial) from
the freezer and thoroughly thaw inside the Biosafety Cabinet. Determine the number of tests
and prepare the appropriate volume of Master Mix required according to the chart. Mix
gently, do not vortex. Make only enough master mix for the tests you are running. After
vial A has been added to Vial B it cannot be frozen again.
No. of samples
1
2
3
4
5
6
7
8
9
10
11
12
Preparation of Master Mix
Master A (µl)
5
10
15
20
25
30
35
40
45
50
55
60
Master B (µl)
20
40
60
80
100
120
140
160
180
200
220
240
b. Place a 1.5ml microcentrifuge tube for each purified sample, Positive control, external QC
and Negative control (H2O) into the Cooling Block (pre-cooled to 4oC).
c. Pipette 25 uL prepared Master Mix (A+B) into each micro tubes
d. Pipette 2.5 uL of internal control into the micro tubes designated for the Positive control and
water.
e. Pipette 25 uL water (PCR grade) into the negative control micro tube. Mix up and down 3X
and cap tightly. Label each microtube 1, 2, 3…. before leaving clean room.
f. Place the cooling block into a clean biohazard bag.
PROCEDURE MANUAL
UNIVERSITY HEALTH NETWORK / MOUNT SINAI HOSPITAL MICROBIOLOGY DEPARTMENT
NOTE: This is a CONTROLLED document. Any documents appearing in paper form that are not stamped in red "MASTER COPY" are not controlled and
should be checked against the document (titled as above) on the server prior to use
D:\106748206.doc
Policy # MI/MD/v50
Microbiology Department
Policy & Procedure Manual
Section: Molecular Diagnostic Tests Manual
Page 212 of
291
g. Change out of dedicated clean room gown.
In the Specimen Processing Room: (Change into specimen room gown)
a. Using a separate filter tip each time, carefully pipette 25 uL each of purified sample, Positive
controls, and external QC (if using) directly into the micro tubes. Mix by pipetting 3x up and
down into the mastermix. Immediately close the cap tightly.
b. Check each micro tube before loading. Make sure there is no bubble at the bottom of the
tube.
c. Load micro tubes into a proper rotor (36-well) and snap close the locking ring. Load the
rotor in Rotor-Gene 6000.
d. Always fill up the empty position of the rotor using empty tubes.
In the Rotorgene room:
a. Turn on computer, turn on Rotorgene;
b. FOR BLUE ROTORGENE ONLY. Choose clinical icon; pass word “msh”; press “→”
button;
c. Double click(left on the mouse) “Rotor-Gene 6000 series software 1.7” icon
d. Wait for “Initializing machine…..”
e. Highlight “ALTONA WNV” assay;
f. Press “New” button;
g. Highlighting the correct Rotor type you are using
h. 36-well (Red) or 72-well Rotor (Blue)
i. Tick the “Locking Ring Attached” option
j. Press “Next” button
k. Enter initials in operator space. Enter Master Mix lot. # In the Notes space and Rotogene used
(Blue or Red). Make sure the Reaction Volume is “50µl”;
l. Press “Next” button
m. Temperature profile window pops up, press “Next” button.
n. Make sure your ring has been loaded in the Rotorgene.
o. Summary window pops up, press “Start Run” button;
p. Save As window pops up; the run is given a filename with a default template. Change it
according to the date and numerical runs the assay performed on the same day; e.g. WNV
2010.03.29 (e.g. assay name-year-month-date-numerical run#);
q. Note:WNV results are stored in \desktop\My Document\WNV results.
r. Press Save button;
s. Machine starts and Edit Samples window pops up;
t. Enter sample LIS# including positive and negative controls. Define the type of samples
according to the chart:
PROCEDURE MANUAL
UNIVERSITY HEALTH NETWORK / MOUNT SINAI HOSPITAL MICROBIOLOGY DEPARTMENT
NOTE: This is a CONTROLLED document. Any documents appearing in paper form that are not stamped in red "MASTER COPY" are not controlled and
should be checked against the document (titled as above) on the server prior to use
D:\106748206.doc
Policy # MI/MD/v50
Microbiology Department
Policy & Procedure Manual
Section: Molecular Diagnostic Tests Manual
Name
Sample
Type
Unknown
Select
Yes
Positive Control
WNV
Positive Control
Yes
Water
NTC
Yes
Page 213 of
291
u. Press Finish button.
v. Once cycling screen comes on, click “Named On” button.
To analyze and print WNV report after a run is finished:
a. The run is done when Profile Program reads: Run has completed.
b. Analyze raw data by clicking on the each of these channels (one at a time): Green
channel (WNV) and Yellow channel (IC). These tabs are found on the second menu bar from
the top, on the left hand side.
c. Click on autoscale (bottom left). Click “All Off” (bottom right). Click “water” on. Compare
the specimen and control curves to the water one at a time (by clicking each sample on and
then off when proceeding to the next sample). A positive curve will have a sigmoidal shape.
A negative result will be a relatively flat line, like the water. Make a note of the positives on
the worklist.
d. Click on “Named On”
e. Perform curve analysis: Click Analysis on the top tool bar.
f. Analysis floating window pops up;
g. Choose “Quantitation” tab.
h. Quantitation window is brought up to the front. There should be two channels: Green
(WNV) and Yellow (IC).
i. Highlight Cycling A. Green (Page 1) (WNV) option and press Show button.
j. Maximize cycling green window (or the channel you are working on)
k. Highlight slope correct tab.
l. Click on Ignore first… tab. A window will pop-up, type in 5 (i.e. ignore 5 cycles).
m. Set threshold at 0.05. A threshold line will appear on the screen.
n. Move threshold line to above the noise (i.e. Negative specimens)
o. To Print reports: Press Reports button on the top toolbar.
Report Browser window pops up.
Choose Cycling A. Green (Page 1). Under templates box, choose “Quantitation full
report”.
Press Show button
Maximize the report window, check that only the positives that you have identified from
your raw data analysis are positive (i.e. have a crosspoint)
Choose print report. (for the red and yellow channels print only pages 2-4).
Once finished printing, close the report window
PROCEDURE MANUAL
UNIVERSITY HEALTH NETWORK / MOUNT SINAI HOSPITAL MICROBIOLOGY DEPARTMENT
NOTE: This is a CONTROLLED document. Any documents appearing in paper form that are not stamped in red "MASTER COPY" are not controlled and
should be checked against the document (titled as above) on the server prior to use
D:\106748206.doc
Policy # MI/MD/v50
Microbiology Department
Policy & Procedure Manual
Section: Molecular Diagnostic Tests Manual
Page 214 of
291
Go to the floating Analysis window;
p. Repeat the step from “e” to “m” for Cycling A. Yellow (internal control)
VI.
Reporting:
Green Channel
(WNV)
Yellow Channel
(IC specific)
Interpretations
+
+ or -
Preliminary report:
Positive for WNV:
Repeat assay to confirm* (Donor samples
should be repeated in duplicates)
If repeat is positive in the green channel,
report: Positive
If repeat is negative, consult
Senior/Charge on final report
-
+
Negative for WNV
Indeterminate
Test needs to be repeated. Sample may be
diluted 1:4 with lysis buffer
*Repeated specimen should be re-extracted from the original clot
Negative Report:
Negative for WNV
This is a research test.
WNV RT-PCR Kit v1.0.
Altona Diagnostics Inc. and RotorGene, ?Corbett Life Sciences
Indeterminate Report: Indeterminate by RT-PCR
This is a research test.
WNV RT-PCR Kit v1.0.
Altona Diagnostics Inc. and RotorGene, Corbett Life Sciences
Positive Report:
POSITIVE for WNV
This is a research test.
WNV RT-PCR Kit v1.0.
Altona Diagnostics Inc. and RotorGene, Corbett Life Sciences
Record CT value in media PCWNV
Notify Senior/Charge Technologist/Microbiologist on positive WNV results
Notify Medical Officer of Health on positive WNV results
PROCEDURE MANUAL
UNIVERSITY HEALTH NETWORK / MOUNT SINAI HOSPITAL MICROBIOLOGY DEPARTMENT
NOTE: This is a CONTROLLED document. Any documents appearing in paper form that are not stamped in red "MASTER COPY" are not controlled and
should be checked against the document (titled as above) on the server prior to use
D:\106748206.doc
Policy # MI/MD/v50
Microbiology Department
Policy & Procedure Manual
Section: Molecular Diagnostic Tests Manual
Page 215 of
291
Shut down computer:
a. Exit from software. A pop-up window will appear “save changes”. Click “yes”.
b. Click “start” button. Click “Turn off computer”.
c. Turn off Rotorgene
At the end of the day, follow the cleaning protocol below using 1% hypochorite or Eliminase followed
by 70% alcohol:
Clean Room:
Clean Biological Safety Cabinet
Specimen Preparation Room:
Clean Biological Safety Cabinet, pippettors, centrifuge, and bench top.
Cap discard container.
Wash racks.
Amplification Room:
Discard micro tubes into a disposal bag and close the bag.
Discard the bag into biohazard waster container.
Perform the cleaning procedure according the daily maintenance sheet.
VII.
Quality Control
Reagent QCs:
Before every lot change of isolation and/or master mix kit:
An External Control (external to Altona Diagnostics) is used to monitor the isolation,
amplification and detection procedures. The result must correspond to expected value
supplied by the manufacturer.
Before every lot change of master mix kit:
Daily QCs:
Every run:
Each patient specimen must have an Internal Control (IC) added to monitor both isolation
and PCR inhibition.
A Positive Control is included and shows a positive reading in Green Channel (WNV)
A Negative Control is include and shows a negative reading in Green Channel (WNV)
Report all failed QCs to senior/charge technologist.
PROCEDURE MANUAL
UNIVERSITY HEALTH NETWORK / MOUNT SINAI HOSPITAL MICROBIOLOGY DEPARTMENT
NOTE: This is a CONTROLLED document. Any documents appearing in paper form that are not stamped in red "MASTER COPY" are not controlled and
should be checked against the document (titled as above) on the server prior to use
D:\106748206.doc
Policy # MI/MD/v50
Microbiology Department
Policy & Procedure Manual
Section: Molecular Diagnostic Tests Manual
Page 216 of
291
Failed QC:
Test is invalid without satisfactory QC results.
a. Do not release results pending resolution of QC failure.
b. Inform charge/senior technologist.
c. Record in Reagent Log Chart, Instrument Maintenance Log or Incident Report where
appropriate.
d. If the QC failure was due to a simple matter of position reversal or misplacement, the run can
be released (positive QC material yielded positive result, negative yielded negative result).
e. If positive QC material yielded negative result, repeat the entire run.
f. If negative QC material yielded positive result, it may be due to cross-contamination from
adjacent positive sample within the run or carry-over contamination from previous runs via
equipment or the environment. Review procedure and equipment to establish and eliminate
potential sources of contamination.
g. The extent and nature of contamination can also be evaluated by comparing the positive rate
of the run with its expected positive rate.
h. If the contamination is extensive, it is necessary to quarantine/discard potentially
contaminated reagents and consumables and disinfect equipment and environment before
repeating the run.
i. If a carry-over contamination is suspected (e.g. two or more runs with negative QC being
positive or patient samples have higher than expected positive rate and these samples are
often non-repeatable positives), it is necessary to have a thorough environmental disinfection
followed by swabbing to monitor.
j. Successful ending to a carry-over contamination may be indicated by QC results and patient
positivity rate falling back to the expected normal range and three negative environmental
swabs.
ROTORGENE QC:
Semi-Annual:
Perform optical temperature verification (See Appendix - Rotorgene Optical
Temperature Verification (OTV) Procedure)
VI.
References:
QIAamp Viral RNA Mini Kit Handbook 01/99, Qiagen
WNV RT-PCR Kit 1.2 User Manual, Altona Diagnostics, 22767 Hamburg, Germany
PROCEDURE MANUAL
UNIVERSITY HEALTH NETWORK / MOUNT SINAI HOSPITAL MICROBIOLOGY DEPARTMENT
NOTE: This is a CONTROLLED document. Any documents appearing in paper form that are not stamped in red "MASTER COPY" are not controlled and
should be checked against the document (titled as above) on the server prior to use
D:\106748206.doc
Policy # MI/MD/v50
Microbiology Department
Policy & Procedure Manual
Section: Molecular Diagnostic Tests Manual
Page 217 of
291
West Nile Virus Donor Screen NAT PCR by Cobas® s201 Ampliprep/TaqMan
I.
Introduction
West Nile Virus is a member of the Flaviviridiae family, the genus Flavivirus and the Japanese
encephalitis virus serocomplex. Viruses in this complex are arboviruses with the potential to
cause meningitis, encephalitis and meningoencephalitis.
The Cobas® TaqScreen West Nile Virus Test is a qualitative test that enables the screening and
detection of WNV RNA in infected pooled and individual specimen donations. The Cobas®
TaqScreen West Nile Virus Test uses a generic nucleic acid preparation technique on the
Cobas® Am;liPrep Instument. WNV test incorporates an Internal control for monitoring test
performance in each individual test as well as the AmpErase enzyme to reduce potential
contamination by previously amplified material (amplicon).
II.
Specimen Collection and Storage
Living donor specimen:
Blood collected in EDTA may be stored in one of two conditions:
For condition 1, blood may be stored for up to 24 hours at 2-30 oC, followed by 24 hours
at 2-25 oC, followed by 72 hours at 2-8 oC, prior to plasma separation. For storage longer
than five days, separate the plasma from the red blood cells by centrifugation at 8001,600 x g for 20 minutes. Following removal, plasma my be stored at 2-8 for seven days,
followed by up to 30 days at ≤-20 oC
For condition 2, blood may be stored for up to 72 hours at 2-25 oC, followed by 48 hours
at 2-8 oC, prior to plasma separation. For storage longer than five days, separate the
plasma from the red blood cells by centrifugation at 800-1,600 x g for 20 minutes.
Following removal, plasma my be stored at 2-8 for seven days, followed by up to 30 days
at ≤-20 oC
EDTA plasma can be frozen and thawed a maximum of three(3) times
Cadaveric blood specimen-EDTA plasma or serum may be used
Cadaveric blood specimens collected in EDTA may be stored for up to 24 hours at 225oC, prior to plasma separation. For storage long than one day, separate the plasma from
the red blood cells by centrifugation at 800-1,600 x g for 20 minutes. Following removal,
plasma may be stored at 2-8oC for an additional seven days. Alternatively, plasma my be
stored at ≤18 oC for up 30 days. Cadaveric EDTA plasma can be frozen and thawed a
miximum of three (3) times.
Cadaveric blood collected as serum may be stored for up to 24 hours at 2-8 oC, prior to
separation. For storage longer than one day, separate the serum from the clot by
centrifugation at 800-1,600 x g for 20 minutes. Following removal, serum specimens may
PROCEDURE MANUAL
UNIVERSITY HEALTH NETWORK / MOUNT SINAI HOSPITAL MICROBIOLOGY DEPARTMENT
NOTE: This is a CONTROLLED document. Any documents appearing in paper form that are not stamped in red "MASTER COPY" are not controlled and
should be checked against the document (titled as above) on the server prior to use
D:\106748206.doc
Policy # MI/MD/v50
Microbiology Department
Policy & Procedure Manual
Section: Molecular Diagnostic Tests Manual
Page 218 of
291
be stored for up to three days at 2-8 oC. Alternatively, in the case of serum removed from
the clot, moderately hemolyzed cadaveric serum specimens may be stored at ≤18 oC for
up 15 days and highly hemolyzed cadaveric serum specimens may be stored at at ≤18 oC
for up 8 days.Cadaveric serum specimens can be frozen and thawed a mximum of three
(3) times.
Cadaveric plasma or serum is tested at 1:5 dilution.
!Do not freeze whole blood
!Heparin Plasma is NOT acceptable
Donor Serology and Molecular Testing Specimen Storage
III.
Materials, Equipments and Facilities
Reagents:
1. Cobas® TaqScreen WNV Test (CS1-CS4) stored at 2-8 oC
magnetic glass particles reagent cassette
lysis reagent cassette
Multi-reagent cassette
Test-specific reagent cassette
2. Cobas® TaqScreen MPX/WNV Control Kit stored at 2-8 oC
WNV negative control
WNV positive control
3. Cobas® TaqScreen Wash Reagent stored at 15-30 oC
4. Cobas® TaqScreen Cadaveric Specimen Diluents:
Unopened CADV SPEC DIL is table until the expiration date.
Once opened, this reagent is stable for 30 days at 2-8 oC or until the expiration date,
whichever comes first.
Equipment:
Hamilton MICROLAB STAR/STARlet IVD Pipettor
Cobas® Ampliprep Instrument
Cobas® Taqman Analyzer
Pooling, AMPLILINK and Data Management Workstation, Data Station
Pipette tips (high volume CO-RE tips (1000mL), filter
Waste bags
Sample Input tubes (S-tubes) and barcode clips
24 and 32 test tube sample carrier
Plate carrier
PROCEDURE MANUAL
UNIVERSITY HEALTH NETWORK / MOUNT SINAI HOSPITAL MICROBIOLOGY DEPARTMENT
NOTE: This is a CONTROLLED document. Any documents appearing in paper form that are not stamped in red "MASTER COPY" are not controlled and
should be checked against the document (titled as above) on the server prior to use
D:\106748206.doc
Policy # MI/MD/v50
Microbiology Department
Policy & Procedure Manual
Section: Molecular Diagnostic Tests Manual
IV.
Page 219 of
291
Tip carrier
Sample Racks (SK24)
SK24 Rack Carrier
SPUs
SPU racks
Reagent Racks
Racks of K-tips
K-tubes
BD Vacutainer
Procedure
1. Take out WNV reagent kits and controls from the fridge, and leave at room temperature.
2. If Hamilton STAR was off during the weekend, turn on Hamilton STAR at least 1 minute before
turn on the computer!
