GENERAL GUIDELINES - Seattle Children`s
advertisement

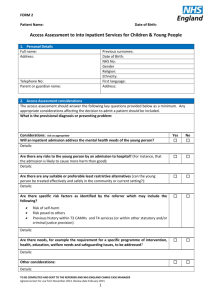
COE4CCN Mental Health Measures Data Abstraction Tool GENERAL GUIDELINES 1. Abstraction Form – This abstraction form collects data for six quality measures applying to children or adolescents with selected mental health conditions treated in the emergency department (ED) or as an inpatient. The conditions of interest for children (5 to 11 years of age) and adolescents (12 to 19 years of age) are dangerous self-harm and suicidal ideation and psychosis. Cases are selected for abstraction based on specifications including age at the time of admission, site of care (ED and/or inpatient), and discharge-related ICD-9 codes. (See separate specifications for case selection.) Cases are assigned to just one condition of interest for abstraction. 2. Site of Care – The quality measures are specific to the site of care. Therefore, not all measures for a particular condition may apply to the case being abstracted for a particular condition. 3. Exclusions – There are some conditions or circumstances that would exclude a patient from being included in a quality measure. For the most part, these patients will be excluded in an automated fashion based on administrative data codes and other parameters during the sample selection. However, if additional data collected in the abstraction indicate that the case is to be excluded, the abstraction tool will display this information. 4. Quality Measures – The quality measures included in the abstraction tool are the following: Measure number Measure MH Quality Measure for Children/Adolescents Presenting with Danger to Self and Suicidality (Applies to children/adolescents ≥5 years-old - ≤19 years-old) DSD9 Children/adolescents admitted to the hospital for dangerous self-harm or suicidality should have documentation in the hospital record of discussion between the hospital provider and the patient's outpatient provider regarding the plan for follow-up (discussion can be by phone or email). MH Quality Measures for Children/Adolescents Presenting with Psychosis (Apply to children/adolescents ≥5 years-old – ≤19 years-old) P2 P3 All children/adolescents who present to the ED with psychotic symptoms should receive the following screening laboratory tests: a) Urine drug screening b) Serum alcohol screening All children/adolescents admitted to the hospital with psychotic symptoms should have a psychiatric consult (in person or by telepsychiatry) within 24 hours of admission. COE4CCN MH Measures Abstraction Tool Guidelines 1 10-05-2015 CLINICAL GUIDELINES The mental health module focuses on two conditions and looks at both ED and inpatient care, as indicated. The conditions of interest for children (5 to 11 years of age) and adolescents (12 to 19 years of age) are dangerous self-harm/suicidal ideation and psychosis. 1. Date of Birth – Enter the patient’s date of birth. 2. Condition of Interest – Select the condition that was designated for this emergency department/inpatient admission from the denominator specified age categories and ICD-9 codes. 3. Place of Care – Distinguish among patients who were seen in the ED of the marker hospital (either exclusively or before admission to the marker hospital) and those who were admitted directly to the marker hospital. Response 3 includes patients admitted directly to the marker hospital who may have been seen in a different ED or hospital prior to admission, but were NOT treated in the marker hospital’s ED. 4. Date of ED Admission – For those patients seen in the marker ED, enter the date of the admission to the ED. 5. Dates of Admission and Discharge – For those patients admitted to the marker hospital (either via the marker ED or directly), give the dates and times of the hospital admission and discharge. Do not include any time spent in the ED. 6. This item has been deleted. 7. This item has been deleted. 8. Discharge Disposition – [Module: Dangerous self-harm/suicidal ideation, inpatient care] Indicate the patient’s disposition at discharge. If the patient was transferred to an acute or non-acute inpatient facility other than the marker hospital, select response 1. This case will be excluded since care continued at that institution. Response 2 includes patients who left AMA or who eloped. Response 3 is for patients who were discharged to some sort of holding facility such as jail, juvenile detention, or other holding placement. Response 4 is for patients who were discharged to half- or partial-hospitalization. The definition of this varies among sites, but in general indicates an arrangement where the patient is at home at night, but in a therapeutic environment during the day. Response 5 is for patients who were discharged to home, which includes a foster home or other group homelike arrangement. 9. Follow-up MD – [Module: Dangerous self-harm/suicidal ideation, inpatient care] Indicate “1” if at the time of discharge, the patient had a designated primary care provider (PCP) or psychiatrist who would manage the patient’s care post-discharge. Even patients with no known provider at the time of hospital admission should have been referred to a follow-up provider who was a PCP or a psychiatrist at the time of discharge. Indicate “2” if there is no follow-up provider identified. COE4CCN MH Measures Abstraction Tool Guidelines 2 10-05-2015 10. Follow-up MD: SI Plan – [Module: Dangerous self-harm/suicidal ideation, inpatient care] Indicate “1” if the hospital provider communicated (by telephone or email) with the follow-up provider (PCP or psychiatrist) during the time window of 24 hours prior to discharge to 48 hours after discharge. The window of time is computed based on the discharge date and time and is displayed within the question text in the data collection tool. The purpose of this communication is to be sure a safe transition is in place, as this item applies only to patients hospitalized for self-harm/suicidal ideation. Select response “2” if the hospital provider is also the follow-up outpatient provider OR if outpatient care has been arranged to be continued in the marker hospital's own psychiatric outpatient clinic. The latter arrangement is considered to be an adequate communication of the safety plan for the patient. If you cannot verify that there was any communication between the hospital provider and the follow-up PCP/psychiatrist AND there is no same-institution psychiatric clinic follow-up arranged, select response “3” (Neither of the above/No data). 11. Urine Drug Screening /Serum Alcohol Screening – [Module: Psychosis, ED care] This item applies to children and adolescents presenting with psychotic symptoms who were admitted to the marker ED. Indicate if the patient had a urine drug screen or serum alcohol screen while in the ED. The alcohol test will be a separate test from the drug tests. The drug test must be comprehensive in that it tests for multiple types of illicit drugs. Do NOT give credit for tests that include results of just a single drug. Drug screens commonly include tests for benzodiazepines, barbiturates, methamphetamine, cocaine, methadone, opiates, tetrahydrocannabinol, etc. 12. Psychiatric Consult – [Module: Psychosis, inpatient care] Indicate if the patient had a psychiatric consult within 24 hours of admission. The end of the 24-hour time frame will be computed (based on admission time) and displayed. Include in this interval any psychiatric consult that may have been done in the marker ED prior to admission if the patient was admitted via the marker ED. The consult may be in person or by telemedicine. The consult must have been done by a psychiatrist or PhD psychologist. If the consult was done by a clinician-extender (nurse practitioner, advanced practice nurse, physician assistant, licensed social worker, or licensed counselor), this is acceptable as long as the assessment is co-signed by a psychiatrist. If an appropriate person did not assess the patient during the first 24 hours, choose response 2 (No/No data), and continue to Q12a). 12a) Indicate if the patient had a psychiatric consult within 48 hours of admission. (The end of this time frame is computed based on the date and time of admission will be displayed in the question text.) If a qualifying MH provider assessed the patient by the indicated time, select response 1 only if a justification was noted for the delay that prevented the consult from occurring within the first 24 hours. The abstractor is not asked to evaluate the content or acceptability of the justification. Any justification that specifically refers to the time delay for the assessment is acceptable. If there is no justification noted for the delay, select response 2. If the consult did not occur or only occurred more than 48 hours after admission, select response 3 (Neither of the above/No data). COE4CCN MH Measures Abstraction Tool Guidelines 3 10-05-2015