2003 Edition - Association of Air Medical Services
advertisement

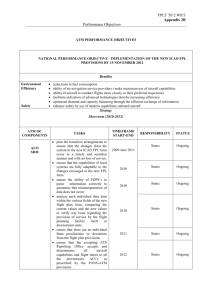
Association of Air Medical Services and CORE Industry Safety Committees Position Statements Published by Association of Air Medical Services 526 King Street Suite 415 Alexandria, VA 22314-3143 (703) 836-8732 phone (703) 836-8920 fax www. aarns org 2003 Edition Copyright © 2000 Association of Air Medical Services & CORE Industry Safety Committee Safety Position Paper 2000 Association of Air Medical Services and CORE Industry Safety Committees Position Statements Table of Contents Safety within an Air Medical Program 2 Improving Safety through the Establishment of a Safety Based Culture 4 Appropriate Flight Crew Scheduling and Provision for Adequate Rest 7 Improved Flight Safety through Crew Member Interaction (CRM) with Pilot in Command 10 Personal Protective Equipment for Flight Crew Members 13 Flight Crew Refusal to Participate in a flight as a Result of Concern for Personal Safety 19 Special Programs designed to Improve the Flight Team Members’ Physical and Mental Well Being 21 The Role of the Communications Center in Enhancing Air Medical Safety 23 Safety Consideration for the Combative or Potentially Combative Patient 26 Loading and Unloading of Patients with the Aircraft Rotors Turning 28 Aircraft Emergencies 29 Weapons of Mass Effect 30 2 Association of Air Medical Services & CORE Industry Safety Committee Safety Position Paper 2000 SAFETY WITHIN AN AIR MEDICAL PROGRAM Problem Statement: Air medical accidents continue to occur despite efforts to improve safety within the air medical industry. Significance: The use of helicopters and fixed wing aircraft to transport patients is a recognized part of the health care system in the US as well as several countries around the globe. EMS helicopters are twice as likely to be involved in a reportable crash and four times as likely to involve fatalities as were all helicopters operated under FAR Part I 35. Helicopters and airplanes used in EMS require extensive modification to accommodate the medical equipment on board the aircraft for patient care. In case of an aircraft accident, these modifications may contribute to occupant injury and death. As an industry, we must continue to pursue opportunities to minimize the risks associated with air medical transport for our pilots, crewmembers and patients. 7 3 Association of Air Medical Services & CORE Industry Safety Committee Safety Position Paper 2000 Bibliography 1. Dodd, R. (1992). Factors Related to Occupant Crash Survival in Emergency Medical Service Helicopters. Dissertation John Hopkins University/Aviation Science and Technology. 4 Association of Air Medical Services & CORE Industry Safety Committee Safety Position Paper 2000 IMPROVING SAFETY THROUGH THE ESTABLISHMENT OF A SAFETY-BASED CULTURE Background: A safety-based culture is defined by everyone feeling a responsibility for safety and pursues safety improvement opportunities on a daily basis (1). A safety-based culture provides the framework for the safety program for any air medical service. Recommendations: Paradigm Shifts for a Safety-Based Culture “In order to exceed current levels in safety excellence and reach the goal of a safety-based culture, there needs to be changes in behavior, attitudes and perception a true paradigm shift for total safety. These shifts require new principles, approaches and procedures and will result in different behaviors and attitudes among the entire team, from top management to hourly staff. An added benefit will be a sense of empowerment and consequently, support throughout the entire culture”(l). — The ten changes are: From Government Regulations to Corporate Responsibility From Failure Oriented to Achievement Oriented From Outcome Focused to Behavior Focused From Top-Down Control to Bottom-Up Involvement From individualism to Team Work From a Piecemeal to a Systems Approach From a Fault-finding to Fact-finding From Reactive to Proactive From Quick Fix to Continuous Improvement From Priority to Value (2). 4 5 Association of Air Medical Services & CORE Industry Safety Committee Safety Position Paper 2000 As an outgrowth of a safety-based culture, human factors associated with air medical transport need be a day-to-day focus for all members of the air medical transport team and support staff. Initial and annual training in the various aspects of human factors should be required of all team members (administration, pilots, mechanics, communications and medical crews). Creating A Safety Committee: A Safety Committee is a part of every air medical program and can contribute to the development of a safety-based culture. The air medical program’s safety committee, when applicable, must be a partnership between the aviation operator and the program/hospital. The Safety Committee should be aware of industry trends for safety enhancement including professional organizations’ efforts to address safety standards for their membership. The Safety Committee should be empowered to develop policies and make recommendations for safety enhancement to include but not be limited to: Develop and communicate a Safety Mission Statement Create an Education and Training Process Develop Evaluation Procedures Contribute to a Performance Feedback Mechanism Continuous Quality Improvement as it Pertains to Safety Association Position: The Air Medical Program leadership has a responsibility to develop a safety-focused culture by identifying and implementing the essential elements of a safety culture and by developing and empowering a safety committee. 