3. Re-start computers for Pooling Manager, and Data Manager every week day.
4. Perform daily maintenance procedures for HAMILTON and AMPLIPREP.
5. Use Pooling Manager Terminal for the maintenance of Hamilton:
a. Click Wizard icon
b. Click Maintenance Tab
c. Click Daily Maintenance
d. Click Start
e. Follow instructions to finish daily maintenance procedure
Perform weekly maintenance every Tuesday.
!Push Back Up tape into driver every Tuesday morning after the weekly maintenance
Turn off Hamilton STAR and computer at the end of the Friday!
* Do not touch the red scanner
* Clean inside of HAMILTON with de-ionized water and 70%alcohol
* Clean the pipette ejector ledge with alcohol
6. Loading of reagents and disposables in AmpliPrep
a. Loading of Reagent Cassettes in AmpliPrep
Place all CS1 for WNV onto a same reagent cassette
Place CS2, CS3, CS4 for WNV onto to a separate reagent cassettes
Load the reagent cassette containing all CS1 onto position A of the AmpliPrep
PROCEDURE MANUAL
UNIVERSITY HEALTH NETWORK / MOUNT SINAI HOSPITAL MICROBIOLOGY DEPARTMENT
NOTE: This is a CONTROLLED document. Any documents appearing in paper form that are not stamped in red "MASTER COPY" are not controlled and
should be checked against the document (titled as above) on the server prior to use
D:\106748206.doc
Policy # MI/MD/v50
Microbiology Department
Policy & Procedure Manual
Section: Molecular Diagnostic Tests Manual
Page 220 of
291
Load the reagent cassettes containing CS2, CS3, CS4 onto position B,C,D or E of the
AMPLIPREP
b. Loading of Disposables in AmpliPrep
Load enough SPUs in the SPU rack(s) and load the rack(s) onto position J, K or L of the
AmpliPrep.
Load enough K-tubes onto position M-N of the AmpliPrep.
Load enough K-tips onto position O-P of the AmpliPrep.
! Do NOT unload any partial rack of K-tube or K-tips even the LEDs are green
! Position M-N are designated for K-tubes, position O-P are designated for K-tips.
7. Prepare Sample rack and S-tube rack
8. Using the Work list, match labels of sample tube with the 6mL BD Vacutainer tube
a. Add 1200ul plasma of Living Donor samples to the empty 6mL BD Vacutainer tubes
b. Add 300ul plasma/serum Cadaveric samples to the 6mL BD Vacutainer tube with 1200
uL Cadaveric diluent
c. Centrifuge at 3000 rpm for 5-10 minutes
! Make sure the sample tube is free of bubbles, clots and flocculates.
d. De-cap and place 6mL BD Vacutainer tubes onto 32 test tube sample carrier
e. Take out enough clips and S-tubes (4 controls plus the sample number)
f. Slightly bend the clip before place it onto the S-tubes rack starting position#1
g. Place S-tubes into clips
h. Place S-tube rack onto SK24 Rack Carrier
i. De-cap S-tubes
9. Set up MPX NEGATIVE CONTROL and POSITIVE CONTROL racks
!!!Mix controls by inversion at least 3 times, avoiding the creation of bubbles, as
specified below:
Inversion each time is defined as turning the control upside down and right side
up again
Within inversion each time, hold the control for at least 2 seconds in each
orientation (i.e. turn the control upside down, and hold for at least 2 seconds.
Then, turn the control right side up again, and hold for at least 2 seconds
a. Place clean Kleenex paper on Control Working Area
b. Remove positive control lids and leave on Kleenex paper.
c. Load positive controls in Positive Control Rack Position #1, 2, and 3 with barcode labels
visible.
Yellow cap positive control is in position#1
Orange cap positive control is in position#2
Red cap positive control is in position#3
CHANGE GLOVES AFTER SETTING UP POSITIVE CONTROL RACK
d. Load negative control in negative Control Rack Position #1 with barcode label visible.
PROCEDURE MANUAL
UNIVERSITY HEALTH NETWORK / MOUNT SINAI HOSPITAL MICROBIOLOGY DEPARTMENT
NOTE: This is a CONTROLLED document. Any documents appearing in paper form that are not stamped in red "MASTER COPY" are not controlled and
should be checked against the document (titled as above) on the server prior to use
D:\106748206.doc
Policy # MI/MD/v50
Microbiology Department
Policy & Procedure Manual
Section: Molecular Diagnostic Tests Manual
Page 221 of
291
! Pop bubbles from control tubes by lightly tapping with control tube cover
! Return Control boxes back to fridge after finish loading.
10. Pooling Manager Terminal
a. Click Wizard Icon
b. Make sure Batch Run is selected
c. Click Assay/Start
d. Choose WNV
e. Click Next
f. Click Pools of 1
g. Follow the instruction to load sample rack
h. Click Done button after all samples are loaded
i. All required quantities of S-Tubes,SK24 racks,tips, RMEC (roche manufactured external
controls) are calculated
j. Follow instructions to load S-tube rack, control racks, and pipette tip rack.
k. After tips are loaded, pipetting is automatically started
l. All racks are automatically unloaded after the pooling procedure is finished
m. Re-cap the S-tubes .Double check that caps are not so tight and properly placed
n. Press the ‘ctrl’ on the keyboard + the ‘logoff’ button on the lower right corner of the
pooling wizard to exit the pooling wizard
o. To start a new pooling run, click pooling wizard and click tab Batch Run
p. If window is freeze, press Ctrl key and Logoff icon at the same time to active the
windows
11. Extraction/Amplification/Detection
AMPLIPREP USER ID: MSH
PASSWORD: Msh12345
Load in AMPLIPREP – AMPLIPREP Terminal
!NO order needs to be manually created. The order is automatically
transmitted from Pooling manager to Ampliprep
a. In the Amplilink computer, click order icon to check if the order is send to Amliprep.
If the order is not sent over, proceed the procedure of Synchronize Hamilton with
Amliprep
b. Remove S-tube rack from carrier. Load S- tube rack in AMPLIPREP
(Start with Track F), check the End time (Time to transfer k-tubes to Taqman)
c. Load only FULL K-tube / K-tip rack when required.
d. When the run is complete, the indicator light on the Cobas® Ampliprep will be
orange, and SK24 racks may be removed.
12. Load the SK24 racks directly to the Cobas® TaqMan.
13. If the Amplification and detection run does not start automatically, click Start
14. Check finished time.
15. When testing is finished in Cobas® TaqMan , the results are automatically transmitted to
Data Manager.
PROCEDURE MANUAL
UNIVERSITY HEALTH NETWORK / MOUNT SINAI HOSPITAL MICROBIOLOGY DEPARTMENT
NOTE: This is a CONTROLLED document. Any documents appearing in paper form that are not stamped in red "MASTER COPY" are not controlled and
should be checked against the document (titled as above) on the server prior to use
D:\106748206.doc
Policy # MI/MD/v50
Microbiology Department
Policy & Procedure Manual
Section: Molecular Diagnostic Tests Manual
Page 222 of
291
!DO NOT NEED TO MANULLY ACCEPT RESULTS FROM Cobas® TaqMan
16. Print Results from Data Manager (follow instructions) Print Donor Result Report only
a. DMS
b. Query Tab
c. Today
d. Search
e. Highlight batch, Next
f. Confirm any information in Alarm Review
g. Donor Review Tab,
h. Print
If all sample tests are negative, only check Donor Result Report
If there is positive result for patient’s sample, check both PCR Batch Report
and Donor Result Report
17. Report results in LIS manually.
18. Clean Up and Shutdown Procedures
a. Check number of reagents left and write in CS1 then cover with parafilm and store in
fridge.
b. Discard used SPU tubes and save clean ones.
V.
Synchronize Hamilton with Ampliprep
VI.
Click Pooling icon
Click Amplilink Status tab
Under Amplilink workstation, click PCR-LAB-W1-220
Under Current Batches, click the Rack ID
Click Synchronize button
Assay Validation
All controls have to be valid before specimen results are released.
All result data are stored in main frame computer HPR 300XR in Rm 1438.
VII.
Interpretatiion of Results
If all controls are valid:
Non Reactive: reported as Negative
Reactive: reported as Positive.
Invalid Result: repeat test once. If still invalid, reported as Indeterminate
PROCEDURE MANUAL
UNIVERSITY HEALTH NETWORK / MOUNT SINAI HOSPITAL MICROBIOLOGY DEPARTMENT
NOTE: This is a CONTROLLED document. Any documents appearing in paper form that are not stamped in red "MASTER COPY" are not controlled and
should be checked against the document (titled as above) on the server prior to use
D:\106748206.doc
Policy # MI/MD/v50
Microbiology Department
Policy & Procedure Manual
Section: Molecular Diagnostic Tests Manual
Page 223 of
291
VIII. Reporting
For Negative Result
Result
NonReactive
NonReactive
CT Values
WNV│IC
─ │###
─ │─
Internal
Control
Valid
Report
Comment
8WNVR:Negative@RWNv
Verify 8WNVR
If there is enough sample for
repeating, repeat the test
Order 8COM to record initial
invalid result
After repeating, if the IC is still
invalid, result as following:
8WNVR: Indeterminate@RWNv
Verify 8WNVR
In the comment
for 8COM,
record the 2nd
result
Verify 8COM
If there is not enough sample for
repeating, result as following:
8WNVR: Indeterminate@ RWNv
In the comment for 8WNVR, type:
Not Sufficient Quantity for
repeating
Verify 8WNVR
Verify 8COM
Invalid
For Positive Result
Result
CT Values
Internal Control
WNV│IC
Reactive
─ │###
Valid
Repeat in
Duplicate
YES
Report
Living Donor??
Cadaveric Donor:
a. 2/3 Positive8WNVR:Positive@ RWNv
Order 8COM in LIS and record all CT
b. 2/3 Negative8WNVR:Negative@ RWNv
Order 8COM in LIS and record all results
PROCEDURE MANUAL
UNIVERSITY HEALTH NETWORK / MOUNT SINAI HOSPITAL MICROBIOLOGY DEPARTMENT
NOTE: This is a CONTROLLED document. Any documents appearing in paper form that are not stamped in red "MASTER COPY" are not controlled and
should be checked against the document (titled as above) on the server prior to use
D:\106748206.doc
Policy # MI/MD/v50
Microbiology Department
Policy & Procedure Manual
Section: Molecular Diagnostic Tests Manual
IX.
Trouble Shooting:
Problem
Internal Control fails
on ONE specimen
Internal Control fails
on a specimen for the
second time
Pooling manager
computer is frozen
while loading
specimen
X.
Page 224 of
291
Solutions
Repeat specimen
Result specimen as: Invalid
In result comment: hit F5 to add comment “@SPIN”
“Likely due to specimen integrity, unable to obtain
valid test result after repeated attempts)”.
Verify result.
1 Press Ctrl key and Logoff icon at the same time to
active the windows
2. If computer is still frozen, press Ctrl+Alt+Del to
restart the pooling manager computer
3. If the computer is still frozen, turned off the Hamilton
STAR and computer
4. Manually unload the specimens from the Hamilton
STAR
5. Wait for couple of minutes, turn back the Hamilton
STAR at least 1 minute before turn on the computer
6. Wait for the log on screen before pressing
Ctrl+Alt+Del to log in
7. Restart the pooling procedure
Quality Control :
Run External Positive and negative control (previously tested CAP proficiency samples)
monthly.
XI.
CAP and NML provide external proficiency testing.
Reference:
Roche cobas s 201 System
Hardware and Software reference Manual, P/N 05575982190-01.
PDM Software Software Guide,P/N 05575974190-01.
Operator’s Manual for Use with small Pools(Pools of 1 and 6) P/N 05576008190-01
Roche Hot Line Tel# 877-273-3433
michael.salem@roche.com
xinyu.song@roche.com
PROCEDURE MANUAL
UNIVERSITY HEALTH NETWORK / MOUNT SINAI HOSPITAL MICROBIOLOGY DEPARTMENT
NOTE: This is a CONTROLLED document. Any documents appearing in paper form that are not stamped in red "MASTER COPY" are not controlled and
should be checked against the document (titled as above) on the server prior to use
D:\106748206.doc
Policy # MI/MD/v50
Microbiology Department
Policy & Procedure Manual
Section: Molecular Diagnostic Tests Manual
Page 225 of
291
APPENDIX I - Molecular Diagnostic Tests Schedule
BK Virus PCR………………………………………………………………………………...…….weekly
Chlamydia trachomatis and Neisseria gonorrhoeae PCR …………………………………………weekly
Clostridium difficile toxin B gene PCR ……………………………………………………………..hourly
Cytomegalovirus Quantitative PCR ………………………………………………….……………….daily
Cytomegalovirus Qualitative PCR ………………………………………..………….……………….daily
Epstein Barr Virus PCR. ……………………………………………...……………………………weekly
Enterovirus RNA PCR …………………………………………………………………………....weekly*
Hepatitis B/Hepatitis C/HIV Donor Screen NAT PCR………………………………………..…….daily*
Herpes simplex Virus/Varicella-Zoster Virus PCR …………………………………………...…….daily*
Human Papilloma Virus PCR …………………………..………………………………………..biweekly
Influenza A/B & RSV PCR …………………………………………………………………...…….hourly
Parvovirus B19 PCR …………………………………………………………………...…………..weekly
West Nile Virus PCR ……………………………………………………………………………as needed
West Nile Virus Donor Screen NAT PCR ……………………………………………………….….daily*
*
Stat testing may be required where clinically justified.
PROCEDURE MANUAL
UNIVERSITY HEALTH NETWORK / MOUNT SINAI HOSPITAL MICROBIOLOGY DEPARTMENT
NOTE: This is a CONTROLLED document. Any documents appearing in paper form that are not stamped in red "MASTER COPY" are not controlled and
should be checked against the document (titled as above) on the server prior to use
D:\106748206.doc
Policy # MI/MD/v50
Microbiology Department
Policy & Procedure Manual
Section: Molecular Diagnostic Tests Manual
Page 226 of
291
APPENDIX II - Nucleic Acid Extraction –Biomerieux NucliSENS easyMAG
I.
Introduction
The NucliSENS easyMAG is an automated platform for the isolation (purification and
concentration) of total nucleic acids (RNA/DNA) from biological specimens. Used for batch
processing of 1-24 samples.
The nucleic extraction method is based on Boom Chemistry using magnetic silica particles. Briefly,
under high salt conditions, nucleic acid will bind to the silica particles. These silica particles act as
solid phase and non-nucleic acid components are removed by several washing steps performed in the
NucliSENS easyMAG instrument. Next, nucleic acids are eluded from the silica particles and the
silica particles are removed from the extracted specimens by the NucliSENS easyMAG
instrument.the resulting eluate contains purified and concentrated total nucleic acids.
II.
Specimens Types
Plasma (minimum 200uL) collected in EDTA tube and separated by centrifugation; 3000rpm for 10
minutes. Do not test plasma collected in heparin tubes.
CSF, sterile body fluids (amniotic fluid, vitreous fluid), Urine, BAL
Viral transport media (VTM) from swabs collected in VTM and vortexed on high for 10 seconds.
III.
Materials, Equipments
NucliSENS easyMAG
NucliSENS easyMAG extraction products:
NucliSENS Lysis Buffer
NucliSENS easyMAG Lysis Buffer
NucliSENS easyMAG Magnetic Silica
NucliSENS easyMAG Extraction Buffer 1
NucliSENS easyMAG Extraction Buffer 2
NucliSENS easyMAG Extraction Buffer 3
NucliSENS easyMAG Disposables –vessels and pipettes
BioHit Multichannel pipettor
Ranin 1000uL, 100ul, 20ul Pipettors
Aerosol Resistant Tips (ART) 1000ul, 200ul, 20ul
Powder-free gloves
Internal controls (for CMV, HSV, BKV, Parvovirus B19, VZ, Enterovirus)
PROCEDURE MANUAL
UNIVERSITY HEALTH NETWORK / MOUNT SINAI HOSPITAL MICROBIOLOGY DEPARTMENT
NOTE: This is a CONTROLLED document. Any documents appearing in paper form that are not stamped in red "MASTER COPY" are not controlled and
should be checked against the document (titled as above) on the server prior to use
D:\106748206.doc
Policy # MI/MD/v50
Microbiology Department
Policy & Procedure Manual
Section: Molecular Diagnostic Tests Manual
Page 227 of
291
GENERAL PRECAUTIONS:
Do not allow the NucliSENS easyMAG Lysis Buffer, NucliSENS easyMAG Extraction Buffer 1 or
waste from the instrument to come in contact with acidic materials.
Certain reagents contain guanidine thiocyanate.
Buffers containing guanidine thiocyanate MUST NOT be mixed with cleaning solutions containing
bleach. Liquid waste from extractions procedures contain guanidine thiocynate MUST NOT be mixed
with other laboratory waste. Proper waste disposal is required.
IV.
Procedure
1.
Turn ON easyMAG. Wait for orange light to turn GREEN, then switch ON the easyMAG
computer.
2.
Perform and record easyMAG Daily Maintence:
Inspect drip tray.
Inspect reagent cap filters.
Inspect carbon filter.
Empty & rinse waste bottle with water.
3.
easyMAG
4.
Click on “reagent” icon
5.
Scan reagent stand and scan reagent bottle for all four reagents (A, B, C, D).
6.
Click on “Sample” icon
Login name: bmx
Password: bmx
For BKV/CMV/HSV/VZV/PARVO/ENTERO/
Enter Protocol: Generic 2.0.1
Enter Matrix: Plasma or “other” for urine & BAL, CSF for CSF
Enter Volume (mL): 0.200
Eluate (uL): 50
PROCEDURE MANUAL
UNIVERSITY HEALTH NETWORK / MOUNT SINAI HOSPITAL MICROBIOLOGY DEPARTMENT
NOTE: This is a CONTROLLED document. Any documents appearing in paper form that are not stamped in red "MASTER COPY" are not controlled and
should be checked against the document (titled as above) on the server prior to use
D:\106748206.doc
Policy # MI/MD/v50
Microbiology Department
Policy & Procedure Manual
Section: Molecular Diagnostic Tests Manual
7.
