PUBLIC HEALTH EMERGENCY OPERATIONS PLAN
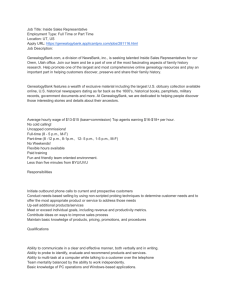
advertisement

DEPARTMENT OF HUMAN RESOURCES DIVISION OF PUBLIC HEALTH EMERGENCY OPERATIONS PLAN: EMERGENCY PREPAREDNESS COORDINATOR ALERT AND NOTIFICATION STANDARD OPERATING PROCEDURE SUPPORT ANNEX A1 11 Dec 2007 I. PURPOSE This Standard Operating Procedure (SOP) provides guidance for the alert and notification of the Georgia Division of Public Health (DPH) Emergency Preparedness Coordinators (EC) at the State and District levels. This SOP will assist the Department of Human Resources (DHR) Emergency Manager, Public Health Leadership, and Public Health District Director’s staff to contact and notify the appropriate level ECs of situations or events that have the potential to be of Public Health significance. II. SITUATION All incidents occur locally and are handled by the local jurisdiction, as stated in the National Incident Management System (NIMS) guidance, as well as through Department of Homeland Security-Federal Emergency Management Agency (DHS-FEMA) and Georgia Emergency Management Agency (GEMA). As incidents mature, assistance may be requested from other agencies, including DHR and/or Public Health. To coordinate intra-state/inter-state/federal assistance/support, Division and District Public Health personnel need to know how to contact the appropriate personnel at all levels and notify them of the situation. The On-Call Representative (OCR) is a generic term that will be used throughout this SOP describing the representative member of the Public Health Emergency Preparedness Staff at all levels that will receive an initial alert. Division OCR signifies the representative at the State level and District OCR signifies the representative at the District level. The OCR can be found by visiting the Division of Public Health State Electronic Notifiable Disease Syndromic Surveillance (SendSS) web site, http://sendss.state.ga.us and searching the On Call Calendar. Page 1 of 125 To assist with the myriad of responsibilities, there are Annexes and Attachments to refer to: -Responsibilities Of On-Call Representative Standard Operating Plan: Attach I: pg 11 -Suggested Responsibilities Of On-Call Emergency Coordinator: Attach II: pg 12 -ESF8 Response in an Emergency, A Public Health Primer Support: Attach III: pg 14 -Suggested “go-bag” Contents: Attach IV: pg 17 -ESF8 (Public Health) Responsibilities, Emergency Operations Center: Attach V: pg 18 -DHR EOC MACC Structure: Attach VI: pg 22 -Threat Level Actions (State, Hospital, Public Health): Attach VII: pg 23 -1-866 PUB-HLTH SOP; Annex A1, Appendix I: pg 43 -1-866-PUB-HLTH SOP: Hotlines Manual; Support Annex A1, Appendix 1, Attachment I: pg 46 -Call-Down Exercise Program Standard Operating Plan: Support Annex A1, Appendix II: pg 112 -Call-Down Feedback Form Support: Annex A1, Appendix II, Attach 1: pg 118 Page 2 of 125 III. ASSUMPTIONS The affected District is aware of its Public Health and non-Public Health capabilities and resources, as related to the primary role of Emergency Support Function (ESF) 8 and support of Emergency Support Function 6. During an event, the affected District will not only use its available resources, but will request and coordinate assistance from adjacent Districts through official and unofficial Memorandum of Understandings (MOUs) or Memorandum of Agreement (MOAs). The District OCR is the “local Public Health” point of contact for any event, emergency or request of Public Health significance. (Note: While the District Emergency Coordinator is expected to be the initial contact during business hours at the District level, identifying the District OCR as the initial contact in this SOP ensures that the representative “on-call” at the time an alert is given is prepared to follow the procedures outlined below.) It is the responsibility of the District OCR to contact and coordinate response activities with other available District resources. As this coordination is occurring, the District OCR will notify the Division OCR, briefing that individual on the situation, including potential requirements. The Division OCR may be aware of events throughout the State, due to alerts/notifications from GEMA, other partners and the media. Therefore, the Division OCR is expected to contact the respective District OCR(s), briefing them of the situation and requesting periodic feed back from the District EC staff. The Division OCR is the conduit to State level resources, including DHR, DPH and GEMA. The Division EC is the conduit to regional/federal resources, including various out of state resources, Disaster Medical Assistant Teams (DMAT), Disaster Mortuary Operational Response Teams DMORT), Strategic National Stockpile (SNS) resources, Assistant Secretary of Preparedness and Response (ASPR) resources, to name a few. Therefore, the District OCR will contact the Division OCR for assistance requesting any out of District resources not previously covered under an MOU or MOA. Page 3 of 125 IV. ALERT AND NOTIFICATION HIERARCHY Consideration must be given to which hierarchy is appropriate under any given incident. The hierarchies listed below can be followed individually or in conjunction with each other. During normal duty hours, alerts should be conducted based on the department’s structure. The department’s lead will make the determination which hierarchy is appropriate. After normal duty hours, the individual reporting an incident must notify the OCR. The OCR will then make the determination which hierarchy is appropriate. A. Intra-Division/Intra-District Alerts requiring responses from key responders within the Division of Public Health will be initiated by the Division Emergency Coordinator or OCR; which ever is available/appropriate. This will be referred to as an Intra-Division alert. Districts will use a similar system where the District Emergency Coordinator/OCR will ensure alerts are given to key responders within the district. This alert will be referred to as an Intra-District alert. B. Division to District, District to District, District to Division Alerts that require notification of key responders outside of the Division/District will fall into three categories: Division to District, District to District, and District to Division. Division to District and District to Division alerts will be the most common. These alerts will be initiated by the department which is the first to become aware of an incident requiring notification of key responders outside of their department. There may also be times which will require a District to alert another District of an immediate, imminent threat. Under any of these three categories, the lead Emergency Coordinator or OCR will determine the appropriate individual/office to contact outside of their department. C. Division to State/Regional/Federal The Division Emergency Coordinator or representative will determine when to contact an agency/department which sits outside of and higher than the Division of Public Health. Districts who need to contact an agency outside of their district (other than another district) and is outside of DPH, must contact the Division Emergency Coordinator to request assistance in contacting that agency/department. V. PUBLIC HEALTH EMERGENCY RESPONDERS The following is a list of offices, agencies, teams, partners, or individuals who have a role within Public Health to respond to and/or coordinate an incident covered under either ESF 6 or ESF 8. This list may not include all potential responders, but should be used as a guide in developing an alert and notification roster. Division Health Emergency Assistance and Resource Team (DHEART), District Health Emergency Assistance and Resource Team (DHEART), County Health Emergency Assistance and Resource Team (CHEART), Regional Coordinating Hospitals (RCH), Page 4 of 125 Other Hospitals, Emergency Preparedness Staff, Emergency Medical Services (EMS), Nurse Managers, Environmental Health Managers, Strategic National Stockpile Staff, PH Directors, Medical Reserve Corps, Emergency Management Agencies (EMA), Public Information Officer, Fire, School System Liaisons, Pharmacists, Immunization Managers, Epidemiologists, Information Technology Manager. Page 5 of 125 VI. CONCEPT OF OPERATIONS: This SOG supports the PH EOP’s 3 phases of emergency management: Phase I: Preparedness and Prevention Phase II: Detection and Response Phase III: Recovery and Mitigation Phase I: PREPAREDNESS/PREVENTION This phase includes preparation for an event of public health significance and prevention of circumstances leading to emergencies. All Districts must be aware of their ESF 6 and 8 capabilities and resources. The District Health Director’s staff should also be aware of the local Emergency Medical Services (EMS), hospital capabilities, Emergency Management Agency (EMA), local Red Cross chapter, Division of Family and Children Services (DFCS), nursing home and other resources and capabilities within their District. This awareness will assist the District Health Director’s staff to know when to request resources from outside the district. The District staff needs to be aware that the DPH staff is available to assist them during an event. Being aware of the procedure to request the appropriate DPH assistance is critical to acquiring that aid quickly. The Division EC works with additional state resource emergency coordinators, including, but not limited to the Assistant Secretary of Preparedness and Response (ASPR) Coordinators, the Strategic National Stockpile (SNS) Coordinator, Chempack Coordinator, the Public Health Exercise Coordinator, Public Health Laboratory, Public Health Chemical-Radiological Emergency Coordinator, Environmental Health, Epidemiology, Division of Mental Health/Developmental Disabilities and Addictive Diseases (MHDDAD), DHR Emergency Management, Nursing, Pharmacy and many others. The Division EC works with and coordinates asset requests with state, regional and federal partners within GEMA, Health and Human Services (HHS) Region IV, DHS-FEMA Region IV, Federal Coordinating Center in Atlanta, Federal Bureau of Investigation (Atlanta Office), Centers For Disease Control and Prevention, and many other partners. The Division Emergency Preparedness staff is responsible to contacting the requested resource coordinators as well as additional DPH and DHR staff to assist in a response. As of December 2006, the Senior Planner within the Division Emergency Preparedness Staff is responsible for all Division on call related duties and is usually the primary normal duty hour Division OCR, with back up from other Division level staff. A) The DHR Emergency Manager, applicable Division of Public Health office and branch leadership, Division Emergency Preparedness Staff, and District ECs contact information is available on SendSS. All OCRs and applicable Division and District staff members are responsible for registering on SendSS and maintaining current contact Page 6 of 125 information. This includes after hours contact information. The on-call calendar needs to be accurately filled in for the current and following month. B) The Division and Districts must identify an OCR for 24/7/365 availability. The OCR will ensure their radio(s), cell phone(s), pager(s) and other electronic contact resources (as stated on the SendSS Contact list) are in good working condition. C) During normal duty hours, the primary means of communication/alert will be the duty phone/work phone. If a District or other contact does not respond within 10 minutes of the initial alert, then other means of contact (as identified in SendSS) will be used until that contact has been alerted. D) The OCR will be immediately available for emergency calls via one of their contact devices and be available to physically respond within a reasonable time to the requested location. If the Primary OCR does not respond to calls or pages, the Back-up OCR will be contacted. If neither responds and it is urgent the Division needs to be notified, the Director of the Office of Emergency Preparedness or the Director of Planning will be contacted. Reasonableness is defined below, unless otherwise stated. 1. Alert and Response – Within 15 minutes 2. Physically respond to designated EOC or other location – Within 90 minutes Page 7 of 125 Phase II: DETECTION/RESPONSE This phase includes the detection of and response to an event of public health significance. Depending upon the nature of the incident, the appropriate response will be determined and acted upon using appropriate annexes, Standard Operating Procedures (SOP) and Standard Operating Guides (SOG). The OCR will make brief notes of the calls and responses, enabling a record log to be maintained for potential legal reasons. The notes will be entered onto WebEOC, under “Significant Events”. Refer to the WebEOC Manual and the PH Emergency Operations Plan Annex A-9 for further guidance to open a new District specific or Statewide Incident. The nature of the event, personnel and/or agencies notified, outcome and any other pertinent information related will be entered into the note. Separate entries by the same reporting individual do not need to me made; the original entry will be updated and saved. If there are entries made by additional personnel, those will be entered as new entries. The log can also be used as a training tool for new on call personnel. At their earliest convenience, the affected District Health Director’s staff will notify the Division EC that an event is occurring in their District. The Division EC will ensure appropriate State, regional and/or federal personnel are notified per protocol or based on the event. As a minimum, the Division EC may notify other members of the PH Emergency Preparedness Team, the Division’s Health Assistance and Resource Team, DHR Emergency Manager and OHSGEMA SOC. As an event matures, the Division EC is responsible to coordinate resource needs for the affected district(s). Most responses can be coordinated while at their work station. As the event becomes more complex, the Division EC may require additional PH and DHR personnel to assist in the response. As those personnel are contacted, the Division EC will coordinate with the DHR Emergency Manager, opening the DHR EOC. The Division EC and DHR Emergency Manager will coordinate with appropriate DHR and DPH management personnel to staff the OHS-GEMA SOC. The Division EC will coordinate with the DHR Emergency Manager, establishing the DHR EOC Incident Command structure, ensuring it is posted on WebEOC and in the DHR EOC. The Division EC and DHR Emergency Manager will establish DHR EOC operational periods with appropriate manning. Appropriate contact numbers within the DHR EOC and OHS-GEMA SOC (PH and DHR only), will be appropriately posted on WebEOC. If there is a National Disaster Medical System (NDMS) response occurring in Atlanta, Augusta or other areas of the state, a personnel support plan will need to be developed. For other extensive and extended operations, such as SNS deployment, large scale evacuations, mass casualties, administration assistance teams may be deployed from DHR to the affected areas. The Division EC and DHR Emergency Manager will coordinate with the deploying team leader(s), assisting as required. The DHR, Division EC and support staff assigned to the OHS-GEMA SOC will notify the Division EC verbally and through WebEOC, that they are on site and available to assist and Page 8 of 125 coordinate activities as requested and required by either the DHR EOC and/or the OHS-GEMA SOC action officers and/or Emergency Support Function staff. Staff assigned to the OHSGEMA SOC will monitor the virtual EOC management system used in the OHS-GEMA SOC, as well as the WebEOC. The Public Health Districts will notify the DHR EOC of all requests for information (RFI), requests for assistance (RFA), mission taskings, and significant event notifications through the WebEOC. During events requiring activation and staffing of the DHR EOC and the OHSGEMA SOC, there is heightened activity, limiting radio/phone access. It is best to use WebEOC as the primary method of communicating these types of messages. Page 9 of 125 Phase III: RECOVERY/MITIGATION Recovery is the transition to normal operations. Short-term recovery actions are taken to assess damage and return vital life-support systems to minimum operating standards. Long-term recovery may go on for years and involve the development, coordination, and execution of services. Mitigation minimizes the adverse impact of an emergency and reduces vulnerability to future emergencies. Mitigation measures may be implemented at any time. The DPH Exercise Coordinator will conduct monthly and quarterly Call-Downs in order to test the State and District Public Health Staffs’ ability to rapidly respond to a significant event or public health incident. The Call-Down exercise program and schedule is located at Appendix 2 to Support Annex A1. After action reviews will be conducted quarterly to determine the strengths and weaknesses of the alert and notification process. These reviews will help shape this SOP, drive how Call-Downs are conducted, and focus on those areas that need improvement. Page 10 of 125 DEPARTMENT OF HUMAN RESOURCES Division Of Public Health Emergency Operations Plan Responsibilities Of On-Call Representative Standard Operating Plan Support Annex A1, Attachment I As a disclaimer, it is recognized this list is not all inclusive. It serves as a guide of suggested activities of the On-Call Representative. This list is arbitrary and no ranking should be assumed. Be available for the assigned period, unless otherwise stated Be accessible by more than one means of communication devices and have all available devices listed, including unlisted home/cell numbers on SendSS current statewide radio (Southern LINC) will be mass voice notification of choice maintain good battery charge of all communication devices keep all assigned radios on the designated channel If somebody else takes your call, ensure they notify the caller of your current status Caller should then notify an alternate (if necessary) or another key individual (if available). Another key individual could include, but is not limited to: peer staff member or higher emergency responder or manager. As a minimum, maintain easy access to an alert roster of all essential personnel and teams, at the State and District level Have easy access to all essential operations plans and contact numbers of essential partners Notify fellow staff, appropriate PH management team members and DHR Emergency Manager of incidents in a timely manner: includes, but not limited to bomb threats of PH property, evacuation of a PH office for any reason, power outages or computer server crashes, unusual or increase in disease presentations to local hospitals or clinics as related by District staff, any unusual occurrences that may be of PH significance, and powder/suspicious package incidents requiring a law enforcement, HAZMAT, medical, EMA response Limit use of alcohol during On Call period Contact and change On Call status with alternate, notifying appropriate personnel, if you become physically or mentally impaired. Be familiar with the roles and responsibilities of the Emergency Support Function 8 Be familiar with the roles and responsibilities supporting Emergency Support Function 6 Be familiar with the OHS-GEMA Georgia Emergency Operations Plan and how it supports the National Response Plan Be familiar with the DHR Emergency Management Plan and how it supports the Division of Public Health Emergency Operations Plan Be familiar with Division of Public Health Emergency Operations Plan and various Support Annexes, Incident Annexes and Appendices Page 11 of 125 Suggested Responsibilities Of On-Call Emergency Coordinator Support Annex A1, Attachment II As a disclaimer, it is recognized this list is not all inclusive. It serves as a guide of suggested activities of the on-call Emergency Coordinator. The ranking is arbitrary. -ensure contact information is up to date in the SendSS “On Call Calendar” -be available for the stated/assigned 24 hour period, unless otherwise stated -be accessible by more than one means of communication devices and have all available devices listed, including unlisted home/cell numbers ---maintain good battery charge of all communication devices ---keep the SouthernLinc radio on the predesignated channel (determined by your protocol) -if you are on call and have somebody else take your call, make appropriate changes in SendSS “On Call Calendar” and notify all pertinent individuals ---pertinent individuals (minimum) include, but are not limited to: fellow staff, District Health Director, District Administrator, District Epi on call, District PIO, designated OEMS/BT staff member, others as determined by your SOP -as a minimum, maintain easy access to SendSS “On Call Calendar”of all essential personnel and teams, at both the District and State level -have easy access to District SOP and all essential operations plans, including hospital 24 hour points of contacts and numbers, EMA’s, other essential partners -notify appropriate OEMS/BT staff of incidents occurring in your District, in a timely manner: ---includes, but not limited to bomb threats of PH property, evacuation of a PH office for any reason, power outages or computer server crashes, unusual or increase in disease presentations to local hospitals or clinics as determined by the DHD or Epi, any unusual occurrence you were informed of that may be of interest at the state level, powder incidents requiring a law enforcement, HAZMAT, medical, EMA response ---if event does not evolve into a large response or has no untoward outcome, complete an entry on WebEOC, in the “Significant Event” Board. Include type of event, whom contacted and the outcome. ---upon resolution of event or every 24 hours, complete and submit a SITREP/STATUS REPORT to the OEMS/BT Section. Minimal information includes that as found on the distributed SITREP TEMPLATE -limit use of alcohol during on call period ---contact and change on call statue with alternate, notifying appropriate personnel -if taking medications that may alter mental status --- contact and change on call statue with alternate, notifying appropriate personnel -have authority and responsibility to contact senior District personnel -know location of and have authority and responsibility to open Emergency Operations Center and initiate call down of essential personnel (or respond per procedure as outlined in the District SOP) -be familiar with the roles and responsibilities of the Emergency Support Function 8 -be familiar with the roles and responsibilities supporting Emergency Support Function 6 -be familiar with the GEMA Operations Plan and how it supports the National Response Plan Page 12 of 125 -be familiar with the DHR Emergency Management Plan and how it supports the Division of Public Health Emergency Response Plan -be familiar with the District SNS Plan ---maintain authority and responsibility to call down and activate initial personnel for staffing the RSS as soon as a decision is made to do so ---during a heightened alert situation, if the decision is made not to activate the District SNS Plan, review the plan with essential personnel ASAP, in the event you will need to activate the plan --be familiar with the various SOPs and SOGs, including the “Advice for first Responders Dealing with Suspicious Substances”, as found under the PH EOP IA4. Page 13 of 125 ESF8 Response in an Emergency A Public Health Primer Support Annex A1, Attachment III This is not intended to be an all encompassing review of the Public Health Response to Presidentially Declared Disaster. Its primary intent is to familiarize state and District Public Health personnel with the possible response of the state and federal government. The scenario is one that has created or has the potential to create an overwhelming number of casualties or overwhelm the medical resources in a given location. LOCAL AND STATE EMERGENCY: -a situation has occurred in a given location, either creating or has the potential to create a large number of casualties or overwhelm the medical resources -the District Health Director, in consultation with the Local/County Emergency Manager and local hospital(s), determines their resources will either deplete soon or are depleted -the District Health Director requests mutual aid with surrounding District Health Directors -the Public Health mutual aid will not suffice -the District Health Director consults with the Medical Director of the Office of Emergency Preparedness (or representative) - Medical Director of the Office of Emergency Preparedness (or representative) Director of Public Health, updating the situation -based on the information received, the Director of Public Health deploys available unaffected Public Health resources to the affected area STATE RESPONSE: -the Director of the Office of Emergency Preparedness designee contacts and briefs the Department of Human Resources Emergency Management and the Division’s Health Emergency Assistance and Resource Team. If the event is resource intensive (cannot be handled at the work station), the DHR Emergency Operations Center will be opened -the DHR Emergency Management or member of the Office of Emergency Preparedness will contact Georgia Emergency Management Agency, updating of the situation, requesting assistance -a member of the Office of Emergency Preparedness may courtesy call the Health and Human Services Region IV Response Emergency Coordinator -the Director of Public Health and Director of the Office of Emergency Preparedness (or designee), based on consultation with the affected area’s District Health Director and Georgia Emergency Management Agency, will contact the Governor, requesting a Public Health Emergency be declared -the Governor’s Office will consult Georgia Emergency Management Agency, being updated on the situation -based on the information received, the Governor requests a declaration of a Federal Emergency through the Department of Homeland Security Office of Emergency Response/Federal Emergency Management Agency, Washington, DC Page 14 of 125 -based on the information received at the Federal level and from the State authorities, the President does designate a Presidentially Declared Disaster, authorizing the implementation of the National Response Plan, deploying Federal assets to the state and the affected area -Georgia Emergency Management Agency’s State Operations Center is “activated” and the Emergency Support Function representatives and representatives of other vital agencies are contacted to report to the State Operations Center FEDERAL RESPONSE (initial): -the Department of Homeland Security Office of Emergency Response/Federal Emergency Management Agency Regional Operations Center, Federal Emergency Management Agency Region IV, Atlanta, GA is contacted by its Headquarters in Washington, DC and is “activated” -the National Management Response Team, stationed in Thomasville, GA is alerted and all of its equipment and personnel are prepared for deployment to the affected area -the Regional Response Coordination Center is prepared for the arrival of response personnel -response personnel include all of the Emergency Support Functions (1-12), Department of Homeland Security Emergency Coordinators, Federal Department of Defense Regional Emergency Preparedness Liaison Officers, Health and Human Services Region IV Response Emergency Coordinator, Federal Department of Defense US Northern Command’s Joint Regional Medical Planning Officers (upon request of the Regional Emergency Preparedness Liaison Officers and/or the Emergency Coordinators) -response of additional State resources is coordinated through Georgia Emergency Management Agency’s State Operations Center -representatives coordinated the initial Federal response through the State Operations Center, continually assessing the situation and needs FEDERAL RESPONSE (maturing): -in concert with the State Operations Center, a Federal Department of Homeland Security Emergency Response/Federal Emergency Management Agency’s Field Office will be established near the disaster site, becoming the focal point for coordinating the Federal response (near is relative; could be 10’s of miles from the scene) -from the White House, a Federal Coordinating Officer will be appointed, the highest ranking federal official on scene, reporting directly to the President of the United States -all Requests for Information and Requests for Assistance will be assigned a number through the Operations Section -National Management Response Team will be assigned to this location -representatives from the various Emergency Support Functions, including the Federal Department of Homeland Security’s Emergency Coordinators, US Northern Command’s Joint Regional Medical Planning Office, Federal Department of Defense Regional Emergency Preparedness Liaison Officer, and others as requested will be deployed -the Federal Department of Defense deploys a Defense Coordinating Officer with the Defense Coordinating Element to coordinate the Federal and State Department of Defense response. They will closely coordinate with other agencies located at the Field Office. The Defense Coordinating Officer is responsible for ALL State and Federal Department of Defense personnel and equipment deploying the site Page 15 of 125 -as this is occurring, other Federal Agencies and Department of Defense are establishing their respective Emergency Operations Centers -all requests received by the Field Office for medical supplies and personnel, are coordinated by the Department of Homeland Security’s Emergency Coordinators -those requests requiring Department of Defense medical assets, will be coordinated through US Northern Command’s Joint Regional Medical Planners -as the situation unfolds, if it appears it might be a chemical/biological event, US Northern Command may deploy its Joint Task Force-Civil Support command team. The Joint Task forceCivil Support will assist coordinating the deployment of the Federal Department of Defense assists with the Defense Coordinating Element, ensuring the appropriate integration into the response force -the Health and Human Services Region IV Response Emergency Coordinators will coordinate the response and integration into the response theater of Federal medical assets, such as the Disaster Medical Assistance Teams, Disaster Mortuary Operational Response Teams, Veterinary Medical Assistance Teams and other civilian relief teams and/or organizations attempting to assist Mature Response: -for both the State Operations Center and the Federal Field Office, planning for a coordinated drawdown will occur as suggested by the observations of senior staff -this drawdown will occur as it appears the civilians will be capable of handling the situation -it is understood the drawdown may not actually begin for several weeks or even months after their deployment Page 16 of 125 Suggested “go bags” for EOC activation Support Annex A1, Attachment IV The below is a suggested content listing for an unannounced EOC activation. The intent is for the individual to be able to work in a sustained operational environment for up to three days. 1) 2) 3) 4) 5) 6) 7) 8) 9) 10) 11) 12) 13) 14) Sweater/long sleeve shirt/similar item (DHR EOC can be cold) Bottled water/tea/other drinks as desired (not requiring refrigeration) Some snack food (high protein/low fat, as an example) Personal care items, e.g., tooth brush, tooth paste, baby wipes (assist with cleaning if showers not available), deodorant, additional hygiene items Any medications you are taking ID badge Comfortable shoes Cash, small bills/change (snack bar, ordering food, etc). Suggest NMT $50 to start. Change of clothes/underwear/socks for 3 days (suggest comfortable-no dress clothes) Book/magazines/journals to read during down times Sleep wear (sweat clothes, etc) appropriate to sleep in the DHR EOC Conference Room; mixed company Sleeping bag or similar and pillow; suggest rubber mat or similar to sleep on (no cots/bedding provided) Flash light with extra batteries/bulb Appropriate personal and professional communication devices (cell phones, radios, pagers, etc) Page 17 of 125 ESF8 (Public Health) Responsibilities: Emergency Operations Center Support Annex A1, Attachment V This is not meant to be all inclusive, but to provide guidance for those Public Health (PH) personnel who will assigned to the Emergency Support Functions (ESF) 8 desk (Health and Medical Services) in an Emergency Operations Center (EOC). It is understood each District is different, therefore the response has to be modified according to the District and local EMA agreements. Some of the areas listed below are strictly State functions and cannot be accomplished by the District or County. It is up to the District/County to refine this document to reflect their roles and responsibilities. As this is a suggested guide, it may be best utilized as a reference document for a check list. Per the Georgia Department of Human Resources (DHR) DPH Emergency Operations Plan (EOP), PH has both primary and support responsibilities. Their Primary role is the Health and Medical Services and the Secondary role is support of the Mass Care and Shelter process. The three (3) primary areas of responsibility, as described in the Georgia Emergency Operations Plan (GEOP) are: (1) Medical Care: Emergency Medical Services (EMS): may need to assist with simultaneous response of multiple vehicles, specialized medical and dental care (may need to provide at the District clinic or coordinate through the existing or responding medical community); pharmaceutical acquisition and distribution: including, coordinating and distributing medical supplies and personnel, to include licensed health care providers, nurses, medical technicians, equipment, immunizations, hospitals, first aid clinics, facilities, Strategic National Stockpile and other medically related services. Medically related services could include assisting with patient redistribution within a county or PH District or coordinate the redistribution across PH District boundaries; assisting the medical on-scene commander and EOC staff understand the PH implications of the situation; coordinate with other agencies that have a medically related mission. Enforce laws and regulations to protect public health and safety Assist the hospital community with decisions facing potential/actual surge capacity issues; may include redistribution of patients to other facilities or to alternate care settings as established by District/State Public Health Mobilize and coordinate the volunteer public health workforce Be aware of and coordinate the Public Health response in accordance to the appropriate Federal and Georgia Homeland Security Threat Levels Coordinate integration of Regional and Federal response assets into the local response Page 18 of 125 Provide and/or coordinate representation to designated Special Needs Population Shelters and other alternate care facilities. Coordinate public information releases related to health care concerns with the PH PIO and the EOC Information and Planning (ESF5). Coordinate through your EMA, debris removal in/near medical treatment facilities and private property that may create health and safety hazards (obtain as much information as possible, including type of debris, location, how its interfering with operations). Ensure you keep in touch with the medical agency until mission is complete Mobilize and coordinate partners to identify and solve health problems Coordinate Epidemiological response to the incident area, as well as affected citizens and local receiving hospitals. Assist hospital community with infection control questions and issues. Coordinate the Epidemiological response: ensure the appropriate level infectious disease epidemiology and environmental epidemiological investigations are instituted, Coordinate with Epidemiology (District and/or State), Emergency Management, Public Safety and other officials/agencies if it is decided to recommend/institute isolation/quarantine conditions Coordinate transportation of appropriately contained laboratory samples, including environmental samples, body fluid samples and other samples as approved by the Georgia Division of Public Health Laboratory; Need to coordinate and/or inform the DHR Emergency Operations Center of the medical activities and other pertinent activities within the EOC; The District Health Director (DHD) will be kept abreast of all requests and actions, as the ESF8 representative is acting on behalf of the DHD; (2) Environmental Health: Staffing, supplies and equipment essential to: Prevent communicable diseases and contamination of food and water and Develop and monitor health information, inspection and control of sanitation measures, disease vector and epidemic control; Laboratory testing, facility and daily shelter inspections; Assist as requested with private water testing; Assist with potable water testing; Assist with decision making concerning best locations for feeding stations, types of foods to be served and food inspections during a disaster situation Assist Department of Natural Resources and Department of Agriculture with disposal of contaminated animal remains (as requested); Assist GBI with human remains disposal (including contaminated remains guidance); (3) Crisis Counseling, Grief Assistance and Rehabilitation Services: Professional personnel; services and facilities to relieve mental health problems of victims caused or aggravated by an emergency or disaster or the aftermath; and rehabilitation services, including accessibility determinations of shelter facilities. Page 19 of 125 AS A RESOURCE, THE PUBLIC HEALTH FUNCTIONS ARE PROVIDED: In the Georgia Division of Public Health (DPH), the ESF 8 Health and Medical Services representative is responsible to integrate the following into their response (as defined in the Public Health Emergency operations Plan, October 2005: Core Functions: -Assessment of the health of the community -Assurance of necessary services through regulation and provision of these services -Policy development to establish the framework for healthy individuals and communities Essential Functions: -Conducting community diagnosis -Preventing and controlling disease and injury -Ensuring a safe, healthy environment -Measuring performance, effectiveness and outcomes of health services -Promoting healthy lifestyles -Laboratory testing -Providing personal health services -Assuring public health capacity and infrastructure and ensuring rules and Regulations EMERGENCY OPERATIONS CENTER OVERVIEW The ESF 8 representative will establish and operate their Emergency Operations Center (EOC) within the National Incident Management System (NIMS) compliant Incident Command System (ICS) structure that is unique for the incident/event, including Type 1-5. It is beyond the scope of this document to provide an overview of NIMS, therefore, please refer to http://www.fema.gov/emergency/nims/nims_training. Additionally, the various standard and applicable emergency management tools and principles can be further researched at www.training.fema.gov/EMIWeb/IS/crslist.asp (IS 100, 200, 235, 701 and ICS 300 and 400, along with other incident command related units). Within the EOC, the ESF8 representative’s primary duty is to coordinate all health and medical Requests for Information (RFI) and Requests for Action (RFA), keeping the applicable Emergency Management Agency informed. Affected Districts will keep the Division abreast of events. This includes ensuring other appropriate ESFs are included as necessary. An example would be the request for medical supplies. The ESF 8 would work with the requester, determining the actual need, coordinating that request with the DHR EOC; and coordinating the transportation related issues with their local Emergency Management Agency’s Department of Transportation ESF 1 representative. The ESF 8 representative will use all of the available tools at hand, including, but not limited to WebEOC, LiveProcess, SendSS On Call Calendar, GroupWise and other systems that are available. The primary event management tool is WebEOC. Page 20 of 125 A tool providing management of the event is the internet based system, WebEOC. WebEOC is paid for and maintained by the Division of Public Health, maintained by the DHR Office of Information Technology and based on a separate server. The WebEOC manual is located on the website, as well as in the PH EOP Annex A9, “Communications (Equipment, Services, Information Technology). Users are approved by the Division’s Office of Emergency Preparedness that have a direct supporting role with Public Health. The management of the event is expandable and contractable. This is determined by many factors, including, but not limited to the type of event, number of citizens involved, responding agencies and involvement of Public Health (Division and District). Public Health recognizes and will incorporate as needed, the roles of the Command and General Staff. However, it is not imperative to operationalize all segments of either, nor is it imperative to actually open their respective EOC (if manageable off site, i.e, home). An important factor, as stated in the “Public Health Exercise Design and Evaluation Guide” and emails to the Emergency Preparedness staff, document the process of the management of the event through WebEOC. It is the intent of the Office of Emergency Preparedness to not mandate that all of the Command and General Staff functional roles be activated and staffed during an event. However, it is imperative that functional roles be spelled out, including the names of personnel in those positions. As applicable, an After Action Report will be completed after the event. If the event is less than one operational period (generally 12 hours), the notes in the WebEOC “Significant Events Board” are sufficient. If the event exceeds one operational period, a Situation Report (SITREP) will be accomplished (located on WebEOC dash board). Page 21 of 125 DEPARTMENT OF HUMAN RESOURCES DIVISION OF PUBLIC HEALTH EMERGENCY OPERATIONS PLAN: DEPARTMENT OF HUMAN RESOURCES EMERGENCY OPERATIONS CENTER ACTIVATION/DEACTIVATION STANDARD OPERATING PROCEDURE SUPPORT ANNEX A1, ATTACHMENT VI (Primary Location is inSUPPORT ANNEX A14, APPENDIX I, ATTACHMENT II) DHR EOC MACC STRUCTURE, PROPOSED, 16 Nov 07 DHR MACC (DHR EM and PH EP) PIO/RC Liaisons: Affected District, SOC, PHLn Safety Legal OPS EP Coord LOG Pharm PLAN EP Coord Med Intel EP or EPI GHA EH EH VolunteersMRC/ESARVP ORS Epi Epi EMS HCO Surge OTWD OIT Nursing Nursing Augusta Vaccines PHL Epi Chem-Rad SNS SNPS Shelters CISM ARC RSS Team Vital Records EOC Staffing Atlanta NDMS Fin/Admin Admin Coord Communications Officer PODs CHEMPACKS Page 22 of 125 Threat Level Actions (State, Hospital, Public Health): Support Annex A1, Attachment VII Georgia Office of Homeland Security: Threat Levels LOW • Ensure that existing security measures and communications equipment are in place and functioning. • Make sure that contact lists, phone numbers, contingency and business continuity plans are current. • Distribute security awareness bulletins, prepared by GOHS or designee, throughout State agencies. • Report the presence of unknown personnel, unidentified vehicles, vehicles operating out of the ordinary, abandoned parcels or packages, and other suspicious activities. • Assure that all facilities are regularly assessed for vulnerabilities. • Develop procedures for shutting down and evacuating the facility. • Survey surrounding areas to determine activities that might increase potential risks to the facility. GUARDED • Maintain close coordination with GOHS, GEMA, and law enforcement to share information. • Require all employees and visitors to display proper ID while on State property. • Review facility operation plans, security plans and procedures to include bomb threat, chemical, biological or radiological, and evacuation. • Designate employees to make regular sweeps of the facility to look for suspicious items or activities. • Require each visitor to check in and verify his or her identification. • Be familiar with vendors who service the facility and investigate changes in vendor personnel. • Inspect emergency supplies to ensure equipment is in good working order. ELEVATED • Review all appropriate plans with personnel. Review notification/recall lists. • Ensure that vital personnel are informed and on-call. • Prepare specialized units for activation. • Escort all unknown visitors in the facility. • Heighten the mail examination process. • Reduce the number of access points for vehicles and personnel to minimum levels. • Coordinate emergency plans as appropriate with nearby jurisdictions. • Inspect the interior/exterior of buildings for suspicious items at the beginning and end of each workday and at random intervals. • Check all deliveries to facility and loading docks. • Ensure security of vehicles at the facility by locking all vehicles. • Inform GEMA and GOHS Public Information Officer of events as they occur. • Coordinate the release of information with GOHS PIO. HIGH • All employees should remain in close contact with their supervisor for pertinent instructions regarding work activities and scheduling. • Make preparations for changes in tours of duty (extended hours, cancellation of off days and/or leave). • Put all employees on high alert for suspicious persons, items, or activities and instruct them to report any such findings immediately. • Inspect all mail and packages coming into a facility, but do not open suspicious packages (review the USPS "Suspicious Mail Alert" and the "Bombs by Mail" publications with all personnel involved in receiving mail and packages). • Establish Command Center(s). Prepare to execute contingency procedures. • Implement Emergency Operations Plans and form contingency plans in all agencies, as conditions require. • Keep all personnel responsible for implementing antiterrorist plans on call. • Restrict access to all non-public areas of State facilities to properly identified employees and escorted guests. • Curtail certain functions or close State facilities at discretion of the Governor or his designee. • Close and lock gates and barriers except those needed for immediate ingress and egress. Inspect perimeter fences regularly. • Consult with local authorities about control of public roads and accesses that make the building more vulnerable. • Move cars and objects (e.g., crates, trash containers) at least 25 meters from buildings (consider centralized parking). • Take additional precautions at public events and consider alternative venues or cancellations. Page 23 of 125 SEVERE • Release non-essential employees from duty at the discretion of the Governor or designee. • Set all employees on the highest alert for suspicious persons, items or activities. • Increase or redirect personnel to address critical emergency needs. • Assign emergency response personnel; pre-position and mobilize specially trained teams or resources. • Implement emergency and continuity plans as appropriate. • Restrict access and implement positive identification of all personnel; minimize administrative journeys and visits. • Search all suitcases, briefcases, packages, etc. brought into the facility. • Search all vehicles and their contents before allowing entrance to facility. • Cancel or delay all non-vital facility work conducted by contractors, or continuously monitor their work. • Reduce restricted area access points to an operational minimum. • Coordinate the possible closing of public roads and facilities with local authorities. • Coordinate the sharing of media information with Governor’s Office via State PIO. State of Georgia: General Response to Georgia Office of Homeland Security (GOHS) Threat Conditions In some instances, emergency conditions may be declared based on information gathered by State or Federal intelligence agencies, law enforcement activities or Homeland Security. Conditions involving potential terrorist threats require increased vigilance on the part of State employees, supervisors, and law enforcement/security personnel. In order to ensure a systematic, measured response to emergencies or potential emergency conditions for the protection of State of Georgia citizens, employees and State property, a system of “Threat Conditions” has been established to define levels of risk and appropriate levels of response. Each State department/agency head can evaluate agency operations and, at their discretion, establish procedures and responsibilities applicable to each threat level in order to provide for the safety of its employees and the public at large. Purpose: To establish general security procedures and define Threat Condition Levels for the State of Georgia. Policy: The protection of State of Georgia citizens, employees and property is the primary mission of the Georgia Office of Homeland Security. To enhance this mission, Threat Condition definitions and procedures will be used to help determine staffing, deployment and assignment of State and other assets. It will be the responsibility of the Director of Georgia’s Office of Homeland Security to advise the Governor in designating the current Threat Level. Definitions: Threat Condition—Alert level, based on the potential of threat against citizens, employees, and property. Threat Condition Levels—Levels of risk posed against State interests on a scale of normal, or no known risks, to an actual terrorist or large impact criminal event. Threat Condition GREEN—No known threat against State interests exists. Only normal, everyday security precautions are to be in effect. Threat Condition BLUE—A general risk or threat of possible terrorist or large impact criminal activity (riot, civil unrest, major demonstrations, local or national emergency) against State interests exists, though the nature and extent do not warrant actions Page 24 of 125 beyond normal liaison notifications or placing assets or resources on a heightened alert (agencies are operating under normal day-to-day conditions). Threat Condition YELLOW—Intelligence or an articulated threat indicates a potential for a terrorist incident or large-scale criminal act. However, this threat has not yet been assessed as credible. Threat Condition ORANGE—An attack or incident has not taken place on State or Nation, but a threat assessment indicates that the potential threat is credible, and confirms the involvement of a high risk of terrorist attack or large impact criminal action. Threat Condition RED—This is the highest level of threat condition. An attack or incident has occurred or is in progress against State and/or national interests. This requires implementation of an immediate process already in place to identify, acquire, and plan the use of State resources to augment state and local authorities in response to limited or major consequences of terrorist use of or employment of Weapons of Mass Destruction (WMD). It is anticipated that actions listed under this threat level will be initiated and sustained for a relatively short period of time, based on guidance from federal and state governments, due to significant personnel and economic considerations. General Security Measures: Each employee must aid in the effort to maintain proper security. To increase the security consciousness of the entire organization, it is important for administrators to share security information with their staffs. The purpose is to help employees recognize and appropriately report unusual activity. 