Infectious Diseases - Introduction and Notification
advertisement

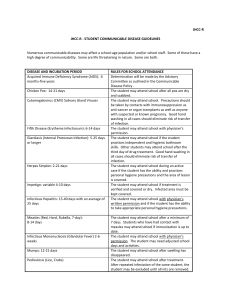
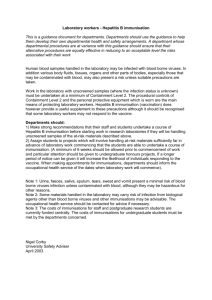
SECTION ONE INTRODUCTION AND NOTIFICATION 1. INTRODUCTION AND NOTIFICATION 1.0 INTRODUCTION The guidance is divided into sections as follows: Section 1 Introduces infection control and explains notification; Section 2 deals with general infection control procedures; Section 3 gives guidance on the management of outbreaks; Section 4 describes specific infectious diseases; Section 5 contact numbers and sources of information; Section 6 contains additional detailed information and a table of diseases; Section 7 contains risk assessments relevant to infection control; Section 8 research sources, references and useful web sites Further information is available from the Food Safety Adviser at Leicestershire County Council and from the Health Protection Agency – East Midlands South. Contact numbers are listed in Section 5. The aim of this document is to provide simple advice on the actions needed in the majority of situations likely to be encountered in social care settings. It is written in everyday language and presented so that individual subject areas can be easily copied for use as a single sheet. 1.1 HOW ARE INFECTIONS TRANSMITTED? Infectious diseases are usually caused by viruses or bacteria and can be transmitted from one person to another in a number of ways: By direct skin to skin contact This is unusual, as the majority of infections cannot penetrate the skin without an open wound. An infection that can spread in this way is Scabies. Infections, which do not spread this way, include HIV, Hepatitis B and Tuberculosis. By swallowing contaminated material Most infections of the gut are spread by this route. For example: food poisoning and Typhoid. Other infections, including HIV and Hepatitis B, cannot be caught this way as the acid in the stomach destroys them. By droplets in the air Many infections are spread by the airborne route. Measles, the common cold and influenza are spread in this way, by coughing and sneezing. By sexual intercourse Infections such as Syphilis, Gonorrhoea, HIV infection, Hepatitis B and Hepatitis C can be spread by sexual contact. By blood to blood transmission A small number of infections can be spread through blood transfusion and some can also be transmitted sexually, including HIV, Hepatitis B and Hepatitis C. Vertical transmission from a pregnant mother to her child Transmission can occur at any stage during pregnancy, at the time of birth and during breast feeding. Examples include HIV, Syphilis and some common viral infections such as Rubella (German Measles). Insects and Parasites e.g. Malaria is spread via a mosquito’s bite. 1.2 INFECTION CONTROL GUIDANCE Infection control forms part of our everyday lives, usually in the form of common sense and basic hygiene procedures. Where large numbers of people come in contact with each other, the risk of spreading infection increases. This is particularly so where people are in close contact and share eating and living accommodation. It is important to have guidelines to protect service users, staff and visitors. Adopting these guidelines and standard infection control practices will minimise the spread of infectious diseases to everyone. External Factors If you or someone in your immediate family has a “Notifiable Disease” such as Measles (see 1.3) or infection such as Impetigo, diarrhoea, vomiting or Scabies, please inform your line manager before coming to work. If you regularly visit people in hospital please be aware of the potential risk of cross infection to yourself and the person you are visiting. Above all when dealing with service users and their families we must all remember we are dealing with people. There will be personal issues of privacy and sensitivity, which we must handle with tact and discretion at all times. What are Infection Control Practices? Infection control practices are ways that everyone (staff, service users & volunteers) can prevent the transmission of infection from one person to another. They are practices which should be routinely adopted, at all times with every individual, on every occasion, regardless of whether or not that person is known to have an infection. 