Click on sample ID bar and scan specimen barcodes.
8.
Click on “organize run” icon
9.
Click on “create run” icon
10.
A box will appear with today’s date and run #. Click on OK.
11.
Click on
12.
Click on “load run” icon
Page 228 of
291
to transfer all scanned items onto the worklist.
PROCEDURE MANUAL
UNIVERSITY HEALTH NETWORK / MOUNT SINAI HOSPITAL MICROBIOLOGY DEPARTMENT
NOTE: This is a CONTROLLED document. Any documents appearing in paper form that are not stamped in red "MASTER COPY" are not controlled and
should be checked against the document (titled as above) on the server prior to use
D:\106748206.doc
Policy # MI/MD/v50
Microbiology Department
Policy & Procedure Manual
Section: Molecular Diagnostic Tests Manual
13.
14.
Page 229 of
291
To identify vessels, click on vessel icon
Scan position A barcode and then vessel barcode for first 8 samples, continue with position B
and C depending on how many samples you have.
15.
Click on the silica icon
16.
Scan in silica barcode from top of silica box.
17.
Highlight all samples by touching screen or with mouse.
18.
To apply silica barcode to all samples click on “downward arrow” icon
19.
Click on the “progress tab”
20.
Print worklist. Select printer icon on right hand vertical menu bar. Pop-up appears, click OK.
Sign your initials beside “Operater”.
21.
Click on the “dispense lysis icon”
>>>>
on third menu bar from top.
PROCEDURE MANUAL
UNIVERSITY HEALTH NETWORK / MOUNT SINAI HOSPITAL MICROBIOLOGY DEPARTMENT
NOTE: This is a CONTROLLED document. Any documents appearing in paper form that are not stamped in red "MASTER COPY" are not controlled and
should be checked against the document (titled as above) on the server prior to use
D:\106748206.doc
Policy # MI/MD/v50
Microbiology Department
Policy & Procedure Manual
Section: Molecular Diagnostic Tests Manual
Page 230 of
291
22.
Once the lysis buffer has been dispensed, remove vessels form easyMag and put them in rack
and take them to the BSC.
23.
For CMV/BKV/HSV/VZV/PARVO/ENTERO, add 200 uL to the lysis buffer.
Mix by pipetting up and down three times.
24.
Vortex internal control (IC).
For CMV/BKV/HSV/VZV/PARVO/ENTERO add 5 uL IC.
Mix up and down three times.
25.
Incubate at room temperature for 10 minutes.
26.
To make silica premix add 550 uL PCR grade water to silica (program 1 of pipette)
27.
Vortex silica premix before dispensing.
28.
Dispense 125 uL silica into Elisa strip (program 2 of pipette)
29.
After the 10 incubation period add 100 uL silica premix to vessel (program 3 of pipette)
30.
Reload vessels into the easyMAG.
31.
Scan position barcode and then vessel barcode (make sure the vessel icon is highlighted).
32.
Click on start icon
on right hand vertical menu bar.
A pop-up box will appear asking if you have added the premix silica, click YES.
33.
Once the samples have been eluted, transfer the eluate from the vessels to labeled microtube. Set
pipette at 55uL to remove all of the eluate.
34. If elutes are to be tested same day store eluates at 4C. If PCR testing is to be performed at a later
date, store eluate at -20oC as soon as possible.
35. A printout with reagent lot numbers must be printed at the end of the run.
- When the extraction is complete, click on the magnifying glass icon.
- Select your run from the list on the left. Make sure it is highlighted.
- Click on the printer icon, print pages 1 of 1 only.
- A pop up will appear “The run results are being printed. Mark this run ASSESSED?”. Click YES
to this and the document will print.
- File this with the corresponding tasklist printed at the beginning of the procedure.
PROCEDURE MANUAL
UNIVERSITY HEALTH NETWORK / MOUNT SINAI HOSPITAL MICROBIOLOGY DEPARTMENT
NOTE: This is a CONTROLLED document. Any documents appearing in paper form that are not stamped in red "MASTER COPY" are not controlled and
should be checked against the document (titled as above) on the server prior to use
D:\106748206.doc
Policy # MI/MD/v50
Microbiology Department
Policy & Procedure Manual
Section: Molecular Diagnostic Tests Manual
Page 231 of
291
DAILY CLEAN UP:
1.
Remove consumables from easyMAG, bag them and discard in biohazard waste box.
2.
Clean easyMAG according to maintenance worksheet and record maintenance on worksheet.
3.
To shut down easyMAG computer:
Click on bmx key on the bottom menu bar.
Click on “quit” in the pop-up box.
4.
Wait 10 minutes after the easyMAG Computer is OFF before switching off the easyMAG.
TO EMPTY WASTE: as required maximum 1/3 full
1. Go to reagent icon.
(If reagent icon is not on the screen, then click on machine icon
and click on reagent icon.)
2. Click on icon with droplet picture
(top icon on right vertical bar)
3. Empty waste in media room fume hood.
The Waste container should be labeled with the “Start date” and “contains guanidine
thiocyanate”. Empty any remaining buffer from easyMAG Lysis Buffer and easyMAG
Extraction Buffer1 into the fume hood waste container. Move the waste container to the 6th
floor outside the Autopsy Suite for disposal every Tuesday afternoon. Discard these empty
plastic containers (Lysis Buffer & Extraction Buffer 1) into the biohazard box.
Extraction buffer 2 and Extraction buffer 3 can be discarded in the sink and bottles can be
rinsed and recycled.
4. Rinse easyMAG waste container with water and return to easyMag.
PROCEDURE MANUAL
UNIVERSITY HEALTH NETWORK / MOUNT SINAI HOSPITAL MICROBIOLOGY DEPARTMENT
NOTE: This is a CONTROLLED document. Any documents appearing in paper form that are not stamped in red "MASTER COPY" are not controlled and
should be checked against the document (titled as above) on the server prior to use
D:\106748206.doc
Policy # MI/MD/v50
Microbiology Department
Policy & Procedure Manual
Section: Molecular Diagnostic Tests Manual
Page 232 of
291
5. Click “I confirm that the waste container is empty. A check mark should appear in that box.
6. Press OK.
WEEKLY MAINTENANCE:
Clean Dispense Probe on the EasyMag
1.
Click on maintenance icon
.
2.
Put in empty vessels and pipettes.
3.
Choose start from vertical side bar menu
To file runs that has been completed.
V.
Choose the magnifying glass (second menu bar from the top)
Highlight the runs you wish to file.
Choose the filing cabinet (right menu bar).
Quality Control
Failed extraction runs, should be reviewed with senior and/or Charge technologist to establish causes
and corrective actions; repeating extraction run maybe necessary.
If the easyMag system becomes inoperable call Biomerieux technical support phone number, provided
on each easyMag.
External controls are extracted on the easyMag according to schedule in the table below.
PROCEDURE MANUAL
UNIVERSITY HEALTH NETWORK / MOUNT SINAI HOSPITAL MICROBIOLOGY DEPARTMENT
NOTE: This is a CONTROLLED document. Any documents appearing in paper form that are not stamped in red "MASTER COPY" are not controlled and
should be checked against the document (titled as above) on the server prior to use
D:\106748206.doc
Policy # MI/MD/v50
Microbiology Department
Policy & Procedure Manual
Section: Molecular Diagnostic Tests Manual
Analyte/target
BKV
HSV1 & 2
External control
High positive and Low
Positive
High positive and Low
positive
High positive and Low
Positive
Positive control
VZV
Positive control
H1N1
Positive control
Influenza A
Positive control
Influenza B
Positive control
RSV A
Positive control
RSV B
Positive control
Parvovirus B19
Positive control
Enterovirus
Positive control
CMV
EBV
VI.
Page 233 of
291
Extraction schedule
Each day when test is done
(once/week)
Each day when quant. test is
done (weekdays)
Each day when quant. test is
done
Once a month and/or with
each new lot
Once a month and/or with
each new lot
Once a month and/or with
each new lot
Once a month and/or with
each new lot
Once a month and/or with
each new lot
Once a month and/or with
each new lot
Once a month and/or with
each new lot
Once a month and/or with
each new lot
Once a month and/or with
each new lot
References
NucliSENS easyMAG User Manual v2.0 ref: 280163
PROCEDURE MANUAL
UNIVERSITY HEALTH NETWORK / MOUNT SINAI HOSPITAL MICROBIOLOGY DEPARTMENT
NOTE: This is a CONTROLLED document. Any documents appearing in paper form that are not stamped in red "MASTER COPY" are not controlled and
should be checked against the document (titled as above) on the server prior to use
D:\106748206.doc
Policy # MI/MD/v50
Microbiology Department
Policy & Procedure Manual
Section: Molecular Diagnostic Tests Manual
Page 234 of
291
APPENDIX III - Nucleic Acid Extraction for Whole Blood – Biomerieux NucliSENS easyMAG
I.
Introduction
The NucliSENS easyMAG is an automated platform for the isolation (purification and
concentration) of total nucleic acids (RNA/DNA) from biological specimens. Used for batch
processing of 1-24 samples.
The nucleic extraction method is based on Boom Chemistry using magnetic silica particles.
Briefly, under high salt conditions, nucleic acid will bind to the silica particles. These silica
particles act as solid phase and non-nucleic acid components are removed by several washing steps
performed in the NucliSENS easyMAG instrument. Next, nucleic acids are eluded from the silica
particles and the silica particles are removed from the extracted specimens by the NucliSENS
easyMAG instrument.the resulting eluate contains purified and concentrated total nucleic acids.
II.
Specimens Types:
EDTA Whole blood minimum volume 200uL
III. Materials, Equipments
NucliSENS easyMAG
NucliSENS easyMAG extraction products:
NucliSENS Lysis Buffer
NucliSENS easyMAG Lysis Buffer
NucliSENS easyMAG Magnetic Silica
NucliSENS easyMAG Extraction Buffer 1
NucliSENS easyMAG Extraction Buffer 2
NucliSENS easyMAG Extraction Buffer 3
NucliSENS easyMAG Disposables –vessels and pipettes
BioHit Multichannel pipettor
Ranin 1000uL, 100ul, 20ul Pipettors
Aerosol Resistant Tips (ART) 1000ul, 200ul, 20ul
Powder-free gloves
Internal controls (EBV)
IV.
GENERAL PRECAUTIONS:
Do not allow the NucliSENS easyMAG Lysis Buffer, NucliSENS easyMAG Extraction Buffer 1
or waste from the instrument to come in contact with acidic materials.
Certain reagents contain guanidine thiocyanate.
PROCEDURE MANUAL
UNIVERSITY HEALTH NETWORK / MOUNT SINAI HOSPITAL MICROBIOLOGY DEPARTMENT
NOTE: This is a CONTROLLED document. Any documents appearing in paper form that are not stamped in red "MASTER COPY" are not controlled and
should be checked against the document (titled as above) on the server prior to use
D:\106748206.doc
Policy # MI/MD/v50
Microbiology Department
Policy & Procedure Manual
Section: Molecular Diagnostic Tests Manual
Page 235 of
291
Buffers containing guanidine thiocyanate MUST NOT be mixed with cleaning solutions
containing bleach. Liquid waste from extractions procedures contain guanidine thiocynate MUST
NOT be mixed with other laboratory waste. Proper waste disposal is required.
Only Aerosol Resistant Tips (ART) should be used in this procedure; single use tips, one tip per
sample.
V.
PROCEDURE: Off-Board Preparation
I.
II.
III.
Thaw whole blood samples at room temperature. DO NOT vortex samples while thawing.
When samples are completely thawed, mix by inverting sample tubes 5 times.
Prepare the Premix. Invert 10 times, vortex 10 seconds, and invert x10 again to mix. Avoid
creating bubbles.
Number of extractions One
8 extractions/
24 extractions/
extraction
one vessel
3 vessels
600 uL
5.1 mL
15 mL
Lysis Buffer volume
5 uL
44 uL
125 uL
EBV Internal Control
(IC)
140 uL
*1190 (595 x2)
**3.5 mL
Silica
uL
*4 silica aliquots needed
**6 silica aliquots needed
IV.
Prepare the NucliSENS easyMAG. See Section VI
VI. ON Board the NucliSENS easyMAG
1. Turn ON easyMAG. Wait for orange light to turn GREEN, then switch ON the easyMAG
computer.
2. Perform and record easyMAG Daily Maintence:
Inspect drip tray.
Inspect reagent cap filters.
Inspect carbon filter.
Empty & rinse waste bottle with water.
3. easyMAG Login name: bmx
Password: bmx
PROCEDURE MANUAL
UNIVERSITY HEALTH NETWORK / MOUNT SINAI HOSPITAL MICROBIOLOGY DEPARTMENT
NOTE: This is a CONTROLLED document. Any documents appearing in paper form that are not stamped in red "MASTER COPY" are not controlled and
should be checked against the document (titled as above) on the server prior to use
D:\106748206.doc
Policy # MI/MD/v50
Microbiology Department
Policy & Procedure Manual
Section: Molecular Diagnostic Tests Manual
Page 236 of
291
4. Click on “reagent” icon
Scan reagent stand and scan reagent bottle for all four reagents (A, B, C, D).
5. Click on “Sample” icon
Enter Protocol: Specific B Protocol 2.0.1
Enter Matrix: Whole Blood
Enter Volume (mL): 0.200
Eluate (uL): 50
Type: Primary
6. Click on sample ID bar and scan specimen barcodes.
7. Click on “organize run” icon
8. Click on “create run” icon
9. A box will appear with today’s date and run #. Click on OK.
10. Click on
to transfer all scanned items onto the worklist.
11. Click on “load vessel” icon
12. Load easyMAG sample vessels and pipette tips.
PROCEDURE MANUAL
UNIVERSITY HEALTH NETWORK / MOUNT SINAI HOSPITAL MICROBIOLOGY DEPARTMENT
NOTE: This is a CONTROLLED document. Any documents appearing in paper form that are not stamped in red "MASTER COPY" are not controlled and
should be checked against the document (titled as above) on the server prior to use
D:\106748206.doc
Policy # MI/MD/v50
Microbiology Department
Policy & Procedure Manual
Section: Molecular Diagnostic Tests Manual
Page 237 of
291
13. To identify vessels, click on vessel icon
14. Scan position A barcode, then scan vessel barcode; continue with position B and C, depending
on how many samples are being extracted.
15. Click on the silica icon
16. Scan silica barcode from top of silica box in use.
17. Highlight all samples by touching screen or with mouse.
18. To apply silica barcode to all samples click on “downward arrow” icon
19. Print worklist. Select printer icon on right hand vertical menu bar. Pop-up printer window
appears, click OK.
20. On the right side menu bar. Select
vessels.
to dispense lysis buffer into the extraction
PROCEDURE MANUAL
UNIVERSITY HEALTH NETWORK / MOUNT SINAI HOSPITAL MICROBIOLOGY DEPARTMENT
NOTE: This is a CONTROLLED document. Any documents appearing in paper form that are not stamped in red "MASTER COPY" are not controlled and
should be checked against the document (titled as above) on the server prior to use
D:\106748206.doc
Policy # MI/MD/v50
Microbiology Department
Policy & Procedure Manual
Section: Molecular Diagnostic Tests Manual
Page 238 of
291
21. Once the lysis buffer has been dispensed, remove vessels from the easyMag .
Place vessels into rack and take them to the Biological Safety Cabinet (BSC).
22. Carefully pipette 200uL of each EBV whole blood sample into each well of the extraction
vessels; pipette up and down three times to mix.
23. Invert and vortex the Premix. Using one ART tip per sample.
Pipette 740uL of the Premix into each well of the extraction vessels.
24. Using the BioHit Multichannel Pipette on Program 3; mix the sample, silica, and lysis buffer in
the vessel wells.
Using one ART tip per sample.
25. Load the vessels back on-board the easyMag.
Scan position A barcode, then scan vessel barcode; continue with position B and C.
26. Click on start icon
on right hand vertical menu bar.
A pop-up window will appear asking if you have added the premix silica, select YES.
Extraction of 24 samples will take approximately 60 minutes on the easyMAG.
27. Once extraction is completed, transfer the eluate from the vessel well to labeled microtube. Set
pipette at 55uL to remove all of the eluate.
28. If elutes are to be tested same day store eluates at 4C. If PCR testing is to be performed at a later
date store at -20C as soon as possible.
29. Perform Clean Dispense Probe on the EasyMag after each whole blood extraction run. See
weekly maintenance below.
PROCEDURE MANUAL
UNIVERSITY HEALTH NETWORK / MOUNT SINAI HOSPITAL MICROBIOLOGY DEPARTMENT
NOTE: This is a CONTROLLED document. Any documents appearing in paper form that are not stamped in red "MASTER COPY" are not controlled and
should be checked against the document (titled as above) on the server prior to use
D:\106748206.doc
Policy # MI/MD/v50
Microbiology Department
Policy & Procedure Manual
Section: Molecular Diagnostic Tests Manual
VII.
Page 239 of
291
DAILY CLEAN UP:
1. Remove consumables from easyMAG, bag them and discard in biohazard waste box.
2. Clean easyMAG according to maintenance worksheet and record maintenance on worksheet.
3. EMPTY WASTE: Maximum 1/3 full performed as required.
a. Select Buffer icon.
(If the Buffer icon is not on the screen, then select the Main easyMag
to access the Buffer icon.)
icon
b. Select Waste icon with droplet picture
(top icon on right vertical bar)
c. Empty waste in media room fume hood.
The Waste container should be labeled with the “Start date” and “contains guanidine
thiocyanate”. Empty any remaining buffer from easyMAG Lysis Buffer and easyMAG
Extraction Buffer1 into the fume hood waste container. Discard these empty plastic
containers (Lysis Buffer & Extraction Buffer 1) into the biohazard box.