1. Familiarize employees with existing security procedures and emergency numbers for appropriate local law enforcement agencies. 2. Familiarize employees with the locations of and activation procedures for emergency and fire alarm systems. 3. Instruct employees that when every small area is secure, the entire facility is secure. All security deficiencies or hazards that are reported will be checked and corrected. 4. All employees are to be alert to strangers loitering or lingering in or around the premises and to suspicious vehicles parked near the building. In such situations, the employee will document a description of any person(s) observed and/or the license plate(s), color and make of the vehicle and any other points that could be significant. Information should be immediately reported to security or supervision. 5. Familiarize all employees with the facility’s routine operational procedures relating to deliveries, vendors, frequent visitors, new hires, terminations, and changes in workspace or common areas. 6. Review evacuation procedures included in employee orientation packages periodically. Hold drills periodically. 7. Assign staff members to regularly check specific areas. Close and lock desks and door locks. Note and report inoperable, damaged, or inadequate hardware to the proper supervisor. 8. Appoint, train, and equip a supervisor or mid-management person to function as the building security coordinator. 9. Establish a building-wide alert system to inform all employees in the event of an emergency. Page 25 of 125 10. Institute a positive identification process and access control system. 11. Establish a mail/package inspection procedure. 12. Unnecessary information about the facility or fellow employees will not be given out. Report anything questionable to supervisors or security, including: • Threats or harassment • Persons who ask unusual questions or show unnatural interest in the organization or an employee, such as building layout or design, security measures, staffing, or institutional procedures, or anyone tampering with building equipment or fixtures • Any deviation in delivery procedures • Unattended packages 13. Develop and distribute lists to appropriate personnel of names and telephone numbers of management and key personnel to contact in an emergency. Review and update such lists and procedures periodically. 14. Georgia’s Office of Homeland Security (GOHS) will ensure that all steps are taken to successfully mitigate and respond to the incident or attack, and the Georgia Emergency Management Agency (GEMA) will ensure recovery operations are initiated at the earliest opportunity. Procedures and Responsibilities-Elevated Threat Levels: � Threat Condition Green Personnel 1. Ensure that personnel receive proper training on the Homeland Security Advisory System and specific pre-planned department or agency protective measures. 2. Develop terrorist and security awareness; provide information and educate employees on security standards and procedures. Caution employees not to talk with outsiders concerning their facility or related issues. 3. Establish contact information for state and local public safety, and public health officials. 4. Distribute security awareness bulletins prepared by GOHS or designee, and upon discretion of the Director of GOHS, distribute throughout the State agencies. 5. Advise all personnel to report the presence of unknown personnel, unidentified vehicles, vehicles operated out of the ordinary, abandoned parcels or packages, and other suspicious activities. Facilities/Equipment 1. Develop a process assuring that all facilities are regularly assessed for vulnerability to terrorist attacks and all reasonable measures are taken to mitigate those vulnerabilities. 2. Ensure existing security measures are in place and functioning, such as fencing, locks, camera surveillance, intruder alarms, and lighting. 3. Develop and implement hardware, software, and communications security for computer-based operational systems. 4. Ensure contingency and business continuity plans are current and include a response to terrorist threats. 5. Require all contractors and visitors to check in and out of designated facilities or areas that are considered key command, control, or communications centers. Page 26 of 125 6. Develop procedures for shutting down and evacuating the facility. Vigilant security measures will be observed for facilities located near critical community assets. 7. Survey surrounding areas to determine activities that may increase security risks for the facility, e.g., airports, government buildings, industrial facilities, pipelines, etc. � Threat Condition BLUE- Includes procedures in Threat GREEN plus: Personnel 1. Management will maintain a close local liaison with operational and intelligence units of State law enforcement. 2. Sustain close coordination with GOHS and GEMA to share information 3. Alert all State Agency Communications personnel of heightened alert status. 4. Require all employees and visitors to display proper ID while on State property. 5. Review facility security plans and procedures including bomb threat, chemical, biological or radiological threat, and evacuation procedures. 6. Review personnel details, logistics requirements, and all operations plans including emergency operations plans and business continuity plans that pertain to implementing a change in Threat levels. 7. Remind all personnel, at regular intervals, to be suspicious and inquisitive about strangers, particularly those carrying suitcases or other containers. 8. Be especially alert to repeat visitors or outsiders with no apparent business at the facility that are seeking information about the facility or related issues including personnel. Facilities/Equipment 1. Designate employees to make regular sweeps of the facilities for suspicious items or activities. 2. Watch for unidentified vehicles in or near the facilities. Watch for unusual activity, abandoned parcels, or suitcases. 3. Increase checks of vent and fan rooms, emergency exits, and electrical and control room doors. 4. Inspect perimeter fencing routinely and repair all fence breakdowns. Review all outstanding maintenance and capital project work that might affect security of facilities. 5. Require each visitor to check in at designated facilities or areas that are considered key command and control or communications centers, and verify their identification. 6. Be familiar with vendors and packages. Investigate changes in vendor personnel. 7. Inspect emergency supplies, and ensure emergency equipment is in good working order. 8. Inspect all CCTV/Video Camera/VCR equipment and intercom systems to ensure equipment is operational. � Threat Condition YELLOW-Includes procedures in Threat BLUE plus: Personnel 1. Review with all facility employees the operation plans, personnel safety, security details, and logistics requirements that pertain to implementing increased security Page 27 of 125 levels. Review notification/recall lists. Reinforce awareness of responsibilities with employees. 2. Inform all agency employees with an operational need to know of the specifics of the increased threat. 3. Make staff aware of the general situation in order to prevent unnecessary alarm and stop rumors. 4. Ensure that personnel with access to building plans and area evacuation plans be available at all times. Personnel will be capable of sealing off an area immediately. 5. Keep key personnel on call that are involved in implementing contingency plans. 6. Prepare specialized units for activation. 7. Limit visitor access to key security areas and confirm that the visitor has a need to be there and is expected. All unknown visitors will be escorted. 8. Interface with vendors and contractors to heighten awareness and report suspicious activity. 9. Coordinate emergency plans as appropriate with nearby jurisdictions. 10. Confirm availability of security resources that may assist 24/7 coverage. 11. Examine mail (above the regular examination process) for letter or parcel bombs. 12. At the discretion of the GEMA Director, GEMA State Operations Center (SOC) may increase activation of normal 24-hour operation. State agencies and other organizations may be asked to provide a liaison to the SOC. Facilities/Equipment 1. Reduce the number of access points for vehicles and personnel to minimum levels. Be alert to vehicles parked for an unusual length of time in or near a facility. 2. Periodically spot check vehicles and persons entering facilities. 3. Secure and regularly inspect all interior and exterior buildings and storage areas at frequent intervals. 4. Check designated unmanned and remote sites at more frequent intervals for signs of unauthorized entry, suspicious packages, or unusual activities. 5. Interface with vendors and contractors to heighten awareness and report suspicious activity. 6. Check to ensure all emergency telephone, radio, intercom, television, and satellite communication devices are in place and are operational. 7. Ensure all personal, company, and contractor vehicles at the facilities are secured by locking the vehicles. Media 1. Monitor national and local events and keep GEMA and GOHS Public Information Officer (PIO) informed of events as they occur. 2. Coordinate the release of information with GOHS PIO. � Threat Condition ORANGE- Includes procedures in Threat YELLOW plus: Personnel 1. Instruct all employees to remain in close contact with their supervisor for pertinent instructions regarding work activities and scheduling. 2. Make preparations for possible extended tours of duty, cancellation of off days and or/leave. 3. Prepare to release non-essential employees from duty at the discretion of the Page 28 of 125 Governor or his designee. 4. Curtail or suspend certain services at the discretion of the Governor or his designee. 5. Put all employees on high alert for suspicious persons, items, or activities and instruct them to immediately report any findings to law enforcement or supervision. 6. Inspect all mail and packages coming into the facility. Do not open suspicious packages. Review the US Postal Service’s "Suspicious Mail Alert" and the "Bombs by Mail" publications with all appropriate personnel. 7. Review procedures and make necessary preparations to establish Command Center(s) where applicable. Dispatch Mobile Command Centers in an actual emergency, and initiate an incident command system or similar incident management structure for organizing emergency responses. Prepare to execute contingency procedures, such as moving to an alternate site or dispersing the workforce. 8. Implement Emergency Operations and contingency plans in all agencies, as conditions require. 9. Keep all personnel responsible for implementing contingency plans on call. 10. Restrict access of all non-public areas of State facilities to properly identified employees and escorted guests. 11. Limit access of designated facilities to personnel with a legitimate and verifiable need to enter. Implement positive identification of all personnel with no exceptions. 12. Physically inspect visitors and inspect their suitcases, parcels, and other containers. Facilities/Equipment 1. Curtail certain functions or close State facilities at the discretion of the Governor or his designee. 2. Close and lock gates and barriers except those needed for immediate ingress and egress. Reduce facility access points to the absolute minimum necessary for continued operation. Restrict threatened facility access to essential personnel only. Inspect perimeter fences on a regular basis. � Threat Condition ORANGE (continued) 3. Strictly enforce control of entry. Inspect all vehicles entering key areas/facilities including the vehicle's cargo areas, undercarriage, glove boxes, and other areas where dangerous items might be concealed. 4. Erect barriers and obstacles to control direction of traffic flow and protect key areas from an attack by a parked or moving vehicle. Implement centralized parking and shuttle bus service where feasible. 5. Identify the owner of all vehicles parked at key command, control, or communications areas or other critical areas/facilities and have all unidentified vehicles removed. 6. Move cars and objects (e.g., crates, trash containers) at least 25 meters from buildings—particularly highly populated, mission-related, or high profile buildings. Identify areas where explosive devices could be hidden. 7. Consult with local authorities about control of public roads and accesses that might make the building more vulnerable to terrorist attack if they remain open. Take Page 29 of 125 additional precautions at public events and consider alternative venues or cancellation. 8. Check all security systems routinely to ensure they are functioning properly. Install additional, temporary lighting if necessary. 9. Disable all baggage lockers where applicable. 10. Implement frequent inspection of key areas or facilities including the exterior and roof of all buildings and parking areas. Increase patrolling and ensure all vulnerable critical points are fully illuminated and secure. � Threat Condition RED- Includes procedures in Threat ORANGE plus: Personnel 1. Release non-essential employees from duty at the discretion of the Governor or designee. 2. Put all employees on the highest alert for suspicious persons, items or activities and instruct them to immediately report findings to law enforcement/supervision. 3. Instruct all employees to remain in close contact with their supervision for pertinent instructions regarding work activities and scheduling. 4. Increase or redirect personnel to address critical emergency needs. 5. Assign emergency response personnel, and pre-position and mobilize specially trained teams or resources. 6. Implement emergency and continuity plans as appropriate. 7. Restrict access and implement positive identification of all personnel. 8. Minimize all administrative journeys and visits. 9. Search all suitcases, briefcases, packages, etc., brought into the facility. 10. Recognize that an incident of this type will affect the duty performance of employees and prepare to handle signs of fear, anxiety, and apprehension with compassion and discretion. Utilize professionals to assist as needed. Management must ensure that business continuity measures are being adequately employed. Facilities/Equipment 1. Curtail services and close facilities at the discretion of the Governor. 2. Reduce restricted area access points to an operational minimum. 3. Search all vehicles and their contents before allowing entrance to facilities. 4. Check building exteriors and parking areas frequently. 5. Cancel or delay all non-vital facility work conducted by contractors, or monitor their work continuously with facility personnel. 6. Coordinate the possible closing of public roads and facilities with local authorities. Media 1. Coordinate the release of information with Governor’s Office/State PIO. April 17, 2003 Page 30 of 125 State of Georgia Homeland Security Threat Hospital Alert System Recommended Actions Level GREEN Emergency Department Provide training or refresher courses for all hospital staff on threat colorcoding system. Review implications, roles and responsibilities for each individual and each department. Perform monthly assessment/ inventory of decontamination area/supplies/ personal protection equipment (PPE). Be alert for trends in patient symptoms. Ensure telephone numbers for local and state health departments AND resource hospital are readily available and current. Maintain in-house calling tree. Develop staffing modification plans, including rest cycles and Laboratory Pharmacy Identify level capabilities of laboratory (Level A, B, C, or D) Maintain calling tree. Maintain calling tree. Maintain calling tree. Develop staffing modification plans, including rest cycles and provision of family member care. Develop staffing modification plans, including rest cycles and provision of family member care. Develop staffing modification plans, including rest cycles and provision of family member care. Develop and maintain plans for assisting with community pharmacy support requirements. Continue common sense practices in daily security routines. Arrange for contracted laboratory to provide specimen testing beyond facility capabilities. Arrange for transport of specimens and for education of transporters on safe transport of specimens. Maintain calling tree. Develop staffing modification plans, including rest cycles and provision for family member care. Be alert for trends in culture/test ordering. Identify appropriate personnel for notification. Report concerns to appropriate personnel. Page 31 of 125 Public Safety Security Report suspicious circumstances and/or individuals to appropriate person (director of public safety/law enforcement). Administration Review hospital, local community, and state disaster plans. Have public relations or public safety staff monitor news information stations for change in Threat Con. Have a "basic" unified public information (PI) message available to in an "all – hazards" form. Provide Public Information seminars to key personnel within the institution. provision for family member care. Perform and document weekly radio checks. BLUE Continue all measures outlined in GREEN Threat Alert. Continue all measures outlined in GREEN Threat Alert. Continue all measures outlined in GREEN Threat Alert. Continue all measures outlined in GREEN Threat Alert. Alert staff in all departments (Administration, Laboratory, Pharmacy, Public Safety/Security, Nursing Directors, EMS Coordinator, Infection Control) to heightened Threat Con. Alert appropriate staff concerning the heightened Threat Alert. Alert appropriate staff to heightened Threat Alert. Alert appropriate staff to heightened Threat Alert. Alert appropriate staff, including medical staff, to heightened Threat Alert. Review disaster preparedness protocols specific to department. Review disaster preparedness protocols specific to department. Review disaster preparedness protocols specific to department. Review disaster preparedness protocols specific to department. Ensure that the laboratory is secure. Ensure that pharmacy is secure. Ensure that the department is secure. Review call tree and staff modification plan. Review call tree and staff modification plan. Implement security plans appropriate to the facility (e.g., monitoring of entrances/exits, including those in professional office buildings). Be alert for trends in patient culture/testing patterns. Inform appropriate personnel if suspicious patterns noted. Inventory antidotes/ medications levels. Note expiration dates. Include information in shift reports. Review disaster preparedness protocols for department. Review calling tree and staff modification plan. Assign staff person to watch for faxes/E-mails/ correspondence from GDPH, the GHA, the Health District and the Health Alert Network (HAN). Check all equipment for operational readiness. Prohibit casual access by unauthorized personnel. Ensure all vehicles are secured. Check all communications equipment for operational readiness. Inventory emergency disaster medical bags. Check expiration dates Be alert for suspicious activity and report it to the appropriate Page 32 of 125 Continue all measures outlined in GREEN Threat Alert. Review call tree and staff modification plan. Check all communication equipment for operational readiness. Test group page capabilities with Threat Alert status. Have public relations and public safety/security staff monitor news information stations (CNN, FOX, MSNBC) for change in Threat Alert. Refresh key personnel on media and completeness of bags. persons (director of public safety, law enforcement). Check that all disaster related paper work is available. Duplicate as necessary protocols. Provide media training for all key personnel (e.g., ED physicians, charge nurses, EMS coordinator, nursing supervisor). Conduct tabletop exercises for key personnel. Assess communications readiness (telemetry radios, walkie-talkies and other redundant communication systems). Inventory decontamination area supplies and equipment, including PPE. Be alert for trends in patient symptoms. YELLOW Continue all measures outlined in Green and Blue Threat Alert. Alert staff in all departments (Administration, Laboratory, Pharmacy, Public Safety, Nursing Directors, EMS Coordinator, Infection Control) to heightened Threat Alert. Assign staff person to watch for faxes/E-mails/ correspondence from GDPH, the GHA, the Health District and the Continue all measures outlined in Green and Blue and Threat Alert. Continue all measures outlined in Green and Blue Threat Alert. Continue all measures outlined in Green and Blue Threat Alert. Ensure that all staff is alerted to the heightened Threat Alert. Ensure that all staff is alerted to the heightened Threat Alert. Ensure that all staff is alerted to the heightened Threat Alert. Review emergency plans for this alert level with all shifts. Review emergency plans for this alert level with all shifts. Review emergency plans for this alert level with all shifts. Ensure security of laboratory. Ensure security of pharmacy. Ensure call tree is available and current. Ensure call tree is available and current. Consider Consider Remind all hospital staff to be suspicious and inquisitive and to maintain heightened awareness of people, vehicles Page 33 of 125 Continue all measures outlined in Green and Blue Threat Alert. Ensure that all staff is alerted to the heightened Threat Alert. Review emergency plans for this alert level with all shifts. Ensure security of department. Ensure call tree is available and current. Consider alternative work schedules to Health Alert Network (HAN). Ensure security of emergency department. Ensure call tree is available and current. alternative work schedules to implement for operational staff if threat