Study Guide – Pharmacology Test #1
advertisement

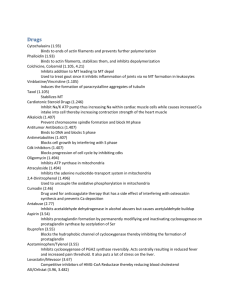
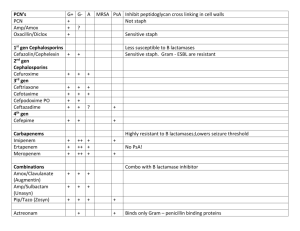
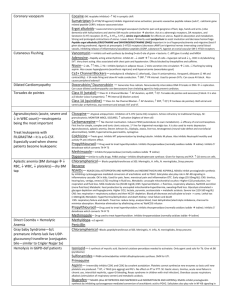
Study Guide – Pharmacology Test #1 Thyroid Gland and hypothyroidism: Abnormality in the thyroid gland. Unable to release thyroid hormones from their storage sites, coupling iodine with tyrosine, trapping iodine, or converting iodide to iodine or any combination. Pituitary gland dsfx and does not secrete TSH to trigger release of T3 and T4. Or level of thyrotropin releasing hormone TRP secreted from hypothalamus is reduced, which results in decreased TSH levels Symptoms: decreased BMR, goiter, thickened skin, hair loss, lethargy, constipation and anorexia. Synthroid (levothyroxine) SE/AE: What does it cause? Cardiac dysrhythmia , palpitations, weight loss Primary teaching points: Do not d/c meds, take at the same time every day, do not switch brands, report chest pain/palpitations, effects may take several months to occur. Always consult your physician before taking OTC meds with levothyroxine. Thyroidectomy, potential complications/symptoms: OD of thyroid replacement drugs. Agonist vs. Antagonist Agonist: binds/stimulates the activity of one or more biochemical receptors in the body…elicits a response Antagonist: binds to and inhibits the activity of one or more biochemical receptors (inhibitors). Define forms of meds: Compressed: scored/shiny coat; keeps dust from forming and keeps from sticking to throat Sustained release (SR): releases drug in controlled/predictable manner; enteric coating to create barrier against stomach acids Osmotic pump: tabs with semiperm. Membrane which allows H20 to enter and drug leave slowly through small hole made by laser when forming the tablet Repeat action: second dose within inner shell Why meds are given one route vs. another Its route of administration effects the rate and extent of absorption of that drug. Enteral: absorbed into systemic circulation through oral/gastric mucosa, small int. or rectum. Absorbed from GI into portal circulation (liver). It may be extensively metabolized by liver before reaching systemic circ Oral: stomach can alter meds, pH, food, etc. Exercise/sepsis cause blood flow to GI tract to be reduced Sublingual: rapid absorption Parenteral: fastest route followed by enteral and topical routes. Refers to any route of admin other than GI tract. SubQ and IM: long acting dosages that take several hours to absorb. Topical: long lasting, local effects with some drugs, but slow in onset and prolonged in offset. Transdermal: bypasses liver and first pass effect, and suitable for pt. who cannot tolerate PO Inhalation: Pulmonary; absorption occurs at the pulmonary alveolus in contact w/ capillaries. Med errors as a nurse – how to reduce risk What is a medication error? “ Any preventable event that may cause or lead to inappropriate med use or pt. harm while the med. Is in control of the healthcare providers, pt. or consumer…” Assessing all parameters w/pt. (vitals, labs & document). Assessing pt. for effects of drugs and consulting reference materials or colleages. Completing ME reporting forms after contacting MD or charge nurse. Monitor pt. progress/condition. Think/act critically to prevent further errors. Conducting detailed RCE (root cause errors). Analyze methods to reduce complexity of drug administration. 