Extraction buffer 2 and Extraction buffer 3 can be discarded in the sink and bottles can be
rinsed and recycled.
Rinse easyMAG waste container with water and return to easyMag.
d. Place the Waste Bottle back into the stand and attach the waste line to the Waste Bottle.
Select the box “I confirm that the waste container is empty.
A check mark should appear in that box.
Select OK.
4. To shut down easyMAG computer:
Select bmx key on the bottom menu bar.
PROCEDURE MANUAL
UNIVERSITY HEALTH NETWORK / MOUNT SINAI HOSPITAL MICROBIOLOGY DEPARTMENT
NOTE: This is a CONTROLLED document. Any documents appearing in paper form that are not stamped in red "MASTER COPY" are not controlled and
should be checked against the document (titled as above) on the server prior to use
D:\106748206.doc
Policy # MI/MD/v50
Microbiology Department
Policy & Procedure Manual
Section: Molecular Diagnostic Tests Manual
Page 240 of
291
Select “Quit” in the pop-up window.
Select Shutdown.
5. Wait 10 minutes after the easyMAG Computer is OFF before switching off the easyMAG.
VIII. Quality Control
Failed extraction runs, should be reviewed with senior and/or Charge technologist to establish causes
and corrective actions; repeating extraction run maybe necessary.
If the easyMag system becomes inoperable call Biomerieux technical support phone number, provided
on each easyMag.
External controls should be extracted on the easyMag according to schedule in the table below.
Analyte/target External control
EBV
High Positive (HP), Negative,
and Low Positive (LP)
Extraction schedule
once a week/ per PCR run
IX. WEEKLY MAINTENANCE:
Perform Clean Dispense after each whole blood extraction run.
Clean Dispense Probe on the EasyMag
4. Click on maintenance icon
.
5. Put in empty vessels and pipettes.
6. Choose start from vertical side bar menu
To file runs that has been completed.
Choose the magnifying glass (second menu bar from the top)
Highlight the runs you wish to file.
Choose the filing cabinet (right menu bar).
PROCEDURE MANUAL
UNIVERSITY HEALTH NETWORK / MOUNT SINAI HOSPITAL MICROBIOLOGY DEPARTMENT
NOTE: This is a CONTROLLED document. Any documents appearing in paper form that are not stamped in red "MASTER COPY" are not controlled and
should be checked against the document (titled as above) on the server prior to use
D:\106748206.doc
Policy # MI/MD/v50
Microbiology Department
Policy & Procedure Manual
Section: Molecular Diagnostic Tests Manual
IX.
Page 241 of
291
References
NucliSENS easyMAG User Manual v2.0 ref. 280163
Vignoles, M. and Bertrand, M. et al, CVS May 2013, “Improvement of Nuclisens EasyMAG
Whole Blood Extraction Protocol For Virus”
PROCEDURE MANUAL
UNIVERSITY HEALTH NETWORK / MOUNT SINAI HOSPITAL MICROBIOLOGY DEPARTMENT
NOTE: This is a CONTROLLED document. Any documents appearing in paper form that are not stamped in red "MASTER COPY" are not controlled and
should be checked against the document (titled as above) on the server prior to use
D:\106748206.doc
Policy # MI/MD/v50
Microbiology Department
Policy & Procedure Manual
Section: Molecular Diagnostic Tests Manual
Page 242 of
291
APPENDIX IV – Influenza A, B and H1N1 Virus rPCR back up testing by RotorGene
I.
Introduction
Influenza, commonly referred to as the flu, is and infectious disease caused by RNA viruses of
the family Orthomyxoviridae (the influenza viruses), that affects birds and mammals. The
influenza virus gets spread via aerosols. The major surface antigens are hemagglutinin (H) and
neuraminidase (N). The surface antigens change continuously (antigenic drift).
By using Altona Influenza Screen & Type rPCR Kit 1.2, this assay is designed to detect
Influenza B, all Influenza A strains in combination with a H1N1 (swine flu) specific primer
probe system for the detection of all swine influenza strains including the current pandemic
strain. The amplification and detection take place simultaneously, continually and in real time in
the Rotor-GeneTM.
In real-time PCR, fluorescent dyes are linked to oligonucleotide primer/probes, which bind
specifically to the amplified product. Monitoring the level of fluorescence allows the detection
of the amplicon. In the Altona Influenza Screen & Type rPCR assay version 1.2, four fluorescent
dyes are incorporated in the master mix to detect four amplified products: One for SwineFlu
specific amplicon; one for Influenza A specific (non-SwineFlu) amplicon; one for Influenza B
and another one for the Internal Control (IC). The IC is added to each specimen in the initial step
to both control the isolation procedure and to check for PCR inhibition.
The Rotor-GeneTM simultaneously monitors the four different amplicons using four fluorimeter
channels.
II.
Collection and Transport
Nasopharyngeal swabs collected in Viral Transport Media (VTM), store at 4C. Vortexed swabs
on high for 10 seconds; aliquot off the VTM and store at 4C, extract on the easyMag as soon as
possible.
BAL specimens if mucoid treat with working sputolysin. Remove red blood cells and large
particulate matter by micro-centrifuging sample for 5minutes at 3000 rpm in the Eppendroff
5415 C Micro-centrifuge. Aliquot supernatant and store at 4C, extract on the easyMag as soon as
possible.
PROCEDURE MANUAL
UNIVERSITY HEALTH NETWORK / MOUNT SINAI HOSPITAL MICROBIOLOGY DEPARTMENT
NOTE: This is a CONTROLLED document. Any documents appearing in paper form that are not stamped in red "MASTER COPY" are not controlled and
should be checked against the document (titled as above) on the server prior to use
D:\106748206.doc
Policy # MI/MD/v50
Microbiology Department
Policy & Procedure Manual
Section: Molecular Diagnostic Tests Manual
III.
Page 243 of
291
Specimen Processing
Please refer to Nucleic Acid Extraction – Biomerieux NucliSENS easyMAG
I.
Procedure:
a. Worklist Preparation:
Take the Rotor Gene worklist from the virology planting along with the extra labels.
b. Specimens Processing:
Specimens should be processed as soon as possible after arriving in virology
laboratory.
Nasophargneal swabs, sputum and BAL’s are used to detect H1N1 and
Influenza A & B.
After processing, an aliquot of the left-over specimens should be stored frozen
at-70C.
c. Materials, Equipments and Facilities:
Clean Room with dedicated Biosafety Cabinet (MIBCT3), freezer (MIFTG), gowns and
gloves.
Specimen Preparation area with Biosafety Cabinet (MIBCT7 or MIBCT8)
and microcentrifuge(MICT17)
Vortex
Detection Room for Rotor-Gene 6000
Rotor-Gene 6000 Multiplexing System programmed for ALTONA H1N1 virus RT PCR
96-Well Loading Block (pre-cooled to 4oC)
72-Well Loading Block (pre-cooled to 4oC)
36-Well High Profile Rotor
36-Well Rotor Locking Ring
72-Well 6000 Series Rotor
72-Well Rotor Locking Ring
0.2mL Tubes
0.1 mL Strip Tubes and Caps
Variable volume pipettes:
1 to 20 uL
10 to 200 uL
100 to 1000 uL
PROCEDURE MANUAL
UNIVERSITY HEALTH NETWORK / MOUNT SINAI HOSPITAL MICROBIOLOGY DEPARTMENT
NOTE: This is a CONTROLLED document. Any documents appearing in paper form that are not stamped in red "MASTER COPY" are not controlled and
should be checked against the document (titled as above) on the server prior to use
D:\106748206.doc
Policy # MI/MD/v50
Microbiology Department
Policy & Procedure Manual
Section: Molecular Diagnostic Tests Manual
Page 244 of
291
From: Altona Influenze Screen & Type rPCR Kit 1.0, (stored at -20o C in clean room):
Swine Flu Positive Control
Influenza A Positive Control
Influenza B Positive Control
Master A (12 tests per vial)
Master B (12 tests per vial)
Internal Control (IC)
Water (PCR grade)
External Control: To be run when a new lot is used, during training or if QC failure
occurs.
GENERAL PRECAUTIONS:
There must be separate PCR work areas:
c. Clean room
d. Specimen preparation room
Amplification room Supplies and equipment must be dedicated to each PCR
area and not used for other activities or moved between areas.
Change lab coats and gloves between work areas. Only blue gowns are to be
worn in the clean room.
Use only filtered pipette tips
Use only sterile RNase, Dnase-free microcentrifuge tubes
Use sterile, disposable polypropylene tubes throughout the procedure
Always wear powder-free gloves when handling reagents
Change gloves frequently and keep tubes closed whenever possible
Thaw components thoroughly at room temperature
Mix components and centrifuge briefly
Work quickly in the cooling block
Use 1% sodium hypochloride or Eliminase to disinfect equipment and
surfaces and then rinse with 70% alcohol or water.
Sample Preparation:
Use Specimen Preparation area; work in cabinet with gown and frequent glove change
Use EasyMag to extract DNA and RNA
PROCEDURE MANUAL
UNIVERSITY HEALTH NETWORK / MOUNT SINAI HOSPITAL MICROBIOLOGY DEPARTMENT
NOTE: This is a CONTROLLED document. Any documents appearing in paper form that are not stamped in red "MASTER COPY" are not controlled and
should be checked against the document (titled as above) on the server prior to use
D:\106748206.doc
Policy # MI/MD/v50
Microbiology Department
Policy & Procedure Manual
Section: Molecular Diagnostic Tests Manual
Page 245 of
291
PCR Set-up:
In the Clean Room: (Change into dedicated clean room gown and gloves, work in Biosafety Cabinet)
d. Take out the necessary number of H1N1 Master Mix A and B vials (24 tests per vial) from the
freezer and thoroughly thaw inside the Biosafety Cabinet. Determine the number of tests and
prepare the appropriate volume of Master Mix required according to the chart. Mix gently, do
not vortex. Make only enough master mix for the tests you are running. After vial A has
been added to Vial B it cannot be frozen again.
No. of samples
1
2
3
4
5
6
7
8
9
10
11
12
Preparation of Master Mix
Master A (µl)
5
10
15
20
25
30
35
40
45
50
55
60
Master B (µl)
10
20
30
40
50
60
70
80
90
100
110
120
b.
Place proper micro tubes for each purified sample, Positive controls, external QC and Negative
control (H2O) into the Cooling Block (pre-cooled to 4oC).
c.
Pipette 15 uL prepared Master Mix (A+B) into each micro tubes
h.
Pipette 1.0 uL of internal control into the micro tubes designated for the Positive controls and
water.
i.
Pipette 10uL water (PCR grade) into the negative control micro tube. Mix up and down 3X and
cap tightly. Label each microtubes 1,2,3…. before leaving clean room.
j.
Place the cooling block in to a clean biohazard bag.
PROCEDURE MANUAL
UNIVERSITY HEALTH NETWORK / MOUNT SINAI HOSPITAL MICROBIOLOGY DEPARTMENT
NOTE: This is a CONTROLLED document. Any documents appearing in paper form that are not stamped in red "MASTER COPY" are not controlled and
should be checked against the document (titled as above) on the server prior to use
D:\106748206.doc
Policy # MI/MD/v50
Microbiology Department
Policy & Procedure Manual
Section: Molecular Diagnostic Tests Manual
k.
Page 246 of
291
Changed out of dedicated clean room gown.
In the Specimen Processing Room: (Changed into specimen room gown)
e.
f.
g.
h.
Using a separate filter tip each time, carefully pipette 10 uL each of purified sample, Positive
controls, and external QC (if using) directly into the micro tubes. Mix by pipetting 3x up and
down into the mastermix. Immediately close the cap tightly.
Check each micro tube before loading. Make sure there is no bubble at the bottom of the tube.
Load micro tubes into a proper rotor (e.g. 36-well or 72-well) and snap close the locking ring.
Load the rotor in Rotor-Gene 6000.
Always fill up the empty position of the rotor using empty tubes.
In the Rotorgene room:
a.
b.
c.
d.
e.
f.
g.
h.
i.
j.
k.
l.
m.
n.
o.
p.
q.
r.
s.
t.
u.
Turn on computer, turn on Rotorgene;
FOR THE BLUE ROTORGENE ONLY. Choose clinical icon; pass word “msh”; press “→”
button;
Double click(left on the mouse) “Rotor-Gene 6000 series software 1.7” icon
Wait for “Initializing machine…..”
Highlight “Influenza A,B & H1N1” assay;
Press “New” button;
Highlighting the correct Rotor type you are using
36-well Rotor (Red)
72-well Rotor (Blue)
Tick the “Locking Ring Attached” option
Press “Next” button
Enter initials in operator space. Enter Master Mix lot. # in the Notes space. Make sure the
Reaction Volume is “25µl”;
Press “Next” button
Temperature profile window pops up, press “Next” button
Make sure your ring has been loaded in the Rotorgene.
Summary window pops up, press “Start Run” button;
Save As window pops up; the run is given a filename with a default template. Change it
according to the date and numerical runs the assay performed on the same day; e.g. H1N1 200907-17-01 (assay name-year-month-date-numerical run#);
Note: Influenza results are stored in \desktop\My Doucument\Influenza A,B&H1N1
Press Save button;
Machine is starting and Edit Samples window pops up; Enter sample LIS# including positive
and negative controls.
Define the type of samples according to the chart:
PROCEDURE MANUAL
UNIVERSITY HEALTH NETWORK / MOUNT SINAI HOSPITAL MICROBIOLOGY DEPARTMENT
NOTE: This is a CONTROLLED document. Any documents appearing in paper form that are not stamped in red "MASTER COPY" are not controlled and
should be checked against the document (titled as above) on the server prior to use
D:\106748206.doc
Page 247 of
291
Policy # MI/MD/v50
Microbiology Department
Policy & Procedure Manual
Section: Molecular Diagnostic Tests Manual
v.
w.
Name
Type
Select
Sample
Unknown
Yes
Positive Controls H1N1, FluA, FluB
Positive Control
Yes
Water
Negative Control
Yes
Once finishing all samples, press Finish button.
Once cycling screen comes on, click “Named On” button.
To analyze and print H1N1 report after a run is finished:
a.
b.
c.
d.
e.
f.
g.
h.
i.
j.
k.
l.
m.
n.
The run is done when Profile Program reads: Run has completed.
Analyze raw data by clicking on the each of these channels (one at a time): Green channel
(H1N1), Red channel (Flu A other than H1N1), Orange channel (Flu B) and Yellow channel (IC).
These tabs are found on the second menu bar from the top, on the left hand side.
Click on autoscale (bottom left). Click “All Off” (bottom right). Click “water” on. Compare the
specimen and control curves to the water one at a time (by clicking each sample on and then off
when
proceeding to the next sample). A positive curve will have a sigmoidal shape. A negative
result will be a relatively flat line, like the water. Make a note of the positives on the worklist.
Click on “Named On”
Perform curve analysis: Click Analysis on the top tool bar.
Analysis floating window pops up;
Choose “Quantitation” tab.
Quantitation window is brought up to the front. There should be four channels: Green (H1N1),
Red (Flu A other than H1N1), Orange (Flu B) and Yellow (IC).
Highlight Cycling A. Green (Page 1) (H1N1) option and press Show button.
Maximize cycling green window (or the channel you are working on)
Highlight slope correct tab.
Click on Ignore first… tab. A window will pop-up, type in 5 (i.e. ignore 5 cycles).
Set threshold at 0.05. A threshold line will appear on the screen.
Move threshold line to above the noise (i.e. Negative specimens)
To Print reports: Press Reports button on the top toolbar.
a.
b.
c.
d.
e.
f.
Report Browser window pops up.
Choose Cycling A. Green (Page 1). Under templates box, choose “Quantitation full report”.
Press Show button
Maximize the report window, check that only the positives that you have identified from your raw
data analysis are positive (i.e. have a crosspoint)
Choose print report. (for the red, orange and yellow channels print only pages 2-4).
Once finishing the print, close the report window
Go to the floating Analysis window;
PROCEDURE MANUAL
UNIVERSITY HEALTH NETWORK / MOUNT SINAI HOSPITAL MICROBIOLOGY DEPARTMENT
NOTE: This is a CONTROLLED document. Any documents appearing in paper form that are not stamped in red "MASTER COPY" are not controlled and
should be checked against the document (titled as above) on the server prior to use
D:\106748206.doc
Policy # MI/MD/v50
Microbiology Department
Policy & Procedure Manual
Section: Molecular Diagnostic Tests Manual
g.
Page 248 of
291
Repeat the step from “e” to “m” for Cycling A. Red (Influenza A), Cycling A. (Influenza B) and
Cycling A. Yellow (internal control)
Shut down computer:
d. Exit from software. A pop-up window will appear “save changes”. Click “yes”.
e. Click “start” button. Click “Turn off computer”.
f. Turn off Rotorgene
At the end of the day, follow the cleaning protocol below using 1% hypochorite or Eliminase
followed by 70% alcohol:
Clean Room:
Clean Biological Safety Cabinet
Specimen Preparation Room:
Clean Biological Safety Cabinet, pipettors, centrifuge, and bench top.
Cap discard container.
Wash racks.
Amplification Room:
Discard micro tubes into a disposal bag and tight the bag.
Discard the bag into biohazard waster container.
Perform the cleaning procedure according the daily maintenance sheet.
