, Metro North Hospital and Health
advertisement
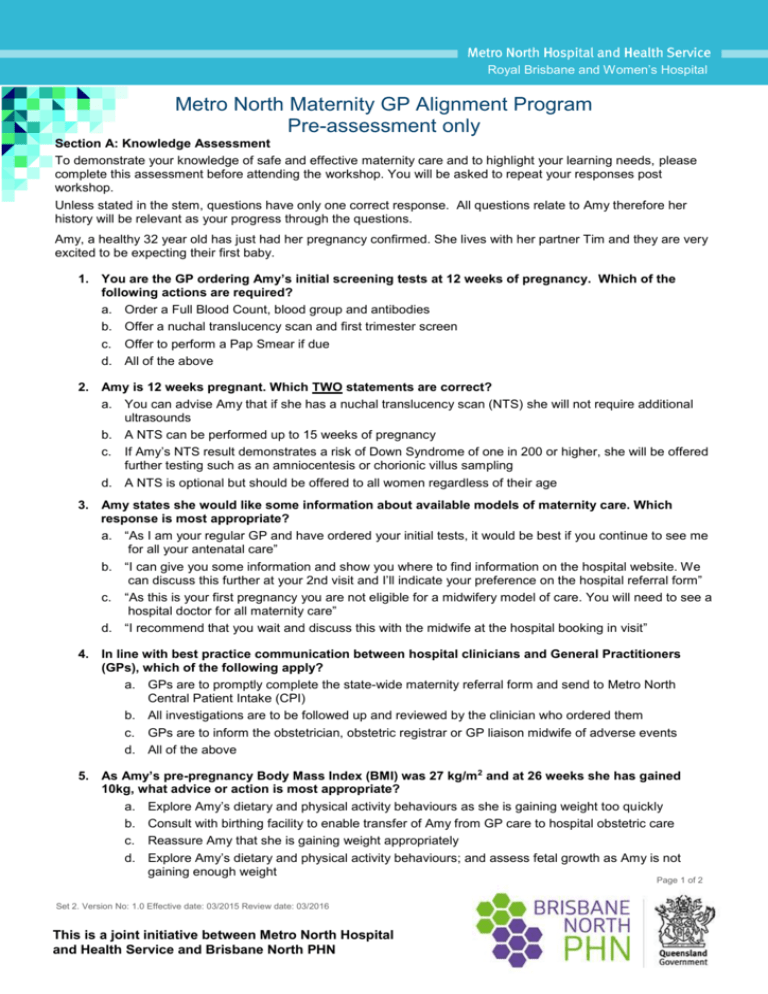
Royal Brisbane and Women’s Hospital Metro North Maternity GP Alignment Program Pre-assessment only Section A: Knowledge Assessment To demonstrate your knowledge of safe and effective maternity care and to highlight your learning needs, please complete this assessment before attending the workshop. You will be asked to repeat your responses post workshop. Unless stated in the stem, questions have only one correct response. All questions relate to Amy therefore her history will be relevant as your progress through the questions. Amy, a healthy 32 year old has just had her pregnancy confirmed. She lives with her partner Tim and they are very excited to be expecting their first baby. 1. You are the GP ordering Amy’s initial screening tests at 12 weeks of pregnancy. Which of the following actions are required? a. Order a Full Blood Count, blood group and antibodies b. Offer a nuchal translucency scan and first trimester screen c. Offer to perform a Pap Smear if due d. All of the above 2. Amy is 12 weeks pregnant. Which TWO statements are correct? a. You can advise Amy that if she has a nuchal translucency scan (NTS) she will not require additional ultrasounds b. A NTS can be performed up to 15 weeks of pregnancy c. If Amy’s NTS result demonstrates a risk of Down Syndrome of one in 200 or higher, she will be offered further testing such as an amniocentesis or chorionic villus sampling d. A NTS is optional but should be offered to all women regardless of their age 3. Amy states she would like some information about available models of maternity care. Which response is most appropriate? a. “As I am your regular GP and have ordered your initial tests, it would be best if you continue to see me for all your antenatal care” b. “I can give you some information and show you where to find information on the hospital website. We can discuss this further at your 2nd visit and I’ll indicate your preference on the hospital referral form” c. “As this is your first pregnancy you are not eligible for a midwifery model of care. You will need to see a hospital doctor for all maternity care” d. “I recommend that you wait and discuss this with the midwife at the hospital booking in visit” 4. In line with best practice communication between hospital clinicians and General Practitioners (GPs), which of the following apply? a. GPs are to promptly complete the state-wide maternity referral form and send to Metro North Central Patient Intake (CPI) b. All investigations are to be followed up and reviewed by the clinician who ordered them c. GPs are to inform the obstetrician, obstetric registrar or GP liaison midwife of adverse events d. All of the above 5. As Amy’s pre-pregnancy Body Mass Index (BMI) was 27 kg/m2 and at 26 weeks she has gained 10kg, what advice or action is most appropriate? a. Explore Amy’s dietary and physical activity behaviours as she is gaining weight too quickly b. Consult with birthing facility to enable transfer of Amy from GP care to hospital obstetric care c. Reassure Amy that she is gaining weight appropriately d. Explore Amy’s dietary and physical activity behaviours; and