1 Transcribing MED order, you can’t read it. What action do you take? Repeat order to confirm with prescriber – never assume! Definitions: Adverse drug event: an injury caused by a medicine or failure to admin. Intended med (may/not be preventable and may/not cause harm) Adverse drug reaction: an unexpected, unintended, undesired or excessive response to a med. (may/not be preventable; i.e. error) Allergic reaction: immunologic hypersensitivity reaction resulting from unusual sensitivity of pt. to a drug. Idiosyncratic reaction: abnormal/unexpected susceptibility to a medication (other than allergy) peculiar to an individual patient. Pharmacuetics: Science of drug dosage form design. Pharmacodynamics: Study of biochemical/physiologic interaction of drugs. Pharmacogenetics: study of genetic factors & their influence on drug response (absence, overabundance, insufficiency of drug metabolism enzymes). Pharmacognosy: study of drugs obtained from natural/plant resources. Pharmacokinetics: study of drug distribution rates between various body compartments, after drug has entered body including (Absorption, Distribution, Metabolism, and Excretion). Empiric theory: admin of antibiotics based on most likely pathogens causing infx. Prophylactic antiB therapy: taken before anticipated exposure Host factor: unique to the body of particular pt. I.e: pregnancy, genetics, site of infx, host defenses, determines success or failure of antiB therapy. B receptors: heart rate increases and bronchial relaxation B1: cardiac, B2: smooth muscle, glands and lungs. Excretion: properties of elimination, which organ systems are involved and how do they excrete? Drugs metabolized by liver are more polar and H20 soluable…by glucuronidasees and hydroxylation/acetylation) Kidneys themselves can form glucorunides and sulfates from various drugs and their metabolites. Filtered via glomerlar filtration, reabsorptiona nd tubular secretion – go through glom. Filtration between the blood vessels and afferent arterioles & glomeruli. Intestines: fat soluble drugs; once in bile, resorbed into bloodstream, returned to liver & again secreted into the bile…this is called enterohepatic circulation Lungs, sweat, salivary and mammary glands excrete drugs. What is distinctive about each of these medications? Erythromycin: (Macrolide) Inhibits protein synth. @ 50S ribosome Contraindicted: hepatic/renal dysfx Upset GI Azythromycin (Zithromax) (Macrolide) Inhibits protein synth @ 50S ribosome Trimethoprimsulfamethoxazole (Septra) (Sulfanamide) Inhibits metabolism of folic acid Prevents prophylaxis of HIV Bronchitis Gonorrhea Rapid PO 2 Tetracycline Inhibits bacteria @ 30S Discolors teeth in children Photosensitivity and avoid DAIRY Contraindicted in pregnancy, and children < 8 Allupurinol Inhibits (xanthine oxidase) production of uric acid – lowering serum uric acid Contraindictions: oral hypoglycemic/warfarin increase efx of drugs *watch kidney fx (toxicity) Cefazolin (Ancef) Cehpalosporin IM or IV Contraindicted: penicillin allergies Gentamycin (Aminoglycoside) gram (-) and (+) *serious toxicities NEPHRO/OTO Interactions: diuretics, skeletal musc. relaxants, anticoags. Tobramycin (Aminoglycoside) gram (-) and (+) *serious toxicities NEPHRO/OTO psueudomonas Interactions: diuretics, skeletal musc. relaxants, anticoags. Ciprofloxin (Cipro) Fluroquinolone gram (+) and (-) Inhibits DNA gyrase s. aureus Contraindicted: Pregnancy/child..alters efx of warfarin, inc. BUN and serum creatinine labs Vancomycin (Fluroquinolone) gram (+) and (-) Inhibits DNA gyrase MRSA Contraindicted: Pregnancy/child..alters efx of warfarin, inc. BUN and serum creatinine labs Amoxicillin Ped. Drops/tabs Infx: ears, nose throat, GU, skin Contraindictions: PKL, watch renal insuff. Decreases contraceptives (warfarin) Insulin lispro (Humalog) Rapid acting: onset 15m, peak 60-90m, dur 3-4h Regular insulin (Humulin R) Short acting: onset 30m, peak 2-3h, dur. 4-6 h NPH (Lente) Intermediate acting: onset 2 h, peak 6-8h, dur 12-16h Humulin U (Ultralente) Long-acting: onset 2 h., peak 16-20h, dur 24+h 3 Sulfonylureas: increase secretion of insulin (stimulate B cells of pancreas). Pt. must have firing pancreas & no sulfa allergies A/E: hypoglycemia Salicylates (Acetic acids) fever, pain, arthritis, thrombolytic; NSAIDs blocks the LT (except ASA) and PG pathway specifically by blocking COX or lipooxygenase Proprionic Acids – tx of rheumatoid arthritis, etc. not for nursing women, preg. Cat D Alpha – glucagons Beta – insulin 4