PROCEDURE MANUAL
UNIVERSITY HEALTH NETWORK / MOUNT SINAI HOSPITAL MICROBIOLOGY DEPARTMENT
NOTE: This is a CONTROLLED document. Any documents appearing in paper form that are not stamped in red "MASTER COPY" are not controlled and
should be checked against the document (titled as above) on the server prior to use
D:\106748206.doc
Policy # MI/MD/v50
Microbiology Department
Policy & Procedure Manual
Section: Molecular Diagnostic Tests Manual
Page 249 of
291
IV. Interpretation and Reporting
Green
Channel
(H1N1
specific)
Red
Channel
(Influenza
A specific,
nonswineflu)
Orange
Channel
(Influenza B)
Yellow
Channel
(IC
specific)
Interpretations
+
-
-
+/-
Positive for H1N1
-
+
-
+/-
Positive for Influenza A, NOT H1N1
+
+
-
+/-
Positive for H1N1 and Influenza A (ask
senior for confirmation)
-
-
+
+/-
Positive for Influenza B
-
-
-
+
Negative for both H1N1 and Influenza A
-
-
-
-
INVALID
Test needs to be repeated. Sample needs to
be diluted 1:4
-
-
-
-
Repeated Diluted 1:4 Sample tested:
INDETERMINATE
Note: Check for each curve of the samples showing positive reactions either/or for the Red, Orange and
Green Channel in comparison with the positive and water (negative) controls. Do this step by clicking
the ALL OFF tab and then highlighting the samples showing positive reactions in the Quantitation result
channel.
Positive for H1N1, Influenza A, or Influenza B report as an isolate in the (F7) Isolate Window.
Date the media on the back of the LIS workcard. PCH1R: F6 to add run date
Enter on the media line the cross point (ct) value: Ct=
Report the virus as an isolate in the F7 window.
Isolate window (F7)
Isolate #: 1
PROCEDURE MANUAL
UNIVERSITY HEALTH NETWORK / MOUNT SINAI HOSPITAL MICROBIOLOGY DEPARTMENT
NOTE: This is a CONTROLLED document. Any documents appearing in paper form that are not stamped in red "MASTER COPY" are not controlled and
should be checked against the document (titled as above) on the server prior to use
D:\106748206.doc
Policy # MI/MD/v50
Microbiology Department
Policy & Procedure Manual
Section: Molecular Diagnostic Tests Manual
Page 250 of
291
Org. ID: 23ah1n1 Influenza A H1N1 (Swine) virus
23notsw Influenza A virus NOT H1N1 (Swine)
23infb Influenza B virus
Open the Isolate Comment window F8.
Go to the Virology keypad, type “V”. Ctrl D. Select from the keypad: \ANH1 to add the comment
phrase:
DETECTED by PCR.
This is a research test. Influenza Screen & Type RT-PCR Kit v1.2
Altona Diagnostics Inc.
This isolate has been forwarded to PHL (Public Health Laboratory) for subtyping.
Results to follow.
Note: Remove (delete) the sentences that refer to subtyping at PHL when reporting H1N1, and Influenza
B; subtyping is only required for Influenza A isolates.
Grave (`) the result.
Ctrl-F to finalize the report.
Call all positives to ward/doctor and Infection Control Practitioner (ICP). The Medical Officer of Health
(MOH) must be notified by fax and phone. Record all calls and faxes made on the LIS workcard; under
the CALL media and in the Call Window.
Negative for H1N1, Influenza A, and Influenza B.
Date the media on the back of the LIS workcard. PCH1R: F6 to add run date.
On the front of the LIS workcard. Select from the keypad: }H1}H1- Negative for Influenza A and B including H1N1 (Swine) virus.
This is a research test.
Influenza Screen and Type RT-PCR Kit v1.2
Altona Diagnostics Inc.
Ctrl-F to finalize the report.
Indeterminate Report. Date the media on the back of the LIS workcard. PCH1R: F6 to add run date.
Select from the keypad “Failed single”, type “IC no amplification”, select >FAIL
Select from keypad ^PRH1R. Under this media report the dilution test result.
On the front of the LIS workcard. Select from the keypad: }H1Change “Negative” to INDETERMINATE.
INDETERMINATE for Influenza A and B including H1N1 (Swine) virus.
This is a research test.
Influenza Screen and Type RT-PCR Kit v1.2
Altona Diagnostics Inc.
PROCEDURE MANUAL
UNIVERSITY HEALTH NETWORK / MOUNT SINAI HOSPITAL MICROBIOLOGY DEPARTMENT
NOTE: This is a CONTROLLED document. Any documents appearing in paper form that are not stamped in red "MASTER COPY" are not controlled and
should be checked against the document (titled as above) on the server prior to use
D:\106748206.doc
Policy # MI/MD/v50
Microbiology Department
Policy & Procedure Manual
Section: Molecular Diagnostic Tests Manual
Page 251 of
291
Ctrl-F to finalize the report.
II.
Quality Control
Reagent QCs:
An External Control (external to Altona Diagnostics) is used to monitor the isolation,
amplification and detection procedures. The result must correspond to expected value
supplied by the manufacturer.
External control for H1N1, Influenza A (not H1N1), and Influenza B should be extracted on
the on the easyMag and run once a month and/or with each new lot.
Daily QCs:
Every run:
Each patient specimen must have an Internal Control (IC) added to monitor both isolation
and PCR inhibition.
A Positive Control is included and shows either a positive reading in Green Channel
(SwineFlu specific) or a positive reading in Red Channel (Infuenza A specific-non SwineFlu)
A Negative Control is include and shows a negative reading in both Green Channel
(SwineFlu specific) and Red Channel (Infuenza A specific-non SwineFlu)
Report all failed QCs to senior/charge technologist.
Failed QC:
Test is invalid without satisfactory QC results.
a. Do not release results pending resolution of QC failure.
b. Inform charge/senior technologist.
c. Record in Reagent Log Chart, Instrument Maintenance Log or Incident Report where
appropriate.
d. If the QC failure was due to a simple matter of position reversal or misplacement, the run can be
released (positive QC material yielded positive result, negative yielded negative result).
e. If positive QC material yielded negative result, repeat the entire run.
f. If negative QC material yielded positive result, it may be due to cross-contamination from
adjacent positive sample within the run or carry-over contamination from previous runs via
equipment or the environment. Review procedure and equipment to establish and eliminate
potential sources of contamination.
g. The extent and nature of contamination can also be evaluated by comparing the positive rate of
the run with its expected positive rate.
PROCEDURE MANUAL
UNIVERSITY HEALTH NETWORK / MOUNT SINAI HOSPITAL MICROBIOLOGY DEPARTMENT
NOTE: This is a CONTROLLED document. Any documents appearing in paper form that are not stamped in red "MASTER COPY" are not controlled and
should be checked against the document (titled as above) on the server prior to use
D:\106748206.doc
Policy # MI/MD/v50
Microbiology Department
Policy & Procedure Manual
Section: Molecular Diagnostic Tests Manual
Page 252 of
291
h. If the contamination is extensive, it is necessary to quarantine/discard potentially contaminated
reagents and consumables and disinfect equipment and environment before repeating the run.
i. If a carry-over contamination is suspected (e.g. two or more runs with negative QC being
positive or patient samples have higher than expected positive rate and these samples are often
non-repeatable positives), it is necessary to have a thorough environmental disinfection followed
by swabbing to monitor.
j. Successful ending to a carry-over contamination may be indicated by QC results and patient
positivity rate falling back to the expected normal range and three negative environmental swabs.
III.
References:
Altona Influenza screen & Type RT-PCR Kit 1.2 User Manual, Altona
PROCEDURE MANUAL
UNIVERSITY HEALTH NETWORK / MOUNT SINAI HOSPITAL MICROBIOLOGY DEPARTMENT
NOTE: This is a CONTROLLED document. Any documents appearing in paper form that are not stamped in red "MASTER COPY" are not controlled and
should be checked against the document (titled as above) on the server prior to use
D:\106748206.doc
Policy # MI/MD/v50
Microbiology Department
Policy & Procedure Manual
Section: Molecular Diagnostic Tests Manual
Page 253 of
291
APPENDIX V - Respiratory Synctial Virus (RSV) PCR backup testing by RotorGene
VI. Introduction
Respiratory Synctial Virus (RSV) is a negative sense, single stranded RNA virus of the family
Paramyxoviridae. Based on antigenic properties and sequence analysis RSV are subdivided into
RSV A and RSV B. Different genotypes of both subgroups can co-circulate within one epidemic
with varying frequency. RSV causes respiratory tract infections. For most people, a RSV
infection produces only mild symptoms like common cold. But RSV is the most important cause
of severe respiratory illness in infants and young children and the major cause of infantile
bronchiolitis and pneumonia in industrialized countries. Nearly all children will have been
infected with the virus by 2-3 years of age. RSV also is a significant problem in the elderly, in
persons with cardiopulmonary diseases and in immunocompromised individuals. Repeated
reinfections occur throughout life. RSV is spread by infectious droplets or by contact with nasal
or oral secretions from infected people. Outbreaks of RSV infections are reported worldwide,
with striking annual epidemics in the winter and early spring in temperate climates, like Europe
and North America, and in the rainy season in the tropics.
VII.
Collection and Transport
Nasopharyngeal swabs collected in Viral Transport Media (VTM), store at 4C. Vortexed swabs
on high for 10 seconds; aliquot off the VTM and store at 4C, extract on the easyMag as soon as
possible.
BAL specimens if mucoid treat with working sputolysin. Remove red blood cells and large
particulate matter by micro-centrifuging sample for 5minutes at 3000 rpm in the Eppendroff
5415 C Micro-centrifuge. Aliquot supernatant and store at 4C, extract on the easyMag as soon as
possible.
VIII. Specimen Processing
Please refer to Nucleic Acid Extraction –Biomerieux NucliSENS easyMAG
GENERAL PRECAUTIONS:
There must be separate PCR work areas:
e. Clean room
f. Specimen preparation room
Amplification room Supplies and equipment must be dedicated to each PCR
area and not used for other activities or moved between areas.
PROCEDURE MANUAL
UNIVERSITY HEALTH NETWORK / MOUNT SINAI HOSPITAL MICROBIOLOGY DEPARTMENT
NOTE: This is a CONTROLLED document. Any documents appearing in paper form that are not stamped in red "MASTER COPY" are not controlled and
should be checked against the document (titled as above) on the server prior to use
D:\106748206.doc
Policy # MI/MD/v50
Microbiology Department
Policy & Procedure Manual
Section: Molecular Diagnostic Tests Manual
Page 254 of
291
Change lab coats and gloves between work areas. Only blue gowns are to be
worn in the clean room.
Use only filtered pipette tips
Use only sterile RNase, Dnase-free microcentrifuge tubes
Use sterile, disposable polypropylene tubes throughout the procedure
Always wear powder-free gloves when handling reagents
Change gloves frequently and keep tubes closed whenever possible
Thaw components thoroughly at room temperature
Mix components and centrifuge briefly
Work quickly in the cooling block
Use 1% sodium hypochloride or Eliminase to disinfect equipment and
surfaces and then rinse with 70% alcohol or water.
a. Materials, Equipments and Facilities:
Clean Room with dedicated Biosafety Cabinet (MIBCT3), freezer (MIFTG), gowns and
gloves
Specimen Preparation area with Biosafety Cabinet (MIBCT7 or MIBCT8)
and microcentrifuge(MICT17)
Vortex
Detection Room for Rotor-Gene 6000
Rotor-Gene 6000 Multiplexing System programmed for ALTONA RSV A & B RT
PCR
72-Well Loading Block (pre-cooled to 4oC)
72-Well 6000 Series Rotor
72-Well Rotor Locking Ring
0.1 mL Strip Tubes and Caps
36-Well High Profile Rotor
36-Well Rotor Locking Ring
0.2mL Tubes
Variable volume pipettes:
1 to 20 uL
10 to 200 uL
100 to 1000 uL
From: Altona RSV A & B RT-PCR Kit 1.0, (stored at -20o C in clean room):
RSV A Positive Control
RSV B Positive Control
RSV Master A (12 tests per vial)
RSV Master B (12 tests per vial)
RSV Internal Control (IC)
Water (PCR grade)
PROCEDURE MANUAL
UNIVERSITY HEALTH NETWORK / MOUNT SINAI HOSPITAL MICROBIOLOGY DEPARTMENT
NOTE: This is a CONTROLLED document. Any documents appearing in paper form that are not stamped in red "MASTER COPY" are not controlled and
should be checked against the document (titled as above) on the server prior to use
D:\106748206.doc
Policy # MI/MD/v50
Microbiology Department
Policy & Procedure Manual
Section: Molecular Diagnostic Tests Manual
Page 255 of
291
External Control: To be run when a new lot is used, during training or if QC failure
occurs.
IX. Procedure:
Take RSV worklist from the virology prep bench and arrange eluates in order according to the
worklist, store the eluates at 4C until ready to add to the RSV Master mix.
PCR Set-up:
In the Clean Room: (Change into dedicated clean room gown and gloves, work in Biosafety Cabinet)
a. Take out the necessary number of RSV A & B Master Mix A and B vials (24 tests per vial) from
the freezer and thoroughly thaw inside the Biosafety Cabinet. Determine the number of tests and
prepare the appropriate volume of Master Mix required according to the chart. Mix gently, do
not vortex. Make only enough master mix for the tests you are running. After vial A has
been added to Vial B it cannot be frozen again.
No. of samples
1
2
3
4
5
6
7
8
9
10
11
12
Preparation of Master Mix
Master A (µl)
5
10
15
20
25
30
35
40
45
50
55
60
Master B (µl)
15
30
45
60
75
90
105
120
135
150
165
180
b. Place proper micro tubes for each purified sample, Positive controls, external QC and Negative
control (H2O) into the Cooling Block (pre-cooled to 4oC).
c. Pipette 20 uL prepared Master Mix (A+B) into each micro tubes
d. Pipette 0.5 uL of internal control into the micro tubes designated for the RSV A Positive Control,
RSV B Positive Control and PCR grade Water- Negative Control.
PROCEDURE MANUAL
UNIVERSITY HEALTH NETWORK / MOUNT SINAI HOSPITAL MICROBIOLOGY DEPARTMENT
NOTE: This is a CONTROLLED document. Any documents appearing in paper form that are not stamped in red "MASTER COPY" are not controlled and
should be checked against the document (titled as above) on the server prior to use
D:\106748206.doc
Policy # MI/MD/v50
Microbiology Department
Policy & Procedure Manual
Section: Molecular Diagnostic Tests Manual
Page 256 of
291
e. Pipette 5uL water (PCR grade) into the negative control micro tube. Mix up and down 3X and
cap tightly. Label each microtubes 1,2,3…. before leaving clean room.
f. Place the cooling block into a clean biohazard bag.
g. Changed out of dedicated clean room gown.
In the Specimen Processing Area: (Change into specimen room gown)
a. Using a separate filter tip each time, carefully pipette 5 uL each of purified sample, Positive
controls, and external QC (if using) directly into the micro tubes. Mix by pipetting 3x up and
down into the mastermix. Immediately close the cap tightly.
b. Check each micro tube before loading. Make sure there is no bubble at the bottom of the tube.
c. Load micro tubes into a proper rotor (e.g. 36-well or 72-well) and snap close the locking ring.
Load the rotor in Rotor-Gene 6000.
d. Always fill up the empty position of the rotor using empty tubes.
In the Rotorgene Detection Area:
oo. Turn on computer, turn on Rotorgene;
pp. FOR BLUE ROTORGENE ONLY. Choose clinical icon; pass word “msh”; press “→”
button;
qq. Double click(left on the mouse) “Rotor-Gene 6000 series software 1.7” icon
rr. Wait for “Initializing machine…..”
ss. Highlight “ALTONA RSV A&B” assay;
tt. Press “New” button;
uu. Highlighting the correct Rotor type you are using
vv. 72-well Rotor (Blue)
ww.
36-well Rotor (Red)
xx. Tick the “Locking Ring Attached” option
yy. Press “Next” button
zz. Enter initials in operator space. Enter Master Mix lot. # in the Notes space. Make sure the
Reaction Volume is “25µl”;
aaa.
Press “Next” button
Temperature profile window pops up, press “Next” button
bbb.
Make sure your ring has been loaded in the Rotorgene.
ccc.
Summary window pops up, press “Start Run” button;
ddd.
Save As window pops up; the run is given a filename with a default template. Change it
according to the date and numerical runs the assay performed on the same day; e.g. RSV A&B
2010.03.29 (e.g. assay name-year-month-date-numerical run#);
a. Note: RSV results are stored in \desktop\My Doucument\RSV A&B results.
eee.
Press Save button;
fff. Machine starts and Edit Samples window pops up;
PROCEDURE MANUAL
UNIVERSITY HEALTH NETWORK / MOUNT SINAI HOSPITAL MICROBIOLOGY DEPARTMENT
NOTE: This is a CONTROLLED document. Any documents appearing in paper form that are not stamped in red "MASTER COPY" are not controlled and
should be checked against the document (titled as above) on the server prior to use
D:\106748206.doc
Policy # MI/MD/v50
Microbiology Department
Policy & Procedure Manual
Section: Molecular Diagnostic Tests Manual
Page 257 of
291
ggg.
Enter sample LIS# including positive and negative controls. Define the type of samples
according to the chart:
Name
Sample
RSV A Positive Control
RSV B Positive Control
Water
Type
Unknown
Positive Control
Positive Control
Negative Control
Select
Yes
Yes
Yes
Yes
hhh.
Press Finish button.
iii. Once cycling screen comes on, click “Named On” button.
To analyze and print RSV A &B report after a run is finished:
tt. The run is done when Profile Program reads: Run has completed.
uu. Analyze raw data by clicking on the each of these channels (one at a time): Green channel
(RSV B), Red channel (RSV A) and Yellow channel (IC). These tabs are found on the second
menu bar from the top, on the left hand side.
vv. Click on autoscale (bottom left). Click “All Off” (bottom right). Click “water” on. Compare the
specimen and control curves to the water one at a time (by clicking each sample on and then off
when proceeding to the next sample). A positive curve will have a sigmoidal shape. A negative
result will be a relatively flat line, like the water. Make a note of the positives on the RSV
worklist.
ww.