1.2 INFECTION CONTROL GUIDANCE – cont. Infection control practices include: Effective hand washing and hand hygiene Safe Management of blood or body fluid spillages Safe use and disposal of sharps Appropriate use of personal protective equipment STANDARD INFECTION CONTROL PRACTICES Safe Management of contaminated waste Maintenance of a clean environment by appropriate use of cleaning equipment Safe Management of laundry TRAINING Underpins all these Routine Infection Control Practices 1.3 NOTIFICATION OF INFECTIOUS DISEASES A number of infectious diseases are statutorily notifiable under The Public Health (Control of Disease) Act 1984 and The Public Health (Infectious Diseases) Regulations 1988. There are three main reasons for such notification. So that control measures can be taken To monitor preventative programmes For surveillance of infectious diseases in order to monitor levels of infectious diseases and to detect outbreaks so that effective control measures can be taken. All doctors diagnosing or suspecting a case of any of the infectious diseases listed overleaf have a legal duty to report it to the Proper Officer of the Local Authority, who is usually the Consultant in Communicable Disease Control based at the Health Protection Agency. Notification should be made at the time of clinical diagnosis and should not be delayed until laboratory confirmation is received. Infections marked (T) should be notified by telephone to the Consultant in Communicable Disease Control (see Section 5) and confirmed by completion of a written notification form. 1.3 NOTIFICATION OF INFECTIOUS DISEASES – cont. Notifiable Diseases Acute encephalitis Paratyphoid (T) Acute poliomyelitis Plague (T) Anthrax Rabies (T) (T) Cholera (T) Relapsing Fever Diphtheria (T) Rubella Dysentry (T) Scarlet Fever Food poisoning or Small Pox suspected food poisoning Leprosy Tetanus Leptospirosis Tuberculosis Malaria Typhoid fever (T) Measles Typhus fever (T) (T) Meningitis * (T) Viral haemorrhagic fever Meningococcal septicaemia (T) Viral hepatitis ** (without meningitis) Mumps Whooping cough Opthalmia neonatorum Yellow fever * meningococcal, pneumococcal, haemophilus influenzae, viral, other specified, unspecified ** Hepatitis A, Hepatitis B & Hepatitis C, other (T) Please notify the Consultant in Communicable Disease Control or person on call for the Health Protection Agency by telephone. Other specific diseases are designated by the Reporting of Injuries, Diseases and Dangerous Occurrences Regulations 1995 as “Reportable Occupational Diseases” e.g. Legionellosis. Please contact the Health & Safety Team for further information (see section 5 for details). 1.3 NOTIFICATION OF INFECTIOUS DISEASES – cont. Notification of suspected outbreaks An outbreak is defined as two or more cases of a condition related in time and location with suspicion of transmission. Prompt investigation of an outbreak and introduction of control measures depends upon early communication. Suspicion of any association between cases should prompt contact with the Health Protection Agency. 1.4 IMMUNISATION COSHH requires that if a risk assessment shows there to be a risk of exposure to biological agents for which vaccines exist, then these should be offered if the employee is not already immune. In practice, with Social Care Services, this generally amounts to care staff within the Mental Health and Learning Disabilities Services being offered Hepatitis B vaccination. Care home managers, after assessing risks, may also offer ‘flu vaccination to staff and individual cases may indicate the need for immunisation in certain circumstances. The pros and cons of immunisation/non-immunisation should be explained when making the offer of immunisation. The Health & Safety at Work Act 1974 requires that employees are not charged for protective measures such as immunisation. A few GPs will make vaccinations available free to Social Care workers but they are not obliged to do so and can charge at their discretion. Departmental funding for the provision of vaccine, through Occupational Health, is restricted and so it is vital that only those to whom it is essential to provide immunisation are offered this service. The majority of staff will have received immunisation from childhood and have received the appropriate booster doses e.g. Tetanus, Rubella, Measles and Polio. However, it is important for the immunisation state of staff to be checked e.g. women of childbearing age should be protected against Rubella. Good practice and common sense should indicate that the immunisation state of staff is checked and appropriate action taken. If there is a potential risk of infection, change of work rotas or areas of responsibility can sometimes avoid the risk of contamination. Vaccination is not always the only course of action and in some cases staff may not agree to be vaccinated. 