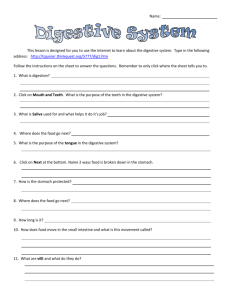
DIGESTIVE SYSTEM
advertisement

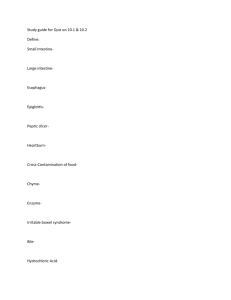
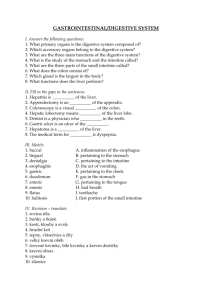
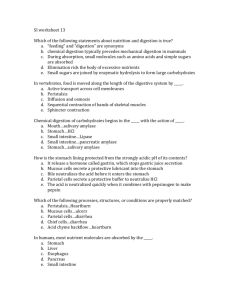
DIGESTIVE SYSTEM The human digestive system passes from the mouth through the oesophagus to the stomach where acids facilitate some chemical changes. From the stomach, food passes to the small intestine, where some nutrients are further broken down to very simple molecules to be absorbed into the blood stream, and then to the large intestine or colon, where water is reabsorbed and the residual material is compacted. Exit is through the rectum and out the anus. Above the stomach is the liver, which plays many important roles in digestion; under the liver it is the pancreas, which secretes many of the digestive enzymes into the small intestine. The process of changing food into its simple components is called digestion, and the changes occur primarily in the digestive tract. The digestive tract is essentially a tube about 30 feet (9m) long that passes through the centre of the body from the mouth to the anus. The GI tract comprises of four layers. From innermost to outermost there is: 1) Mucous membrane 2) Sub mucous layer 3) Muscular layer 4) Serous layer The muscular layer of the stomach is different from other regions of the digestive tract in that it consists of three layers: an outer longitudinal layer, a middle circular layer, and an inner oblique layer. Such an arrangement gives the muscles elasticity, enabling the stomach to expand considerably after meals in order to hold all the food eaten. It also produces strong contractions, which churn the food about so that it mixes with the gastric juices. Foods are digested by a series of mechanical and chemical processes that break them down into particles that can be absorbed. In the mouth: food is physically separated into small pieces by chewing and the movement of the tongue, cheeks, lips and lower jaw. Saliva is mixed with food during the chewing process, and the food becomes a moist, soft mass called bolus. Mucus - a thick, slippery secretion of the mucous membranes that line the mouth – also helps moisten and soften food and to lubricate its passage from the mouth. In the oesophagus: through coordinated contractions and relaxations, the 9 to 10 inch long oesophagus delivers the bolus of swallowed food to the stomach. When the stomach contents spurt up into the oesophagus due to vomiting or indigestion, the walls of oesophagus are irritated by stomach acid and oesophagus signals pain. Because oesophagus is close to the heart, this pain is commonly called “heartburn” In the stomach: after food is fully mixed and liquefied the pyloric sphincter at the end of the stomach relaxes for an instant and allows about 1 to 2 teaspoons of food, now called chyme (semi fluid mass of partly digested food that is expelled by the stomach into the duodenum) to enter the duodenum of the small intestine. This amount of chyme leaves 1 the stomach about every 30 seconds when there is food in the stomach. How does the pyloric sphincter know when to open and close? When the pyloric sphincter relaxes, acidic chyme slips through. The cells of the pyloric muscle on the intestinal side sense the acid, causing the pyloric sphincter to close tightly. Only after the chyme has been neutralized by pancreatic bicarbonate and the medium surrounding the pyloric sphincter has become alkaline can the muscle relax again. This process ensures that the chyme will be released slowly enough to be neutralized as it flows through the small intestine. This is important, because the small intestine has less of a mucous coating than the stomach does and so is not as well protected from acid. The digestive juices secreted in the stomach contain hydrochloric acid, bicarbonate (a base) and enzymes. Hydrochloric acid deactivates the salivary amylase that was combined with food in the mouth and kills many of the bacteria that were consumed along with the food. Hydrochloric acid also activates pepsinogen, the precursor of the protein – splitting enzyme pepsin. Bicarbonate secreted by the stomach partially neutralises the acidity of the food mixture before it is delivered to the small intestine. The fat – digestion enzyme secreted by the stomach is gastric lipase. Fats leave the stomach still requiring a good deal of digestion by enzymes and other substances in the small intestine. Mucus secreted by the stomach protects its lining from its other