Patient Care
o Request an Appointment
o Log in to Patient Account
o See Treatment & Diagnosis Services
o Plan Your Visit
o Find a Doctor
Health Information
o Diseases & Conditions A-Z
o Symptom Checker
o Drugs & Supplements A-Z
o Tests & Procedures A-Z
o Healthy Living
o Expert Blogs
o Mayo Clinic Bookstore
For Medical Professionals
o Online Services for Referring Physicians
o Grand Rounds
o Publications
o Continuing Medical Education
o Mayo Medical Laboratories
Research
o Explore Research Areas
o Find Clinical Trials
o Research Faculty
o Postdoctoral Fellowships
o Discovery’s Edge Magazine
o Search Publications
Education
o Mayo Graduate School
o Mayo Medical School
o Mayo School of Continuous Professional Development
o Mayo School of Graduate Medical Education
o Mayo School of Health Sciences
o Alumni Association
Request an Appointment
Find a Doctor
Find a Job
Log in to Patient Account
Diseases and Conditions
Symptoms
Drugs and Supplements
Tests and Procedures
Healthy Lifestyle
First Aid
Home
Diseases and Conditions
Hives and angioedema
Basics
Definition
Hives and angioedema
Basics
In-Depth
Multimedia
Resources
MayoClinic.com reprints
This single copy is for your personal, noncommercial use only. For permission to reprint multiple
copies or to order presentation-ready copies for distribution, use the reprints link below.
· Order reprints of this article now.
Hives and angioedema
By Mayo Clinic staff
Original Article: http://www.mayoclinic.com/health/hives-and-angioedema/DS00313
D
efinition
CLICK TO ENLARGE
Hives on light skin
Hives on dark skin
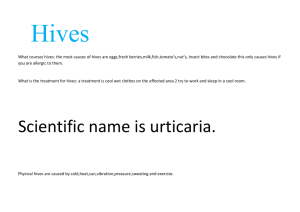
Hives — also known as urticaria (ur-tih-KAR-e-uh) — is a skin reaction that causes raised, red,
itchy welts (wheals, or swellings) in sizes ranging from small spots to large blotches several
inches in diameter. Individual welts appear and fade as the reaction runs its course.
Angioedema is a related type of swelling that affects deeper layers in your skin, often around
your eyes and lips.
In most cases, hives and angioedema are harmless and don't leave any lasting marks, even
without treatment. The most common treatment for hives and angioedema is antihistamine
medications. Serious angioedema can be life-threatening if swelling causes your throat or
tongue to block your airway and leads to loss of consciousness.
Symptoms
CLICK TO ENLARGE
Hives on light skin
Hives on dark skin
Angioedema
Hives
Signs and symptoms of hives include:
Raised red or white welts (wheals, or swellings) of various sizes that can cover large
areas of skin
Welts that resolve while new welts erupt, making it seem as if the condition "moves"
Itching, which may be severe
Rarely, burning or stinging in the affected area
Hives can be either acute or chronic. Acute hives last from less than one day up to six weeks.
Chronic hives last more than six weeks — sometimes for months to years.
Angioedema
Angioedema is a reaction similar to hives that affects deeper layers of your skin, the tissues
underneath your skin, and the lining of your throat and intestines. Angioedema often appears
around your eyes, cheeks or lips, but can also develop on your hands or feet, or genitals, or
inside your throat or bowel. Angioedema and hives can occur separately or at the same time.
Signs and symptoms of angioedema include:
Large, thick, firm welts
Swelling of the skin
Pain or warmth in the affected areas
Difficulty breathing or swallowing, in severe cases
Hereditary angioedema is a rare but more serious inherited (genetic) condition that can cause
sudden, severe and rapid swelling of your face, arms, legs, hands, feet, genitalia, digestive tract
and airway. Signs and symptoms of hereditary angioedema include:
Sudden and severe swelling of the face, arms, legs, hands, feet, genitalia, digestive
tract and airway
Abdominal cramping as a result of digestive tract swelling
Difficulty breathing due to swelling that obstructs your airway
Hereditary angioedema is not usually accompanied by hives.
When to see a doctor
Mild hives and angioedema usually aren't life-threatening. You can usually treat mild cases at
home.
See your doctor if:
Your hives or angioedema doesn't respond to treatment
You have severe discomfort
Your symptoms continue for more than a few days
Seek emergency care if:
You feel lightheaded
You have severe chest tightness or trouble breathing
You feel your throat is swelling
Causes
Hives and angioedema are caused by triggers that produce a skin or tissue reaction by
stimulating certain cells (mast cells) to release histamine and other chemicals into your
bloodstream.
Sometimes it's not possible to pinpoint the cause of hives and angioedema, especially when
these conditions become chronic or recur.
Allergic reactions are one common trigger of acute hives and angioedema. Common allergens
include:
Foods. Many foods can trigger reactions in people with sensitivities. Shellfish, fish,
peanuts, tree nuts, eggs and milk are frequent offenders.