6 Association of Air Medical Services & CORE Industry Safety Committee Safety Position Paper 2000 References 1. Dickinson, L. (1998). Creating a Safety Based Culture. AAMS Medical Transport Leadership Institute, Topic 110. 2. Dodd, R. (1992). Factors Related to Occupant Crash Survival in Emergency Medical Service Helicopters. Dissertation John Hopkins University/Aviation Science and Technology. 7 APPROPRIATE FLIGHT CREW SCHEDULING AND PROVISION FOR ADEQUATE REST Background Many fatigue countermeasures have been proposed. To date, only one approach improved work schedule systems has proven to provide positive long-term effects. Improved work schedule systems recognize that cultural, social, individual, and chrono-biological factors must all be considered in the design of a scheduling system. Such a system requires cooperation and active participation between workers and the organization(s) (1). Chrono-biologists have shown that in order to maximize performance, shifts should be changed infrequently, in a forwardrotating direction (i.e. from day to evening to night), with days off scheduled so as to allow maximum transition between shifts (2). — — The National Transportation Safety Board (NTSB) has published a safety study that clearly documents a relationship between performance levels and adequate rest. Alertness, fine motor skills, and judgment deteriorate significantly when adequate rest is not obtained (3). (Adequate fluids and nutrition are also required for optimal performance) (4). Prior to the institution in the mid-80’s of Federal Aviation Administration (FAA) regulations mandating pilots receive a minimum of eight to ten (8-1 0) hours of uninterrupted rest within a 24-hour period, the air medical transport industry suffered its worst year ever with regard to EMS incidents/crashes. Most of the accidents involved fatalities (5). After the minimum rest statutes were implemented, the accident rate declined sharply. While these Federal Aviation Regulation (FAR) requirements under Part I 35 apply only to pilots and not to other air medical transport crewmembers, it is common sense that safety will be enhanced if every single member of the transport team is adequately rested. To provide for maximum safety and job performance, non-pilot crewmembers should receive a minimum of eight hours uninterrupted rest within every 24-hour period during peak transport seasons and six hours interrupted rest during slow transport seasons. These 24-hour periods include on-call time as well as actual on-duty time. According to the National EMS Pilots Association Safety Guidelines, fatigue cannot always be self-determined, and in most cases it may not be apparent until serious errors are made (6). Therefore, in order to demonstrate a paradigm shift of being ‘proactive rather than reactive’, scheduling must allow for no less than these minimums of rest periods. “. . . . . .“ Recommendation The Association of Air Medical Services recommends that all flight programs recognize that fatigue compromises safe decision-making. Programs must realize the importance of adequate rest and enforce procedures, which through a proactive stance promotes appropriate scheduling. 8 Association Position: A written policy should be established so that fatigued personnel can be removed from service, and/or back-up personnel identified to assume flight duty should a crew member become excessively fatigued or otherwise unable to perform optimally at any time. Association ofAir Medical Services & CORE Industry Safety Committee Safety Position Paper 2000 References 1. Tepas, DI. and Monk, TM. (1987)Workschedules. In: HandbookofHuman Factors, G. Salvendy, (Ed.). New York: John Wiley & Sons. 2. National Flight Nurses Association Position Statement: “Improving safety in the airmedical helicopterenvironmenf’. Issue 1, 1998. 3. National Transportation Safety Board, Dodd R.S. : Safety Study, commercial emergency medical services helicopter operations. U. S. Department of Commerce, National Technical Information Service. January, 1988, Report #NTSB/SS-8801. 4. Rayman R.B.: Passenger safety, health, and comfort: a review. Aviation Space & Environment Medicine. 