secretions. Without this mucus, the stomach lining, too, would be digested. A small amount of simple sugars, alcohol, and water are absorbed by the lining of the stomach and enter the blood stream. Small intestine: the small intestine is 15 to 30 feet in length and consists of the duodenum, jejunum and ileum. Bile is produced by the liver and stored in the gallbladder. It is released by the gallbladder when the small intestine signals that fat has arrived. Bile is not an enzyme, but an emulsifier; it makes fats partially soluble in water and thus more vulnerable to the action of enzymes. The pancreas produces: pancreatic amylase for carbohydrate digestion trypsinogen, chymotrypsinogen, and other substances for protein digestion, and pancreatic lipase for fat digestion. Pancreatic amylase and lipase are used directly for digestion, but enzymes present in the small intestine must first activate trypsinogen and chymotrypsinogen. The -ogen suffix denotes “an agent that produces” an active substance; trypsinogen, for example, is activated by enterokinase and forms trypsin, an active enzyme. Trypsin also converts chymotrypsinogen into the active enzyme chymotrypsin. 2 The small intestine produces enzymes that digest carbohydrates and fats. Sucrose, lactase, and maltase break down sugars and intestinal lipase breaks down fats. Components of foods that are incompletely digested or not digested in the small intestine are passed through the large intestine and excreted in faeces. Little digestion occurs after food particles leave the small intestine. Large intestine – the large intestine, or colon, is about five feet long. It serves to collect and transport waste products of digestion that will be excreted. The large intestine begins with the cecum and ends with the sigmoid colon. In between the cecum and sigmoid colons are the ascending, transverse, and descending portions of the colon. The large intestine is home for many types of bacteria, which break down some types of dietary fibre and produce part of the body’s supply of biotin and vitamin K. The end products of bacterial fibre are primarily fatty acids and gases. Although some of the fatty acids formed by bacteria from dietary fibre are absorbed, the amount appears to be too small to make a significant contribution to caloric intake. Summary of the sites and the nature of digestion Site Mouth Oesophagus Stomach Type of Action Mechanical Chemical How accomplished Mechanical Chemical Mechanical Chemical Peristalsis (delivers bolus to stomach) N/A Peristalsis Action of hydrochloric acid Bicarbonate (a base) Gastric enzymes (pepsinogen activated to pepsin and gastric lipase) Mucus Peristalsis Bile Pancreatic enzymes (pancreatic amylase, trypsinogen activated to trypsin, chymotrypsinogen activated to chymotrypsin, pancreatic lipase) Intestinal enzymes (intestinal lipase, sucrose, lactase, maltase) Intestinal enzymes Small Intestine Mechanical Chemical Intestinal membrane Large intestine Chemical Mechanical Chemical Chewing Salivary enzymes (s. amylase) Lingual enzymes (l. lipase) Collects and transports waste products of digestion that will be excreted Bacterial enzymes 3 In the duodenum the food meets pancreatic juice, which contains several proteolytic (protein-splitting) enzymes all secreted as inactive precursors. An overview of the participation of key enzymes, hydrochloric acid and bile in the digestion of the energy nutrients. Site MOUTH Carbohydrates Salivary amylase Proteins Fats Lingual lipase Pepsinogen (inactive) STOMACH Gastric lipase hydrochloric acid Pepsin (active) Pancreatic amylase SMALL INTESTINE Intestinal amylase Sucrase Lactase Maltase Tryspinogen (inactive) Bile Pancreatic lipase Intestinal lipase Enterokinase (secreted by the intestinal wall) Trypsin (active) Chymotrypsinogen Trypsin chymotrypsin (inactive) (active) Procarboxypeptidase A Trypsin Carboxypeptidases (inactive) Procarboxypeptidase B (active) Trypsin (inactive) Peptidases (active) GASTROINTESTINAL HORMONES The stomach normally maintains a pH between 1.5 and 1.7. How does it stay that way? One of the regulations of the stomach pH is the hormone gastrin, secreted by cells in the stomach wall. The entrance of food into the stomach stimulates these cells to release gastrin, which in turn, stimulates other stomach glands to secrete the components of 4 hydrochloric acid. When pH 1.5 is reached, the acid itself turns off the gastrin – producing cells so that they stop releasing the hormone. Once the hormonal stimulus