assess fetal growth as Amy is not gaining enough weight Page 1 of 2 Set 2. Version No: 1.0 Effective date: 03/2015 Review date: 03/2016 This is a joint initiative between Metro North Hospital and Health Service and Brisbane North PHN 6. Amy has a routine 75 gram Pregnancy Oral Glucose Tolerance Test (POGTT) as recommended between 26 and 28 weeks. The result is a fasting glucose level of ≥ 5.3 mmol/L. What does this mean? a. The result indicates Amy has Gestational Diabetes Mellitus (GDM) b. The result is not indicative of GDM c. Only if Amy has known risk factors for GDM would her results indicate that she has GDM d. It is not clear if Amy has GDM as a diagnosis can only be made if her 1-hr glucose is ≥10.0mmol/L or 2-hr glucose ≥ 8.5 to 11.0 mmol/L 7. Amy brings healthy term 7 day old Jack to you for a routine post birth check. She asks you if she should continue keeping him in her room at night now that she is at home. Which of the following responses would be most appropriate? a. “Yes, it is important, as the safest place for Jack to sleep is in a cot beside your bed. Room-sharing reduces the risk of sudden infant death and allows you to wake to Jack’s early signs that he wants to feed” b. “It is a personal choice, but Jack needs to become familiar with his own room as soon as possible” c. Rooming – in is only important whilst you are in hospital for security reasons d. “No, ideally Jack will sleep in his own room so you don’t disturb one another” 8. At 10 days postpartum Amy has a temperature of 39°C and a tender red area on her right breast consistent with mastitis. Appropriate management of infective mastitis includes which of the following? a. Encourage Amy to express and discard her breast milk due to the presence of bacteria b. Advise Amy to supplement Jack’s feeds with infant formula as the fat concentration is lower than usual during acute infection c. Advise Amy to express and discard her breast milk during antibiotic therapy d. Advise Amy to continue exclusive breastfeeding feeding with appropriate antibiotics use 9. At 4 weeks post-partum, Amy is diagnosed with postnatal depression. Which of the following statements is true in relation to perinatal depression? a. As antidepressant medication is contra-indicated in breastfeeding women, Amy should be advised to wean b. In Qld in 2011, suicide was the number one cause of maternal mortality within a year of the end of pregnancy c. Pregnancy is protective of perinatal depression d. The Edinburgh Postnatal Depression Score (EPDS) is only to be administered if there are valid concerns about a woman’s mental health 10. a. b. c. If Amy was diagnosed with GDM, what would you include in your post natal management? No further testing is required with a diagnosis of Gestational Diabetes Mellitus (GDM) Perform a random blood glucose test at the routine 6 week post-partum visit Order a repeat 75 gram Oral Glucose Tolerance Test (OGGT) to be performed between 6 and 12 weeks after delivery d. Order a 50 gram one hour non-fasting Glucose Challenge Test (GCT) to be performed between 6 and 12 weeks after delivery Page 2 of 2 This is a joint initiative between Metro North Hospital and Health Service and Brisbane North PHN