1997; 68 (5) 432-40. 5. North, Michelle. Rocky Mountain Helicopters Online. White Papers: EMS crew interactive roles; pilot and flight nurse. 1997. 6. National EMS Pilots Association Safety Guidelines. In: National Flight Nurses Association Position Statement: “Improving safety in the air-medical helicopter environment’~ Issue 1. 1998. — — 9 8 Association of Air Medical Services & CORE Industry Safety Committee Safety Position Paper 2000 Bibliography Cauthorne CV., Fedorowicz, R.J.: EMS Helicopter Pilots and TheirWork Schedules: an Analysis. Hospital Aviation I 986; March: 1 8-24. Collett H.M.: Air Medical Accident Rates. JournalofAirMedical Transport 1991; 10 (2): 14-15. Dodd, R.S. : EMS Helicopter Safety Revisited. Hospital Aviation I 989; 1 : 6-8. Martin, T. : Adverse Effects of Rotating Schedules on the Circadian Rhythms of Air Medical Crews. Air MedicaiJournal. April—June, 1995: 83-86. NFNA. Performance Standards, Safety Recommendations. Standards of Flight Nursing Practice, 2ed., 1995. P. 67. Preston, N.: Air Medical Helicopter Accident Rates. Journal of Air Medical Transport. 1992; 11(2): 14 - 16. 10 Wright, D.: Safety Management vs. Picking Leaves. Journal of Air Medical Transport. 1991; 10 (9): 11-2. Wright, D.: An Analysis of Shift Work and Emergency Medical Service Helicopter Pilot Performance: Unpublished Manuscript, 1984. 9 Association ofAir Medical Services & CORE Industry Safety Committee Safety Position Paper 2000 IMPROVED FLIGHT SAFETY THROUGH CREW MEMBER INTERACTION (CRM) WITH PILOT IN COMMAND Background: 11 The paradigm shift from individualism to teamwork requires an “entire-crew-oriented” approach to creating and maintaining a safe environment for air medical transport. In Practice Standards for Flight Nursing, the standards of professional performance for flight nurses are: ‘safe transport of the client and others during transport, as well as, (participating) in the safety ofthe aircraft and all others aboard the aircraft (1). It is well recognized that all air medical crewmembers, in cooperative efforts with the pilot in command, play an important role in assuring a safe aviation environment. Subsequently, Crew Resource Management (CRM) must be a CORE VALUE (rather than a mere priority) of EVERY air medical program. After the unacceptable accident rate (of a high as 13.4 accidents per 100,000 hours most resulting in fatalities) of the early 80’s, the air medical industry attempted every possible course of action to reduce this high rate. Notably, the highest percentage of accidents were a result of some human factor or error, and it was determined that, somehow, there had to be developed interaction between all crewmembers and the pilot. The medical aircrew is a team and must work together helping each other to do the best job possible for the team rather than working separately as an individual (2). — Recommendations: It is believed that effective teamwork and communication between crewmembers will ‘save more lives than Nomex or helmets’ (3). This communication should include pre-mission and/or shift briefings, pre-flight checklists, post-mission briefings, and minimum requirement of annual safety training, to include education and practice of appropriate actions during an aircraft emergency (4). Data identified in the usually more formal and written post-mission briefings should serve as a basis for identifying potential problems and monitoring trends. This information should include feedback from all crewmembers involved in the particular mission, (including dispatch personnel), and should not be used as a punitive measure. According to results of two surveys conducted by the National Flight Nurses Association, 32% of respondents in 1988 and 60% ofthel998 respondents practiced CRM in their programs, while 62% in 1988 and 71 % in I 998 had written policies addressing such (5). If doing all in our power to ensure a safe aviaUon environment is truly a core value, we understand that pilots are no longer solely responsible for creating this safe environment, and therefore, these statistics must become 100% industry-wide! Association Position: . . • All air medical team members should receive training in Crew Resource Management initially upon hire and at least annually thereafter. A policy and practice of conducting pre-mission and/or shift briefings, pre-flight checklists, post-mission briefings with documentation for trending purposes must be in place and tailored to fit each program’s specific needs. A minimum requirement of annual safety training, to include education and practice of appropriate actions during an aircraft emergency should also be in place. 12 1 0 Association ofAir Medical Services & CORE Industry Safety Committee Safety Position Paper 2000 References I . National Flight Nurses Association. Performance Standards, Safety Recommendations. Standards ofFlight Nursing Practice, 2 ed., 1995. P. 67. 