has ceased, the glands stop producing hydrochloric acid. Thus the system adjusts itself. As the chyme enters the intestine, the pancreas adds bicarbonate to it, so that the intestinal contents always remain at a slightly alkaline pH. How does the pancreas know how much to add? The presence of chyme stimulates the cells of the duodenum wall to release the hormone secretin into the blood. As this hormone circulates through the pancreas, it stimulates the pancreas to release its bicarbonate – rich juices. Thus, whenever the duodenum signals that acidic chyme is present, the pancreas responds by sending bicarbonate to neutralise it. When the need has been met, the secretin cells of the duodenum wall are no longer stimulated to release the hormone, the hormone no longer flows through the blood, the pancreas no longer receives the message, and it stops sending pancreatic juice. When fat is present in the intestine, the gall bladder contracts to squirt bile into the intestine to emulsify the fat. How does the gall bladder get the message that fat is present? Fat in the intestine stimulates cells of the intestine wall to release the hormone Cholecystokinin (CCK). This hormone, travelling by way of the blood to the gall bladder, stimulates it to contract, releasing bile into the small intestine. Once the fat in the intestine is emulsified and enzymes have begun to work on it, the fat no longer provokes release of the hormone, and the message to contract is cancelled. Fat takes longer to digest than carbohydrate does. When fat is present, intestinal motility slows to allow time for its digestion. How does the intestine know when to slow down? Cholecystokinin and gastric – inhibitory peptide slow GI tract motility, thus keeping food in the stomach longer. By slowing the digestive process, fat helps to maintain a pace that will allow all reactions to reach completion. Gastric – inhibitory peptide also inhibits gastric acid secretion. Hormonal mechanics like these account for much of the body’s ability to adapt to changing conditions. Summary of Gastrointestinal hormones HORMONE GASTRIN SECRETIN CHOLECYSTOKININ (CCK) GASTRIC INHIBITORY PEPTIDE SITE OF PRODUCTION Cells in the stomach wall Cells in the duodenum wall TARGET ORGAN Stomach Cells of the intestinal wall Small intestine Gall bladder Pancreas Stomach RESPONSE Secretion of gastric juice Secretion of bicarbonate – rich pancreatic juice - Release of bile - Slowing of GI motility - Inhibits gastric acid secretion - Slowing of GI motility 5 SYSTEMS OF THE BODY A system is a group of organs, which are closely allied to one another and are concerned with carrying out a particular bodily function. THE CIRCULATORY SYSTEMS Once a nutrient has entered the bloodstream, it may be transported to any of the cells in the body, from the tips of the toes to the roots of the hair. The circulatory systems deliver nutrients wherever they are needed. THE VASCULAR SYSTEM The circulatory or vascular system consists of the heart, the blood vessels and the blood. It is a closed system of vessels through which blood flows continuously in a figure eight, with the heart serving as a pump at the crossover point. As the blood circulates through this system, it picks up and delivers materials as needed. All the body tissues derive oxygen and nutrients from the blood and deposit carbon dioxide and other wastes into it. The lungs exchange carbon dioxide (which leaves the blood to be exhaled) and oxygen (which enters the blood to be delivered to all cells). The digestive system supplies the nutrients to be picked up. In the kidneys, wastes other than carbon dioxide are filtered out of the blood to be excreted in the urine. Blood leaving the right side of the heart circulates by way of arteries into the lung capillaries and then back through veins to the left side of the heart. The left side of the heart then pumps the blood out through arteries to all systems of the body. The blood circulates in the capillaries, where it exchanges material with the cells, and then collects into veins, which return it again to the right side of the heart. In short, blood travels this simple route: heart to arteries to capillaries to veins to heart. The routing of the blood past the digestive system has a special feature. The blood is carried to the digestive system (as to all organs) by way of an artery, which (as in all organs) branches into capillaries to reach every cell. Blood leaving the digestive system, however, goes by way of vein, not