Medications. Almost any medication may cause hives or angioedema. Common
culprits include penicillin, aspirin, ibuprofen (Advil, Motrin, others), naproxen (Aleve,
others) and blood pressure medications.
Other allergens. Other substances that can cause hives and angioedema include
pollen, animal dander, latex and insect stings.
Additional triggers include:
Environmental factors. In some people, environmental factors can stimulate release
of histamine. Examples include heat, cold, sunlight, water, pressure on the skin,
emotional stress and exercise.
Dermatographia (also known as dermographia). The name of this condition literally
means "skin writing." Stroking or scratching the skin results in raised red lines in the
same pattern as the pressure.
Hives and angioedema also occasionally occur in response to blood transfusions, immune
system disorders such as lupus, some types of cancer such as lymphoma, certain thyroid
conditions, and infections with bacteria or viruses such as hepatitis, HIV, cytomegalovirus or
Epstein-Barr virus.
Hereditary angioedema is a rare inherited (genetic) form of the condition. It's related to low
levels or abnormal functioning of certain blood proteins (C1 inhibitors) that play a role in
regulating how your immune system functions.
Risk factors
Hives and angioedema are common. You may be at increased risk of hives and angioedema if
you:
Have had hives or angioedema before
Have had other allergic reactions
Have a disorder associated with hives and angioedema, such as lupus, lymphoma or
thyroid disease
Have a family history of hives, angioedema or hereditary angioedema
Complications
Hives and angioedema nearly always cause:
Itching
Discomfort
In more-serious cases — such as when swelling occurs inside your mouth or throat —
complications can include:
Difficulty breathing.
Loss of consciousness.
Anaphylactic shock — a serious allergic reaction involving your heart and lungs. Your
bronchial tubes narrow, it's difficult to breathe, and your blood pressure drops, causing
dizziness and perhaps loss of consciousness or even death. Anaphylactic shock occurs
rapidly and requires immediate medical care.
Preparing for your appointment
You're likely to start by seeing your family doctor or primary care doctor. However, in some
cases when you call to set up an appointment, you may be referred immediately to a skin
disease specialist (dermatologist) or to an allergy specialist.
Because appointments can be brief and there's often a lot of ground to cover, it can help to be
well prepared. Here are some tips to help you get ready for your appointment and what to
expect from your doctor.
What you can do
Write down your signs and symptoms, when they occurred, and how long they lasted. Also,
make a list of all medications, including vitamins, herbs, supplements and over-the-counter
drugs that you're taking. Even better, take the original bottles and a written list of the dosages
and directions.
Write down questions that you want to ask your doctor. Don't be afraid to ask questions or to
speak up when you don't understand something your doctor says. For hives and angioedema,
questions you may want to ask include:
What is likely causing my symptoms?
Are tests needed to confirm the diagnosis?
What are other possible causes for my symptoms?
Is my condition likely temporary or chronic?
What is the best course of action?
What are the alternatives to the primary approach that you're suggesting?
Do I need prescription medication, or can I use over-the-counter medications to treat
the condition?
What results can I expect?
Can I wait to see if the condition goes away on its own?
What to expect from your doctor
Your doctor is likely to ask you a number of questions, such as:
When did you first begin experiencing symptoms?
What did your skin reaction look like when it first appeared?
Have your symptoms changed over time?
Have you noticed anything that makes your symptoms worse or better?
Do your skin lesions mainly itch, or do they burn or sting?
Do your skin lesions go away completely without leaving a bruise or a mark?
Do you have any known allergies?
Have you ever had a similar skin reaction before?
Have you tried a new food for the first time, changed laundry products or adopted a
new pet?
What prescriptions, over-the-counter medications and supplements are you taking?
Have you started taking any new medications or started a new course of a medication
you've taken before?
Has your overall health changed recently? Have you had any fevers or lost weight?
Has anyone else in your family ever had this kind of skin reaction? Do other family
members have any known allergies?
What at-home treatments have you used?
Tests and diagnosis
Your doctor will examine your welts or areas of swelling if they are still present and take a
careful medical history to identify possible causes. Your doctor's questions may focus on
recognized factors linked to urticaria and angioedema, such as certain foods, physical triggers
and medications. It's important to tell your doctor about all medications you take, including overthe-counter (nonprescription) drugs and supplements, even if you don't take them every day. To
help pinpoint the cause of your symptoms, your doctor may recommend that you keep a
detailed diary of exposure to possible irritants.
If the cause of your hives or angioedema isn't apparent from your medical history or if your
symptoms persist or recur often, your doctor may recommend an allergy skin test.
Puncture, prick or scratch (percutaneous) test. This is the type of skin test that's
usually performed first. Tiny drops of purified allergen extracts are pricked or scratched
into your skin's surface. This test is usually performed to identify allergies to pollen,
animal dander, foods, insect venom and penicillin.
Intradermal (intracutaneous) test. Purified allergen extracts are injected into the skin
of your arm. Doctors may perform this test if they strongly suspect you're allergic to an
irritant even though your puncture test is negative — especially to an irritant to which a
future reaction could be life-threatening, such as insect venom or penicillin.
