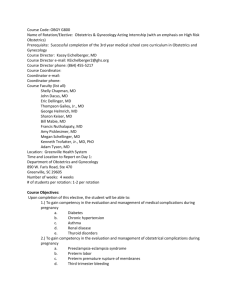
Dr_Said_s_abstract
advertisement

THROMBOPHILIAS AND ADVERSE PREGNANCY OUTCOME Said JM, Higgins JR, Walker SP, Monagle PA, Brennecke SP Royal Women’s Hospital Melbourne Over the past decade, a number of inherited and acquired conditions (Box 1) have been identified which predispose particular groups of patients to an increased risk of thrombosis. The identification of these conditions, collectively referred to as thrombophilias, has greatly altered the investigation and counselling of patients presenting with venous thromboembolism. Venous thromboembolism has long been recognised as a major cause of maternal morbidity and mortality. Pregnancy itself has been recognised as a procoagulant state and the additional impact of a thrombophilia may well tip the balance towards thrombosis in an otherwise healthy pregnant woman. Despite the extreme seriousness of venous thromboembolism in pregnancy, the condition remains relatively rare occurring in approximately 1 per 1000 pregnancies. 1 By contrast, pregnancy complications such as recurrent miscarriages, pre-eclampsia, fetal growth restriction, placental abruption and stillbirth are far more common and affect up to 10% of pregnancies. These conditions have significant implications not only on maternal and perinatal morbidity and mortality but also on long term adult outcomes of affected fetuses. Excessive uteroplacental thrombosis has been proposed as the pathogenic mechanism leading to these obstetric complications. Histopathologic assessment of placentas from pre-eclamptic pregnancies and pregnancies complicated by fetal growth restriction and unexplained stillbirth have demonstrated the presence of mural thrombi within both the maternal and fetal circulations2. In addition, activation of the coagulation cascade in the uteroplacental circulation of preeclamptic patients has been demonstrated.3 The various pregnancy related changes in the uteroplacental circulation make this region of the vascular system vulnerable to the development of intravascular thrombosis in patients who may have an additional risk factor predisposing them to thrombosis. The association between inherited thrombophilias and adverse pregnancy outcome has been debated over the past decade. Since the earliest reports, including those by Dekker and colleagues of an increased rate of thrombophilia in patients with severe pre-eclampsia,4 there have been numerous case control studies which both affirm5-7 and refute this association.8-10 Systematic reviews11, 12 on the topic continue to be constrained by the different study populations used (differing clinical definitions), range of thrombophilias tested, ethnic differences and publication bias, which can all contribute to skewed results which may not necessarily be applicable to all populations and all patients with adverse pregnancy outcomes. Despite this, a recent meta-analysis has once again confirmed an association between thrombophilias and adverse pregnancy outcomes including early and late pregnancy loss, pre-eclampsia, placental abruption, and fetal growth restriction.13 Furthermore, there is growing evidence that the presence of thrombophilic defects is associated with a greater severity of obstetric complications including earlier onset disease and more severe adverse perinatal outcomes.14, 15 However, despite these apparent associations, we still have very little information on which to base therapeutic interventions. The early trials of combinations of aspirin and heparin in patients with the antiphospholipid syndrome demonstrated significant improvements in the live-birth rate.16 Whether it is safe to translate these findings to populations with inherited thrombophilias remains uncertain since the antiphospholipid syndrome is thought to exert its effects at least in part through immune mechanisms which are yet to be fully defined. In addition, heparins may be exerting their beneficial effects through these immunologic pathways rather than via a purely anticoagulant effect. While the combination of heparin and aspirin does appear to increase the chances of a live birth in patients with the antiphospholipid syndrome, uncertainty persists regarding the benefits beyond the first trimester, in particular with regard to a reduction in rates of pre-eclampsia, fetal growth restriction, placental abruption, stillbirth and prematurity. The comparative safety of low molecular weight heparins (LMWH) has seen a trend towards their use in women with adverse pregnancy outcomes and inherited thrombophilias. Gris et al demonstrated a significant improvement in the livebirth rate in thrombophilic patients with a history of a single fetal loss beyond 10 weeks who received Enoxaparin in a subsequent pregnancy compared to those who received only Aspirin.17 This study, together with other small studies reporting improvements in pregnancy outcomes in patients receiving LMWH has prompted what may be somewhat premature recommendations for all thrombophilic patients with adverse pregnancy outcomes to receive LMWH prophylaxis in future pregnancies. 