ECT Orientation Guide

St. Vincent Catholic Medical Center
New York Medical College
Department of Psychiatry
Joseph M Matta, M.D.
(ECT) Electroconvulsive Therapy
Orientation Guide
Based on NY State Office of Mental Health ECT Review Guidelines http://www.omh.state.ny.us/omhweb/ect/guidelines.htm
and
American Psychiatric Association’s recommendations presented in the second edition of
The Practice of Electroconvulsive Therapy: Recommendations for Treatment, Training, and Privileging (2001). –you may find in this guide references to the APA Practice
Guideline with the corresponding page numbers to that guide.
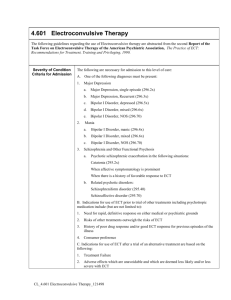
Who is an ECT candidate?
ECT may be considered as a primary treatment (or first-line treatment) for persons exhibiting syndromes such as: severe major depression, acute mania, mood disorders with psychotic features, and catatonia. A decision to use ECT as the primary therapy should be based on an evaluation of the nature and the severity of acute symptoms in conjunction with an evaluation of risks and benefits. ECT may be the initial treatment of choice when a rapid or a higher probability of response is necessary. ECT may also be considered as a primary treatment when there is a history of good response to ECT treatment and/or poor response to alternate treatments during prior episodes.
ECT is most often used as a secondary treatment when a patient has shown insufficient improvement with prescribed treatment(s), which usually includes pharmacotherapy. In addition to lack of substantial clinical response, other reasons to use ECT include, intolerance to side effects of medication or other treatments, deterioration in condition, or appearance of suicidality or pronounced lethargy. In the context of referral for ECT, patients who have not responded to psychotherapy alone should not be considered as having a treatment resistant mental illness - regardless of diagnosis.
Diagnosis:
1.
Major Depression – recent onset, typical symptoms, psychotic features.
2.
Depression not responsive to medication trials – usually a number of various types of antidepressants.
3.
Previous positive response to ECT.
4.
Mania not responsive to mood stabilizers, neuroleptics.
5.
Manic delirium – extreme psychosis, disorganization, pt at medical risk for dehydration, medication toxicity, suicide.
6.
Schizophrenia – catatonic type.
7.
Parkinson’s Disease
8.
Intractable Seizure Disorder
9.
Neuroleptic Malignant Syndrome
Who is not an ECT candidate?
1.
Patients with an active substance abuse problem (all types of drugs and
EtOH).
2.
Patient for whom an axis II diagnosis is thought to be the reason for pt’s symptoms.*
3.
Patients with severe medical and/or cognitive problems that would cause risk to outweigh benefit to patient
*Although the results of these studies appear somewhat divergent, most found that patients with major depression and a personality disorder have a less favorable outcome with ECT than depressed patients without a personality disorder . APA
Practice Guidelines for Treatment of Patients with Borderline PD.
ECT can be administered to persons with severe medical conditions. Although some medical conditions may alter the risk of treatment, there are no “absolute” medical contraindications to the use of ECT. In some medically ill patients ECT may be preferred because of its efficacy and safety profile.
Special populations identified by the APA include:
Coexisting medical illnesses (e.g. neurologic and cardiovascular disorders) and their treatment may affect both the likelihood of response and the risks of ECT. It is critical to recognize potential interactions among coexisting medical conditions, physiologic events associated with anesthesia, electrical stimulation, and induced seizure activity when proposing and administering ECT.
Elderly patients may receive ECT regardless of age. The efficacy of treatment does not diminish with advancing age. ECT may have a lower risk of complications than some forms of pharmacotherapy in the elderly.
Pregnant women and nursing mothers may receive ECT during all trimesters of pregnancy, puerperium and nursing. ECT may be less risky than alternate pharmacologic treatment or non-treatment of mental illness during pregnancy.
Children and Adolescents should receive ECT only when it is evident that other viable treatments have been ineffective or if other treatments cannot be administered safely.
(APA pp. 31-52)
Relative Contraindications:
Factors that significantly increase risk may include: unstable or severe cardiovascular conditions, aneurysm or vascular malformation, increased intracranial pressure, cerebral infarction, pulmonary insufficiency
Severe aortic stenosis
Theophyline toxicity
Brain mass
Preparing the patient for ECT:
Once the decision to treat a patient with ECT is made, the following are necessary elements in preparing the patient:
1.
ECT consent: this is a special consent specific for ECT providing informed consent for the patient. No other hospital consent form is acceptable!
Patient information about ECT should be handed out to the patient.