alert escalates. Check all equipment for operational readiness. Consider alternative work schedules to implement for staff if threat alert escalates. Check inventory of critical supplies; reorder if necessary. Perform and document radio tests daily. Be alert for suspicious activities and report to appropriate person. Perform and document telemetry radio tests (if applicable) daily. alternative work schedules to implement for operational staff if threat alert escalates. Check inventory of critical antidotes/ medications; reorder if necessary. and activities. Ensure call tree is available and current. Consider alternative work schedules to implement for operational staff if threat alert escalates. Increase spot checks of specific high-risk entrances/exits (e.g., loading docks, professional office buildings). Document security checks. Do not leave vehicles unattended and unlocked. Monitor diversion incidents within EMS region. Move vehicles and objects (trash containers, etc.) away from the building. Review hospital and state disaster plans with all shifts. Lock and regularly inspect all buildings, rooms and storage areas not in regular use. Inventory available internal resources (beds, pharmacy stock, laboratory supplies, ancillary services) daily. At the beginning and end of each shift, as well as at other regular and frequent intervals, inspect the interior and exterior of buildings for suspicious packages or Perform disaster call tree drill, including threat alert in call. Review disaster related paperwork. Page 34 of 125 implement for operational staff if threat alert escalates. Review hospital, local community and state disaster plans. Review incident command structure and command center operations. Ensure communications equipment and information, including telephone numbers of governmental agencies, is available and operational. Instruct telecommunications staff to complete a group page with color alert system and document response times. Inventory available internal resources (beds, pharmacy supplies, laboratory capabilities, ancillary services). Evaluate elective admissions and determine need to cancel elective admissions. Review media protocols and have public relations staff monitor news information stations continuously for change in Threat Con. Be aware of large-scale Ensure it is readily accessible. activities. Be alert for suspicious activities and report to appropriate person. Consult with law enforcement officials/emergency medicine/GDPH on message to be disseminated. Ensure that all key personnel have same message (cue cards, talking points, etc.). Ensure decontamination area is operational. Assign person on each shift to be media representative. Ensure that the emergency medical disaster bags are readily available. ORANGE Continue all measures as outlined in Green, Blue and Yellow Threat Alerts. At each shift change alert staff in all departments (Administration, Laboratory, Pharmacy, Public Safety, Nursing Directors, EMS Coordinator, Infection Control) to heightened Threat Alert. Assign staff person to watch for faxes/E-mails/ correspondence from GDPH, the GHA, the Health District and the Health Alert and share with each on-coming shift supervisor. Ready decontamination community events (sporting events, concerts, etc.). Continue all measures as outlined in Green, Blue and Yellow Threat Alerts. Continue all measures as outlined in Green, Blue and Yellow Threat Alerts. Ensure that all staff is alerted to heightened Threat Alert. Ensure that all staff is alerted to heightened Threat Alert. Ensure security of laboratory. Ensure security of pharmacy. Activate call tree; place staff on alert status. Activate call tree; place staff on alert status. Advise staff of shift modifications if threat escalates. Advise staff of shift modifications if threat escalates. Ensure that PPE and specialized response equipment and supplies are checked and readily available. Check inventory of critical antidotes/ medications; reorder if necessary. Page 35 of 125 Continue all measures as outlined in Green, Blue and Yellow Threat Alerts. Continue all measures as outlined in Green, Blue and Yellow Threat Alerts. Ensure that all staff is alerted to heightened Threat Alert. Ensure that all staff is alerted to heightened Threat Alert. Activate call tree; place staff on alert status. Ensure security of department. Advise staff of shift modifications if threat escalates. At the beginning and end of each shift, as well as at other regular and frequent intervals, inspect the interior and exterior of buildings for suspicious packages. Consider activation of facility disaster preparedness plan. Have Incident Command sheets available Assess readiness of the command center Activate call tree; place staff on alert status. Advise staff of shift modifications if area equipment and supplies. Ensure PPE is available for all staff. Inventory categories on disaster form (bed/ blood availability, availability of medical teams/bags). Audit internal resource availability (e.g., beds/monitored beds, blood supply, antibiotic/IV supply, ventilator supply, linen supply, food/water supply). Check inventory of critical supplies; reorder as necessary. Be alert for trends in patient testing. Notify appropriate person if trends noted. Check all equipment for operational readiness. Limit access points to the absolute minimum and strictly enforce entry control procedures. Enforce parking of vehicles away from main hospital buildings. Identify and protect all designated vulnerable points. If unavailable to perform certain tests, contact contracted laboratories. Ensure security of emergency department. Activate call tree; place staff on alert status. Advise staff of shift modifications if threat escalates. Check equipment and supplies at patient care/treatment locations as outlined in facility internal disaster plan (professional office buildings, outpatient departments, etc.). Page 36 of 125 threat escalates. Check all telecommunications equipment for operational readiness. Review transfer agreements in anticipation of patient transfer to other appropriate facilities. Lock all exterior doors except the main facility entrance(s). Have public relations staff monitor news information stations (MSNBC, CNN) continuously for change in Threat Alert. Check identification of all visitors. Require a sign-in log with information from each visitor's identification. Inform private providers of the Threat Alert for possible rapid evacuation of patients to other facilities. Increase defensive perimeters around key structures. Test all internal communications and warning systems. Alert CFO to begin collecting expense data (personnel, equipment, supplies, transfer costs) related to Threat Alert. Be alert for trends in patient symptoms. Notify appropriate person if trends noted. Be alert for increase in ambulance transport times. Check inventory of critical supplies; restock if necessary. RED Continue all measures as outlined in Green, Blue, Yellow and Orange Threat Alerts. Alert staff in all departments (Administration, Laboratory, Pharmacy, Public Safety, Nursing Directors, EMS Coordinator, Infection Control) to heightened Threat Alert. At each shift change report current status of each department. Ensure emergency department is secure. Activate full ED command center if applicable. Assign staff person to watch for faxes/E-mails/ correspondence from GDPH, the GHA, the Health District and the Continue all measures as outlined in Green, Blue, Yellow and Orange Threat Alerts. Continue all measures as outlined in Green, Blue, Yellow and Orange Threat Alerts. Ensure that all staff is alerted to the heightened Threat Alert. Ensure that all staff is alerted to the heightened Threat Alert. Ensure laboratory is secure. Ensure pharmacy is secure. Activate call tree. Secure as many additional staff as necessary. Advise staff of schedule modifications. Activate call tree. Secure as many additional staff as necessary. Advise staff of schedule modifications. Maintain communication with hospital command post. Maintain communication with hospital command post. Ensure critical supplies are available. Ensure critical antidotes/ medications are available for staff and patients. Ensure that PPE and specialized response equipment and supplies are Page 37 of 125 Continue all measures as outlined in Green, Blue, Yellow and Orange Threat Alerts. Continue all measures as outlined in Green, Blue, Yellow and Orange Threat Alerts. Ensure that all staff is alerted to the heightened Threat Alert. Ensure that all staff is alerted to the heightened Threat Alert. Implement parking restrictions and park vehicles away from facility. Activate facility disaster preparedness plan. Place traffic and pedestrian barriers in place. Put up signage indicating patient treatment areas, information area, family area, etc. Control access and implement positive identification of all persons - no exceptions. Search all suitcases, brief cases, packages, etc., brought into Open the hospital incident command center. Ensure department is secure. Activate call tree. Secure as many additional staff as necessary. Advise staff of schedule modifications. Have public relations staff monitor news information stations (FOX, MSNBC, CNN) for change in Health Alert and share with each on-coming shift supervisor. Activate call tree. Secure as many additional staff as necessary. Advise staff of schedule modifications. Maintain communication with hospital command post. available. the facility. Threat Alert. Check all equipment for operational readiness. Secure all doors. Maintain a security presence at a single point of access to each building and check identification of all visitors. Maintain a sign-in log. Check all bags, suitcases, brief cases and packages at the security point. Provide for day care/child care facilities for staff responding to Threat Alert Red. Alert any contracted labs of Threat Alert Red and the possibility that specimens may be sent to them. Increase defensive perimeters around facility. Make frequent checks of the exterior. Deliveries should not be accepted unless approved by supervisory staff. All deliveries are to be opened outside the facility and minimal numbers of personnel should be in the immediate area when deliveries are opened. Maintain communication with support hospitals. Have disaster paperwork in order. Assure availability of the SNS request forms. Activate decontamination area, including supplies and PPE. Screen all arrivals for possible contaminants. Contact Resource hospital in EMS region for additional instructions and/or information. Have medical bags ready for deployment. Page 38 of 125 Arrange for food service to provide meals to staff. Alert CFO to begin collecting expense data (personnel, equipment, supplies, transfer costs) related to Threat Con Alert. GEORGIA HOMELAND SECURITY ADVISORY SYSTEM THREAT LEVELS & RECOMMENDED PUBLIC HEALTH ACTIONS RED Severe risk of terrorist attacks. DHR Emergency Response Center (ERC) may be activated. Individual hospital emergency operation centers and Public Health District emergency operations centers may be activated. In addition to the previously outlined protective measures, the following steps may be taken: Establish functions according to internal operating procedures, responding appropriately for the current threat information. Convene emergency response personnel at each DPH location - conduct situation briefing. Poll hospitals to assess capabilities and resource availability. Poll District and DPH facilities to assess capabilities and resource availability. Coordinate health-related activities with other local, state, and federal public and private response agencies/groups. Increase or redirect personnel to address critical emergency needs. Review the authorities of the State and District Health Officer and advise accordingly. Begin active epidemiology activities as appropriate. Review available threat information and assess impact upon daily activities to determine employee protection activities in response to possible attack. Director DPH will determine and implement limitation of non-critical programs as appropriate. Initiate activities to provide for needs of essential staff in order to maintain critical staffing levels. Page 39 of 125 ORANGE High risk of terrorist attacks. This condition may or may not activate the DHR Emergency Response Center (ERC), depending on the state and local assessments. In addition to the previously outlined protective measures, the following steps may and taken: Implement, as appropriate, DHR contingency and emergency response plans Coordinate security efforts with Georgia Homeland Security. Collaborate with other public and private healthcare provider state level representatives. Inform Districts of threat level increase. Use all available means to alert hospitals of threat level increase. Alert emergency response and special communications teams. Coordinate response efforts with districts, CDC, and PHS Emergency Coordinators, and MMRS. Evaluate availability of alternate sites, multi-agencies/jurisdiction as needed. Restrict access to allow essential and authorized personnel only. Review and ensure the implementation of security measures for mission critical assets. Ensure service and supplies procurement procedures and vendor lists are current for continuity of service and emergency operations needs Review appropriate security and emergency preparedness policies and procedures. Assist in establishing public health surveillance for potential toxic exposures following an emergency/disaster situation. Review operations for general or mass emergency immunizations/pharmaceuticals or quarantine/isolation procedures. Page 40 of 125 YELLOW Significant risk of terrorist attacks. This condition may or may not call for the activation of the DHR Emergency Response Center (ERC), depending on the state and local assessment. In addition to the previously outlined protective measures, the following steps may be taken: Review emergency/contingency plans for DPH. Review/update emergency contact directory and personnel notification procedures. Assess further enhancement of preventive, protective measures, and efforts to ameliorate public concern within the context of the current threat information. Increase human/veterinary/ environmental epidemiological surveillance at critical locations. This includes surveillance and epidemiological issues related to toxic exposures. Review laboratory services for confirmatory testing for possible agents and ensure that alternate facilities are identified and available. BLUE General risk of terrorist attacks. DHR Emergency Response Center (ERC) activation level is inactive. In addition to the previously outlined protective measures in GREEN, the following steps may be taken: Check communications with designated emergency response personnel, including the Public Health facilities. Review and update emergency/disaster assessment response/recovery procedures. In association with the Georgia Homeland Security Taskforce, provide the public with appropriate information, via the DHR Communication Office, Public Health's Web site, and other appropriate vehicles. Increase training of response personnel and other private healthcare facilities within the context of the current threat information. GREEN Low risk of terrorist attacks. DHR Emergency Operations Center (ERC) activation level is inactive. The following protective measures may be applied: Refine and exercise planned preventive and protective measures pertaining to chemical, biological, radiological, nuclear, and explosive incidents. Page 41 of 125 Ensure personnel receive training about the Homeland Security Advisory System, DPH and departmental preventive and protective measures. Assess Hospital community, Emergency Medical Services providers, and Public Health's infrastructure vulnerabilities and adopt measures to mitigate accordingly. Ensure policies and procedures are in place to provide for needs of essential personnel during crisis situations, to enhance maintenance of critical staffing levels when required. Page 42 of 125 DEPARTMENT OF HUMAN RESOURCES Division of Public Health Emergency Operations Plan: 1-866-PUB-HLTH Standard Operating Plan Support Annex A1, Appendix 1 (As an Epi Primary Document, this document stands alone in Support Annex A 10, Appendix 1) I. INTRODUCTION This Standard Operating Plan provides guidance regarding the use of the statewide public health emergency hotline 1-866-PUB-HLTH (1-866-782-4584) for the alert and notification of the Georgia Division of Public Health (DPH) Emergency Preparedness Coordinators (EC) at the State and District levels. 1-866-PUB-HLTH operates under the legal authority of OCGA §31-12-2, which requires notifiable disease reporting, including those diseases that may result from “bioterrorism, epidemic or pandemic disease, or novel and highly fatal infectious agents or toxins and that may pose a substantial risk of a public health emergency”. OCGA §31-12-2 also requires DPH to report “any case of an unusual illness, health condition, or death, or an unusual cluster of such events, or any other suspicious health related event that it reasonably believes has the potential to be caused by bioterrorism” to the Department of Public Safety including state and federal partners. II. PURPOSE The purpose of 1-866-PUB-HLTH is to allow time-sensitive communication among DPH personnel at the State and District levels, as well as among healthcare providers and emergency response partners at all levels of government. 1-866-PUB-HLTH is for the reporting of immediately notifiable diseases, including those that could result from a bioterrorism event, and public health emergencies. 1-866-PUB-HLTH is one easy-to-remember number that should be distributed to all local, state, and federal partners for use in a public health emergency. III. SITUATION AND ASSUMPTIONS 1-866-PUB-HLTH is housed at the Georgia Poison Center (GPC) and staffed by Public Health Specialists (PHS) who respond to calls according to protocols developed by DPH. Calls to 1866-PUB-HLTH are made by local, state, and federal emergency responders as well as healthcare providers, laboratorians, coroners, medical examiners, and other partners. Calls are triaged by the PHS according to DPH protocols, and those that require immediate notification of public health are passed to the On-Call Representative (OCR) at the District level for response. If state or federal assistance is needed, the District OCR responds as stated in the Emergency Preparedness Coordinator Alert and Notification SOP. Page 43 of 125 IV. ROLES AND RESPONSIBILITIES It is the responsibility of DPH to provide GPC with the training and resources necessary to make decisions regarding triage of incoming 1-866-PUB-HLTH calls. It is the responsibility of GPC to staff the hotline with trained PHS 24 hours a day, 7 days a week. It is the responsibility of PHS to follow established protocols regarding triage of incoming 1-866-PUB-HLTH calls. The role of the District OCR is to serve as a first responder to a call from 1-866-PUB-HLTH. The responsibilities of responding to a 1-866-PUB-HLTH call are the same as responding to any other type of notification and are as stated in the Emergency Preparedness Coordinator Alert and Notification SOP. The District OCR should be aware of its Public Health and non-Public Health capabilities and resources, as related to the primary role of Emergency Support Function 8 and support of Emergency Support Function 6. It is the responsibility of the District OCR to contact and coordinate response activities with other available District resources. As this coordination is occurring, the District OCR will notify the Division OCR, briefing that individual on the situation, including potential requirements. The District EC Calendar Administrator is responsible for ensuring that the EC Calendar in SendSS is up to date with current OCR contact information. The Division OCR is the conduit to State level resources, including DHR, DPH and GEMA. The Division EC is the conduit to regional/federal resources, including various out of state resources, Disaster Medical Assistant Teams (DMAT), Disaster Mortuary Operational Response Teams (DMORT), Strategic National Stockpile (SNS) resources, Assistant Secretary of Preparedness and Response (ASPR) resources, to name a few. Therefore, the District OCR will contact the Division OCR for assistance requesting any out of District resources not previously covered under an MOU or MOA. V. CONCEPT OF OPERATIONS 1-866-PUB-HLTH is available 24 hours a day, 7 days a week for use by public health partners in the reporting of notifiable diseases and public health emergencies. A public health partner will use the hotline to report an event of public health significance. A PHS at the GPC will answer the call, record basic event information, and respond according to established protocols (see Attachment I). If the event is of immediate importance, the PHS will call the District OCR. The District OCR will call the initial reporter and gather additional information needed for response. The District OCR will respond to the situation as stated in Roles and Responsibilities. The District OCR will contact the Division OCR as needed to brief the Division on the event and to request state resources as needed. Page 44 of 125 VI. ADMINISTRATION AND LOGISTICS 1-866-PUB-HLTH is administered by the DPH Epidemiology Branch through a contract with GPC. VII. PLAN DEVELOPMENT AND MAINTENANCE This 1-866-PUB-HLTH SOP will be updated annually. The 1-866-PUB-HLTH Manual (PH EOP Annex A-10) is updated as needed (at least annually) to correspond with changing public health needs. VIII. AUTHORITIES AND REFERENCES The Official Code of Georgia §31-12-2. Page 45 of 125 DEPARTMENT OF HUMAN RESOURCES Division Of Public Health Emergency Operations Plan: 1-866-PUB-HLTH Standard Operating Plan Support Annex A1, Appendix 1, Attachment I (As an Epi Primary Document, this document stands alone in Support Annex A 10, Appendix 1) GEORGIA’S PUBLIC HEALTH EMERGENCY AND DISEASE REPORTING HOTLINES MANUAL 1-866-PUB-HLTH (1-866-782-4584) & 1-866-752-3442 Georgia Department of Human Resources Division of Public Health Georgia Poison Center Page 46 of 125 TABLE OF CONTENTS Introduction, Background, & Purpose 4 Introduction Purpose Notifiable Disease Reporting Authority & Confidentiality 5 5 6 6 Procedures, Guidelines, & Flow Charts 8 1-866-PUB-HLTH VS. 1-866-752-3442 General Flow Chart for Calls from Public Health Partners General Flow Chart for Calls from the General Public 9 10 11 Bioterrorism / Mass Casualty Detailed Procedure for Bioterrorism / Mass Casualty Calls from Public Health Partners Blood / Body Fluid Exposures Dead Bird Calls (WNV) Dead Bird Calls (Avian Influenza) Insert: How to Handle Dead Birds or Dead Bird Inquiries Financial Assistance Requests Health Department Routine Services Immunization Availability Questions Infectious Disease Detailed Procedure for Infectious Disease Calls from Public Health Partners Infectious Disease: Smallpox / Smallpox Vaccine / Vaccinia Disease List Insects Crawling In / On A Person Mold Mosquito Complaints Other School / Daycare Issue Swimming Pool Fecal Incident Fecal Incident Chart Records Requests Referral to Advice Nurse Restaurant Complaint Sewage Complaints Unhygienic Tourist Accommodations 12 13 15 16 17 18 19 20 21 22 24 25 31 33 34 35 36 37 38 39 40 41 42 43 Common Mistakes and How to Avoid Them 44 Additional Resources 46 Page 47 of 125 Alphabetical Listing of Georgia Counties and the Districts in which They Belong Insert: Public Health Districts in Georgia Map County & District Hours of Operation Insert: Disease Fact Sheets Page 48 of 125 47 51 INTRODUCTION, BACKGROUND, AND PURPOSE Page 49 of 125 I. INTRODUCTION The Georgia Department of Human Resources, Division of Public Health (GDPH) provides two hotlines for reporting public health emergencies and notifiable diseases. 1-866-PUB-HLTH (1866-782-4584) is for use by public health partners, and 1-866-752-3442 is for use by the general public. The hotlines are housed at and staffed by the Georgia Poison Center (GPC), and are available for use 24 hours a day, 7 days a week. The hotlines are made possible by federal bioterrorism grant funding and a contract between GDPH and GPC, which is renewed annually. II. PURPOSE Georgia’s Public Health Emergency and Disease Reporting Hotlines combine the resources of GDPH at the State and District levels with those of GPC. 1. 