back to the heart, but to another organ – the liver. This vein again branches into capillaries so that every cell of the liver also has access to the blood carried by the vein. Blood leaving the liver then again collects into a vein, which returns to the heart. The route is then like this: heart to arteries to capillaries (in intestines) to vein to capillaries (in liver) to vein to heart. The liver’s placement ensures that it will be first to receive the materials absorbed from the GI tract. In fact, the liver has many jobs to do in preparing the absorbed nutrients for use by the body. It is the body’s major metabolic organ. You might guess that, in addition, the liver serves as a gatekeeper to defend against substances that might harm the heart or brain. This is why, when people ingest poisons that succeed in passing the first barrier (the intestinal cells), the liver quite often suffers the damage – from the hepatitis 6 virus, from drugs such as barbiturates or alcohol from poisons, and from contaminants such as mercury. The liver’s key position in nutrient transport 1. Vessels gather up nutrients and reabsorbed water and salts from all over the digestive tract. 2. The vessels merge into the portal vein, which conducts all absorbed materials to the liver. 3. The hepatic artery brings a supply of freshly oxygenated blood (not loaded with nutrients) from the lungs to supply oxygen to the liver’s own cells. 4. Capillaries branch all over the liver, making nutrients and oxygen available to all its cells and giving the cells access to blood from the digestive system. 5. The hepatic vein gathers up blood in the liver and returns it to the heart. THE LYMPHATIC SYSTEM The lymphatic system is also considered part of the circulatory system. The lymphatic system provides a one-way route for fluid from the tissue spaces to enter the blood. Lymph fluid circulates between the cells of the body and collects into tiny vessels. Lymph is almost identical to blood except that it contains no red blood cells or platelets, because they cannot escape through the blood vessel walls. The lymphatic system has no pump; instead, lymph is squeezed from one portion of the body to another like water in a sponge, as muscles contract and create pressure here and there. Ultimately, much of the lymph collects in a large duct behind the heart. This duct terminates in a vein that conducts the lymph toward the heart. Thus materials from the GI tract that enter lymphatic vessels (large fats and fat-soluble vitamins) ultimately enter the blood circulatory system, circulating through arteries, capillaries, and veins like the other nutrients, with a notable exception – they bypass the liver at first. Thus, in contrast, nutrients absorbed into lymph do not go to the liver first. They go to the heart, which pumps them to all the body’s cells. The cells remove the nutrients they need, and the liver then has to deal only with the remnants. Once inside the vascular system, the nutrients can travel freely to any destination and can be taken into cells and used as needed. Lymph vessels are interrupted by lymph nodes, which remove bacteria and other foreign matter from lymph on its return to the blood system. Lymph nodes are grouped in clumps and can be felt as “glands” in the armpit, groin and neck. They also produce antibodies. Terms used in circulatory systems o Arteries: vessels that carry blood away from the heart o Veins: vessels that carry blood back to the heart 7 o Capillaries: small vessels that branch from an artery. Capillaries connect arteries to veins. Exchange of oxygen, nutrients, and waste materials takes place across capillary walls. o Portal vein: the vein that collects blood from GI tract and conducts it to capillaries in the liver. (Portal = gateway) o Hepatic vein: the vein that collects blood from the liver capillaries and returns it to the heart. (Hepatic = liver) o Lymphatic system: a loosely organized system of vessels and ducts that convey fluids toward the heart; the GI part of the lymphatic system carries the products of digestion into the bloodstream. o Lymph: a clear yellowish fluid that resembles blood without the red blood cells; lymph from the GI tract transports fat and fat-soluble vitamins to the bloodstream via lymphatic vessels. o Thoracic duct: the duct that conveys lymph toward the heart o Subclavian vein: connects thoracic duct with the right upper chamber of the heart, providing a passageway by which lymph can be returned to the vascular system. 8