2. North, Michelle. Rocky Mountain Helicopters Online. White Papers: EMS crew Interactive roles: pilot and flight nurse. I 997. 3. AAMS & CORE Industry Safety Committee Members at 1998 Air Medical Transport Conference, Safety Committee Meeting. Albuquerque, New Mexico; October, 1998. 4. National Flight Nurses Association Position Statement: “Improving safety in the airmedical helicopterenvironment” Issue 1. 1998. 5. National Flight Nurses Association Safety Survey. In: Position Statement; “Improving safety in the air-medical helicopter environmenf’: Appendix B, 1998. — — 13 1 1 Association of Air Medical Services & CORE Industry Safety Committee Safety Position Paper 2000 Bibliography CAMTS. Commission on Accreditation of Medical Transport Systems. Accreditation Standards, 3rd ed., 1997. Collett HM: Air medical accident rates. Journal ofAir Medical Transport, 1991; 10 (2): 14-15. Dickinson, L. (1998). Creating a Safety Based Culture. AAMS Medical Transport Leadership Institute, Topic 110. Dodd, R.S.: EMS helicopter safety revisited. Hospital Aviation 1989; 1: 6-7. Preston, N: Air medical helicopter accidents rates. Journal of Air MedicalTransport. 1992; 11(2): 14-16. Wright, A. E., Campos, J. A., Gorder, T.: The effect of an in-flight, emergency training program on crew confidence. Air Medical Journal, 1994; 13 (4): 127-31. Wright D: Safety management vs. picking leaves. Journal of Air Medical Transport. 1991; 10(9): 11-2. 14 1 2 Association of Air Medical Services & CORE Industry Safety Committee Safety Position Paper 2000 PERSONAL PROTECTIVE EQUIPMENT FOR FLIGHT CREW MEMBERS Background: A systems approach to safety requires recognition that each and every aspect of creating and/or maintaining the safest environment possible must be explored. Certainly, personal protective gear for flight crew members is an important piece of that “puzzle”. But there are other aspects of HEMS operations that likely play a far more important role in the overall safety picture than what crew members wear (1). The focus of safety should be on prevention of the injury and/or fatality-causing incident. Those preventive measures begin with appropriate aircraft selection, configuration, maintenance, etc. and continue along a chain of events, which occur long before the crew members don whatever personal protective equipment is chosen or required for them. , 15 Appropriate crewmember training, effective Crew Resource Management (CRM), and improved crew awareness are at least as important as what personal protective gear is worn. Perhaps the most important protective “gear” of all is the “putting on” of an attitude of personal commitment and responsibility to safety. Until the staggering rise in fatal helicopter crashes in 1 986, most civilian EMS programs required little or no personal protective gear for their crewmembers. Even after it was documented that many of these crashes may well have been survivable had “additional safety equipment” been utilized, the HEMS industry as a whole has not come to agreement on what minimum protective gear should be required (2). Nearly all of the statistical data obtained thus far has come from military, rather than civilian, investigations. While it can be argues that there are some differences in military missions when compared to civilian ones, a helicopter crash is a helicopter crash, regardless of whether it occurs during civilian or military operations (3). Recommendations: The National Transportation Safety Board began an investigation into the growing number of EMS helicopter incidents/crashes, with the completion of the comprehensive study in 1 988. Resulting from this study, safety-improving recommendations were made and presented to both the FAA and the Association ofAir Medical Services (AAMS) as Class-Il, Priority Action recommendations. Specifically related to individual crewmember protective gear was the following recommendation. “Encourage members who operate emergency medical service (EMS) programs to provide medical personnel who routinely fly EMS helicopter missions with protective clothing and equipment to reduce the chance of injury and death in survivable accidents. This clothing and equipment should include protective helmets, flame and heat resistant flight suits and protective footwear”(4). The NTSB recommendations were supported and adopted by AAMS four years later when the I 992 Safety Congress published the position that “flight programs doing scene work have head protection, Nomex uniforms, and boots with steel toes and shanks.” Further, the Safety Congress recommended, “all EMS helicopter personnel wear helmets for head protection” (5). Extensive studies completed by military research teams, largely comprised of U. S. Army operations data, indicate that of accidents in U.S. Army helicopters, 24% of all injuries sustained were to the head and face, and nearly 25% of these were fatal injuries. Further, data presented in the U. S. Army’s Aircraft Crash Survival Design Guide TR 79-22B indicates that spinal injuries resulting from vertical direction impact and head injuries caused by unrestrained contact with the environment are the major cases of both severe injury and disability in rotorcraft accidents (6). 