1-866-PUB-HLTH The purpose of 1-866-PUB-HLTH is to allow time-sensitive communication among GDPH personnel at the State and District levels, as well as among healthcare providers and emergency response partners at all levels of government. 1-866-PUB-HLTH is for the reporting of immediately notifiable diseases, including those that could result from a bioterrorism event, and public health emergencies. 1-866-PUB-HLTH is one easy-toremember number that should be distributed to all local, state, and federal partners for use in a public health emergency as well as to healthcare providers and other disease reporters to report notifiable diseases. Examples of public health partners that might use 1-866-PUB-HLTH include but are not limited to: Healthcare providers Metro Medical Response System (MMRS) Laboratorians Georgia Management Coroners Agency (GEMA) Medical Examiners Seaports Pharmacists Local police/fire/EMS/911 Veterinarians operators Airport Quarantine Stations Federal Bureau of American Red Cross Investigation (FBI) United States Postal Service Centers for Disease Control Disaster Medical Assistance and Prevention (CDC) Teams (DMAT) Members of the general public should not use 1-866-PUB-HLTH. 2. 1-866-752-3442 The purpose of 1-866-752-3442 is to provide the general public with a way to contact public health in an emergency after normal business hours. The hotline provides for Page 50 of 125 better customer service and may aid in detecting and managing a bioterrorism event, as some districts currently have no other way of accepting calls from the general public at nights or on weekends. The general public hotline began as a pilot involving four volunteer health districts: Gainesville, Columbus, Valdosta, and Waycross. Currently, hotline use has expanded to eight health districts, including the original four plus Fulton, LaGrange, Dalton, and Coastal. III. NOTIFIABLE DISEASE REPORTING The purpose of notifiable disease surveillance is to: 1. identify in a timely way any diseases or conditions that may require immediate public health intervention and follow up; 2. detect changing trends or patterns in disease occurrence; 3. identify areas or communities that require special public health response as a result of changes in disease patterns; and 4. assess and evaluate control and prevention interventions. In Georgia, public health surveillance is conducted on more than 40 diseases and conditions. The data are collected by GDPH at the State and District levels in order to analyze, interpret, and disseminate the information for administrative, program planning, and decision making purposes. The diseases are reported by County Health Departments, District Health Offices, hospitals, clinical and state laboratories, physicians and other healthcare providers, as well as public and private clinics to the Epidemiology Branch in the Division of Public Health. The reports are made electronically, by telephone, by letter, or by mailing weekly reporting forms provided by the Department. Callers to 1-866-PUB-HLTH are reporting a disease by dialing 1-866-PUBHLTH. Although 1-866-PUB-HLTH is marketed towards public health partners for after hours use to report immediately notifiable diseases and public health emergencies, there is some use of the hotline during the day and for diseases that are not emergencies. The Disease List therefore lists other diseases that are not emergencies and do not require a phone call to the district health department after hours. These reports are faxed and the district will receive them the next business day (see instructions for more details about the disease list and when to call). IV. AUTHORITY AND CONFIDENTIALITY The hotlines operate under the legal authority of OCGA §31-12-2, which requires notifiable disease reporting, including those diseases that may result from “bioterrorism, epidemic or pandemic disease, or novel and highly fatal infectious agents or toxins and that may pose a substantial risk of a public health emergency”. OCGA §31-12-2 also requires GDPH to report “any case of an unusual illness, health condition, or death, or an unusual cluster of such events, or any other suspicious health related event that it reasonably believes has the potential to be caused by bioterrorism” to the Department of Public Safety including state and federal partners. Page 51 of 125 OFFICIAL CODE OF GEORGIA: 31-12-2 (a) All Georgia physicians, laboratories and other health care providers are required to report patients with certain conditions to their County Health Department or District Health Office. Reporting enables appropriate public health follow-up for your patients, helps identify outbreaks, and provides a better understanding of disease trends in Georgia. THE HIPPA PRIVACY RULE: 45 CFR 164.512 (b)(1)(i) A covered entity may disclose protected health information…to…a public health authority that is authorized by law to collect or receive such information for the purpose of preventing or controlling disease, injury, or disability, including, but not limited to, the reporting of disease, injury, vital events such as birth or death, and the conduct of public health surveillance, public health investigations, and public health interventions. PATIENT CONFIDENTIALITY Georgia Rule 290-5-3-03: Case reports submitted to county boards of health or to the Department shall be deemed confidential and shall not be subject to public inspection. Georgia Code 31-12-2(b): Any person, including but not limited to practitioners of the healing arts, submitting in good faith reports or data to the Department or county boards of health in compliance with the provisions of this Code section shall not be liable for any civil damages therefore. Page 52 of 125 PROCEDURES, GUIDELINES, AND FLOWCHARTS Page 53 of 125 1-866-PUB-HLTH VS. 1-866-752-3442 Hotline calls come from two different groups of people. When answering a call, it is important to find out who is calling. Is it a Public Health Partner, or the General Public? Greeting: “Georgia Public Health Hotline, how may I help you?” 1-866-PUBHLTH Caller is a public health partner* Caller wants to report a notifiable disease. Caller wants to report a public health emergency. 1-866-7523442 Caller is a member of the general public Caller wants to speak to someone in public health immediately for any reason. Caller wants to report a notifiable disease. Caller wants to report a public health emergency. Caller wants advice on a non-emergency issue. *Public Health Partners may include but are not limited to: healthcare providers, laboratorians, public health, coroners, medical examiners, pharmacists, veterinarians, airport quarantine stations, American Red Cross, United States Postal Service, Page 54 of 125 Disaster Medical Assistance Teams (DMAT), Metro Medical Response System (MMRS), Georgia Management Agency (GEMA), seaports, local police/fire/EMS/911 operators, Federal Bureau of Investigation (FBI), Centers for Disease Control and Prevention (CDC). Page 55 of 125 GENERAL FLOW CHART FOR CALLS FROM PUBLIC HEALTH PARTNERS Greeting: Georgia Public Health Hotline. How may I help you? Verify caller is a Public Health Partner (healthcare provider, laboratorian, public health, emergency responder, etc.) To report case(s) of disease Purpose of call? Patient’s county of residence? To contact public health immediately for reason other than to report a case of disease Caller’s county of employment? Complete an Information Request including the Infectious Disease tab. Find disease on disease list. (See detailed instructions). Does caller want a call back from Public Health? If yes (and call is received during non-business hours), ask if the next business day is OK for the return call. Complete Information Request End call. Contact the District Epi On-Call by phone or pager to relay the message. (This will be the District Epi On-Call, unless the caller specifically requests to speak to another On-Call Representative like the EC On-Call or the State). End call. Use Alphabetical List of GA Counties to find the health district in which the county belongs. If the disease reported is “EC” or “EPI”, or the caller requested a same-day return call, CALL the District EC or EPI (depending on disease—check Disease List) On-Call Representative. If the disease reported is “FAX” (and the caller did NOT request a same-day return call), FAX the report to the District EPI On-Call Representative. (If caller wanted a return call the next business day, be sure to fax this information to the District Epi On-Call as well). If you are unable to locate the disease on the list, CONSULT with your supervisor and/or call the State Epi OnCall. Page 56 of 125 GENERAL FLOW CHART FOR CALLS RECEIVED FROM THE GENERAL PUBLIC Greeting: “Georgia Public Health Hotline, how may I help you?” Caller is calling to report an emergency or non-emergency situation related to public health, or to ask a question. Complete an Information Request Form. Tips: The type of call (emergency or non-emergency) may require a judgment call after asking appropriate questions of the caller and assessing the situation. For situations described as food poisonings, infectious diseases, or dead birds a supplemental form will pop up and ask for additional information. Use flow charts/guidelines for common public health inquiries to answer the caller’s questions. If additional information is needed about a specific disease, answer the caller’s questions using the disease fact sheets. Contact or fax the report to the appropriate District Health Department as instructed on the flow chart/guidelines. If the instructions are not clear, consult with your supervisor. Page 57 of 125 BIOTERRORISM / MASS CASUALTY Calls involving chemical exposures or illnesses that the caller reports might be the result of an intentional exposure, criminal act, or terrorist attack. Mass casualty (or the potential for such) including but not limited to the following: large numbers of people ill, accidental exposures, train derailments, tanker truck spills, meth lab explosions, etc. Fill out an Information Request Form. Advise the caller to hang up and dial 911 to report the incident and to request medical help. If it is a chemical exposure or other area of GPC expertise, give them the number for GPC (404616-9000 or 800-222-1222) for more information. Call the State EC On-Call immediately. Tell the State EC On-Call that you will ALSO be calling the District EC On-Call. Give the State EC OnCall the name and phone number for the Primary District EC On-Call. Call the District EC On-Call for the district where the event took place. Tell the District contact that you also called the State EC OnCall, and give the District contact the name and phone number of the State EC On-Call with whom you spoke. Page 58 of 125 DETAILED PROCEDURE FOR BIOTERRORISM/MASS CASUALTY CALLS FROM PUBLIC HEALTH PARTNERS 1. If the caller does not identify himself right away, verify that he is a Public Health Partner (healthcare provider, laboratorian, public health, emergency responder, etc). 2. If the caller is calling to report a single case of disease that is not suspected to be the result of an intentional exposure, criminal act, or terrorist attack, follow the instructions “DETAILED PROCEDURE FOR INFECTIOUS DISEASE CALLS FROM PUBLIC HEALTH PARTNERS”. 3. Request the name of the county where the event took place (event county). If the caller does not know the event county, request the county the caller is calling from (caller county). 4. Complete an Information Request Form to document the call. 5. End the call. 6. Use the Alphabetical Listing of GA Counties to find the health district in which the county belongs. 7. Bioterrorism/Mass Casualty calls from Public Health Partners are ALWAYS an emergency situation! Contact the District EC On-Call Representative AND the State EC On-Call Representative immediately by phone or pager. 1. Log onto SendSS and locate the contact numbers for the Primary State EC OnCall Representative (see SendSS instructions). 2. For pager notifications, wait 10 minutes for the On-Call Representative to respond. If there is no response, go to the next number listed for the Primary OnCall Representative. If no response after attempted contact of the Primary OnCall Representative, call the Backup On-Call Representative(s) in the order listed until a contact is made. 3. Tell the State EC On-Call Representative that you will ALSO be calling the District EC On-Call Representative. Give the State EC On-Call the name and phone number for the Primary District EC On-Call. 4. Call the District EC On-Call Representative for the district where the event took place (event county). Tell the District EC On-Call that you also called the State EC On-Call, and give the District contact the name and phone number of the State EC On-Call with whom you spoke. 8. For chemical exposures of any type or any illness that the caller reports might be the result of an intentional exposure, criminal act, or terrorist attack – Notify the District AND State EC On-Call Representatives immediately! 9. For reports of anthrax, smallpox, or botulism (suspect or confirmed) contact the District AND State On-Call Representatives immediately! Use the Disease List to see if the disease is “EC” or “EPI”. 10. Notify the District EPI On-Call Representative immediately by phone of any reported cluster of ANY illness. 1. Use these guidelines to decide if it’s a cluster (either in this call or among a few calls received in the time span of a few hours): 1. For GI illness or rash illness, 3 or more cases not in the same household. 2. For hospitalized respiratory illness, 2 or more not in the same household. Page 59 of 125 For non-hospitalized respiratory illness and all other illnesses, greater than 10 cases. Page 60 of 125 BLOOD / BODY FLUID EXPOSURES Is the caller the person exposed, or is the caller a person from employee health wanting a public health consult? Person exposed or other member of the public Is the caller employed as a healthcare worker, laboratory worker, EMS worker, or other occupational exposure? Employee health NO Can the caller see his/her doctor that same day? YES Complete an Information Request Form. Call or page the District Epi On-Call (use the district of the exposed person’s residence). If exposed residence is unknown, use the district of the institution. Tell caller to report the incident to employee health immediately and follow their procedures for occupational blood exposures. YES NO Instruct caller to visit his/her doctor that same day. Instruct caller to visit the emergency department within 24 hrs. Complete an Information Request Form. FAX to the District Epi On-Call (use district of the exposed person’s residence). Blood / Body Fluid Exposure Information for Public Health Specialists (note: this information may be used to answer questions if the caller specifically asks for more information) What diseases can be transmitted by what body fluids? HIV Hepatitis A Hepatitis B Hepatitis C Blood or other body fluids containing blood yes no*1 yes yes Saliva Urine Feces no no no no no no no no no yes no no Semen / Vaginal Fluid yes yes yes yes*2 *1 On rare occasions, hepatitis A virus has been transmitted by transfusion of blood or blood products. *2 Sexual transmission of hepatitis C virus appears to occur, but the virus is inefficiently spread in this manner. Additional resource for clinicians only: National Clinicians’ Postexposure Prophylaxis Hotline (PEPline)—Run by University of California-San Francisco / San Francisco General Hospital staff; supported by the Health Resources and Services Administration Ryan White CARE Act, HIV/AIDS Bureau, AIDS Education and Training Centers, and CDC. 1-888-448-4911 Page 61 of 125 DEAD BIRD CALLS (WNV) (revised 11/9/2006) USE THIS FLOW CHART FOR BIRDS OF PREY (E.G. FALCONS, HAWKS, EAGLES), SONGBIRDS, AND SIMILAR SPECIES ONLY (E.G. PIGEONS, CARDINALS, CROWS, WRENS, BLUE JAYS, ETC.) Complete an Information Request Form AND Supplemental Dead Bird Call Form. Does the bird have visible decomposition? Advise the caller to safely dispose of the dead bird by double bagging it in sealed plastic bags and placing it in the trash or burying it. Do not handle the bird with bare hands. YES NO Pet bird What kind of bird is it? Wild songbird or similar species (i.e. pigeon, cardinal, wren, blue jay, crow, etc.) or UNKNOWN Tell caller to consult their veterinarian. Did the call come in on a weekend? YES Will the caller double bag the bird in sealed plastic bags and place in the refrigerator (do not freeze) for the weekend? NO Wild bird of prey (i.e. falcon, hawk, eagle, etc.) YES NO FAX completed form to the caller’s District ENV On-Call Rep. If they have additional questions, tell them to contact their county environ. health office during regular business hours. Educate the caller using “How to Handle Dead Birds or Dead Bird Inquiries”. Tell the caller that it is the district health department’s decision to make (during normal business hours) whether or not the bird will be submitted for testing (i.e. saving it in the refrigerator does not guarantee that it will be tested). See p. 10 in “How to Handle Dead Birds or Dead Bird Inquiries” for reasons why a bird might not be submitted for testing. Page 62 of 125 Bird MIGHT be tested for WNV or Avian Flu. Tell caller to call their regional Georgia Department of Natural Resources (DNR) Game Management Specialist during office hours (look up phone # by county for the caller using p. 7 of “How to Handle Dead Birds or Dead Bird Inquiries”). DNR will decide if/what to test the bird for. If bird not too large, caller should double bag it and store it in a refrigerator or in an iced cooler. If cooler is used, replace ice as needed to keep bird cold. Do not handle with bare hands. DEAD BIRD CALLS (Avian Influenza) (updated 11/9/2006) USE THIS FLOW CHART FOR DEAD WATERFOWL, SHORE BIRDS, CHICKENS, AND OTHER POULTRY. Complete an Information Request Form AND Supplemental Dead Bird Call Form. Does the bird have visible decomposition? YES Advise the caller to safely dispose of the dead bird by double bagging it in sealed plastic bags and placing it in the trash or burying it. Do not handle the bird with bare hands. NO Canada goose What kind of bird is it? If <5 sick/dead, use procedure for WNV testing from the Dead Bird Call Flow Chart (WNV). Canada geese are not migratory and will not be tested for avian influenza unless there is a large die-off. Waterfowl, shore bird (i.e. duck, goose, seagull, etc.) EXCEPT Canada goose If <5 sick/dead, tell caller to call their regional Georgia Department of Natural Resources (DNR) Game Management Specialist during office hours (look up phone # by county for the caller using p. 7 of “How to Handle Dead Birds or Dead Bird Inquiries”. If bird not too large, caller should double bag it and store it in a refrigerator or in an iced cooler. If cooler is used, replace ice as needed to keep bird cold. Do not handle with bare hands. If ≥5 sick/dead, tell caller to call DNR Game Management Specialist (1800-TRYGEMA) Other wild bird, songbird, or pet bird (i.e. pigeon, blue jay, crow, pet cockatiel, pet canary, etc.) Chicken or other poultry (i.e. quail, turkey, gamefowl) If <4 or <10% of flock sick/dead If ≥4 or ≥ 10% of flock sick/dead Stop. Use the other Dead Bird Call Flow Chart (WNV). Tell caller to call the State Veterinarian’s Office (1-800-TRYGEMA) or the USDA Area Veterinarian’s Office (770-922-7860) immediately, 24/7. Tell caller to call the closest Georgia Poultry Lab during normal business hrs (look up phone # on p. 8 of “How to Handle Dead Birds or Dead Bird Inquiries”). Meanwhile, double bag bird(s) and place in an iced cooler or in a refrigerator. If cooler is used, replace ice as needed to keep bird cold. Do not handle with bare hands. Educate the caller using p. 9-11 of “How to Handle Dead Birds or Dead Bird Inquiries”. Page 63 of 125 FAX the completed form to the GA Division of Public Health at 404-6577517 ATTN: Dana Cole. FINANCIAL ASSISTANCE REQUESTS “I need help paying my medical bills.” Fill out an Information Request Form. Instruct the caller to call the Health Department during normal business hours. There is no need to fax a form to the district health department. Remind the caller that this phone number is for public health EMERGENCIES. Page 64 of 125 HEALTH DEPARTMENT ROUTINE SERVICES “I need to schedule an appointment at the health clinic.” Fill out an Information Request Form Instruct the caller to call the Health Department during normal business hours. There is no need to fax a form to the district health department. Remind the caller that this phone number is for public health EMERGENCIES. Page 65 of 125 IMMUNIZATIONS AVAILABILITY QUESTIONS “Where can I get a flu shot?” Fill out an Information Request Form. What kind of vaccine(s) are you seeking? Flu Shots --County health departments offer flu shots, but people should call ahead (during normal business hours) to confirm the county has vaccine and the hours/days it is being offered. At http://www.immunizeadultga.org/search.asp you can search by zip code for the nearest county health department clinic and information about flu shots at that location. --Sometimes people don't want to go to the county health department or it's easier to go to a Publix, Kroger, CVS, Walgreens, etc. The following websites list locations of flu clinics in their neighborhood by zip code: http://www.findaflushot.com/ and http://www.flucliniclocator.org/. --If the person doesn't have internet access, you can do the searches for them over the phone. Page 66 of 125 Travel, school, and all other immunizations Tell the caller to call the Health Department during normal business hours. There is no need to fax the Information Request to the Health Department. INFECTIOUS DISEASE (for smallpox-related calls, see “Infectious Disease: smallpox / smallpox vaccine / vaccinia” flowchart) Caller is calling to report a case of known or suspected infectious disease in him/herself or in another person. Complete an Information Request Form with Infectious Disease Supplemental Form. Is the caller a Public Health Partner (healthcare provider, laboratorian, medical examiner, public health worker, etc.)? YES YES NO or unknown NO Advise the patient to seek medical attention. If it is an emergency, send the patient to the emergency department. YES Did the doctor diagnose this patient with this condition? Locate the disease on the Disease List. Determine if the disease is “EC” (Emergency Coordinator), “EPI” (Epidemiology/Immediately Reportable), or “FAX” (other reportable diseases). Follow detailed instructions next page. Always ask if the physician would like a call back from public health. NO FAX report to the District EPI On-Call of the patient’s residence. If patient’s residence is unknown, use caller’s residence. Tell the patient to return to the doctor if he/she does not get better, or seek a 2nd opinion. If FAX disease or not on the Disease List If “EC” or “EPI” disease Contact the District EC or EPI immediately by phone or pager. Use the district of the patient’s residence. If the patient’s residence is unknown, use the district of the physician’s institution (office or hospital). Has the patient seen a doctor for this condition? YES Could this be a cluster or outbreak of disease? To decide, use these guidelines (either in this call or among a few calls received in the time span of a few hours): For GI illness or rash illness, 3 or more cases not in the same household. For hospitalized respiratory illness, 2 or more not in the same household. For non-hospitalized respiratory illness and all other illnesses, greater than 10 cases. Page 67 of 125 NO FAX report to the District EPI On-Call of the patient’s residence. If patient’s residence is unknown, use the district of the physician’s institution (office or hospital). If callers need more information: Georgia Division of Public Health website www.health.state.ga.us. DETAILED PROCEDURE FOR INFECTIOUS DISEASE CALLS FROM PUBLIC HEALTH PARTNERS 1. If the caller does not identify himself right away, verify that he is a Public Health Partner (healthcare provider, laboratorian, public health, emergency responder, etc). If he is a member of the general public, use the instructions for calls from the General Public (see Infectious Disease flowchart). 