Guidelines :. When consenting a patient for ECT, information should be provided to the patient including but not limited to: 1) reason for the recommendation of ECT, 2) description of alternative treatments, 3) description of ECT procedure, 4) discussion of the benefits and risks of the different stimulus electrode placements and the rationale for the electrode placement being recommended, 5) range of the number of treatments the consentor is approving, 6) statement that there is no guarantee that ECT will be effective,
7) statement regarding the need for continuation/maintenance somatic treatment, 8) description of major risks and their likelihood of occurrence, 9) description of common side effects, 10) statement that consent for ECT also includes consent for clinically necessary emergency treatment, 11) description of restrictions on patient behavior before, during, and after treatment, 12) evidence of an opportunity for patient to ask questions,
13) statement that ECT is voluntary and may be withdrawn by the patient at any time.
2.
Necessary lab work usually include: CBC, SMA, TFT’s LFTs, baseline EKG, chest x-ray, urine pregnancy test in females of childbearing age.
3.
Head CT and/or MRI: to rule out organic causes, especially with new symptom onset with no obvious precipitant.
Specific components of the evaluation of patients identified for ECT vary on a case-bycase basis. Laboratory testing is used to confirm the presence and severity of medical risk factors. No specific laboratory tests are routinely required as part of the pre-ECT work up. (APA pp. 77-79)
Any other necessary tests required for medication clearance must be completed prior to 1 st scheduled treatment.
4.
GMC consults: necessary for all patients with ongoing medical problems and those with new illness onset.
5.
Patients with SVCMC medical attending: that MD can substitute for GMC clearance. SVCMC physician must write a note in the patient’s chart documenting medical clearance for ECT.
6.
complete the MD pre-ECT Checklist prior to 1 st scheduled ECT.
7.
Write orders for ECT in order book: including: date/day of scheduled ECT, type of ECT (right unilateral or bilateral), NPO after midnight except for certain medications---blood pressure, cardiac, pulmonary, give with sip of water at 7 am
day of treatment. Diabetic patients need to have FS blood glucose checked on the unit before treatment. Hold diabetic medications and insulin pre-ECT.
8.
If patient is thought to not be able to comply with NPO status pt can be placed on Continuous Observation after midnight.
If CO is necessary, the order must be written and nursing staff must be alerted as early as possible
(arrangement for additional staffing must be made).
9.
ECT orders must be written prior to each treatment as outlined above.
10.
MAOI’s are contraindicated during ECT, require 2 week “washout period.”
11.
Antidepressants are reduced by 50% prior to 1 st treatment is recommended.
12.
All mood stabilizers including: lithium, depakote, tegretol, lamictal etc must be d/c’d prior to 1 st treatment.
13.
Benzodiazepines: should be avoided.
Montioring Patient During ECT Course:
Providers should address requirements for clinical assessments performed by the attending psychiatrist or designee. Assessment should occur prior to ECT and after every one or two treatments, usually within 24 hours after treatment. Formal clinical rating instruments are available and may be employed in documenting therapeutic responses and changes in symptoms. Policies should also discuss the need to determine whether
ECT should be continued, reduced in frequency, or suspended when hypo-mania or mania emerges during an ECT course.
During the course of treatment, monitoring should include the presence and severity of disorientation, anterograde amnesia (by use of objective measures), treatment emergent mania, etc. and should also include patient self-reporting. Assessment of orientation and memory should be completed before the initial ECT treatment and at least weekly throughout the treatment course. If disorientation or memory loss are substantial during treatment, modifications to the ECT procedure (from bilateral to right unilateral electrode placement, decrease in electrical intensity, longer intervals between treatments, altering dosage of medications, etc.) may be warranted.
1.
Do baseline minimental status exam prior to 1 st treatment, and on nontreatment days. Document findings in MD notes---assess for increasing confusion, anterograde and retrograde memory changes, is the patient confused on the unit? Unable to find room/diningroom/bathroom? If so you may need to skip or space out treatments more (e.g. Monday and Friday).
2.
Do Hamilton Depression Rating Scale or other depression-measuring instrument (or Young Mania Rating Scale) to assess and document improvement.
3.
Patients with ongoing medical problems should have SMA10 and CBC at least weekly.
4.
Remember to tell patients and family memory disruption isn’t permanent and should resolve within 2-4 weeks after last treatment though some memory difficulties persist beyond this point.
MEDICATIONS TO BE USED WITH CAUTION DURING ECT
Theophylline
prolonged seizure, associated with status epilepticus
(monitor drug levels and keep them in low therapeutic range if possible)
Lithium
prolonged seizure increased risk of delirium, interaction with anesthetic agents,
MAOIs
possible cardiac risk, interaction with anesthesia agents
Other antidepr
possible cardiac risk
Newer agents (SSRIs, effexor, cymbalta, nortriptyline) may be used in lower doses.
Wellbutrin prolonged seizure, lower seizure threshold
Benzodiazepines
lower seizure duration, decreased treatment efficacy
(no more than 2 mg ativan/day)
Anticonvulsants
increase seizure threshold, decrease treatment efficacy
Echothiphate
prolonged period of apnea
Clozaril
increased risk of prolonged seizure in doses above 200 mg/day
(recent research is disputing this notion)