1.4.1 IMMUNISATION SCHEDULE Vaccine D/T/P and Hib Polio Age 1st dose at 2 months 2nd dose at 3 months 3rd dose at 4 months Notes Primary Course Measles / Mumps / Rubella (MMR) 12 – 15 months Can be given at any age over 12 months Booster DT and Polio, MMR second dose 3 – 5 years Three years after completion of primary course BCG 10 – 14 years or infancy Only offered to certain high risk groups after an initial risk assessment Booster Tetanus, Diphtheria and Polio 13 – 18 years Children should therefore have received the following vaccines: By 6 months: 3 doses of DTP, Hib and Polio By 15 months: Measles / Mumps / Rubella By school entry: 4th DT and Polio; second dose of Measles / Mumps / Rubella Between 10 & 14 years: BCG (certain high risk groups only) Before leaving school: 5th Polio and Tetanus Diphtheria (Td) Adults should receive the following vaccines: Women sero-negative Rubella For Rubella: Previously un-immunised Polio, Tetanus, Diphtheria Individuals: Individuals in high Hepatitis B, Hepatitis A, Influenza risk groups: Pneumonococcal vaccine 1.5 EXCLUSION FROM WORK The following table gives advice on the minimum period of exclusions from work for staff members suffering from infectious disease (cases) or in contact with a case of infection in their own homes (home contacts). Advice on work exclusions can be sought from CCDC (Consultant in Communicable Disease Control) / HPN (Health Protection Nurse) / CICN (Community Infection Control Nurse) / EHO (Environmental Health Officer) or GP (General Practitioner) Minimum exclusion period Home contact Disease Period of Infectivity Case Chickenpox Infectious for 1-2 days before the onset of symptoms and 6 days after rash appears or until lesions are crusted (if longer) 6 days from onset of rash None. Non-immune pregnant women should seek medical advice Conjunctivitis Until 48 hours after treatment Until discharge stops None Erythema infectiosum (slapped cheek syndrome) 4 days before and until 4 days after the onset of the rash Until clinically well None. Pregnant women should seek medical advice Gastroenteritis (including salmonellosis and shigellosis) As long as organism is present in stools, but mainly while diarrhoea lasts CCDC or EHO will advise on local policy Glandular fever Giardia lamblia Hand, foot and mouth disease When symptomatic While diarrhoea is present As long as active ulcers are present Hepatitis A The incubation period is 15-50 days, average 28-30 days. Maximum infectivity occurs during the latter half of the incubation period and continues until 7 days after jaundice appears For life Until clinically well and 48 hours without diarrhoea or vomiting. CCDC or EHO may advise a longer period of exclusion Until clinically well Until 48 hours after first normal stool 1 week or until open lesions are healed 1 week after onset of jaundice None None HIV/AIDS None None None None – immunisation advised (through GP) may be 1.5 EXCLUSION FROM WORK – cont. Minimum exclusion period Home contact Disease Period of infectivity Case Measles Up to 4 days before and until 4 days after the rash appears Varies with organism Greatest infectivity from 2 days before the onset of symptoms to 4 days after symptoms appear 1 week before and until 5 days after the onset of the rash As long as the organism is present in the throat, usually up to 48 hours after antibiotic is started Until after the last of the lesions are dry Depends on part infected. Patients with open TB usually become noninfectious after 2 weeks of treatment As long as eggs present on perianal skin As long as case harbours the organism 1 week before and until 3 weeks after onset of cough (or 5 days after the start of antibiotic treatment) 4 days from the onset of the rash None Until clinical recovery 4 days from the onset of the rash None None 4 days from the onset of the rash None Until clinically improved (usually 48 hours after antibiotic is started) None Until all lesions are dry – minimum 6 days from the onset of the rash In the case of open TB, until cleared by TB clinic. No exclusion necessary in other situations None but requires treatment None Seek advice from CCDC Seek advice from CCDC Until clinically well, but check with CCDC None Meningitis Mumps Rubella (German measles) Streptococcal sore throat and Scarlet fever Shingles Tuberculosis Threadworm Typhoid fever Whooping cough Will require medical follow-up Treatment is necessary 1.5 EXCLUSION FROM WORK – cont. SKIN CONDITIONS Minimum exclusion period Home contact Disease Period of infectivity Case Impetigo As long as purulent lesions are present As long as lice or live eggs are present Until skin has healed or 48 hours after treatment started Exclude until treated None. Avoid sharing towels As long as active lesions are present Exclusion not always necessary until an epidemic is suspected None None None Until day after treatment is given None None (GP should treat family) None (warts should be covered with waterproof dressing for swimming and barefoot activities) None Head lice Ringworm 1. Tinea capitis (head) 2. Tinea corporis (body) As long as active lesions are present 3. Tinea pedis (athlete’s foot) Scabies As long as active lesions are present Until mites and eggs have been destroyed As long as wart is present Verrucae (plantar warts) Exclude until treated None