Click on “Named On”
xx. Perform curve analysis: Click Analysis on the top tool bar.
yy. Analysis floating window pops up
zz. Choose “Quantitation” tab.
aaa.
Quantitation window is brought up to the front. There should be three
channels: Green (RSV B), Red (RSV A) and Yellow (IC).
bbb.
Highlight Cycling A. Green (Page 1) (RSV B) option and press Show
button.
ccc.
Maximize cycling green window (or the channel you are working on)
ddd.
Highlight slope correct tab.
eee.
Click on Ignore first… tab. A window will pop-up, type in 5 (i.e. ignore 5
cycles).
fff. Set threshold at 0.05. A threshold line will appear on the screen.
ggg.
Move threshold line to above the noise (i.e. Negative specimens)
hhh.
To Print reports: Press Reports button on the top toolbar.
iii. Report Browser window pops up.
jjj. Choose Cycling A. Green (Page 1). Under templates box, choose “Quantitation full report”.
kkk.
Press Show button
lll. Maximize the report window, check that only the positives that you have identified from your
raw data analysis are positive (i.e. have a crosspoint).
PROCEDURE MANUAL
UNIVERSITY HEALTH NETWORK / MOUNT SINAI HOSPITAL MICROBIOLOGY DEPARTMENT
NOTE: This is a CONTROLLED document. Any documents appearing in paper form that are not stamped in red "MASTER COPY" are not controlled and
should be checked against the document (titled as above) on the server prior to use
D:\106748206.doc
Policy # MI/MD/v50
Microbiology Department
Policy & Procedure Manual
Section: Molecular Diagnostic Tests Manual
Page 258 of
291
mmm.
Choose print report. (for the red and yellow channels print only pages 24).
nnn.
Once finished printing, close the report window
ooo.
Go to the floating Analysis window;
ppp.
Repeat the step from “e” to “t” for Cycling A. Red (RSV A) and Cycling
A. Yellow (internal control)
Shut down computer:
a. Exit from software. A pop-up window will appear “save changes”. Click “yes”.
b. Click “start” button. Click “Turn off computer”.
c. Turn off Rotorgene
At the end of the day, follow the cleaning protocol below using 1% hypochorite or Eliminase followed
by 70% alcohol:
Clean Room:
Clean Biological Safety Cabinet
Specimen Preparation Room:
Clean Biological Safety Cabinet, pipettors, centrifuge, and bench top.
Cap discard container.
Wash racks.
Amplification Room:
Discard micro tubes into a disposal bag and close the bag.
Discard the bag into biohazard waster container.
Perform the cleaning procedure according the daily maintenance sheet.
IV.
Interpretation and Reporting:
Green
Channel
(RSV B)
Red
Channel
(RSV A)
Yellow
Channel
(IC specific)
+
-
+/-
Positive for RSV B
-
+
+/-
Positive for RSV A
+
+
+/-
Positive for RSV A & B (ask senior for
confirmation)
-
-
+
Negative for both RSV A & B
Interpretations
PROCEDURE MANUAL
UNIVERSITY HEALTH NETWORK / MOUNT SINAI HOSPITAL MICROBIOLOGY DEPARTMENT
NOTE: This is a CONTROLLED document. Any documents appearing in paper form that are not stamped in red "MASTER COPY" are not controlled and
should be checked against the document (titled as above) on the server prior to use
D:\106748206.doc
Policy # MI/MD/v50
Microbiology Department
Policy & Procedure Manual
Section: Molecular Diagnostic Tests Manual
Page 259 of
291
INVALID
Test needs to be repeated. Sample needs
to be diluted 1:4 with lysis buffer
Note: Check for each curve of the samples showing positive reactions either/or for the Red, Orange
and Green Channel in comparison with the positive and water (negative) controls. Do this step by
clicking the ALL OFF tab and then highlighting the samples showing positive reactions in the
Quantitation result channel.
Positive for RSV A, or RSV B report as an isolate in the (F7) Isolate Window.
Date the media on the back of the LIS workcard PCRSV: F6 to add the date tested.
Enter on the PCRSV media line the crosspoint (ct) value: ct=
Report the virus as an isolate in the F7 window.
Isolate #: 1
Org. ID: 26rsvA
Respiratory syncytial virus type A
26rsvB
Respiratory syncytial virus type B
Open the Isolate Comment window F8
Go to the virology keypad, type “V”. Ctrl D. Select from the keypad: \RSV+ to add the comment
phrase:
\RSV+
DETECTED by PCR.
This is a research test.
RSV RT-PCR Kit v1.0 Altona Diagnostics Inc.
Grave (`) the result.
Ctrl-F to finalize the report.
Call all positives to ward/doctor and Infection Control Practitioner (ICP).
Negative for RSV A and RSV B.
Date the media on the back of the LIS workcard. PCRSV: F6 to add run date.
On the front of the LIS workcard, select from the keypad: }RAB}RAB-
Negative for Respiratory Syncytial Virus A and B.
This is a research test.
RSV RT-PCR Kit v1.
Altona Diagnostics Inc.
Ctrl-F to finalize the report.
Indeterminate Report. (Internal control failed twice to amplify.) Date the media on the back of the LIS
workcard. PCRSV: F6 to add run date. Select from the keypad “Failed single”, type “IC no
amplification”, select >FAIL
Select from keypad ^PRRSV. Under this media ^PRRSV report the 1:4 dilution test result type “IC
no amplification”.
On the front of the LIS workcard. Select from the keypad: }RSVChange “Negative” to INDETERMINATE; final report should appear as:
PROCEDURE MANUAL
UNIVERSITY HEALTH NETWORK / MOUNT SINAI HOSPITAL MICROBIOLOGY DEPARTMENT
NOTE: This is a CONTROLLED document. Any documents appearing in paper form that are not stamped in red "MASTER COPY" are not controlled and
should be checked against the document (titled as above) on the server prior to use
D:\106748206.doc
Policy # MI/MD/v50
Microbiology Department
Policy & Procedure Manual
Section: Molecular Diagnostic Tests Manual
Page 260 of
291
INDETERMINATE for Respiratory Syncytial Virus A and B.
This is a research test.
RSV RT-PCR Kit v1.
Altona Diagnostics Inc.
.
Ctrl-F to finalize the report.
V.
Quality Control
Reagent QCs:
An External Control (external to Altona Diagnostics) is used to monitor the isolation,
amplification and detection procedures. The result must correspond to expected value supplied
by the manufacturer.
External control for RSV A, and RSV B should be extracted on the on the easyMag and run once
a month and/or with each new lot.
Daily QCs:
Every run:
Each patient specimen must have an Internal Control (IC) added to monitor both isolation
and PCR inhibition.
A Positive Control is included and shows either a positive reading in Green Channel
(RSV B) or a positive reading in Red Channel (RSV A)
A Negative Control is include and shows a negative reading in both Green Channel (RSV
B) and Red Channel (RSV A)
Report all failed QCs to senior/charge technologist.
Failed QC:
Test is invalid without satisfactory QC results.
a. Do not release results pending resolution of QC failure.
b. Inform charge/senior technologist.
c. Record in Reagent Log Chart, Instrument Maintenance Log or Incident Report where
appropriate.
d. If the QC failure was due to a simple matter of position reversal or misplacement, the run can be
released (positive QC material yielded positive result, negative yielded negative result).
e. If positive QC material yielded negative result, repeat the entire run.
f. If negative QC material yielded positive result, it may be due to cross-contamination from
adjacent positive sample within the run or carry-over contamination from previous runs via
equipment or the environment. Review procedure and equipment to establish and eliminate
potential sources of contamination.
PROCEDURE MANUAL
UNIVERSITY HEALTH NETWORK / MOUNT SINAI HOSPITAL MICROBIOLOGY DEPARTMENT
NOTE: This is a CONTROLLED document. Any documents appearing in paper form that are not stamped in red "MASTER COPY" are not controlled and
should be checked against the document (titled as above) on the server prior to use
D:\106748206.doc
Policy # MI/MD/v50
Microbiology Department
Policy & Procedure Manual
Section: Molecular Diagnostic Tests Manual
Page 261 of
291
g. The extent and nature of contamination can also be evaluated by comparing the positive rate of
the run with its expected positive rate.
h. If the contamination is extensive, it is necessary to quarantine/discard potentially contaminated
reagents and consumables and disinfect equipment and environment before repeating the run.
i. If a carry-over contamination is suspected (e.g. two or more runs with negative QC being
positive or patient samples have higher than expected positive rate and these samples are often
non-repeatable positives), it is necessary to have a thorough environmental disinfection followed
by swabbing to monitor.
j. Successful ending to a carry-over contamination may be indicated by QC results and patient
positivity rate falling back to the expected normal range and three negative environmental swabs.
X. References:
RSV A & B RT-PCR Kit v1.0 User Manual, Altona
PROCEDURE MANUAL
UNIVERSITY HEALTH NETWORK / MOUNT SINAI HOSPITAL MICROBIOLOGY DEPARTMENT
NOTE: This is a CONTROLLED document. Any documents appearing in paper form that are not stamped in red "MASTER COPY" are not controlled and
should be checked against the document (titled as above) on the server prior to use
D:\106748206.doc
Policy # MI/MD/v50
Microbiology Department
Policy & Procedure Manual
Section: Molecular Diagnostic Tests Manual
Page 262 of
291
APPENDIX VI - General PCR Precautions and Decontamination Procedures
General PCR Precautions:
There must be separate PCR work areas:
Clean room
Specimen preparation room
Amplification room
Workflow must proceed in a uni-directional manner beginning in the clean room area and
moving to the amplification area.
Supplies and equipment must be dedicated to each area and not used for other activities or
moved between areas.
Change laboratory coat and gloves between work areas.
Wear powder-free gloves at all times. Hands and dust particles may carry bacteria and molds
and are the most common sources of Rnase contamination.
All reagents and master mixes must be prepared and stored in the clean room.
Use sterile aerosol resistant pipette tips.
Use 1% sodium hypochloride or Eliminase to disinfect equipment and surfaces
and then rinse with 70% alcohol or water.
Racks, surfaces and equipment that can be cleaned are cleaned daily.
PROCEDURE MANUAL
UNIVERSITY HEALTH NETWORK / MOUNT SINAI HOSPITAL MICROBIOLOGY DEPARTMENT
NOTE: This is a CONTROLLED document. Any documents appearing in paper form that are not stamped in red "MASTER COPY" are not controlled and
should be checked against the document (titled as above) on the server prior to use
D:\106748206.doc
Policy # MI/MD/v50
Microbiology Department
Policy & Procedure Manual
Section: Molecular Diagnostic Tests Manual
Page 263 of
291
Decontamination Procedure:
When contamination occurs the following steps must be followed:
Use 1% sodium hypochlorite followed by alcohol (water) to decontaminate.
Change into clean lab coat
Begin cleaning in the clean room and end in the amplification room.
Discard all reagents and disposable items (eg. pipette tips, capillary caps)
Clean biological safety cabinet, equipment and surfaces.
For WNV PCR decontamination, see checklist below.
WNV Decontamination Procedure:
Clean room:
Discard pipette tips, capillaries, caps, pens and eppendorf tubes
Clean biological safety cabinet, pipettors, racks and capper
Turn UV light on in the safety cabinet
Specimen preparation area:
Discard pipette tips, caps, pens, and reagents (AW1, AW2, alcohol, elution buffer and lysing
buffer)
Clean:
Biological safety cabinet
Pipettors and holder
Racks
Vortex
Centrifuge
Timer
Bench
Capillary capper
Amplification area:
Clean:
Microwave
Capillary centrifuge
Capillary carousel
Light Cycler
PROCEDURE MANUAL
UNIVERSITY HEALTH NETWORK / MOUNT SINAI HOSPITAL MICROBIOLOGY DEPARTMENT
NOTE: This is a CONTROLLED document. Any documents appearing in paper form that are not stamped in red "MASTER COPY" are not controlled and
should be checked against the document (titled as above) on the server prior to use
D:\106748206.doc
Policy # MI/MD/v50
Microbiology Department
Policy & Procedure Manual
Section: Molecular Diagnostic Tests Manual
Page 264 of
291
Perform wipe tests on all 3 areas:
Clean room: biological safety cabinet, pipettors, racks and capper
Specimen preparation area: Biological safety cabinet
Pipettors and holder
Racks
Vortex
Centrifuge
Timer
Bench
Capillary capper
Clean room:
Microwave
Capillary centrifuge
Capillary carousel
Light Cycler
If any wipe test is positive, repeat cleaning procedure for that area.
PROCEDURE MANUAL
UNIVERSITY HEALTH NETWORK / MOUNT SINAI HOSPITAL MICROBIOLOGY DEPARTMENT
NOTE: This is a CONTROLLED document. Any documents appearing in paper form that are not stamped in red "MASTER COPY" are not controlled and
should be checked against the document (titled as above) on the server prior to use
D:\106748206.doc
Policy # MI/MD/v50
Microbiology Department
Policy & Procedure Manual
Section: Molecular Diagnostic Tests Manual
Page 265 of
291
Appendix VII: Creating Standard Curve for Quantitative PCRs
Create standard curve for PCR: CMV, BKV, and EBV
Standard curves are created every 6 months, or as needed; recalibration of a standard curve may be
required.
Materials
CMV PCR Kit, Altona Diagnostics
BKV PCR Kit, Altona Diagnostics
EBV PCR Kit, Altona Diagnostics
Variable pipettes: 1-20uL
Aerosol resistant tips (ART) 20uL
0.01 microtubes and caps
eppendroff epMotion 5075 (benchtop robotic pipettor)
Procedure:
1. In the Clean Room prepare master mix for the standard curve PCR reaction; 12 reactions are
required to create a standard curve. Make 13 reactions (12 + 1), to load on the epMotion 5075.
2. In the processing area thaw the Quantitative Standards: QS1, QS2, QS3, QS4.
3. Use the epMotion 5075 to pipette the master mix into the PCR reaction microtubes. See
Appendix I.
4. Once the master mix is pipetted. Manually pipette 10uL of the Quantitative Standard (QS) into
the master mix in the following order:
Position
1
2
3
4
5
6
7
8
9
10
11
12
QS4 QS4 QS4 QS3 QS3 QS3 QS2 QS2 QS2 QS1 QS1 QS1
Do not add internal control (IC) to the reaction microtubes. Only the target Green channel will be
analyzed. Do not load a negative/PCR water control.
5. After the QSs’ has been added to the master mix cap the PCR reaction microtubes. Load the
Rotorgene. Identify each quantitative standard (QS) as sample type Standard and remember to
enter the concentration of the QSs’ under “Given Conc.” in the Edit Samples window. The QS
concentrations are on the QS sample vials.
6. Name the file as Standard curve and save into the Standard curve (STD) folder. For example:
CMV STD yyyymmdd. My documents… STD folder.
7. When the PCR reaction is complete. Select Analysis, each quantitative standard (QS) will have
three curves. Make sure “Name on” has been selected. Select Slope correct, and Ignore first 5
Cycles; create a threshold.
PROCEDURE MANUAL
UNIVERSITY HEALTH NETWORK / MOUNT SINAI HOSPITAL MICROBIOLOGY DEPARTMENT
NOTE: This is a CONTROLLED document. Any documents appearing in paper form that are not stamped in red "MASTER COPY" are not controlled and
should be checked against the document (titled as above) on the server prior to use
D:\106748206.doc
Policy # MI/MD/v50
Microbiology Department
Policy & Procedure Manual
Section: Molecular Diagnostic Tests Manual
Page 266 of
291
8. Observe the Quant. Results chart window, paying attention to the Given Conc. Column and the
Calc. Conc. Column (calculate concentration column). Look on the Analysis Green Channel
Graph deselect QS curves that cause the calculated concentration of the standard to be far from
the given concentration of the standard. The objective is to have the calculated concentration of
the standards be as close to the given concentration of the standards on the quantitative results
chart. When satisfied save the standard curve run.
9. Clean Up:
10. Place PCR reaction microtubes in a bag, seal shut, and discard into the biohazard waste
containers.
11. Clean Rotorgene rotors and locking rings with Kimwipe dampen with RNAseAway, followed
with Kimwipe dampened with distilled water, and then a Kimwipe dampen with 70% alcohol.
12. Complete daily equipment maintenance, as outlined in RotorGene Maintenance schedule.
PROCEDURE MANUAL
UNIVERSITY HEALTH NETWORK / MOUNT SINAI HOSPITAL MICROBIOLOGY DEPARTMENT
NOTE: This is a CONTROLLED document. Any documents appearing in paper form that are not stamped in red "MASTER COPY" are not controlled and
should be checked against the document (titled as above) on the server prior to use
D:\106748206.doc
Policy # MI/MD/v50
Microbiology Department
Policy & Procedure Manual
Section: Molecular Diagnostic Tests Manual
Page 267 of
291
Appendix VIII - Instructions for Pipetting by epMOTION
Instructions for Pipetting One Test on epMOTION
NOTE:
It takes about 30 minutes (15 samples), from putting the gloves on, removing specimens from the
freezer, making up the Master Mix, loading the epMotion, epMotion at work, loading the Rotorgene
and scanning specimens numbers onto the Rotorgene.
It takes the epMotion 20 minutes to pipette Master Mix only for 30 samples.
40 Minutes, excluding setup, to pipette both Master Mix and samples for about 70 samples.
You can prepare the Master Mix slightly ahead of time. Load the Master Mix, and samples and start
pipetting before the first extraction is finished. Pause (by clicking the Red Button on the left side)
the epMotion either right after pipetting the Master Mix or after it pipetted the last sample, to load
the rest of the specimens after the extraction is finished and finish the pipetting to save time.
Press the Green Arrow without the line, (the lower one) to CONTINUE the pipetting.
REMEMBER TO SPIKE THE QS, POSITIVE CONTROL AND WATER WITH IC
1. Turn on switches in the sequence for computer/epMotion/monitor, wait until the short cut for
epBlue Server appears on the bottom left side of the screen.