1 3 Association of Air Medical Services & CORE Industry Safety Committee Safety Position Paper 16 2000 It is obvious from the statistical review of injury patterns and percentages that flight helmets provide much needed protection to flight crew members. Helmets specifically designed for use in rotor wing aircraft provide additional protection to hearing, and allow for improved communication during operations. The face shields on these helmets also provides visual protection, and may very well prevent a crash in the case of a bird strike or other potentially sight-threatening event encountered during flight (7). However, helmets must be fitted to each individual appropriately, worn according to manufacturer guidelines, and then properly maintained to ensure adequate protective performance. These factors make helmet purchase and/or upkeep a financial commitment, and are, even under ideal circumstances, no substitute for the basics of crash-attenuating seats, clear head-strike zones, and full safety-belt protection, including shoulder harnesses (8). The widespread use of crash-resistance fuel cells has significantly decreased the incidence of post-crash fires. Currently available statistics indicate this incidence in survivable air-medical accidents to be less than 25%, although the potential exists in every serious crash (9). Therefore, the recommendation for crew members’ wearing of flame-retardant (Nomex) clothing is a logical added protection in those occurrences. (For a complete discussion of the appropriate feature of such clothing, minimum recommended flammability and heat-transfer characteristics, and guidelines for proper wearing of Nomex garments, please refer to the National Flight Nurses Association Position Statements: Flight Nurse Safety In The Pdr Medical Environment, Revised January, 1998) (10). However, in orderto achieve maximum protection, such clothing must be specifically laundered, worn within certain air gap and layering guidelines, and used in conjunction with only natural-fiber undergarments. (i.e. cotton, wool) (1 1) It must also be kept in mind that maximum protection from thermal injury is provided only with the use of Nomex gloves and outerwear/coats (12). While the debate regarding the use of helmets and Nomex rages on, the one certainly is that the greater the amount of appropriate protective gear utilized in the operations of air medical transport, the lesser the risk of injury. Such personal protective gear is costly to obtain and maintain. However, programs wishing to provide continuous improvement rather than a “quick fix” in this area will take a serous look at the best use of these frequently limited funds, and training and maintenance will not suffer because of “some helmet of nomex obsession.” (13) Adequate personal protective gear for crew members should not be limited to clothing and headwear. Survival equipment (and training in its effective use) is also included in a plan to provide maximum protection. Since the ability to summon help, or to survive until help arrives, may very well be the crew members’ best protection against life-threatening injury, each member should have a small survival “pack” within easy access inside the cabin of the aircraft (14). This pack can be small in size and contain only minimum equipment for signaling, attracting attention, and maintaining body temperature. Lastly, pilots and other crew members should be in good enough physical shape to safety do the lifting and carrying that are required in their jobs. The physical ability to extricate oneself from an aircraft after an incident/crash should also be considered when setting guidelines for minimum personal protective “gear”(l 5). 17 1 4 Association ofAir Medical Services & CORE Industry Safety Committee Safety Position Paper 2000 Association Position: • • The Association of Air medical Services and the CORE Industry Safety Committee believes that safety can be enhanced through use of personal protective equipment and safety equipment training. Programs should evaluate the benefits of helmets, fire-retardant clothing and survival equipment training and use. Minimally, all air medical crews should routinely wear hearing protection when working in or around an aircraft with engines in operation. 18 1 5 Association ofAir Medical Services & CORE Industry Safety Committee Safety Position Paper 2000 References 1. Flight Med Archive; Tuesday, 09 March 1999 2. Schneider, Andrew. The Pittsburgh Press. “Nation’s Medevac Crews Want Safety Changes to Increase Survival” November 1, 1987. 