2. Request the patient’s county of residence. If the caller does not know the patient’s county of residence, ask for the county of the facility (office or hospital) where the patient was seen. If the caller is not calling about a single specific patient but still needs to contact Public Health, ask for the caller’s county of employment. 3. Complete the Information Request Form including the Infectious Disease tab. (Do this for any disease that the caller is reporting, whether or not you are able to locate it on the Disease List). a. Locate the disease being reported on the Disease List. b. If you cannot find the disease on the list, ask the caller if the disease has another name. If you find something on the list that is similar but not exactly the same as what the caller said, ask the caller if that is the same thing. c. If there is no other name or you cannot find any of the names the caller gives on the list, you should still fill out the Infectious Disease tab using whatever disease name the caller gives you. 4. If the caller does not wish to report a case of disease, but only wants to contact Public Health, still complete an Information Request Form to document the call. 5. Ask the caller, “Do you wish to receive a call back from public health?” If the caller says yes, and the call is not received during regular working hours, ask whether the caller needs a response back before the next business day. Public Health Partners may request to speak with Public Health immediately for any reason. 6. End the call. 7. Use the Alphabetical Listing of GA Counties to find the health district in which the county belongs. 8. Locate the disease on the Disease List and report to the District as follows: a. If the disease is under “EC” (Emergency Coordinator), contact the District EC On-Call Representative immediately by phone or pager. i. Log onto SendSS and locate the contact numbers for the Primary District EC On-Call Representative (see SendSS instructions). ii. For pager notifications, wait 15 minutes for the EC On-Call Representative to respond. If there is no response, go to the next number listed for that person. If no response after attempted contact of the Primary On-Call Representative, call the Backup On-Call Representative(s) in the order listed until a contact is made. iii. If attempts to contact the District are unsuccessful, contact the State EC On-Call Representative (listed at the bottom of the District EC On-Call tab). b. If the disease is under “EPI” (Epidemiology), contact the District EPI On-Call Representative immediately by phone or pager. Page 68 of 125 i. Log onto SendSS and locate the contact numbers for the Primary District EPI On-Call Representative (see SendSS instructions). ii. For pager notifications, wait 15 minutes for the EPI On-Call Representative to respond. If there is no response, go to the next number listed for the Primary On-Call Representative. If no response after attempted contact of the Primary On-Call Representative, call the Backup On-Call Representative(s) in the order listed until a contact is made. iii. If attempts to contact the District are unsuccessful, contact the State EPI On-Call Representative (404-657-2588 during normal working hours, 770-578-4104 after hours). c. If the disease reported is under “FAX” (Other Reportable Diseases / NonEmergency), fax the completed Information Request to the appropriate District Health Department. i. Log onto SendSS and locate the FAX number for the Primary EPI OnCall Representative (see SendSS instructions). d. If you are unable to locate the disease reported anywhere on any of the lists, consult with your supervisor if available, and then contact the State EPI On-Call Representative immediately by phone (404 657-2588 during normal working hours, 770 578-4104 after hours) if there is still a question regarding how to handle the report. 9. If the caller did not want to report a disease but just wanted to contact Public Health immediately, contact the District EPI On-Call Representative by phone or pager in the same manner used for EPI diseases (see “8.b.” above), and give the message and caller’s contact information to the responding official. NOTE: If the call is regarding suspect Bioterrorism, Mass Casualty, or similar, use the instructions “DETAILED PROCEDURE FOR BIOTERRORISM/MASS CASUALTY CALLS FROM PUBLIC HEALTH PARTNERS”. a. Regardless of the reason for the call, if the caller (confirmed to be a Public Health Partner) requested a call back from Public Health, be sure to notify the District EPI On-Call Representative and give them the caller’s contact information. (If the caller stated that a return call on the next business day would be adequate, fax the message and request for a return call, along with the caller’s contact information, to the District EPI On-Call Representative). 10. For chemical exposures of any type or any illness that the caller reports might be the result of an intentional exposure, criminal act, or terrorist attack – Notify the District AND State EC On-Call Representatives immediately! 11. For reports of anthrax, smallpox, or botulism (suspect or confirmed) contact the District AND State On-Call Representatives immediately! 12. Notify the District EPI On-Call Representative immediately by phone of any reported cluster of ANY illness. a. Use these guidelines to decide if it’s a cluster (either in this call or among a few calls received in the time span of a few hours): i. For GI illness or rash illness, 3 or more cases not in the same household. ii. For hospitalized respiratory illness, 2 or more not in the same household. iii. For non-hospitalized respiratory illness and all other illnesses, greater than 10 cases. Page 69 of 125 INFECTIOUS DISEASE: SMALLPOX / SMALLPOX VACCINE / VACCINIA Caller is calling to report a case of (or suspect case of ) smallpox, smallpox vaccine reaction, or vaccinia. Complete an Information Request Form with Infectious Disease Supplemental Form. Is the caller a Public Health Partner (healthcare provider, laboratorian, medical examiner, public health worker, etc.)? NO YES Have you recently received the smallpox vaccine, or are you a close contact of someone who has received the vaccine? Do you want to consult about a patient? YES Contact the District EPI OnCall immediately by phone or pager. Use the district of the patient’s residence. If the patient’s residence is unknown, use the district of the physician’s institution (office or hospital). Also contact the State EPI On-Call immediately. Tell the State EPI on call the name and phone number of the District EPI On-Call with whom you spoke. NO YES FAX the Information Request Form to the District EPI of the patient’s residence. If there is no patient, use the caller’s county. Provide telephone number to District Office for information during regular business hours. NO Do you have any of the following symptoms: Chest pain? Shortness of breath? Extreme weakness? Severe headache? Confusion? Stiff neck? YES Advise caller to get immediate medical attention at the emergency room and to inform the doctor about the smallpox vaccination. Page 70 of 125 Provide telephone number to District Health Director’s office for smallpox information during regular business hours. NO Do you have fever, any concerns about the vaccination site, or a rash or sore? YES NO DISEASE LIST Red = “EC” (Emergency Coordinator) Report immediately by phone to District EC OnCall Representative. Blue = “EPI” (Epidemiology / Immediately Reportable Diseases) Report immediately by phone to District EPI On-Call Representative. Green = “FAX” (Other Reportable Diseases) Report by FAX to District EPI On-Call. *** = Report immediately by phone to BOTH the District AND the State On-Call Rep. 0157:H7 E. coli - EPI 0157:H7 Escherichia coli - EPI AIDS - FAX Animal Rabies – FAX Animal Bites – FAX Anthrax (any type) – EC*** Arboviral Illness - FAX Argentinian Hemorrhagic Fever - EPI Aseptic Meningitis - EPI Avian Influenza - EPI Bacillus anthracis – EC*** Bacterial Meningitis - EPI Bird Flu - EPI Birth Defects – FAX Bites, Animal – FAX Bolivian Hemorrhagic Fever - EPI Bordetella pertussis - EPI Botulism (foodborne type or unspecified type) – EPI*** Botulism (infant, intestinal, wound) – EPI*** Brazilian Hemorrhagic Fever - EPI Brucella - EPI Brucellosis - EPI Bubonic Plague - EPI Campylobacteriosis - FAX Cancer (any type) - FAX Chancroid- FAX Chemical Exposure (any type) – EC Chicken pox - FAX Chlamydia - FAX Cholera - EPI CJD [Creutzfeld-Jakob Disease] - FAX Clostridium botulinum – EPI*** Cluster (more than one case) of any illness - EPI Corynebacterium diphtheriae - EPI Coxiella burnetti - EPI Creutzfeld-Jakob Disease - FAX Crimean-Congo Fever - EPI Cryptosporidiosis - FAX Cutaneous Anthrax – EC*** Page 71 of 125 DISEASE LIST Red = “EC” (Emergency Coordinator) Report immediately by phone to District EC OnCall Representative. Blue = “EPI” (Epidemiology / Immediately Reportable Diseases) Report immediately by phone to District EPI On-Call Representative. Green = “FAX” (Other Reportable Diseases) Report by FAX to District EPI On-Call. *** = Report immediately by phone to BOTH the District AND the State On-Call Rep. Cyclosporiasis - FAX Diphtheria - EPI Eastern Equine Encephalitis - FAX Ebola Hemorrhagic Fever / Ebola - EPI E. coli 0157:H7 - EPI E. coli (Enterohemorrhagic, Shiga Toxin-Producing, Verotoxin-Producing) - EPI Ehrlichia - FAX Ehrlichiosis – FAX Elevated Blood Lead Level - FAX Encephalitis (any type) - FAX Enterohemorrhagic E. coli - EPI Enterohemorrhagic Escherichia coli - EPI Escherichia coli 0157:H7 - EPI Escherichia coli (Enterohemorrhagic, Shiga Toxin-Producing, Verotoxin-Producing) - EPI Flu (suspected avian flu OR hospitalized with international travel) – EPI Flu (seasonal flu) – FAX Flu-associated pediatric death - FAX Foodborne Botulism – EPI*** Francisella tularensis - EPI Gastrointestinal Anthrax – EC*** Giardia - FAX Giardiasis - FAX Gonorrhea - FAX Group A Strep Disease - FAX Group A Streptococcal Disease - FAX Group B Strep Disease - FAX Group B Streptococcal Disease - FAX Haemophilus influenzae Disease - EPI Haemophilus influenzae Meningitis - EPI Haemophilus Meningitis - EPI Hantaviral Infection / Hantaviral Disease - EPI Hantavirus - EPI Hantavirus Pulmonary Syndrome - EPI Hearing Impairment - FAX Hemolytic Uremic Syndrome - EPI Hemorrhagic Fever - EPI Hemorrhagic Fever with Renal Syndrome - EPI Hepatitis A – EPI Hepatitis B – FAX Page 72 of 125 DISEASE LIST Red = “EC” (Emergency Coordinator) Report immediately by phone to District EC OnCall Representative. Blue = “EPI” (Epidemiology / Immediately Reportable Diseases) Report immediately by phone to District EPI On-Call Representative. Green = “FAX” (Other Reportable Diseases) Report by FAX to District EPI On-Call. *** = Report immediately by phone to BOTH the District AND the State On-Call Rep. Hepatitis C – FAX H. flu Disease - EPI H. flu Meningitis - EPI Hib Diseases – EPI Hib Meningitis - EPI HIV - FAX Human Rabies - EPI Infant Botulism – EPI*** Infectious Hepatitis (Report Type A immediately. Report other types by fax) - EPI Infectious Hepatitis (other than Type A – report Type A immediately) - FAX Influenza (suspected avian flu OR hospitalized with international travel) – EPI Influenza (seasonal flu) – FAX Influenza-associated pediatric death -- FAX Inhalational Anthrax – EC*** Intestinal Anthrax – EC*** Intestinal Botulism – EPI*** Invasive Group A Strep Disease - FAX Invasive Group A Streptococcal Disease - FAX Invasive Group B Strep Disease - FAX Invasive Group B Streptococcal Disease - FAX Invasive Haemophilus influenzae Disease - EPI Invasive H. flu Disease - EPI Invasive Hib Disease - EPI Invasive Meningococcal Disease - EPI LaCrosse Encephalitis - FAX Lassa Hemorrhagic Fever / Lassa - EPI Lead Blood Level greater than or equal to 10 micrograms per deciliter - FAX Legionella - FAX Legionellosis - FAX Legionnaires’ Disease - FAX Leptospirosis - FAX LGV [Lymphogranuloma venereum] - FAX Listeria - FAX Listeriosis - FAX Lyme Disease - FAX Lymphogranuloma venereum - FAX Malaria - FAX Marburg Hemorrhagic Fever / Marburg - EPI Measles - EPI Meningitis (any type) - EPI Page 73 of 125 DISEASE LIST Red = “EC” (Emergency Coordinator) Report immediately by phone to District EC OnCall Representative. Blue = “EPI” (Epidemiology / Immediately Reportable Diseases) Report immediately by phone to District EPI On-Call Representative. Green = “FAX” (Other Reportable Diseases) Report by FAX to District EPI On-Call. *** = Report immediately by phone to BOTH the District AND the State On-Call Rep. Meningococcal Disease - EPI Meningococcal Meningitis - EPI Meningococcal Sepsis - EPI Meningococcemia – EPI Meningoencephalitis – EPI Methicillin-resistant Staph aureus – FAX Methicillin-resistant Staphylococcus aureus - FAX Monkeypox – EPI MRSA - FAX Mumps - EPI Neisseria meningitides - EPI Non H1 or H3 Flu - EPI Non H1 or H3 Influenza - EPI Non-Typable Flu - EPI Non-Typable Influenza – EPI Pediatric Influenza Death - FAX Pertussis - EPI Plague (any type) - EPI Pneumococcal Infection / Disease - FAX Pneumonia in someone who traveled recently - EPI Pneumonic Plague - EPI Polio - EPI Poliomyelitis - EPI Psittacosis - FAX Purpura fulminans - EPI Q Fever - EPI Rabies (in a human) - EPI Rabies (in an animal) - FAX Respiratory Disease in someone who traveled recently - EPI Rift Valley Fever - EPI Rocky Mountain Spotted Fever - FAX Saint Louis Encephalitis - FAX Salmonella - FAX Salmonellosis - FAX SARS - EPI Severe Acute Respiratory Syndrome - EPI Shiga Toxin Positive Test - EPI Shiga Toxin-Producing E. coli - EPI Shiga Toxin-Producing Escherichia coli – EPI Shigella - FAX Page 74 of 125 DISEASE LIST Red = “EC” (Emergency Coordinator) Report immediately by phone to District EC OnCall Representative. Blue = “EPI” (Epidemiology / Immediately Reportable Diseases) Report immediately by phone to District EPI On-Call Representative. Green = “FAX” (Other Reportable Diseases) Report by FAX to District EPI On-Call. *** = Report immediately by phone to BOTH the District AND the State On-Call Rep. Shigellosis - FAX South American Hemorrhagic Fever - EPI Smallpox – EPI*** (See Smallpox instructions) Staph aureus resistant to methicillin / with methicillin resistance - FAX Staph aureus resistant to vancomycin / with vancomycin resistance – EPI Staphylococcus aureus resistant to methicillin / with methicillin resistance - FAX Staphylococcus aureus resistant to vancomycin / with vancomycin resistance - EPI Staph aureus with elevated vancomycin MIC [minimum inhibitory concentration] - EPI Staphylococcus aureus with elevated vancomycin MIC [minimum inhibitory concentration] EPI Strep A – FAX Strep B - FAX Strep pneumo – FAX Streptococcal Disease (Group A or B) - FAX Streptococcus pneumoniae - FAX Syphilis - FAX TB - FAX Tetanus - FAX Toxic Shock Syndrome - FAX Toxoplasmosis - FAX Tuberculosis - FAX Tularemia - EPI Typhoid - FAX Unexplained Pneumonia in a Traveler - EPI Unexplained Respiratory Disease in a Traveler - EPI Vancomycin-Intermediately Susceptible Staph aureus - EPI Vancomycin-Intermediately Susceptible Staphylococcus aureus - EPI Vancomycin-Resistant Staph aureus - EPI Vancomycin-Resistant Staphylococcus aureus - EPI Venezuelan Hemorrhagic Fever - EPI Verotoxin-Producing E. coli - EPI Verotoxin-Producing Escherichia coli - EPI Vibrio cholerae - EPI Vibrio Infection - EPI Viral Hemorrhagic Fever (any type) - EPI Viral Hepatitis (Report Type A immediately. Report other types by fax.) - EPI Viral Hepatitis (other than Type A – report Type A immediately) - FAX Viral Meningitis - EPI VISA [pronounced like the credit card] - EPI VRSA [pronounced “versa” or “V-R-S-A”] - EPI Page 75 of 125 DISEASE LIST Red = “EC” (Emergency Coordinator) Report immediately by phone to District EC OnCall Representative. Blue = “EPI” (Epidemiology / Immediately Reportable Diseases) Report immediately by phone to District EPI On-Call Representative. Green = “FAX” (Other Reportable Diseases) Report by FAX to District EPI On-Call. *** = Report immediately by phone to BOTH the District AND the State On-Call Rep. West Nile Virus - FAX Whooping Cough - EPI Wound Botulism – EPI*** Yellow Fever in someone WITH international travel history - FAX Yellow Fever in someone WITHOUT international travel history - EPI Yersinia pestis - EPI Yersinia (Exception: Report Yersinia pestis immediately as Section A Bioterrorism) - FAX Yersiniosis - FAX Page 76 of 125 INSECTS CRAWLING IN / ON A PERSON (always a non-emergency situation) “I have bugs, worms, fibers, or mites crawling out of my skin” Fill out an Information Request Form Answer the person’s questions using the talking points below. Advise the caller to visit their primary care physician. If the caller does not have insurance, tell him to visit the county health department. FAX the form to the District EPI On-Call of the caller’s residence. Information for GPC staff: The caller may have delusory parasitosis. Delusory parasitosis is a mental health condition commonly caused by one of many physical health conditions. There are a few things in common to sufferers of delusory parasitosis: They feel like bugs, worms, fibers, or mites are biting, crawling, or burrowing into, under, or out of their skin. They can feel them and see them, even if no one else can. If someone else can see them, it is never a physician. They think their home or furniture is infested. They may tell you that no one seems to believe the "bugs" or "fibers" exist except themselves, or maybe a friend, who is “also infested”. They may have seen many doctors, who either refuse to listen, refuse to see them, or refer them to someone else. They have tried lots of different remedies, none of which worked at all or for long. They will offer to show/send you the "bugs" or "fibers". They will often say that the problem is spreading to family, family pets, and friends. They will say they saw whatever is causing their problem on the internet. Suggestions for dealing with the caller: Ask the person if they have contacted their health care provider and discussed the issue. Be prepared for a diatribe against physicians. Remind them that this is a medical condition, and must be dealt with by a physician (do this repeatedly). If they are taking any medications, they should ask their physicians about drug reactions. Emphasize that they should continue taking their medications until their physicians tells them to stop. Tell them to visit their primary care physician, or county health department if they have no insurance. Page 77 of 125 If they talk about bugs living under their skin or fibers coming out from their skin, emphasize that insects and parasites do not behave in the manner they are describing. Suggest the use of oils, lotions, or oatmeal soaks to help with itching or dry skin. Emphasize that they should never self-medicate or use other chemicals on their skin without a physician's express order. Tell them this will just aggravate the problem. If they are concerned about fleas on pets, tell them to take their pet to the veterinarian. Other things to consider: o Stress o Drug/alcohol abuse o Allergic sensitivity to nonliving substances in the environment o Dry skin Most of the time, if you listen sympathetically, emphasize eliminating behaviors that will cause harm (over-application of pesticides, digging the "bugs" out of the skin, use of harsh chemicals, etc), suggest the use of oatmeal soaks and skin lotions to reduce itching, and remind them (repeatedly) to see a physician, the caller will be satisfied. It does no good to tell these callers that they are imagining things. To their minds, the itching and infestation is very real. Page 78 of 125 MOLD Complete an Information Request Form. Answer the caller’s questions using the talking points below. If the person is sick, tell them to seek medical attention. FAX the completed Information Request to the District ENV On-Call Representative of the caller’s residence. Mold Talking Points: Mold frequently grows in homes, schools, and other buildings when humid warm conditions and/or where leaks are present indoors. Many different mold species can be found indoors. No particular species has been demonstrated to pose a higher risk to the general public than any other. People with allergies to mold can suffer adverse effects, but the ability of mold to cause other human illness is controversial and not well established. Allergy symptoms may include stuffy or runny nose, difficulty breathing, worsening of asthma, chest tightness, headache, altered sense of smell or seeming to smell unusual odors, or feeling tired. If you develop these or other symptoms, you should see your doctor. The two main strategies for managing mold are removing the sources of moisture and cleaning up the mold. If there is a lot of mold present (an area greater than 3 feet by 3 feet), you may need to hire someone experienced in removing mold rather than attempting it yourself. Whether or not the mold is the cause of health problems, there is clearly no benefit to having the mold present. The best approach to mold can be summarized in the phrase, “Clean up the mold and dry out the building.” Tips for cleaning up mold: o Wear gloves, a filter mask (N-95), and goggles. These items can be purchased at home improvement stores. o First fix any water leaks or obvious sources of moisture. o Damp wipe or scrub thoroughly all contaminated surfaces with warm water and non-ammonia soap / detergent. o Rinse and thoroughly dry the cleaned surface of water and moisture. o If desired, you can use a bleach solution to disinfect the area after cleaning. This does not prevent the re-growth of mold. Do not mix bleach with products containing ammonia as a toxic gas will form. Wearing gloves, mix ½ cup bleach with one gallon of water and apply to the surface using a sponge, mop, or spray bottle. Be sure to ventilate the area. Remove excess bleach solution and allow the area to dry. For more information about landlord issues, call the Georgia Landlord-Tenant Hotline at 404-463-1596 or 800-369-4706. Page 79 of 125 MOSQUITO COMPLAINTS (always a non-emergency situation) Complete an Information Request Form and FAX to the District ENV On-Call Representative. Enter the following information in the comments section: Address/location of the problem if not the same as the caller’s address Time of day mosquitoes are biting (middle of the day vs. dusk and dawn) Educate the caller using the following talking points: 1.) Mosquito control is done at the city or county level. To find out if your city or county has a mosquito control program, contact your public works office. 2.) Not all mosquitoes carry West Nile virus. The ones that do carry West Nile virus breed in water holding containers and polluted waters and do not fly more than half a mile from where they breed. This means that you and your neighbors should act together to find the breeding sites and eliminate them. 3.) Tips for reducing mosquito breeding sites: Dump the water out once a week: bird baths, ornamental ponds, swimming pool covers, boat covers, boats, rain barrels, trash cans, buckets, toys, etc. Eliminate from your yard: tires (or drill holes in tire swings), trash along the roadway, flower pot saucers, leaf litter, and low spots or ditches that hold water for several days Clean and properly maintain: clogged gutters, swimming pools, and window screens 4.) For retention ponds and other bodies of standing water that cannot be drained, use larvacides that kill mosquito larvae before they become biting adults. Larvacides (for example Bti, mosquito dunks, and others) can be purchased at home improvement stores. Alternatively, mosquito-eating fish can be put into the water. 5.) Wear an insect repellent containing DEET (for example Off, Cutter, and others) when outside if mosquitoes are biting. Do not use more than 30% DEET on children. Do not use DEET on infants under 2 months of age (keep them inside or place a mosquito net over the baby carriage). Follow label directions. 