2. Double click the short cut for “epBlue Client” in the center of the screen
3. Type “msh” in both Account and password, click log in
4. Click “Home” tab
5. Click “Open/run Applications” from the bottom Task Card
6. “Open/Run applications” window pops up, make sure the following items are selected:
i.
“msh” under user
ii.
“(msh)” under Folder
iii.
Select and right click
PROCEDURE MANUAL
UNIVERSITY HEALTH NETWORK / MOUNT SINAI HOSPITAL MICROBIOLOGY DEPARTMENT
NOTE: This is a CONTROLLED document. Any documents appearing in paper form that are not stamped in red "MASTER COPY" are not controlled and
should be checked against the document (titled as above) on the server prior to use
D:\106748206.doc
Policy # MI/MD/v50
Microbiology Department
Policy & Procedure Manual
Section: Molecular Diagnostic Tests Manual
Page 268 of
291
a) “OtherVirus Rotorgene.dws” under Applications for CMV, BKV, HSV/VSV, EBV,
PARVO and ADENO;
b) “Flu Rotorgene.dws” for H1N1, RSV A/B and ParaInfluenza.
iv.
Click “Copy”
v.
Click “Daily Run”
vi.
Click the scissors icon in the Application pane and click “Paste”
vii.
Click “Edit Properties”
viii. Change the “Name” from “Other Virus Rotorgene.dws” to Virus type and todays date
(run #) e.g. CMV 2011-08-26 (1)
7. Click “Save” button
8. Double click on the file just created in (6 viii) in the Application pane or click Open Application
with cursor on the file e.g. CMV 2011-08-26 (1).dws
9. If the following window does not pops up, click the “Run” tab. Make sure “Filter Devicelist” is
checked.
PROCEDURE MANUAL
UNIVERSITY HEALTH NETWORK / MOUNT SINAI HOSPITAL MICROBIOLOGY DEPARTMENT
NOTE: This is a CONTROLLED document. Any documents appearing in paper form that are not stamped in red "MASTER COPY" are not controlled and
should be checked against the document (titled as above) on the server prior to use
D:\106748206.doc
Policy # MI/MD/v50
Microbiology Department
Policy & Procedure Manual
Section: Molecular Diagnostic Tests Manual
Page 269 of
291
10. Load the microtubes into the cooling block according to diagram:
11. Prepare the mastermix in the 1.5mL snapcap conical microtubes and placed in first position of
PROCEDURE MANUAL
UNIVERSITY HEALTH NETWORK / MOUNT SINAI HOSPITAL MICROBIOLOGY DEPARTMENT
NOTE: This is a CONTROLLED document. Any documents appearing in paper form that are not stamped in red "MASTER COPY" are not controlled and
should be checked against the document (titled as above) on the server prior to use
D:\106748206.doc
Policy # MI/MD/v50
Microbiology Department
Policy & Procedure Manual
Section: Molecular Diagnostic Tests Manual
Page 270 of
291
12. the Reagents Rack.
13. Press the microtube down firmly so that it sits flushed with the top of rack
14. Place samples column-wise in Sample Racks labeled “Sample 1-24” according to the worklist
including necessary controls. Subsequent samples may be placed in “Sample 25-28” and
“Sample 49-72” for a maximum of 72 reactions.
15. Close the epMotion hood firmly. You should hear a click.
16. Click “Run>>” button.
PROCEDURE MANUAL
UNIVERSITY HEALTH NETWORK / MOUNT SINAI HOSPITAL MICROBIOLOGY DEPARTMENT
NOTE: This is a CONTROLLED document. Any documents appearing in paper form that are not stamped in red "MASTER COPY" are not controlled and
should be checked against the document (titled as above) on the server prior to use
D:\106748206.doc
Page 271 of
291
Policy # MI/MD/v50
Microbiology Department
Policy & Procedure Manual
Section: Molecular Diagnostic Tests Manual
17. The Process Control window pops up
18. Enter the total number of reactions including controls over the highlighted ”1”.
19. Click “OK”
20. Cancel the level sensing for Levels and Location. Keep the level sensing for Tips.
21. Keep clicking the “RUN>>” button until the “MasterMix A+B” window shows up
*
22. At the “Labware information” menu, enter the number “*” shown in the “Minimum Volume”
column in the ““Volume” column highlighted with
23. Click “Run>>”
24. Close the run by highlighting the run, right click and click “Close”.
PROCEDURE MANUAL
UNIVERSITY HEALTH NETWORK / MOUNT SINAI HOSPITAL MICROBIOLOGY DEPARTMENT
NOTE: This is a CONTROLLED document. Any documents appearing in paper form that are not stamped in red "MASTER COPY" are not controlled and
should be checked against the document (titled as above) on the server prior to use
D:\106748206.doc
Policy # MI/MD/v50
Microbiology Department
Policy & Procedure Manual
Section: Molecular Diagnostic Tests Manual
Page 272 of
291
25. Wipe down the blocks and the epMotion with RNase AWAY, distilled water, alcohol and
distilled water in the above sequence.
26.Turn off the Computer/computer switch/epMotion/Monitor
Instruction For Pipetting Two Or More Tests On Epmotion:
1. Turn on switches in the sequence for computer/epMotion/monitor, wait until the short cut for
epBlue Server appears on the bottom left side of the screen.
2. Double click the short cut for “epBlue Client” in the center of the screen
3. Type “msh” in both Account and password, click log in
4. Click “Home” tab
5. Click “Open/run Applications” from the bottom Task Card
6. “Open/Run applications” window pops up, make sure the following items are selected:
i.
“msh” under user
ii.
“(msh)” under Folder
iii.
Select and right click
iv.
Select and right click
a) “OtherVirus Rotorgene.dws” under Applications for CMV, BKV, HSV/VSV, EBV,
PARVO and ADENO;
b) “Flu Rotorgene.dws” for H1N1, RSV A/B and ParaInfluenza.
v.
Click “Copy”
vi.
Click “Daily Run”
vii.
Click the scissors icon in the Application pane and click “Paste”
viii. Click “Edit Properties”
ix.
Change the “Name” from “Other Virus Rotorgene.dws” to Virus type and todays date
(run #) e.g. CMV 2011-08-26 (1)
PROCEDURE MANUAL
UNIVERSITY HEALTH NETWORK / MOUNT SINAI HOSPITAL MICROBIOLOGY DEPARTMENT
NOTE: This is a CONTROLLED document. Any documents appearing in paper form that are not stamped in red "MASTER COPY" are not controlled and
should be checked against the document (titled as above) on the server prior to use
D:\106748206.doc
Policy # MI/MD/v50
Microbiology Department
Policy & Procedure Manual
Section: Molecular Diagnostic Tests Manual
Page 273 of
291
PROCEDURE MANUAL
UNIVERSITY HEALTH NETWORK / MOUNT SINAI HOSPITAL MICROBIOLOGY DEPARTMENT
NOTE: This is a CONTROLLED document. Any documents appearing in paper form that are not stamped in red "MASTER COPY" are not controlled and
should be checked against the document (titled as above) on the server prior to use
D:\106748206.doc
Policy # MI/MD/v50
Microbiology Department
Policy & Procedure Manual
Section: Molecular Diagnostic Tests Manual
Page 274 of
291
7. Click “Save” button.
8. i)
RSV can be pipetted right after the FLU;
ii)
PARVO, ADENO can be pipetted after HSV/VZV.
9. Create the second or third test as above, edit the name and save with the corresponding “TEST
NAME date”
10. Double click on the file (the new file i.e. the second or third file) just created in (6 viii) in the
Application pane. e.g. RSV 2011-08-26 (1).dws
11. Click the “Procedure” Tab on the left side.
12. Click on the “Master Mix Dispense” –#3
i) Click “New Pattern” on the bottom left corner.
a) Click the highlighted circle, the placement of the second Master Mix.
b) Click 2 consecutive circles on the samples “Cooling block” to indicate the direction the
Master mix are to be dispensed
PROCEDURE MANUAL
UNIVERSITY HEALTH NETWORK / MOUNT SINAI HOSPITAL MICROBIOLOGY DEPARTMENT
NOTE: This is a CONTROLLED document. Any documents appearing in paper form that are not stamped in red "MASTER COPY" are not controlled and
should be checked against the document (titled as above) on the server prior to use
D:\106748206.doc
Policy # MI/MD/v50
Microbiology Department
Policy & Procedure Manual
Section: Molecular Diagnostic Tests Manual
Page 275 of
291
13. Click on the “Sample dispense” #5
i) Click “New Pattern” on the bottom left corner.
a) Click the highlighted circle, the placement of the second Master Mix.
b) Click 2 consecutive circles on the samples “Cooling block” to indicate the direction the
Master mix are to be dispensed
14. Click “File” then “Save”.
15. Click the first test to be dispensed.
16. Run the first test until it is completed.
17. Close the window by right click and close the first run.
18. Start the second run by clicking on the run.
PROCEDURE MANUAL
UNIVERSITY HEALTH NETWORK / MOUNT SINAI HOSPITAL MICROBIOLOGY DEPARTMENT
NOTE: This is a CONTROLLED document. Any documents appearing in paper form that are not stamped in red "MASTER COPY" are not controlled and
should be checked against the document (titled as above) on the server prior to use
D:\106748206.doc
Policy # MI/MD/v50
Microbiology Department
Policy & Procedure Manual
Section: Molecular Diagnostic Tests Manual
Page 276 of
291
19. If the following window does not pops up, click the “Run” tab. Make sure “Filter Devicelist” is
checked.
20. Load the microtubes into the cooling block according to diagram:
PROCEDURE MANUAL
UNIVERSITY HEALTH NETWORK / MOUNT SINAI HOSPITAL MICROBIOLOGY DEPARTMENT
NOTE: This is a CONTROLLED document. Any documents appearing in paper form that are not stamped in red "MASTER COPY" are not controlled and
should be checked against the document (titled as above) on the server prior to use
D:\106748206.doc
Policy # MI/MD/v50
Microbiology Department
Policy & Procedure Manual
Section: Molecular Diagnostic Tests Manual
Page 277 of
291
21. Prepare the mastermix in the 1.5mL snapcap microtubes and placed in first position of the
Reagents Rack.
22. Press the microtube down firmly so that it sits flushed with the top of rack
23. Place samples column-wise in Sample Racks labeled “Sample 1-24” according to the worklist
including necessary controls. Subsequent samples may be placed in “Sample 25-28” and
“Sample 49-72” for a maximum of 72
reaction
24. Close the epMotion hood firmly. You should hear a click.
25. Click “Run>>” button.
PROCEDURE MANUAL
UNIVERSITY HEALTH NETWORK / MOUNT SINAI HOSPITAL MICROBIOLOGY DEPARTMENT
NOTE: This is a CONTROLLED document. Any documents appearing in paper form that are not stamped in red "MASTER COPY" are not controlled and
should be checked against the document (titled as above) on the server prior to use
D:\106748206.doc
Page 278 of
291
Policy # MI/MD/v50
Microbiology Department
Policy & Procedure Manual
Section: Molecular Diagnostic Tests Manual
26. The Process Control window pops up
27. Enter the total number of reactions including controls over the highlighted ”1”.
28. Click “OK”
29. Cancel the level sensing for Levels and Location. Keep the level sensing for Tips.
30. Keep clicking the “RUN>>” button until the “MasterMix A+B” window shows up
*
31. At the “Labware information” menu, enter the number “*” shown in the “Minimum Volume”
column in the ““Volume” column highlighted with
32. Click “Run>>”.
33. Close the run by highlighting the run, right click and click “Close”.
PROCEDURE MANUAL
UNIVERSITY HEALTH NETWORK / MOUNT SINAI HOSPITAL MICROBIOLOGY DEPARTMENT
NOTE: This is a CONTROLLED document. Any documents appearing in paper form that are not stamped in red "MASTER COPY" are not controlled and
should be checked against the document (titled as above) on the server prior to use
D:\106748206.doc
Policy # MI/MD/v50
Microbiology Department
Policy & Procedure Manual
Section: Molecular Diagnostic Tests Manual
Page 279 of
291
34. Wipe down the blocks and the epMotion with RNase AWAY, distilled water, alcohol and
distilled water in the above sequence.
35. Turn off the Computer/computer switch/epMotion/Monitor
PROCEDURE MANUAL
UNIVERSITY HEALTH NETWORK / MOUNT SINAI HOSPITAL MICROBIOLOGY DEPARTMENT
NOTE: This is a CONTROLLED document. Any documents appearing in paper form that are not stamped in red "MASTER COPY" are not controlled and
should be checked against the document (titled as above) on the server prior to use
D:\106748206.doc
Policy # MI/MD/v50
Microbiology Department
Policy & Procedure Manual
Section: Molecular Diagnostic Tests Manual
Page 280 of
291
Appendix IX – RotorGene Worksheet
Forms_Worksheets\RotorGene Worksheet MI_MD_06_09
PROCEDURE MANUAL
UNIVERSITY HEALTH NETWORK / MOUNT SINAI HOSPITAL MICROBIOLOGY DEPARTMENT
NOTE: This is a CONTROLLED document. Any documents appearing in paper form that are not stamped in red "MASTER COPY" are not controlled and
should be checked against the document (titled as above) on the server prior to use
D:\106748206.doc
Policy # MI/MD/v50
Microbiology Department
Policy & Procedure Manual
Section: Molecular Diagnostic Tests Manual
Page 281 of
291
Appendix X – RotorGene Calculations for Reports
RotorGene Calculations for Reports MI_MD_06_10
PROCEDURE MANUAL
UNIVERSITY HEALTH NETWORK / MOUNT SINAI HOSPITAL MICROBIOLOGY DEPARTMENT
NOTE: This is a CONTROLLED document. Any documents appearing in paper form that are not stamped in red "MASTER COPY" are not controlled and
should be checked against the document (titled as above) on the server prior to use
D:\106748206.doc
Policy # MI/MD/v50
Microbiology Department
Policy & Procedure Manual
Section: Molecular Diagnostic Tests Manual
Page 282 of
291
Appendix XI – Rotorgene Optical Temperature Verification (OTV) Procedure
I.
II.
III.
Introduction:
Optical Temperature Verification (OTV) Kit uses 3 thermochromic liquid crystals (TLCs) optical
properties to verify the temperature of the RotorGene real-time cyclers. When heated the thermochromic
liquid crystals change from opaque to transparent at very precise temperatures (50oC, 70oC, and 90oC).
The thermochromic liquid crystals do not fluoresce, and it is necessary to cover the excitation source
with a fluorescence scatter plate allowing the liquid crystal temperature transition points to be detected.
The temperature transition reported by the RotorGene cycler is compared to the temperature encoded in
the OTV Rotor-Disc serial number. Every batch of thermochromic liquid crystals has specific melting
temperatures encoded in the OTV Rotor-Disc serial number. If the instrument is not within temperature
specifications, automatic recalibration of the RotorGene can be performed by selecting “Apply
Adjustment” in the OTV Temperature Verification Results window. Optical Temperature Verification
(OTV) should be performed every 6 months.
Equipment:
RotorGene 6000
Rotor-Disc 72 Rotor and Rotor-Disc 72 Locking Ring
Rotor-Disc OTV Kit (Qiagen catalog no. 981400) Store at Room Temperature (15-25oC). Keep OTV
Rotor-Disc away from light. Can be used a maximum of 30 times until expiration kit date.
Procedure:
Place the large green fluorescent insert over the excitation lens –bottom right of the RotorGene cycler.
Place the OTV Rotor-Disc into the Rotor-Disc 72 Rotor. Ensure that the disc is properly aligned in the
rotor; the locator tab on the disc must be seated into the slot on the rotor.
PROCEDURE MANUAL
UNIVERSITY HEALTH NETWORK / MOUNT SINAI HOSPITAL MICROBIOLOGY DEPARTMENT
NOTE: This is a CONTROLLED document. Any documents appearing in paper form that are not stamped in red "MASTER COPY" are not controlled and
should be checked against the document (titled as above) on the server prior to use
D:\106748206.doc
Policy # MI/MD/v50
Microbiology Department
Policy & Procedure Manual
Section: Molecular Diagnostic Tests Manual
Page 283 of
291
Attach the locking ring. Load the Rotor with OTV disc into the RotorGene 6000.
Select the RotorGene 6000 icon to open the RotorGene 6000 application.
New Run Window. Select Advanced (this menu tab should be the default).
Select Instrument Maintenance.
PROCEDURE MANUAL
UNIVERSITY HEALTH NETWORK / MOUNT SINAI HOSPITAL MICROBIOLOGY DEPARTMENT
NOTE: This is a CONTROLLED document. Any documents appearing in paper form that are not stamped in red "MASTER COPY" are not controlled and
should be checked against the document (titled as above) on the server prior to use
D:\106748206.doc
Policy # MI/MD/v50
Microbiology Department
Policy & Procedure Manual
Section: Molecular Diagnostic Tests Manual
Page 284 of
291
Select OTV.
The program will prompt for the OTV Rotor-Disc serial number.
Insert the CD provided with each OTV Kit and select the Browse.
Select the OTV calibration file provided on the CD (*.otv file). The serial number and be imported from
the OTV calibration file on the CD. (Alternatively the serial number can be read from the label on the
OTV Rotor-Disc.)
Ensure the check box for “Fluorescent insert placed correctly” is marked off; and the insert is in
place.
Save the run file in My Documents > OTV folder > OTV-lot.number _yyyy-mm-dd
PROCEDURE MANUAL
UNIVERSITY HEALTH NETWORK / MOUNT SINAI HOSPITAL MICROBIOLOGY DEPARTMENT
NOTE: This is a CONTROLLED document. Any documents appearing in paper form that are not stamped in red "MASTER COPY" are not controlled and
should be checked against the document (titled as above) on the server prior to use
D:\106748206.doc
Policy # MI/MD/v50
Microbiology Department
Policy & Procedure Manual
Section: Molecular Diagnostic Tests Manual
Page 285 of
291
The run begins. The OTV run performs a series of melts that determine the thermal characteristics of the
RotorGene Cycler. The total run time is approximately 45 minutes.