3. 4. 5. National Transportation Safety Board, Bureau of Safety Program. Safety Study: Commercial Emergency Medical Service Helicopter Operations, NTSB/SS-88/01, Washington, D.C. January 28, 1988. 6. Aviation Safety Institute: Analysis of 84 Aeromedical Helicopter Accidents and Incidents for the Period 1975-1986; December 3, 1986. 7. National Transportation Safety Board, Dodd, R.S. : Safety Study: Commercial Emergency Medical Service Helicopter Operations. U.S. Department of Commerce, National Technical Information Service. January, 1 988; Report #NTSB/SS-88/01. 8. National Transportation Safety Board, Bureau of Safety Program. Safety Study: Commercial Emergency Medical Service Helicopter Operations, NTSB/SS-8801 Washington, D.C. January 28, 1988. 19 , 9. Association of Air Medical Services: Air Medical Safety Congress Proceedings and Recommendations. Recommendation: Protective Clothing. 12.1-12.1, 1992. 10. ASHBEAMS: Interim Safety Guidelines, developed in conjunction with NFNA, NFPA, and HAl/EMS Committee. 1987. 11. Shanahan, D. R., Shanahan, MO.: Injury in U. DS. Army Helicopter Crashes, October, 1979-September, 1985. J. Trauma 1989; 29 (4):415-423 12. Analysis of U. S. Army HelicopterAccidents to Define Impact Injury Problems. Paper published by NATO/AGARD Conference on ImpactAcceleration, June 1971. I 3. Crowley JS: Should Helicopter Frequent Flyers Wear Head Protection? A Study of Helmet Effectiveness. J. 0cc. Med. 1991:33 (7):766-769. 14. Reading, T.E., et al. SPH-4, U.S. Army Flight Helmet Performance 1972-1983, USAARL Report No 85-1 I -31 November, 1984. , , I 5. Dodd, R. S. : The Cost-Effectiveness of Air Medical Helicopter Crash Survival Enhancements. An Evaluation of the Cost, Benefits and Effectiveness of Injury Prevention Interventions Air Medical Journal. 13 (7): 281-96, July, 1994. 16. Coleman, J. W., Akif, 0. B., Laananen D, Simula, Inc.: Analysis of Rotorcraft Crash Dynamics for Development of Improved Crashworthiness Design Criteria: Sponsored by FAA Technical Center, Final Report June 1985:DOT/FAA/CT-85/11. 1 6 Association ofAir Medical Services & CORE Industry Safety Committee Safety Position Paper 2000 17. Albright, J.D., Et al. The Testing ofThermal Protective Clothing in a Reproducible Fuel Fire Environment, a Feasibility Study. USAARL Report No. 71-24: 1-15, June 1971. References (cont.) 18. Ripple, G. R.; Torrington, K. G.; Phillips, Y.Y.: Predictive Criteria For Burns From Brief Thermal Exposures. J. 0cc. Med. 1990:32(3):215-219. I 9. National Flight Nurses Association Position Statement: “Improving Safety in the Air Medical HelicopterEnvironment” Issue 1, 1998. — 20 20. 21 Know, F. S. Ill, et al: Engineering Test of Lightweight Underwear of the Winter Flight Clothing Systems Thermal Protection. USAARL Report No 71-19: 1-31, June 1971. . Neilson G: Safety in a Flash. E.l.duPont de Nemours & Co., Wilmington, DE. 22. Knox F S. Ill, et al: Bioassay ofThermal Protection Afforded by Candidate Flight Suit Fabrics. Aviat Space Environ. Med. 50 (10): 1023-1030, 1979. 23. Knox F. S. Ill, et al: Evaluation of Four Thermally Protective Fabrics Using the USAARL Bioassay Method, USAARL Report No. 78-9:1-19, June 1978. 24. Ripple. G.R., Torrington, K. G. Phillips Y.Y.: Predictive Criteria For Burns From Brief Thermal Exposures. J. 0cc. Med 1990; 32 (3) 215-219. 25. Flight Med Archive: Tuesday, 09 March 1999. 26. Presentation by crew member from team in one of the Carolinas had a crash just 100 yards from an interstate, but could not summon help. Left hanging upside-down in a tree for numerous hours. 27. Flight Med Archive: Tuesday, 09 March 1999. — 1 7 Association ofAir Medical Services & CORE Industry Safety Committee Safety Position Paper 21 2000 Bibliography Analysis of U. S. Army Helicopters Accidents to Define Impact Injury Problems. Paper published by NATO/AGARD Conference on ImpactAcceleration, June 1971. CAMTS. Commission on Accreditation of Medical Transport Systems. Accreditation Standards. 3rd edition, 1997. Carolina Air Care Task Force. Program Safety Review of Carolina Air Care, The North Carolina Memorial Hospital, Chapel Hill, NC, January 1987. Collett, HM: Aeromedical Accident Trends. Hospital Aviation 6:2-6-7/ Collett HM: Air Medical Accident Rates. Journal ofAirMedical Transport 1991; 10(2): 14-15. Crash Survival Design Guide. USAAVI.ARS. Technical report 67-22, U. S. Army Aviation Material Lab. Fr. Eustis, Virginia, August, 1967, updated in 1971. Crashworthiness vs. Cost: A Study of Army Rotary Wing Aircraft Accidents in Period January 1970 through December 1 971 Paper presented at Aircraft Crashworthiness Symposium. University of Cincinnati, Ohio, 6-8 October, 1975. . Crowley J. S. Lucina, JR, Bruckart JE: Flight Helmets: How They Work and Why You Should Wear One. Journal ofAir Medical Transport I 992; 1 1 (8): 1 9-23, 26. Dodd, R.S.: EMS Helicopter Safety Revisited. HospitalAviation 1989; 1:6-8. “General Accident Investigation”. In Aircraft Crashworthiness. Saczalski et al (editors), University of Virginia Press (1975). Harvey, D: Do the Pilots Have the Answers to EMS Safety? Rotor and Wing 15 December, 1980. Helmet Design Criteria for Improved Crash Survival. USAAVLAHSTR 65-44, U. S. Army Aviation Material Lab., Ft. Eustis, Virginia, 1966. Oleske, D.M., Hahn, JJ. Leibold, M. Work-related Injuries to the Foot. (Data from an occupational injury/illness surveillance system). J. 0cc Med. 1992,34(6): 650-655. 