18 This treatment modality must be subjected to the scrutiny of well conducted double blind randomized control trials before it becomes established practice.19 As the topic of thrombophilias and adverse pregnancy outcomes is so broad and controversial, this presentation will primarily be limited to the association between the inherited thrombophilias and pre-eclampsia20. Pre-eclampsia remains a challenging condition for the obstetrician with the precise aetiology remaining elusive and definitive therapy ultimately limited to timely delivery. Consequences for the neonate of premature delivery must be carefully balanced against the maternal consequences of delaying delivery which include neurologic sequelae, pulmonary oedema, DIC, and even death. A genetic predisposition to pre-eclampsia is currently under investigation21 and thrombophilic polymorphisms represent potential candidates in the pathogenesis of pre-eclampsia. The findings of current studies must be confirmed and further assessed in a prospective manner in both asymptomatic cohorts as well as in patients who have previously experienced pre-eclampsia to determine whether therapeutic interventions such as LMWH may alter the development or course of pre-eclampsia. Box 1 Antithrombin deficiency Protein C deficiency Protein S deficiency Activated Protein C Resistance / Factor V Leiden Prothrombin Gene Mutation Hyperhomocysteinaemia Anticardiolipin Antibodies Lupus Anticoagulant References 1. 2. 3. Barbour LA, Bulletins--Obstetrics ACoP. ACOG practice bulletin. Thrombembolism in pregnancy. International Journal of Gynaecology & Obstetrics. 2001; 75:203-12. Many A, Schreiber L, Rosner S, Lessing JB, Eldor A, Kupferminc MJ. Pathologic features of the placenta in women with severe pregnancy complications and thrombophilia. Obstetrics & Gynecology. 2001; 98:1041-4. Higgins JR, Walshe JJ, Darling MR, Norris L, Bonnar J. Hemostasis in the uteroplacental and peripheral circulations in normotensive and pre-eclamptic pregnancies. American Journal of Obstetrics & Gynecology. 1998; 179:520-6. 4. 5. 6. 7. 8. 9. 10. 11. 12. 13. 14. 15. 16. 17. 18. 19. 20. 21. Dekker GA, de Vries JI, Doelitzsch PM, et al. Underlying disorders associated with severe early-onset preeclampsia. American Journal of Obstetrics & Gynecology. 1995; 173:1042-8. Kupferminc MJ, Eldor A, Steinman N, et al. Increased frequency of genetic thrombophilia in women with complications of pregnancy. New England Journal of Medicine. 1999; 340:9-13. Kupferminc MJ, Fait G, Many A, Gordon D, Eldor A, Lessing JB. Severe preeclampsia and high frequency of genetic thrombophilic mutations. Obstetrics & Gynecology. 2000; 96:45-9. Alfirevic Z, Mousa HA, Martlew V, Briscoe L, Perez-Casal M, Toh CH. Postnatal screening for thrombophilia in women with severe pregnancy complications. Obstetrics & Gynecology. 2001; 97:753-9. Livingston JC, Barton JR, Park V, Haddad B, Phillips O, Sibai BM. Maternal and fetal inherited thrombophilias are not related to the development of severe preeclampsia. American Journal of Obstetrics & Gynecology. 2001; 185:153-7. Infante-Rivard C, Rivard G-E, Yotov WV, et al. Absence of Association of Thrombophilia Polymorphisms with Intrauterine Growth Restriction. New England Journal of Medicine 2002; 347:19-25. Higgins JR, Kaiser T, Moses EK, North R, Brennecke SP. Prothrombin G20210A mutation: is it associated with pre-eclampsia? Gynecologic & Obstetric Investigation. 2000; 50:254-7. Alfirevic Z, Roberts D, Martlew V. How strong is the association between maternal thrombophilia and adverse pregnancy outcome? A systematic review. European Journal of Obstetrics, Gynecology, & Reproductive Biology. 2002; 101:6-14. McLintock CN, RA. Dekker G. Inherited thrombophilias: implications for pregnancy associated venous thromboembolism and obstetric complications. Current Problems in Obstetrics, Gynaecology and Fertility 2001; 24:115-149. Robertson L, Wu O, Langhorne P, et al. Thrombophilia in Pregnancy: a systematic review. British Journal of Haematology 2005; 132:171-196. Kupferminc MJ, Many A, Bar-Am A, Lessing JB, Ascher-Landsberg J. Mid-trimester severe intrauterine growth restriction is associated with a high prevalence of thrombophilia. BJOG: an International Journal of Obstetrics & Gynaecology. 2002; 109:1373-6. Mello G PE, Marozio L, Pizzi C, Lojacono A, Frusca T, Facchinetti F, Benedetto C. Thrombophilia is significantly associated with severe preeclampsia: results of a largescale, case-controlled study. Hypertension 2005; 46:1270-1274. Rai R, Cohen H, Dave M, Regan L. Randomised controlled trial of aspirin and aspirin plus heparin in pregnant women with recurrent miscarriage associated with phospholipid antibodies (or antiphospholipid antibodies)[comment]. BMJ 1997; 314:253-7. Gris JC, Mercier E, Quere I, et al. Low-molecular-weight heparin versus low dose aspirin in women with one fetal loss and a constitutional thrombophilic disorder. Blood 2004; 103:3695 - 3699. Bates S, Greer I, Hirsh J, Ginsberg J. Use of Antithrombotic Agents During Pregnancy. The Seventh ACCP Conference on Antithrombotic and Thrombolytic Therapy. Chest. 2004; 126:627S - 644S. Sibai B. Thrombophilia and Severe Preeclampsia. Time to screen and treat in future pregnancies? Hypertension 2005; 46:1252-1253. Said J, Dekker G. Pre-eclampsia and thrombophilia. Best Practice & Research in Clinical Obstetrics & Gynaecology 2003; 17:441-58. Moses EK LJ, Guo G, Wilton AN, Grehan M, Freed K, Borg A, Terwilliger JD, North R, Cooper DW, Brennecke SP. A genome scan in families from Australia and New Zealand confirms the presence of a maternal susceptibility locus for pre-eclampsia, on chromosome 2. Am J Hum Genet. 2000; 67:1581-1585.