When the run is completed. OTV Temperature Verification Results window will appear indicating if
“No Adjustments are required.” Select Report and print for filing in Equipment binder. Record, with
inital, that Optical Temperature Verification OTV was performed in the Analyzer History Log
RotorGene.
Or
“Adjustments Required”. Select Apply Adjustments. This will prompt for a verification run; after
the verification run no further adjustments should be required. Select Report and print. Record, with
inital, that Optical Temperature Verification OTV was performed in the Analyzer History Log
RotorGene.
If further adjustment is required inform seniors/and Charge.
Contact:
Montreal BioTech Inc.
75 Guthrie, Suite202
Dorval, QC H9P 2P1
PH: 514-697-2312
References:
Qiagen Rotor-Disc OTV Handbook, January 2011
PROCEDURE MANUAL
UNIVERSITY HEALTH NETWORK / MOUNT SINAI HOSPITAL MICROBIOLOGY DEPARTMENT
NOTE: This is a CONTROLLED document. Any documents appearing in paper form that are not stamped in red "MASTER COPY" are not controlled and
should be checked against the document (titled as above) on the server prior to use
D:\106748206.doc
Policy # MI/MD/v50
Microbiology Department
Policy & Procedure Manual
Section: Molecular Diagnostic Tests Manual
Page 286 of
291
Appendix XII – WNV PCR Procedure Abbreviated *
(In clean room)
1. Add 560uL Lysis buffer into 5.6 uL cRNA microcentrifuge tubes
(In hood)
1. Add 140 uL specimen to Lysis buffer, vortex 15 seconds
2. Incubate for 10 minutes at room temperature
3. Centrifuge for 10 seconds at 3000 rpm to remove drops from lid
4. Change gloves
5. Add 6uL WNV internal control
6. Add 560uL ethanol (96-100%), vortex 15 seconds
7. Centrifuge for 10 seconds at 3000 rpm to remove drops from lid
8. Change gloves
9. Add 630 uL to the spin column, centrifuge for 1 minute at 8000 rpm
10. Discard filtrate in collection tube and transfer spin column to a new collection tube
11. Add remaining 630 uL to spin column, centrifuge for 1 minute at 8000 rpm
12. Discard filtrate in collection tube and transfer spin column to a new collection tube
13. Change gloves
14. Add 500 uL of Buffer AW1, centrifuge for 1 minute at 8000 rpm
15. Discard filtrate in collection tube and transfer spin column to a new collection tube
16. Add 500 uL of Buffer AW2, centrifuge for 3 minutes at 14,000 rpm
17. Discard filtrate in collection tube and transfer spin column to a new collection tube
18. Dry spin for 3 minutes at 14,000 rpm
19. Discard filtrate in collection tube and place spin column in clean microcentrifuge tube
20. Add 60 uL of Elution Buffer. Incubate for 1 minute at room temp
21. Centrifuge for 1 minute at 8000 rpm.
22. Store the eluate at -20C if not using immediately
* Abbreviated version for bench quick reference only. For complete manual, please refer to
WNV PCR by ALTONA KIT v. 1.0 and ROTORGENE
PROCEDURE MANUAL
UNIVERSITY HEALTH NETWORK / MOUNT SINAI HOSPITAL MICROBIOLOGY DEPARTMENT
NOTE: This is a CONTROLLED document. Any documents appearing in paper form that are not stamped in red "MASTER COPY" are not controlled and
should be checked against the document (titled as above) on the server prior to use
D:\106748206.doc
Policy # MI/MD/v50
Microbiology Department
Policy & Procedure Manual
Section: Molecular Diagnostic Tests Manual
Page 287 of
291
Record of Edited Revisions
Manual Section Name: Molecular Diagnostic Tests
Page Number / Item
Date of Revision
Signature of
Approval
Molecular Testing - HBV DNA-Reporting Added Para.
October 10, 2003
Annual Review
Page 67 - Molecular Testing - Chlamydia Trachomatis &
Neisseria gonorrhoeae
Page 67 – urine but not more than 60 mL added
Page 68 – specimen not lysed…added
Page 68 – tubes may be blotted
Page 70 – handling samples after lysing
Page 71,72 Procedure change
Page 72, interpretation of result - change MOTA score
Page 73, reporting – indeterminate
Page 76 – do not vortex working master mix
Page 76 – specimen dilution protocol
Page 77 – 80 procedure and reporting changed
Page 81 – QC procedure changed
Page 93 – procedure changed
Page 86 – 88, instrument instructions
Page 90 – WNV RT-PCR
Page 92 – lysis buffer
Page 93 – General Precaution section revised
Page 94-100 – procedure revised
Page 128 – Updated decontamination procedure
Annual Review
Added links to TGLN Procedures
Revised HBV-DNA and HCV-RNA procedures with
Ampliprep instructions
Procleix Ultrio and WNV added
Procleix Discriminatory Assay
Annual Review
CMV DNA Amplification and Detection Procedures
updated
Molecular Testing – updated
EBV DNA Amplification and Detection Procedures
updated
HSV DNA Amplification and Detection Procedures
updated
May 30, 2004
May 20, 2005
Dr. T. Mazzulli
Dr. T. Mazzulli
Dr. T. Mazzulli
May 20, 2005
May 20, 2005
May 20, 2005
May 20, 2005
May 20, 2005
May 20, 2005
May 20, 2005
May 20, 2005
May 20, 2005
May 20, 2005
May 20, 2005
May 20, 2005
May 20, 2005
May 20, 2005
May 20, 2005
May 20, 2005
May 20, 2005
June 2, 2005
May 30, 2006
March 21, 2007
May 11, 2008
Dr. T. Mazzulli
Dr. T. Mazzulli
Dr. T. Mazzulli
Dr. T. Mazzulli
Dr. T. Mazzulli
Dr. T. Mazzulli
Dr. T. Mazzulli
Dr. T. Mazzulli
Dr. T. Mazzulli
Dr. T. Mazzulli
Dr. T. Mazzulli
Dr. T. Mazzulli
Dr. T. Mazzulli
Dr. T. Mazzulli
Dr. T. Mazzulli
Dr. T. Mazzulli
Dr. T. Mazzulli
Dr. T. Mazzulli
Dr. T. Mazzulli
Dr. T. Mazzulli
Dr. T. Mazzulli
July 21, 2008
July 21, 2008
July 21, 2008
November 01, 2008
Dr. T. Mazzulli
Dr. T. Mazzulli
Dr. T. Mazzulli
Dr. T. Mazzulli
November 01, 2008
November 01, 2008
Dr. T. Mazzulli
Dr. T. Mazzulli
November 01, 2008
Dr. T. Mazzulli
PROCEDURE MANUAL
UNIVERSITY HEALTH NETWORK / MOUNT SINAI HOSPITAL MICROBIOLOGY DEPARTMENT
NOTE: This is a CONTROLLED document. Any documents appearing in paper form that are not stamped in red "MASTER COPY" are not controlled and
should be checked against the document (titled as above) on the server prior to use
D:\106748206.doc
Policy # MI/MD/v50
Microbiology Department
Policy & Procedure Manual
Section: Molecular Diagnostic Tests Manual
Page Number / Item
Parvovirus B19 DNA PCR Amplification and Detection
Procedures updated
Enterovirus RNA Amplification and Detection
Procdeures added
West Nile Virus RT PCR - Failed QC added
Annual Review
Annual Review
Added revised easyMag
Added revised CMV PCR
Added revised BKV PCR
GeneXpert C. difficile added
Updated Procleix Ultrio
Updated QC section of easyMag extraction
Updated Influenza procedure
Added Virology specimen accessioning guide link
Deleted CMV DNA Amplification and Detection
Procedures by Lightcycler
Deleted VZV Amplification and Detection Procedures by
Lightcycler
Deleted HSV Amplification and Detection Procedures by
Lightcycler
Added HSV/VZV Detection (Altona Alpha herpes)
Added Multiplex Respiratory virus detection
Annual Review
Parvovirus PCR revised
RSV PCR added
Replace Procleix with MPX
Updated WNV PCR with Altona kits
Annual Review
Added Appendix VIII - epMotion procedure
Added Appendix VII - Creating Standard Curve for
Quantitative PCRs
Added Links to RotorGene Worksheets and calculations
and reports
Chlamydia/Neisseria gonorrhoeae detection method
changed to Roche COBAS 4800
Appendix II to IV BD ProbeTec related documents
removed
Added HPV testing
Added Focus Simplexa Flu A/B and RSV testing
Date of Revision
Page 288 of
291
Signature of
Approval
November 01, 2008
Dr. T. Mazzulli
November 01, 2008
Dr. T. Mazzulli
July 10, 2009
July 31, 2009
July 31, 2010
August 23, 2010
August 23, 2010
October 31, 2010
January 10, 2011
April 14, 2011
May 31, 2011
May 31, 2011
May 31, 2011
May 31, 2011
Dr. T. Mazzulli
Dr. T. Mazzulli
Dr. T. Mazzulli
Dr. T. Mazzulli
Dr. T. Mazzulli
Dr. T. Mazzulli
Dr. T. Mazzulli
Dr. T. Mazzulli
Dr. T. Mazzulli
Dr. T. Mazzulli
Dr. T. Mazzulli
Dr. T. Mazzulli
May 31, 2011
Dr. T. Mazzulli
May 31, 2011
Dr. T. Mazzulli
May 31, 2011
May 31, 2011
May 31, 2011
May 31, 2011
May 31, 2011
September 11, 2011
June 13, 2012
June 13, 2012
June 13, 2012
June 13, 2012
Dr. T. Mazzulli
Dr. T. Mazzulli
Dr. T. Mazzulli
Dr. T. Mazzulli
Dr. T. Mazzulli
Dr. T. Mazzulli
Dr. T. Mazzulli
Dr. T. Mazzulli
Dr. T. Mazzulli
Dr. T. Mazzulli
June 13, 2012
Dr. T. Mazzulli
October 17, 2012
Dr. T. Mazzulli
October 17, 2012
Dr. T. Mazzulli
December 12, 2012
December 12, 2012
Dr. T. Mazzulli
Dr. T. Mazzulli
PROCEDURE MANUAL
UNIVERSITY HEALTH NETWORK / MOUNT SINAI HOSPITAL MICROBIOLOGY DEPARTMENT
NOTE: This is a CONTROLLED document. Any documents appearing in paper form that are not stamped in red "MASTER COPY" are not controlled and
should be checked against the document (titled as above) on the server prior to use
D:\106748206.doc
Policy # MI/MD/v50
Microbiology Department
Policy & Procedure Manual
Section: Molecular Diagnostic Tests Manual
Page Number / Item
Moved RotorGene Flu and RSV tests to Appendix II and
III for backup use
Renumbered procedures
Revised Positive C. diff resulting message
Espanded C. diff resulting messages
Realigned bullets and numbering format
Added Appendix XI WNV PCR Procedure abbreviated
Update QC & Maintenance for Focus Simplexa Flu A/B
and RSV testing
Annual Review
MPX procedure updates
Simplexa Flu A/B and RSV reporting procedure updated
Simplexa Flu A/B and RSV testing procedure updated
Addition of Appendix IV: Simplexa A/B/RSV worksheet
Manual Creation: Cobas Ampliprep/TaqMan CMV PCR
MI/MD/19/v01
Reporting C.diff GeneExpert Updating
C.diff reporting update, WNV PCR manual and WNV
PCR appreviated appendix dry spin time update.
Annual Review
Removed Luminex, HBV DNA, HCV RNA procedure
Updated MPX NAT to new version and in its own
manual as well as WNV NAT
Updated Virology accessioning chart to it’s own manual
Move Easymag manuals to Appendix
Updated APPENDIX I - Molecular Diagnostic Tests
Date of Revision
Page 289 of
291
Signature of
Approval
December 12, 2012
Dr. T. Mazzulli
December 12, 2012
February 05, 2013
April 18, 2013
July 31, 2013
July 31, 2013
July 31, 2013
Dr. T. Mazzulli
Dr. T. Mazzulli
Dr. T. Mazzulli
Dr. T. Mazzulli
Dr. T. Mazzulli
Dr. T. Mazzulli
July 31, 2013
December 9th, 2013
December 18,2013
January 15, 2014
January 24, 2014
February 21, 2014
Dr. T. Mazzulli
Dr. T. Mazzulli
Dr. T. Mazzulli
Dr. T. Mazzulli
Dr. T. Mazzulli
Dr. T. Mazzulli
April 14, 2014
May 28, 2014
Dr. T. Mazzulli
Dr. T. Mazzulli
November 3, 2014
Dr. T. Mazzulli
November 12, 2014
January 28, 2015
Dr. T. Mazzulli
Dr. T. Mazzulli
February 18, 2015
Dr. T. Mazzulli
February 26, 2015
March 15, 2015
Dr. T. Mazzulli
May 6, 2015
May 6, 2015
May 6, 2015
Dr. T. Mazzulli
Dr. T. Mazzulli
Dr. T. Mazzulli
Schedule
C. diff reporting update for results
Addition of :
Sputolysin Procedure and Stool preparation in
Virology Accessioning tables split and updated
Simplexa manual resulting updated.
Parainfluenza and human Metapneumovirus procedure
added
Update C.diff comments
Parainfluenza and human Metapneumovirus BIORAD
procedure added
Added C. diff with eSwab section
Added links for BK/EBV to calculation excel worksheet
p.8 BK general precautions modified
PROCEDURE MANUAL
UNIVERSITY HEALTH NETWORK / MOUNT SINAI HOSPITAL MICROBIOLOGY DEPARTMENT
NOTE: This is a CONTROLLED document. Any documents appearing in paper form that are not stamped in red "MASTER COPY" are not controlled and
should be checked against the document (titled as above) on the server prior to use
D:\106748206.doc
Policy # MI/MD/v50
Microbiology Department
Policy & Procedure Manual
Section: Molecular Diagnostic Tests Manual
Page Number / Item
Added introduction and specimen collection/transport to
BKV section and updated materials section
Adenovirus PCR by Rotorgene Section Added in
Added:
ROTORGENE QC
Semi-Annual: Perform optical temperature verification
Annual Review
Added Appendix XI – Rotorgene Optical Temperature
Verification (OTV) Procedure
Added link in WNV PCR to OTV Procedure
Added PCR ordering chart to accessioning section
Updated BK Virus procedure
Updated BK Manual section,
Updated full EBV manual
BK and EBV manual addition of summary information
South West Health Ordering information added to PCR
accessing chart.
Virology specimen accessioning guide changes:
-add tx pt to edta for hz,
-add pleural to peritoneal/pericardial fluids (entero)
-removed “if requested” Entero from BALs
-removed adeno to PHL from eye specimens (done in
house)
Influenza Simplexa section:
- added report using virology worklist Respiratory PCR
- Error EC500 retest 1:10
- Add media PRABR if retesting simplexa sample
- Add dates in media PCABR
WNV Rotorgene:
- Removed use of 72-well rotor parts
- Document which rotorgene was used (blue or red)
- Removed Red Channel RSV A (typo) p.172
- Reporting section: note for positives to re-extract from
original clot and re run, for donors repeat in duplicates &
record CT values in PCWNV media.
-Updated troubleshooting section Influenza Simplexa
manual & added instructions for insufficient sample
error.
-Reorganize manuals alphabetically
Date of Revision
Page 290 of
291
Signature of
Approval
May 6, 2015
Dr. T. Mazzulli
May 6, 2015
June 15, 2015
Dr. T. Mazzulli
Dr. T. Mazzulli
June 15, 2015
Dr. T. Mazzulli
June 25, 2015
July 16, 2015
Dr. T. Mazzulli
Dr. T. Mazzulli
August 12, 2015
Dr. T. Mazzulli
September 1, 2015
Dr. T. Mazzulli
September 11, 2015
Dr. T. Mazzulli
September 25, 2015
Dr. T. Mazzulli
PROCEDURE MANUAL
UNIVERSITY HEALTH NETWORK / MOUNT SINAI HOSPITAL MICROBIOLOGY DEPARTMENT
NOTE: This is a CONTROLLED document. Any documents appearing in paper form that are not stamped in red "MASTER COPY" are not controlled and
should be checked against the document (titled as above) on the server prior to use
D:\106748206.doc
Policy # MI/MD/v50
Microbiology Department
Policy & Procedure Manual
Section: Molecular Diagnostic Tests Manual
Page Number / Item
Date of Revision
Page 291 of
291
Signature of
Approval
Under trouble shooting section of manuals: MPX NAT,
WNV NAT, Chlamydia PCR added to the table if IC
fails:
First time: repeat
Second time: result as invalid with result comment
@SPIN “Likely due to specimen integrity, unable to
obtain valid test result after repeated attempts.”
Added BK BIO RAD section
Virology Accessioning Chart changes: Adeno request for
stool send to PHL, parvo request on plasma: requires
microbiologist approval
Under Virology ordering chart added link to Send out
Manual for processing specimens to be send for external
testing.
October 7, 2015
Dr. T. Mazzulli
October 15, 2015
Dr. T. Mazzulli
October 20, 2015
Dr. T. Mazzulli
Updated MPX NAT and WNV NAT to include storage
temperature of reagents
Updated WNV storage conditions of specimen
October 26, 2015
Dr. T. Mazzulli
PROCEDURE MANUAL
UNIVERSITY HEALTH NETWORK / MOUNT SINAI HOSPITAL MICROBIOLOGY DEPARTMENT
NOTE: This is a CONTROLLED document. Any documents appearing in paper form that are not stamped in red "MASTER COPY" are not controlled and
should be checked against the document (titled as above) on the server prior to use
D:\106748206.doc