22 “Patterns of Injury in Fatal Aircraft Accidents” Aerospace Pathology, Reals and Mason (editors). College ofAmerican Pathologists Foundation (1973), pp. 170-176. , Preston, N. Air Medical Helicopter Accident Rates. Journal of Air Medical Transport 1992 11(2): 14-16. Shanahan, Jim. L.: Basilar Skull Fracture in U. S. Army Aircraft Accidents. Aviat. Space Environ. Med. 54(7)628-631. 1083. Wright, D.: Safety Management vs. Picking Leaves. Journal of Air Medical Transport 1991; 10(9) 11-2. 1 8 Association of Air Medical Services & CORE Industry Safety Committee Safety Position Paper 2000 Wright D.; Einhorn, T: The Final Authority: Hospital Aviation 5:10:36. October, 1986. 23 1 9 Association ofAir Medical Services & CORE Industry Safety Committee Safety Position Paper 2000 FLIGHT CREW REFUSAL TO PARTICIPATE IN A FLIGHT AS A RESULT OF CONCERN FOR PERSONAL SAFETY Background: According to the Federal Aviation Regulation 91 .3a, “The pilot in command of an aircraft is directly responsible for, and is the final authority as to, the operation of that aircraft” (1). Within the air medical transport industry, the pilot in command is responsible for his/her decision to accept a flight request and to continue or terminate the flight. Nobody should not be allowed to influence the pilot to accept or continue a flight when the PlC does not believe that continuing the flight is the safe thing to do. Recommendations: 24 The Association of Air Medical Services and the CORE Industry Safety Committee believe that the personal safety of all flight team members would be enhanced if: Each program leadership team demonstrated their commitment to these principles by implementing a policy describing the flight team members’ responsibility to cancel a flight for reason of concern for personal safety. The policy would define acceptable reasons for refusal to participate. The policy would include a reporting mechanism for such events. The outcome of such refusal and reporting would include an action plan to prevent future occurrences. Association Position: The medical team members have a responsibility to ensure their own safety as well as that of the patient. For these reasons, the medical team members have the right and responsibility to refuse to participate in a flight and to cancel a flight if there is concern for personal safety. 2 0 Association of Air Medical Services & CORE Industry Safety Committee Safety Position Paper 2000 Reference 25 1. Section 91 .3a of Federal Aviation Regulations (FAR). 21 26 Association ofAir Medical Services & CORE Industry Safety Committee Safety Position Paper 2000 SPECIAL PROGRAMS DESIGNED TO IMPROVE THE FLIGHT TEAM MEMBERS’ PHYSICAL AND MENTAL WELL BEING Background: The eight classic stresses of flight as described by the US Air Force (1 ) are discussed as part of flight physiology, a required topic of study for aviators and flight team members. Mitchell (2) describes emergency service stress as common to the rescue. Chronic stress or cumulative stress may be overlooked and in the end, be more destructive than an acute stress reaction because it is often unrecognized and thus not addressed. Excessive suppression of emotions can lead to post Traumatic Stress Disorder (PTSD). In addition, it is well described in the literature that improved physical fitness and physical well being reduces the level of stress and decreases the likelihood of n individual being involved in an accident. Recommendations: Each air medical transport program develops formalized physical fitness programs, stress management programs and Critical Incident Stress Management interventions. Program mangers should be knowledgeable regarding the signs and symptoms of stress and factors leading to critical incident stress. Air Medical Programs should have policies and procedures in place identifying the resources available for air medical crews to access CISD, or other psychological counseling following a critical event. Policies should support the flight team member’s ability to take themselves out of service until the stress response can be mitigated. CISM should be part of every flight team member’s basic curriculum of study. Association Position: The Association of Air medical Services and the CORE Industry Safety Committee believes that safety can be enhanced through improved flight team members’ performance and job satisfaction. • Air medical programs should have a policy and procedure addressing a crewmembers access to Critical Incident Stress Management (CISM). If the psychological impact of the event poses the risk of impairing safe decision making, the crewmember should be removed from duty. 27 2 2 Association of Air Medical Services & CORE Industry Safety Committee Safety Position Paper 2000 References 1. United States Air Force of Aerospace Medicine: Flight nurse handouts, June 1995. 