6.) Spraying to kill adult mosquitoes is the least effective means of controlling mosquito populations, and should not be relied upon completely for control. Reducing breeding sites and larvaciding is essential for a complete mosquito control program. Page 80 of 125 OTHER There is no flow chart or guidelines sheet for the situation at hand. Is there an immediate threat to someone’s life? YES Tell the caller to hang up and dial 911 or go to the emergency department. NO Fill out an Information Request Form. Consult with your supervisor regarding whether or not to contact the District EC, EPI, or ENV On-Call Representative immediately, or whether to fax the report. If needed, the State EPI On-Call can provide guidance (404-657-2588 during working hours, 770-578-4104 after hours). Use good judgment—if the issue is one of public safety or environmental hazard, call public health! Page 81 of 125 SCHOOL / DAYCARE ISSUE “When can a child return to school or daycare after having an illness?” Fill out an Information Request Form and supplemental Infectious Disease Form. Consult Common Infectious Illnesses poster to answer the caller’s questions. Follow Infectious Disease flow chart for how to report to public health (whether to call or fax report). Page 82 of 125 SWIMMING POOL FECAL INCIDENT Fill out an Information Request Form. Ask: Is it a public or private pool? Private Public FAX the Information Request Form to the District ENV OnCall Representative. Ask: Is it diarrhea or unknown type? Yes Call the District ENV On-Call Representative for the district where the pool is located. Follow Fecal Incident Chart to answer questions about cleaning the pool. Page 83 of 125 No FAX the Information Request Form to the District ENV On-Call Representative. FECAL INCIDENT Log Fecal Incident by recording date, time, observations and chlorine level at time of event. Document actions taken and applicable chemical parameters used. CLOSE POOL NO YES DIARRHEA? CLOSE POOL, CALL HEALTH DEPARTMENT or unknown type YES REMOVE ALL VISIBLE FECAL MATTER CHECK CHLORINE LEVELS *CHLORINE LEVEL 2 PPM OR HIGHER? REMOVE ALL VISIBLE FECAL MATTER FROM POOL DRAIN POOL YES RUN SYSTEM FOR 30 MINUTES HOURS CLEAN SKIMMERS, GUTTERS AND STRAINERS BACKWASH OR CLEAN FILTERS NO REMOVE ALL VISIBLE FECAL MATTER NO RAISE CHLORINE LEVEL TO 2 PPM OR HIGHER RUN SYSTEM FOR 30 MINUTES MINIMUM BRUSH POOL SURFACE'S WITH 100 PPM CHLORINE SANITIZING SOLUTION RINSE AND THEN FILL POOL ADJUST TOTAL ALKALINITY, CORRECT pH, 7.2 - 7.5, *INCREASE CHLORINE TO 2 PPM RUN SYSTEM FOR 30 MINUTES OPEN POOL BACKWASH, CLEAN OR REPLACE FILTERS Georgia Environmental Health (2004) POOL DRAINABLE? (SPA or WADING) RAISE CHLORINE TO 20 PPM MINIMUM BRUSH SIDES, BOTTOM, AND DECK IF CONTAMINATED, WITH 100 PPM CHLORINE RUN SYSTEM 8 HOURS AND UNTIL CHLORINE HAS REACHED ALLOWABLE LEVELS CLEAN SKIMMERS, GUTTERS AND STRAINERS BACKWASH, CLEAN OR REPLACE FILTERS OPEN POOL Note: Maintain pH, between 7.2- 7.5. *If stablizer is used raise chlorine level to 3 ppm. Page 84 of 125 OPEN POOL RECORDS REQUESTS “I need a copy of a birth or death certificate, or a copy of my immunization record.” Fill out an Information Request Form. What records is the caller requesting? Birth or Death Certificate Immunization Records Birth certificates must be requested from the state Vital Records Office by mail, online, phone, or in person. OR they can be requested from the county vital records office. All the information about ordering birth certificates can be found at http://www.health.state.ga.us/programs/vita lrecords/birth.asp, including a link to the county vital records office listing with addresses and phone numbers of county offices. If someone calls to request a birth certificate, please give him/her this link. If they do not have internet access, use this website to answer their questions and look up the phone number for the vital records office in their county. Do NOT just refer them to their county health department, as in most cases it's not the health department that deals with issuing birth certificates. Death certificate information is at http://www.health.state.ga.us/programs/vital records/death.asp and the same guidelines apply. There are several options you may choose from in searching for your record: (1) There may be a record of your immunizations in GRITS, the Georgia Registry of Immunization Transactions and Services. The registry is not all-inclusive or comprehensive but may be helpful. To request this information, call 1-888-223-8644; FAX your request to 404-657-7496; or send an email to immreg@dhr.state.ga.us. (2) Contact the health care provider who administered your last immunizations and request your record from them. (3) Call the last school you attended to see if they still have your immunization certificate on file. (4) If you had your immunizations administered in a public health clinic in Georgia, contact the County Health Department in the county the clinic was located in during normal business hours. NOTE: For other immunization FAQs, visit: http://health.state.ga.us/programs/i mmunization/faq.asp. It is not necessary to fax these Information Requests to the Health District. Page 85 of 125 REFERRAL TO ADVICE NURSE “I have a question about some symptoms I’m having and need some advice.” Fill out an Information Request Form. Are the symptoms severe or life-threatening? YES NO Instruct the caller to call 911 or go to the emergency room immediately. Advise caller to call the Health Department during business hours or call the Advice Nurse at FAX report to District EPI On-Call Representative. Use the district of the patient’s residence. It is not necessary to fax the Information Request Form to the District. Page 86 of 125 RESTAURANT COMPLAINTS Fill out an Information Request Form Anything having to do with power outages, floods, sewage failures, water outages, or fires Any other complaint FAX to the District ENV On-Call Representative. Use the county where the restaurant is located. Contact the District ENV On-Call Representative immediately. Use the county where the restaurant is located. Page 87 of 125 SEWAGE COMPLAINTS Fill out an Information Request Form Any other sewage complaint, including sewage on the ground or running into a creek Sewage backing up into a restaurant Contact the District ENV On-Call Representative immediately. Use the county where the restaurant is located. What is the SOURCE of the sewage discharge? Public sewer line discharge Contact the Georgia Environmental Protection Division emergency hotline at 404-656-4863 or 1-800-241-4113 (24 hours a day, 7 days a week). Septic tank discharge or unknown source of discharge FAX the notification to the District ENV On-Call Representative. Use the county where the property is located. Page 88 of 125 UNHYGIENIC TOURIST ACCOMMODATIONS “The hotel I stayed in last night was filthy and had rats and roaches.” Fill out an Information Request Form. FAX to the District ENV On-Call Representative. Use the county where the reported unhygienic accommodation is located. Page 89 of 125 COMMON MISTAKES AND HOW TO AVOID THEM NEVER tell a healthcare provider/1-866-PUB-HLTH caller to call the health department in the morning to report the disease/situation. It’s YOUR job to do the reporting. You do this by either calling the district, or by faxing the report to the district, depending on the disease. Do NOT fax anything to Laurel Garrison for follow up. Faxes should always go to the District. If there is a particular case that went wrong that you want to draw my attention to, fax or e-mail me, but his is not a reliable way to get a message to a doctor or someone at the state or district office. These should only be in reference to procedural issues. For example, you should NOT e-mail me to let me know that Dr. Fixit is trying to get in touch with someone at the District Health Department. If Dr. Fixit is trying to get in touch with someone at the Health Department, you should CALL the District EPI On-Call Representative. An example of something you SHOULD e-mail me about is if you don’t have a flow chart for something and would like to have one in the future, or if you would like clarification on how to handle something (non-urgent). The District On-Call Representative is your first person to contact. If you are unsure of whether to call him/her, consult with your supervisor. If your supervisor is unsure, contact the STATE EPI On-Call to ask if you need to contact the district. You should never call the State On-Call Representative without also calling the District (for example, a bioterrorism situation). For pager notifications, wait 15 minutes for a response. If no response, go to the next phone number listed on the contact list. Don’t forget you’ve paged the person! If they don’t call you back you haven’t made your notification. Try another number or another person until you talk to a LIVE person. NEVER leave a message when you are making a notification. If you get an answering machine, hang up and try the next number or next person on the list. NEVER give the phone number of the public health (either State or District) employee to the caller directly. It’s YOUR job to make the notification for them. EXCEPTION: when someone in public health is calling to get a phone number (ex: a District Epi is calling to get the number for another District Epi or the State Epi is calling to get the number for a District Epi). Always fax a report to the district for anything concerning follow up the district needs to do (ex: caller reports mold in home). Examples of calls you do NOT need to fax a report on include: making appointments, seeking monetary assistance, birth certificates, and immunization records. These are not emergencies and people need to call the health department on their own during normal business hours. For EC or EPI Infectious Diseases, you should ALSO fax the report after you contact someone and talk to a LIVE person. Page 90 of 125 Not all animal bite calls should be referred to the Poison Center. In all cases, take a report. If the caller has questions regarding testing the animal, putting the person on prophylaxis, etc. then you can transfer them to the Poison Center. Human rabies is NOT equal to animal rabies and animal bite calls. Human rabies (suspect or confirmed) is an EMERGENCY. Even if you get calls regarding specimen coordination with the lab, treat human rabies testing, suspect, or confirmed cases as an IMMEDIATE notification of the district. For calls that come in during normal business hours, document these well. Make sure to write down enough information so that the District can understand that the call came in when the health department was supposed to be open. FAX the report to the district, so they know that they are missing these calls during the day. The district NEEDS TO KNOW if people aren’t able to reach them during the day. Example: “Caller wants to make an appointment. She tried calling the Hart county health department a few minutes ago (about 10:15am) and got a recording with our number on it so she called us. I told her that the HD should be open right now according to their hours of operation and to try back in a few minutes.” Use “1-866-PUB-HLTH” to refer ONLY to healthcare provider, lab, public health, emergency responder, etc. General public calls should not have this phrase anywhere in the record. This is a signal to me about what kind of call it is and these are treated differently than those from the general public. Page 91 of 125 ADDITIONAL RESOURCES Page 92 of 125 Alphabetical Listing of Georgia Counties and the Districts in which they belong COUNTY HEALTH DISTRICT DISTRICT NUMBER Appling Waycross--Southeast HD 9-2 Atkinson Waycross--Southeast HD 9-2 Bacon Waycross--Southeast HD 9-2 Baker Albany--Southwest HD 8-2 Baldwin Macon--North Central HD 5-2 Banks Gainesville--North HD 2-0 Barrow Athens--Northeast HD 10-0 Bartow Rome--Northwest HD 1-1 Ben Hill Valdosta--South HD 8-1 Berrien Valdosta--South HD 8-1 Bibb Macon--North Central HD 5-2 Bleckley Dublin--South Central HD 5-1 Brantley Waycross--Southeast HD 9-2 Brooks Valdosta--South HD 8-1 Bryan Coastal HD 9-1 Bulloch Waycross--Southeast HD 9-2 Burke Augusta--East Central HD 6-0 Butts LaGrange--LaGrange HD 4-0 Calhoun Albany--Southwest HD 8-2 Camden Coastal HD 9-1 Candler Waycross--Southeast HD 9-2 Carroll LaGrange--LaGrange HD 4-0 Catoosa Rome--Northwest HD 1-1 Charlton Waycross--Southeast HD 9-2 Chatham Coastal HD 9-1 Chattahoochee Columbus--West Central HD 7-0 Chattooga Rome--Northwest HD 1-1 Cherokee Dalton--North Georgia HD 1-2 Clarke Athens--Northeast HD 10-0 Clay Columbus--West Central HD 7-0 Clayton Morrow -- Clayton County HD 3-3 Clinch Waycross--Southeast HD 9-2 Cobb Marietta--Cobb/Douglas HD 3-1 Coffee Waycross--Southeast HD 9-2 Colquitt Albany--Southwest HD 8-2 Columbia Augusta--East Central HD 6-0 Cook Valdosta--South HD 8-1 Coweta LaGrange--LaGrange HD 4-0 Crawford Macon--North Central HD 5-2 Crisp Columbus--West Central HD 7-0 Dade Rome--Northwest HD 1-1 Page 93 of 125 Dawson Decatur DeKalb Dodge Dooly Dougherty Douglas Early Echols Effingham Elbert Emanuel Evans Fannin Fayette Floyd Forsyth Franklin Fulton Gilmer Glascock Glynn Gordon Grady Greene Gwinnett Habersham Hall Hancock Haralson Harris Hart Heard Henry Houston Irwin Jackson Jasper Jeff Davis Jefferson Jenkins Johnson Jones Gainesville--North HD Albany--Southwest HD Decatur--DeKalb HD Dublin--South Central HD Columbus--West Central HD Albany--Southwest HD Marietta--Cobb/Douglas HD Albany--Southwest HD Valdosta--South HD Coastal HD Athens--Northeast HD Augusta--East Central HD Waycross--Southeast HD Dalton--North Georgia HD LaGrange--LaGrange HD Rome--Northwest HD Gainesville--North HD Gainesville--North HD Atlanta--Fulton HD Dalton--North Georgia HD Augusta--East Central HD Coastal HD Rome--Northwest HD Albany--Southwest HD Athens--Northeast HD Lawrenceville--East Metro HD Gainesville--North HD Gainesville--North HD Macon--North Central HD Rome--Northwest HD Columbus--West Central HD Gainesville--North HD LaGrange--LaGrange HD LaGrange--LaGrange HD Macon--North Central HD Valdosta--South HD Athens--Northeast HD Macon--North Central HD Waycross--Southeast HD Augusta--East Central HD Augusta--East Central HD Dublin--South Central HD Macon--North Central HD Page 94 of 125 2-0 8-2 3-5 5-1 7-0 8-2 3-1 8-2 8-1 9-1 10-0 6-0 9-2 1-2 4-0 1-1 2-0 2-0 3-2 1-2 6-0 9-1 1-1 8-2 10-0 3-4 2-0 2-0 5-2 1-1 7-0 2-0 4-0 4-0 5-2 8-1 10-0 5-2 9-2 6-0 6-0 5-1 5-2 Lamar Lanier Laurens Lee Liberty Lincoln Long Lowndes Lumpkin Macon Madison Marion McDuffie McIntosh Meriwether Miller Mitchell Monroe Montgomery Morgan Murray Muscogee Newton Oconee Oglethorpe Paulding Peach Pickens Pierce Pike Polk Pulaski Putnam Quitman Rabun Randolph Richmond Rockdale Schley Screven Seminole Spalding Stephens LaGrange--LaGrange HD Valdosta--South HD Dublin--South Central HD Albany--Southwest HD Coastal HD Augusta--East Central HD Coastal HD Valdosta--South HD Gainesville--North HD Columbus--West Central HD Athens--Northeast HD Columbus--West Central HD Augusta--East Central HD Coastal HD LaGrange--LaGrange HD Albany--Southwest HD Albany--Southwest HD Macon--North Central HD Dublin--South Central HD Athens--Northeast HD Dalton--North Georgia HD Columbus--West Central HD Lawrenceville--East Metro HD Athens--Northeast HD Athens--Northeast HD Rome--Northwest HD Macon--North Central HD Dalton--North Georgia HD Waycross--Southeast HD LaGrange--LaGrange HD Rome--Northwest HD Dublin--South Central HD Macon--North Central HD Columbus--West Central HD Gainesville--North HD Columbus--West Central HD Augusta--East Central HD Lawrenceville--East Metro HD Columbus--West Central HD Augusta--East Central HD Albany--Southwest HD LaGrange--LaGrange HD Gainesville--North HD Page 95 of 125 4-0 8-1 5-1 8-2 9-1 6-0 9-1 8-1 2-0 7-0 10-0 7-0 6-0 9-1 4-0 8-2 8-2 5-2 5-1 10-0 1-2 7-0 3-4 10-0 10-0 1-1 5-2 1-2 9-2 4-0 1-1 5-1 5-2 7-0 2-0 7-0 6-0 3-4 7-0 6-0 8-2 4-0 2-0 Stewart Sumter Talbot Taliaferro Tattnall Taylor Telfair Terrell Thomas Tift Toombs Towns Treutlen Troup Turner Twiggs Union Upson Walker Walton Ware Warren Washington Wayne Webster Wheeler White Whitfield Wilcox Wilkes Wilkinson Worth Columbus--West Central HD Columbus--West Central HD Columbus--West Central HD Augusta--East Central HD Waycross--Southeast HD Columbus--West Central HD Dublin--South Central HD Albany--Southwest HD Albany--Southwest HD Valdosta--South HD Waycross--Southeast HD Gainesville--North HD Dublin--South Central HD LaGrange--LaGrange HD Valdosta--South HD Macon--North Central HD Gainesville--North HD LaGrange--LaGrange HD Rome--Northwest HD Athens--Northeast HD Waycross--Southeast HD Augusta--East Central HD Macon--North Central HD Waycross--Southeast HD Columbus--West Central HD Dublin--South Central HD Gainesville--North HD Dalton--North Georgia HD Dublin--South Central HD Augusta--East Central HD Macon--North Central HD Albany--Southwest HD Page 96 of 125 7-0 7-0 7-0 6-0 9-2 7-0 5-1 8-2 8-2 8-1 9-2 2-0 5-1 4-0 8-1 5-2 2-0 4-0 1-1 10-0 9-2 6-0 5-2 9-2 7-0 5-1 2-0 1-2 5-1 6-0 5-2 8-2 County & District Hours of Operation (created March 2006) County Facility Appling Appling County HD Atkinson Atkinson County HD Bacon Bacon County HD Baker Baker County HD Baldwin Baldwin County HD Banks Banks County HD Barrow Barrow County HD Bartow Bartow County HD Ben Hill Ben Hill County HD Berrien Berrien County HD Bibb Bibb County HD Bibb Department of Family & Children Services Clinic Bibb Felton Homes Clinic Bibb Teen Parent Center Clinic Bleckley Bleckley County HD A-1-97 Phone Number (912) 3674601 (912) 4223332 (912) 6324712 (229) 7345226 (478) 4454264 (706) 6772296 (770) 3073011 (770) 3821920 (229) 4265288 (229) 6865411 (478) 7450411 (478) 7451333 (478) 7435893 (478) 7521887 (478) 9346590 Hours of Operation M-F: 8-5 M-F: 8-5 M-F: 8-5 M-F: 8-5 M, W, Th, F: 8-4:30, Tu: 8-6 M-F: 8-5, closed 12-1 M: 8-7, Tu, W, Th: 8-5, F: 8-2 M-W: 7:30-5, Th: 8-7, F: 8-2 M-F: 8-5 M-F: 8-5 M-F: 8-4:30 M-F: 8-4:30 M-F: 8-4:30 M-W: 8-5, Th: 8-6:30, F: 8-12:30 Brantley Brantley County HD Brooks Brooks County HD Bryan Bryan County HD Bryan Richmond Hill Clinic Bulloch Bulloch County HD Burke Burke County HD Burke Burke County HD (Sardis) Butts Butts County HD Calhoun Calhoun County HD Camden Camden County HD (Kingsland) Camden Camden County HD (St. Mary's) Camden Camden County HD (Woodbine) Candler Candler County HD Carroll Carroll County HD (Carrollton) Carroll Carroll County HD (Villa Rica) Catoosa Catoosa County HD Charlton Charlton County HD Chatham Chatham County HD Chattahoochee Chattahoochee County HD Chattooga Chattooga County HD Cherokee Cherokee County HD (Canton) Cherokee Cherokee County HD (Woodstock) Clarke Clarke County HD A-1-98 (912) 4626165 (229) 2637585 (912) 6534331 (912) 7562611 (912) 7643800 (706) 5543456 (478) 5694949 (770) 5042230 (229) 8492515 (912) 7294554 (912) 8828515 (912) 5763040 (912) 6855765 (770) 8366667 (770) 4590031 (706) 9352366 (912) 4962561 (912) 3562441 (706) 9893663 (706) 8573471 (770) 3457371 (770) 9280133 (706) 542- M-F: 8-5 M-F: 8-5 M, W, Th: 8-5, Tu: 8-6, F: 8-4 M, W, Th: 8-5, Tu: 8-6, F: 8-4, so M-F: 8-5 M-F: 8-4:30, closed 12-1 Only open 2x a month M-F: 8-5 M-F: 8-5 M-F: 8-5 M-F: 8-5 Closed Temporarily M-F: 8-5 M-F: 8-5 Tu & W: 8-4:15, F: 8-11:15, M&T M-W: 8-5, Th: 8-7, F: 8-2 M-F: 8-5 M-F: 8-5 M-F: 8-4:30 M-W: 7:30-5, Th: 8-6:30, F: 8-2 M-F: 8-5 M-F: 8-5 M, W, Th: 8-5, Tu: 8-7, F: 8-2 Clarke East Athens Clinic Clarke Teen Matters Clay Clay County HD Clayton Clayton County HD Clayton Forest Park Health Center Clayton Jonesboro Health Center Clayton Tara Health Center Clinch Clinch County HD Cobb Acworth Public Health Center A-1-99 8600 (706) 3695816 (706) 3695670 (229) 7682355 (678) 6107199 (404) 3666231 (770) 4718635 (770) 4736024 (912) 4872199 (770) 9743330 M, W, Th: 8:30-5, Tu: 8:30-7, F: 8 M, W, Th: 8:30-5:30, Tu: 8:30-7:3 M-F: 8-4:30 M-F: 8:30-5 Location moved to 1 Jonesboro Location closed: Moved to Clay Battle Creek Rd, Jonesboro Ph# M, Th: 9:30-6, T, W, F: 8:30-5 Location closed: Moved to Clay Battle Creek Rd, Jonesboro Ph# M-F: 8-5 M-F: 8-5 Cobb Cobb Cobb Cobb Cobb Coffee Colquitt Columbia Columbia Columbia Cook Coweta Crawford Crisp Dade Dawson Decatur DeKalb Dodge Dooly Dougherty Douglas Early (770) 5142300 (678) 784East Cobb Public Health Center 2180 (770) 919Roosevelt Circle 0025 (770) 438Smyrna Public Health Center 5105 (678) 385South Cobb 1362 (912) 389Coffee County HD 4450 (229) 891Colquitt County HD 7100 (706) 541Columbia County HD 1318 (706) 556Columbia County HD (Grovetown Clinic) 3727 Columbia County HD (Martinez-Evans (706) 868Clinic) 3330 (229) 896Cook County HD 3030 (770) 254Coweta County HD 7400 (478) 836Crawford County HD 3167 (229) 276Crisp County HD 2680 (706) 657Dade County HD 4213 (706)-265Dawson County HD 2611 (229) 248Decatur County HD 3055 (404) 294DeKalb County HD 3700 (478) 374Dodge County HD 5576 (229) 268Dooly County HD 4725 (229) 430Dougherty County HD 6200 (770) 949Douglas County HD 1970 Early County HD (229) 723Cobb County HD A-1-100 M-F: 8-5 M-F: 8-4 M-Th: 8-5, F: 8-12, closed Th 1-2 M-F: 8-5 M-F: 8-4 M-F: 8-5 M-Th: 7:30-6, F: 8-4:30 M-F: 8-5 M-F: 8-5 M-F: 8-5 M-F: 8-5 M-F: 8-4:30 M-F: 8-4:30 M-F: 8-5 M-W: 8-5, Th: 8-6:30, F: 8-2 M-F: 8-5, closed 12-1 M-F: 7:30-6 M-F: 8:15-5 M, W, Th: 8-5, Tu: 8-7, F: 8-12 M-F: 7:30-6:00, closed Thursday M-F: 8-5 M-F: 8-4:30 M-F: 8-5 Echols Echols County HD Effingham Effingham County HD Elbert Elbert County HD Emanuel Adrian Clinic Emanuel Emanuel County HD Emanuel Twin City Clinic Evans Evans County HD Fannin Fannin County HD Fayette Fayette County HD 3707 (229) 5595103 (912) 7546484 (706) 2833775 (478) 6683436 (478) 2377501 (478) 7633452 (912) 7392088 (706) 6323023 (770) 4611178 A-1-101 M-F: 8-5 M-F: 8-5 M: 8-6:30, Tu, W, Th: 8-4, F: 8-1 W: 8:30-4, closed M, Tu, Th, F ex 8:30-4 M, W, Th: 8-4:30, Tu: 8-6:30, F: 8 M, W, Th: 8-4:30, Tu: 8-6:30, F: 8 M-F: 8-5 M-F: 8-5, closed 12-1 M-F: 8:30-5 Floyd Floyd County HD Floyd Floyd County HD Satellite Office Floyd Floyd County Teen Resource Center Forsyth Forsyth County HD Franklin Franklin County HD Fulton Adamsville Health Center Fulton Aldredge Health Center Fulton Center Hill Health Center Fulton Fairburn Health Center WIC Office Fulton Hapeville Health Center WIC Office Fulton Infant WIC Program Fulton Lakewood Health Center Fulton Lindbergh Women’s & Children’s Health Center Fulton Maternal WIC Program Fulton Neighborhood Union Health Center Main Desk (706) 2956123 (706) 8025409 (706) 8025372 (770) 7816900 A-1-102 (706) 3845575 (404) 6994204 (404) 7301448 (404) 6996370 (770) 3063119 (404) 7624027 (404) 6165190 (404) 6240628 (404) 6166999 (404) 6164621 (404) 7304665 M-W: 8-5, Th: 8-6:30, F: 8-2 M-W: 8-5, Th: 8-6:30, F: 8-2, clos M, W, Th: 9-6, Tu: 9-5, F: 9-4, Sat M-F: 8-4, closed 11-1, Exception: month clinic closes at 7pm. Exce month, clinic closes at noon. M-F: 8-5, closed 12-1, 1st Thursd until 7 pm. Friday following 1st M-F: 8-5 M: 8-7, Tu-F: 8-5 M-F: 8:30-5 M-F: 8:30-5 M-F: 8:30-5 M-F: 8-4:30 M-F: 8-5 M-F: 8-5 M-F: 8-4:30 M-F: 8:30-4 Fulton Neighborhood Union Health Center WIC Office Fulton North Fulton Health Center (dental care) Fulton Northeast Health Center Main Number Fulton Pediatric WIC Program Fulton Ponce Medical Center WIC Office Fulton Roy McGee Health Clinic Fulton Sandy Springs Health Center Fulton South Fulton Health Center WIC Office Fulton Southside Healthcare, Inc Fulton West End Medical Center (Bowen Homes) Fulton West Lake Medical Center Fulton Willie J. Freeman College Park Regional Health Center Gilmer Gilmer County HD Glascock Glascock County HD Glynn Glynn County HD A-1-103 (404) 7308314 (770) 7402403 (404) 7305835 (404) 6168549 (404) 6169836 (404) 7528753 (404) 3036162 (404) 7305408 (404) 6881350 (404) 7990851 (404) 7521400 (404) 7654146 (706) 6354363 (706) 5982061 (912) 2643961 M-F: 8:30-5 M, Tu, W, F: 9-5, Th: 9-7 M-F: 8:30-5, 2nd Tuesday of eac M-F: 7:30-4 M-F: 8-4:30, this number is for p referred to the WIC Office by Gr any other services. Temporarily Closed but there m Neighborhood Union Health Cen M-F: 8:30-5 M-F: 8:30-5 M: 8am-8:30pm, Tu-F: 8-5 M-Th: 8-5, F: 8-12 M-F: 8-5 M, W, F: 8-5, Tu, Th: 8-7, Open 2 M-F: 8-5, closed 12-1 M-F: 8-5 M-W & F: 8-5, Th: 8-7 Gordon Gordon County HD Grady Grady County HD Greene Greene County HD Gwinnett Buford Health Center Gwinnett Lawrenceville Health Center Gwinnett Norcross Health Center Habersham Habersham County HD Hall Hall County HD Hancock Hancock County HD Haralson Haralson County HD Harris Harris County HD Hart Hart County HD Heard Heard County HD Henry Henry County HD (McDonough) Henry Henry County HD (Stockbridge) (706) 6241444 (229) 3772992 (706) 4537561 (770) 6142401 (770) 3394283 (770) 6385700 (706) 7787156 (770) 5315600 (706) 4446616 (770) 6465541 (706) 6285037 (706) 3765117 A-1-104 (706) 6753456 (770) 9542250 (770) 3897887 M-W: 8-5, Th: 8-6:30, F: 8-2 M-F: 8-5 M, Tu, Th: 8-4, W: 8-6:30, F: 8-1 M-F: 8-5, Sat: 8-12 M-F: 8-4:15, Sat: 8-11:15 M-F: 8-5, Sat: 8-12 M, W, Th: 8-5, Tu: 8-7, F: 8-3, clo M, W, Th: 8-5, Tu: 8-7, F: 8-3, clo Wednesday of each month open M-F: 8-4:30 M-W: 8-5, Th: 8-7, F: 8-2 M: 7-6. Tu-Th: 8-5, F: 8-3 M-F: 8-5, closed 12-1, 1st Tuesda closes at 