2. Mitchell, J., Bray, G. (1990), Emergency Services Stress, guidelines for preserving the health and careers of emergency services personnel. Englewood Cliffs, NJ: Prentice Hall. 28 2 3 Association ofAir Medical Services & CORE Industry Safety Committee Safety Position Paper 2000 THE ROLE OF THE COMMUNICATIONS CENTER IN ENHANCING AIR MEDICAL SAFETY Background: Several areas of the communication specialists’ duties and responsibilities have a direct role in enhancing safety. Recommendations: The following have a direct role in enhancing safety and outlines items that communication centers should put into place. 29 Training: Training must include all program specific policies and procedures, job expectations, standards, and duties and responsibilities. A formal training program should be developed and followed to ensure that all new hires are given consistent information. Specific items that must be covered in orientation are: Post Accident/Incident Planning Flight Following (Related to FAR 135 requirements) Weather Map Reading Landing Zone Preparation Navigational Aids Stress Management Radio Skills Additional Training: It is recommended that all communication specialists take. The National Association of Air Medical Communication Specialists Training Class. This all inclusive class is the most comprehensive training tool available for new staff. 16 hours of Continuing Education Units (CEU’s) should be completed each calendar year by all communication specialists. These CEU’s should include job specific areas and training. Post Accident Incident Drills. Biannual PAIP drills should be conducted and debriefed with all program members for performance improvement and lessons learned. Commission on Accreditation of Medical Transport Systems (CAMTS). It is recommended that all air medical communication centers adopt the CAMTS standards for communication centers. This will help ensure a quality communication center is in place. 2 4 Association of Air Medical Services & CORE Industry Safety Committee Safety Position Paper 2000 30 Procedures: The following procedures must be developed and readily available in the communication center: Post Accident Incident Plan (Which Includes) Precautionary Landing due to Patient Condition Precautionary Landing due to Weather or Mechanical Conditions Missing or Overdue Aircraft MayDay Post Accident/Incident Lost Communications Equipment Failure Procedures. This procedure must include trouble- shooting procedures for each piece of equipment, emergency procedures for working without the particular item, and the procedure for getting the equipment repaired. Flight Following. The flight following procedure must be in writing and should require the communication specialist to physically plot the aircraft’s flight progress on an area map. If other systems are used to monitor and track flight progress, these too must be of demonstrated proficiency. Schedules: Communication Specialist’s should be scheduled on the console for a maximum of 12 hours per day. Unlike pilots and flight crew members, the communication specialist cannot sleep during duty time. On rare occasions 16-hour shifts are acceptable for coverage of sick call. A minimum of 8 hours between shifts for rest is also highly recommended. Breaks: Staff should be given beaks away from the console. lfthe program’s staffing consists ofjust one communication specialist, the relief person should be equally trained. Breaks should always be delayed when the aircraft is in the air. Meals should be allowed at the console if an unpaid lunch break is the policy. Equipment and Resources: The following equipment and resources must be present in the communication center. Audio Recorder with auto playback capabilities. 2-way~adio system. Service area maps. Emergency Phone Lists Post Accident/Incident Plan Manual. List of all serviced hospitals including landing site information and telephone numbers Committee Participation: A communication specialist should be included on the Safety and Quality committees. Communication Center Layout: Some things to consider when building or remodeling the communication center: 31 Restrooms should be located in close proximity to the communication center. Carpeting should be used on the floor to absorb sound and reduce slipping. Ergonomic seating and console designs should be used to reduce discomfort and personal injury. 2 5 32