7pm. Friday after the 1 3 pm. M-F: 8-5, closed 12-1 M-F: 8-5 M-F: 8-5, closed 12-1 Houston Houston County HD (Perry) Houston Houston County HD (Warner Robins) Irwin Irwin County HD Jackson Jackson County HD (Commerce) Jackson Jackson County HD (Jefferson) Jasper Jasper County HD Jeff Davis Jeff Davis County HD Jefferson Jefferson County HD Jenkins Jenkins County HD Johnson Johnson County HD Lamar Lamar County HD Laurens Laurens County HD Lee Lee County HD Liberty Liberty County HD Lincoln Lincoln County HD Long Long County HD Lowndes Hahira Clinic Lowndes Lowndes County HD Lowndes Lake Park Lowndes Teen Clinic Lumpkin Lumpkin County HD Macon Macon County HD Madison Madison County HD A-1-105 (478) 9871717 (478) 2182000 (229) 4685003 (706) 3353895 (706) 3675204 (706) 4686850 (912) 3752425 (478) 6253716 (478) 9822811 (478) 8643542 (770) 3581483 (478) 2722051 (229) 7593014 (912) 8762173 (706) 3593154 (912) 5452107 (229) 7942665 (229) 3335257 (229) 5596470 (229) 2457274 (706) 8672727 (478) 4728121 (706) 795- M-F: 8-4, closed 12-12:30 M-F: 8:30-3:30 M-F: 8-4 M, W, Th: 8-4, Tu: 8-6:30, F: 8-1 M, W, Th: 8-4:30, T: 8-7, F: 8-1:30 M-F: 8-4:30 M-F: 8-5 M, Tu, Th: 8-4:30, W: 8-6:30, F: 8 M-F: 8-5 M: 8-7, Tu-Th: 8-5, F: 8-12 M-F: 8:30-5, closed 12-1 M, W, Th: 8:15-5, Tu: 8:15-7, F: 8 M: 9-5, Tu-F: 8-5 M, Tu, F: 8-5, W: 9:30-5, Th: 8-3 M-F: 8-4:30 M-F: 8-5 M-F: 8-4:30 M, Tu, W, F: 8-5, Th: 8am-8pm M-F: 8-4:30, closed 12-12:30 M-F: 8-6:30, sometimes closed 1M-F: 8-5, closed 12-1, Thursday clinic opens at 10am. M-F: 8-4:30 M: 8-6:30, Tu, W, Th: 8-4, F: 8-1 Marion Marion County HD McDuffie McDuffie County HD McIntosh McIntosh County HD Meriwether Meriwether County HD (Greenville) Meriwether Meriwether County HD (Manchester) Miller Miller County HD Mitchell Mitchell County HD Monroe Monroe County HD Montgomery Montgomery County HD A-1-106 2131 (229) 6495664 (706) 5951740 (912) 4374561 (706) 6724974 (706) 8463353 (229) 7583344 (229) 3362055 (478) 9925083 (912) 5834602 M-F: 8-5 M-F: 8-5 M-F: 8-5 M-F: 8-5 M-Th: 8:30-5, closed 12-1 daily an M-F: 8-5 M-F: 8-5 M-F: 8:30-3:30 M, W, Th: 8-5, Tu: 8-7, F: 8-12 Morgan Morgan County HD Murray Murray County HD Muscogee Muscogee County HD Muscogee SHAPP/Hypertension Muscogee STD Clinic Muscogee Teen Health Services Muscogee Tuberculosis Clinic Muscogee WIC Services: Columbus Muscogee WIC Services: Fort Benning Muscogee Women's Health Services Newton Newton County HD Oconee Oconee County HD Oglethorpe Oglethorpe County HD Paulding Paulding County HD Peach Peach County HD (Byron Clinic) Peach Peach County HD (Fort Valley) Pickens Pickens County HD Pierce Pierce County HD Pike Pike County HD Polk Rockmart HD Polk Polk County HD Pulaski Pulaski County HD Putnam Putnam County HD A-1-107 (706) 7521266 (706) 6954585 (706) 3216300 (706) 3216241 (706) 3216240 (706) 3210619 (706) –3216636 (706) 3216205 (706) 6826280 (706) 3216225 (770) 7869086 (706) 7693983 (706) 7438181 (770) 4437881 (478) 9567679 (478) 8256939 (706) 2532821 (912) 4492032 (770) 5678972 (770) 6841385 (770) 7492270 (478) 7831361 (706) 485- M, W, Th: 8:30-5, Tu: 8:30-7, F: 8 M&W: 8-5, Tu&Th: 8-7, F: 8-12 M-F: 8-5 M-F: 8-4 M-F: 8-4 M-F: 8-6 M-F: 8-4:30 M-F 8-5 M-F: 8-5 M-F: 8-5 M, Th: 8-7, Tu, W, F: 8-5 M, W, Th: 8-4:30, T: 8-6:30, F: 8-1 M: 8-6:30, Tu, W, Th: 8-4, F: 8-1 M-W: 8-5, Th: 8-7, F: 8-2 Tu-F: 8-4:30, closed Monday M-F: 8-4:30 M-F: 8-5 M-Th: 7:30-6:30, F: 8-5 M-F: 8-5, closed 12-1 M-W: 8-4:30, Th: 8-6:30, F: 8-2 M-W: 8-5, Th: 8-6:30, F: 8-2 M, W, Th: 7-5:30, Tu: 7-6:30, F: 7 M-F: 8-4:30 Quitman Quitman County HD Rabun Rabun County HD Randolph Randolph County HD Richmond Fort Gordon WIC Clinic Richmond Richmond County HD Richmond South Augusta Clinic Rockdale Rockdale County HD Schley Schley County HD Screven Screven County HD 8591 (229) 3343697 (706) 2120289 (229) 7322414 (706) 7215800 (706) 7215800 (706) 7900661 (770) 7855936 (229) 9372208 (912) 5642190 A-1-108 M-F: 8-5, closed 12-1 M, W, Th: 8-5, Tu: 8-7, F: 8-3, clo M-F: 8-4, closed 12-1 Located at the main Richmond C M-F: 8-5 M-W: 8-5, Th: 8-7:30, F: 8-12:30 M, W, F: 8-5, Tu, Th: 8-7 M-F: 8-5, closed 12-1 M-F: 8-4 (229) 5242577 (770) 4674740 Seminole Seminole County HD Spalding Spalding County HD Stephens Stephens County HD Stewart Stewart County HD Sumter Sumter County HD Talbot Talbot County HD Taliaferro Taliaferro County HD Tattnall Tattnall County HD (Glennville) Tattnall Tattnall County HD (Reidsville) Taylor Taylor County HD Telfair Telfair County HD Terrell Terrell County HD Thomas Thomas County HD Tift Tift County HD Toombs Toombs County HD (706) 2824507 A-1-109 (229) 8384859 (229) 9243637 (706) 6658561 (706) 4562316 (912) 6545290 (912) 5577850 (478) 8625628 (229) 8687404 (229) 9958435 (229) 2264241 (229) 3868373 (912) 5268108 M-F: 8-5 M-F: 8:30-4:30 M-Th: 8-5, F: 8-3, closed 12-1. 1 close at 7 pm. Friday following 1 pm. M-F: 8-5 M, Tu, Th: 7-5:30, W: 7-3:30, F: 8 M-F: 8-5 M-F: 8-4:30 M-F: 8-5 M-F: 8-5 M-F: 8-4:30, closed 12-12:30 M, Tu, W: 8-5, Th: 8-6:30, F: 8-12 M-F: 8-5 M-Th: 7:30-5, F: 7:30-4:30 M-F: 8-5 M-F: 8-5 Towns Towns County HD Treutlen Treutlen County HD Troup Hogansville Health Center Troup Troup County HD Troup West Point Health Center Turner Turner County HD Twiggs Twiggs County HD Union Union County HD Upson Upson County HD Walker Walker County HD (Lafayette) Walker Walker County HD (Rock Springs) Walton Adolescent Center for Education and Services Walton Walton County HD Walton West Walton County HD Ware Ware County HD Warren Warren County HD Washington Washington County HD Wayne Wayne County HD Webster Webster County HD Wheeler Wheeler County HD White White County HD Whitfield Whitfield County HD Children's Health Whitfield Whitfield County HD Medical Access A-1-110 (706) 8962265 (912) 5294217 (706) 6374834 (706) 8454085 (706) 6431111 (229)5674357 (478) 9453351 (706) 7456292 (706) 6477149 (706) 6385577 (706) 3750775 (770) 2074151 (770) 2074125 (770) 4661789 (912) 2831875 (706) 4652252 (478) 5523210 (912) 4272042 (229) 8283225 (912) 5687161 (706) 8652191 (706) 2262621 (706)-226- M, W, Th: 8-5, Tu: 8-7, F: 8-3, clo M, W, Th: 8-5, Tu: 8-7, F: 8-1 T: 8-5, W: 8-4, F: sometimes M-F: 8-4:30 M, Tu, Th:8-5, closed 12-1, closed M-F: 8-5 M-F: 8-4:30 M-F: 7:30-6, closed 12-12:30 M-F: 8-5 M-W, 7:30-4, Th: 8-5:30, F:8-1 M: 8-2, Tu-Th: 8-3, closed Friday M-Th: 8-5, F: 8-2, closed 11:30-12 M: 8-6:30, Tu, W, Th: 8-4:30, F: 8 M-Th: 8:30-7, closed Friday M-F: 8-5 M, Th: 8-4:30. Tu, 8-6:30, W:8-5, M-F: 8-5 M, Tu, Th, F: 8-5, W: 9-5 M-F: 8-5, closed 12-1 M, Tu, Th: 8-5, W: 8-7, F: 8-12 M-W: 8-5, Th: 8-7, F: 8-3, closed 1 M&W: 8-4, Tu&Th: 8-6, F: 8-1 M&W: 8-5, Tu&Th: 8-7, F: 8-2 Clinic Whitfield Whitfield County HD Women's Clinic Wilcox Wilcox County HD Wilkes Wilkes County HD Wilkinson Wilkinson County HD (Gordon) Wilkinson Wilkinson County HD (Irwinton) Worth Worth County HD A-1-111 5446 (706)-2812259 (229) 3652310 (706) 6782622 (478) 6285353 (478) 9462226 (229) 7772150 M&W: 8-5, Tu&Th: 8-7, F: 8-2 M, Tu, W: 8-5, Th: 8-6:30, F: 8-12 M, W, Th: 8-4:30, Tu: 8-6:30, F: 8 M-F: 8-4:30 M-F: 8-4:30 M-F: 8-5 DEPARTMENT OF HUMAN RESOURCES Division Of Public Health Emergency Operations Plan Call-Down Exercise Program Standard Operating Plan Support Annex A1, Appendix II I. PURPOSE The purpose of the Call Down Exercise Program is to demonstrate our ability to contact our Division Staff, District Coordinators, and Community Partners when a situation requires a rapid response by public health emergency responders across the State of Georgia. NOTE: For the purpose of continuity and brevity, PHERs will be used throughout this Appendix to signify personnel within the public health community with an emergency response role. II. SCOPE This exercise program will target PHERs at the State, District, and County levels. Exercises should test both horizontal and vertical integration with response partners at the state, district and local levels. Methods used to conduct this exercise will be limited only by the technologies currently available. This exercise program is intended to remain flexible and allow for input from all public health partners. Initially this will be a very simple process of contacting PHERs at the State and District level via one of the communication devices that are recognized in the Communications Plan (pending publication). The program will eventually scale up the complexity of these drills to tests the Division’s ability to respond to any given incident. III. GOAL The end goal is to provide the State Public Health Director with a method of assessing, exercising, and improving the ability of the Division of Public Health to rapidly contact PHERS at all levels upon the happening of a significant event requiring actions by the State’s Public Health Community. IV. OBJECTIVES 1. Test the Viability of the Public Health’s Alert and Notification SOP and Database (SendSS). The Division has developed an Alert and Notification SOP contained within the State of Georgia’s Department of Human Resources Emergency Operations Plan under Support Annex A1. This Support Annex outlines the process for alerting the Division of Public Health A-1-112 Emergency Preparedness Coordinators at the State and District levels. Additionally, DPH has a web based system that contains the contact information for all PHERs. This system allows key personnel to identify who the “On-Call Representative” (OCR) will be on any given day. In the event of a Call-Down drill or a “Real-World” event, the OCR will be the first individual notified and will be responsible for conducting further alerts and notifications based on that office’s/agency’s standard operating procedures and as outline in Support Annex 1. To measure this objective, in terms of the ability to contact the OCRs, a ratio will be determined based on the number of first time contacts divided by the total number of contacts attempted. The expected ratio should be at least 90%. 2. Test the Operability of the Various Communication Assets Throughout the State. The Division uses a wide array of systems to contact PHERs throughout the state. These multiple systems are necessary in that they provide redundant methods, each using a different architecture, in the event one or multiple systems are made or become inoperable. This exercise program gives users at all levels a tool to test each system, allows an assessment to be made of the effectiveness of the system(s), and seek ways to improve the use of current systems or seek new systems which better meet their needs. To measure this objective, a ratio will be determined based on the number of systems that functioned as expected without issue divided by the total number of systems employed during the drill. The expected ratio should be at least 90%. 3. Measure the Division’s Response Times to an Alert. The key objective of this exercise program is to assess the Division’s ability to rapidly respond to a public health emergency. Assuming that SendSS is up to date with the contact information of all PHERs and the systems available to conduct the alert are available and working properly, the Division should be able to respond to any public health related emergency in a short time period. To measure this objective, the time a response is obtained is subtracted from the time at which the alert was initiated. The expected response time is 15 minutes or less. Times will be recorded as follows: (a) 0:01 to 15:00 minutes (b) 15:01 to 30:00 minutes (c) 30:01 or more minutes 4. Exercise the Use of WebEOC. While WebEOC is not a method used to alert key personnel, it is used to track an event (it gives a recorded history of an event). Each individual who has a requirement to access WebEOC must first obtain a password. If there is a requirement to log onto WebEOC during a A-1-113 Call Down, the State Emergency Coordinator (Planning) will make that determination and will establish a link for the specified event. To measure this objective, the number of those who log onto WebEOC will be divided by the total number of those who were expected to access WebEOC. The expected ratio should be at least 90%. V. RESPONSIBILITIES All PHERs must ensure their contact information is updated on the SendSS database. Each department, division, or district lead must also ensure that their OCR is identified daily and updated on SendSS. SendSS will be used to determine who will be alerted during a Call Down exercise or a “Real-World” event. The following is a list of participants which are contacted either monthly or quarterly: (This is not an exhaustive list.) DHEART, CHEART, Regional Coordinating Hospitals, Acute Care Hospitals, Community Health Centers, Other Participating Hospitals, Emergency Preparedness Staff, Emergency Medical Services, Nurse Managers, Environmental Health Managers, SNS Staff, District Health Directors, Medical Reserve Corps, Emergency Management Agencies, Public Information Officer, Fire, School System Liaisons, Pharmacists, Immunization Managers, Epidemiologists, IT Manager The OCR for each agency must be available to answer a call 24 hours a day, 7 days a week, and all reports of public health emergencies must be evaluated and acted on, including initiating coordination between the State, District, County and other local public health partners. The OCR is expected to begin this coordination effort, start recording all communications, and exercising a reporting system within 15 minutes of an alert. The Division’s Office of Emergency Preparedness will establish a calendar of Call Down drills and publish the schedule in conjunction with the Multi-Year Exercise Plan. This Office will also initiate the Call Down drill, unless otherwise stated or a “Real World” event has triggered an alert from outside of the Division. Which would mean that the initiating agency should track the alert and notification process and prepare an after action report for submission to the Division within 10 working days at the end of the event. District ECs will develop their own Call Down calendar and SOP for their respective districts. Their Call Down list should include all PHERs within their district. In addition, they should include all Acute Care Hospitals located within their District boundaries. These calendars should mirror the Division’s calendar to minimize confusion, provide for synchronization during Quarterly Call Downs, and establish continuity of reporting. The exercise planning team will develop the drill schedule for the State as well as the scenarios and systems to be tested. The exercise planning team will consist of the following, at a minimum: State EP Exercise Coordinator A-1-114 State EP Planning Coordinator State EP ASPR Liaison, Training and Exercise Coordinator State EP Communications Officer State EP Field Exercise Coordinator VI. CONCEPT OF THE EXERCISE PROGRAM The Call Down Exercise Program is designed to provide a systematic means of testing, evaluating and improving our alert and notification system within the public health community throughout Georgia. This SOP will prescribe the number of exercises per year, the systems to be tested, objectives of each exercise, and expected deliverables. These exercises will also vary in their degree of complexity based on assessments of past exercises and the anticipated requirements of our public health responders as we move forward. The design of these exercises will range from simply calling a limited number of key PHERs during duty hours on a scheduled basis to notifying all PHERs after hours and requiring the DHR EOC to stand up. A pinnacle exercise will include a statewide alert with an expectation that key personnel will stand up their respective EOCs. This exercise will not occur before 2008 and will be scheduled on a cyclical basis with the frequency to be determined at a later date. NOTE: If an event requires the use of the alert and notification process and an EOC to stand up, then an AAR will be completed to give exercise credit for this requirement. Performance measures as previously indicated will be recorded and then reported to the Office of Emergency Preparedness within 5 days of the drill or event. Feedback forms and AARs will be used to capture agency and systems specific issues. Feedback forms are required to report any issues identified during a drill. AARs will be used only when requested by the Office of Emergency Preparedness but will always be used at the completion of an actual event. 1. Drill Types a. Announced: An announced drill will be listed on the Multi-Year Exercise Plan indicating the Month, day, and time of the initial alert. These will normally be conducted during regular duty hours. b. Unannounced: An unannounced drill will be listed on the Multi-Year Exercise Plan indicating the Month which the drill will be conducted but will not indicate the day or time of the initial alert. At least one unannounced drill will be conducted during a weekend and one during the week after regular duty hours. 2. Exercise Scenario: An exercise scenario will be published no later than 60 days prior to the conduct of the scheduled Call Down drill. Scenarios will vary, but will normally mirror the scheduled exercises outline in the Multi-Year Exercise Plan. Call Down participants may be required to submit reports via WebEOC based on these scenarios. Any required report will also be described and a format published no later than 60 days prior to the drill. A-1-115 3. Initial Alert: An initial alert will be given via one of the communication means listed in the Communications Plan of the EOP. Currently, Southern LINC will be the primary means of initiating an alert, but other systems will also be exercised. The system to be exercised will be published no later than 60 days prior to the exercise in conjunction with the exercise scenario. 4. Follow Up Alert: A follow up alert will be conducted when an initial alert fails to generate a response within 5 minutes. Alternate systems, which an agency or emergency responder has listed on SendSS as a means to contact them, will then be used until a response has been received. If the primary contact cannot be reached within 10 minutes, then an alert will be sent to any of the alternates listed on SendSS. 5. WebEOC: WebEOC, while not the system used for an initial alert, will be used to record exercise participation. WebEOC is also the primary means of reporting and recording data during actual events. Incorporating WebEOC in Call Down drills will help to build fluency and efficiency throughout the State. If WebEOC will be used, this too will be identified 60 days prior to the drill. 6. Communication Systems: The current primary means of initiating an alert is using the State Group on Southern LINC. A State wide alert and notification (PCA) system in being negotiated during the drafting of this SOP. Once this system is in place, it will become the primary means of alerting the public health community due to its capability to reach users regardless of vendor and is wireless carrier agnostic. Southern LINC will then become secondary. The tertiary system that will be used is phone, either wireless or landline. NOTE: In the event a key responder is not able to be reached within 30 minutes of an actual “Real World” event, coordination between agencies will be made to physically locate the responder. 7. Frequency of Drills: Drills will be conducted monthly and quarterly. Monthly drills will focus primarily on key Division staff, District Emergency Coordinators, the Georgia Hospital Association, and Regional Coordinating Hospitals. Each District will be required to conduct a monthly Call Down drill and record the average response times as described in this SOP. Quarterly drills will extend beyond the alert list for the Monthly drills and will include all PHERs within the state. This will require each District to conduct a Call Down to all PHERs within their respective districts. The following is the expected frequency of Monthly and Quarterly drills: Monthly drills will be conducted January, February, April, May, July, August, October and November each year. The Multi-Year Exercise Plan will have these months annotated as so, with the months of April and October being designated as an unannounced Call Down. A-1-116 Quarterly drills will be conducted March, June, September, and December each year. The Multi-Year Exercise Plan will have these months annotated as so, with the months of June and December being designated as an unannounced Call Down. 8. Feedback: In order to improve the State’s ability to effectively and efficiently conduct an alert and notification, it is critical to receive feedback from participants. Responses to the following questions will greatly assist in the improvement process: Was the appropriate responder contacted? How long did it take to receive a response? Were there any troubles with the communication system employed? Were there any problems with accessing WebEOC or SendSS? What other issues occurred during the drill? Recommendations on how to improve the process or systems used during an alert and notification drill or event. See: Attachment 1 to Appendix 2 to Support Annex 1 – Call Down Feedback Form VII. REPORTING The Office of Emergency Preparedness and each District will be responsible for reporting the results of each Call Down drill or “Real World” event. The information gathered in these reports will be available for reporting to the CDC on a semi-annual basis. This information will also be used to identify strengths to maintain and areas to improve; as well as to develop corrective actions as appropriate. The following reports are attached to this Appendix: 1. 2. 3. 4. 5. 6. 7. Exercise Events Summary – See: Attachment 2 to Appendix 2 to Support Annex 1 District Response Times – See: Attachment 3 to Appendix 2 to Support Annex 1 Hospital Response Times – See: Attachment 4 to Appendix 2 to Support Annex 1 Other Contacts Response Times – See: Attachment 5 to Appendix 2 to Spt Annex 1 Average Response Times – See: Attachment 6 to Appendix 2 to Support Annex 1 SendSS Ratio – See: Attachment 7 to Appendix 2 to Support Annex 1 Systems Ratio – See: Attachment 8 to Appendix 2 to Support Annex 1 VIII. SUMMARY This SOP is intended to provide guidance on the conduct of regularly scheduled Call Down drills that enable agencies at all levels within the public health community to test, assess, and improve upon the alert and notification processes and systems currently in use. These drills will also enable the public health community to rapidly respond to any public health emergency regardless of the size or timing of the event. This SOP is intended to remain flexible and should be revised at least yearly to reflect the input from all those who participate under the guidance of this SOP. This SOP should be revised immediately if it is determined that a procedure outline within would lead to a detrimental outcome for the citizens of Georgia. A-1-117 Georgia Department of Human Resources Division of Public Health Office of Emergency Preparedness Call Down Feedback Form Support Annex A1, Appendix I Attachment 1 Please complete one form for EACH method of communication tested: Participant Name: Title: Agency: Date of Call-Down: Time of Call-Down: Communications System: 800 Megahertz radios Cell phone Nextel WebEOC Live Process Southern LINC DataFM HAM/Amateur radio 1. Were you able to successfully participate in the call down? If not, please describe: YES 2. NO Did you have any access problems or issues? If so, please describe: YES NO 3. Did you have any equipment problems or issues? If so, please describe: YES NO 4. Please describe any other problems or issues: 5. Suggestions/Comments: PLEASE COMPLETE AND SEND TO: EPExercise@dhr.state.ga.us A-1-118 A-1-A-2-A-1-1 A-1-119 Attachment 2: Exercise Events Summary Date Time Scenario Event, Simulated Player Inject, Player Action Event/Action A-1-120 A-2-A-2-A-1-1 A-1-121 Attachment 6: Average Response Times – In Minutes Date of Exercise: Communication Type: AVG Response Times 0:00 - 15:00 15:01 - 30:00 30:01 - 45:00 45:01 - 60:00 60:01 + EOC Operational Response Times 0:00 - 30:00 30:01 - 60:00 60:01 - 90:00 90:01 - 120:00 120:01 + Districts RCHs PH Districts Others A-6-A-2-A-1-1 A-1-122 Attachment 7: SendSS Ratio Date of Exercise: Communication Type: Total Number To Be Contacted 0 Number Reached Using SendSS Data 0 SendSS Ratio #DIV/0! A-1-123 A-7-A-2-A-1-1 Attachment 8: Systems Ratio Date of Exercise: Communication Type: Total Number Systems Used 0 Number Of Systems Operational 0 Systems Ratio #DIV/0! A-1-124 A-8-A-2-A-1-1 A-1-125