If your doctor suspects hereditary angioedema, he or she may order blood tests to check for
levels and function of specific blood proteins.
Treatments and drugs
If your symptoms are mild, you may not need treatment. Many cases of hives and angioedema
clear up on their own. But treatment can offer relief for intense itching, serious discomfort or
symptoms that persist.
The standard treatment for hives and angioedema is antihistamines, medications that reduce
itching, swelling and other symptoms of histamine release.
For severe hives or angioedema, doctors may also sometimes prescribe an oral corticosteroid
drug — such as prednisone — which can help lessen swelling, redness and itching.
Antihistamines
Antihistamines are divided into older, first-generation drugs and newer, second-generation
medications based on their chemistry and associated side effects. Each category includes
nonprescription and prescription drugs.
Second-generation, newer antihistamines. Doctors generally recommend starting treatment
with these newer, second-generation drugs. For most people, these drugs are less likely to
cause drowsiness or reduce your reaction time while you're driving or performing other mentally
or physically demanding tasks.
Nonprescription second-generation antihistamines include:
Loratadine (Claritin, Alavert)
Cetirizine (Zyrtec)
Prescription second-generation antihistamines include:
Desloratadine (Clarinex)
Fexofenadine (Allegra)
Levocetirizine (Xyzal)
First-generation, older antihistamines. These medications tend to make you drowsy and
respond more slowly than usual while driving or performing other tasks requiring physical
coordination. In addition, they may cause dry mouth, blurred or double vision, constipation or
difficulty passing urine. But they may be more helpful than second-generation antihistamines for
some people with hives or angioedema, especially if your symptoms are severe or involve
significant swelling of your face, tongue or throat. They may also be helpful taken at bedtime if
your symptoms disturb your sleep.
Nonprescription first-generation antihistamines include:
Diphenhydramine (Benadryl, others)
Chlorpheniramine (Chlor-Trimeton, others)
Prescription first-generation antihistamines include:
Hydroxyzine (Vistaril)
Treatment for hereditary angioedema
Antihistamines and oral corticosteroid medications — although useful in treating hives and
acute angioedema — are often ineffective in treating hereditary angioedema. Medications used
to treat hereditary angioedema on a long-term basis include certain androgens (male
hormones), such as danazol, that help regulate levels of blood proteins.
The Food and Drug Administration (FDA) has also approved certain treatments targeting
specific blood proteins that function abnormally in hereditary angioedema. These medications
include:
Cinryze and Berinert, two treatments derived from donated human blood plasma. Both
drugs provide C1 esterase inhibitor, a blood protein that's inadequate or defective in
hereditary angioedema. Cinryze is approved as a therapy to prevent hereditary
angioedema attacks in adults and adolescents. It's taken as an injection by vein every
few days and can be self-administered after training by a health professional. Berinert is
approved to treat acute hereditary angioedema attacks affecting the face and abdomen
while the attacks are under way. Berinert also is taken as an injection by vein, but it
must be given by a health professional.
Ecallantide (Kalbitor) is a protein derived from yeast. It blocks the activity of a blood
protein called kallikrein, which is involved in hereditary angioedema. It's approved for
adolescents and adults as a treatment to counter the effects of acute hereditary
angioedema attacks on all body areas. Ecallantide is taken as an injection under the
skin (subcutaneous) that must be given by a health care professional.
Emergency situations
For a severe attack of hives or angioedema, you may need a trip to the emergency room and
an emergency injection of adrenaline (epinephrine). If you have had a serious attack or your
attacks recur, despite treatment, your doctor may prescribe — and instruct you how to use —
adrenaline to carry with you for use in emergency situations.
Lifestyle and home remedies
If you're experiencing mild hives or angioedema, these tips may help relieve your symptoms:
Try to identify and avoid substances that irritate your skin or that cause an
allergic reaction. These can include foods, medications, pollen, pet dander, latex and
insect stings.
Use an over-the-counter antihistamine. A nonprescription oral antihistamine, such as
loratadine (Claritin), cetirizine (Zyrtec) or diphenhydramine (Benadryl, others) may help
relieve itching.
Apply cool, wet compresses. Covering the affected area with bandages and
dressings can help soothe the skin and prevent scratching.
Take a comfortably cool bath. To relieve itching, sprinkle the bath water with baking
soda, uncooked oatmeal or colloidal oatmeal — a finely ground oatmeal that is made
for the bathtub (Aveeno, others).
Wear loose, smooth-textured cotton clothing. Avoid clothing that's rough, tight,
scratchy or made from wool. This will help you avoid irritation.
Prevention
To lower your likelihood of experiencing hives or angioedema, take the following precautions:
Avoid known triggers. These may include certain foods or medications, or situations
such as temperature extremes, that have triggered past allergic attacks.
Keep a diary. If you suspect foods are causing the problem, keep a food diary. Be
aware that some foods may contain ingredients that are listed by less common names
on the label.
References
Kaplan AP. Urticaria and angioedema. In: Wolff K, et al. Fitzpatrick's Dermatology in
General Medicine. 7th ed. New York, N.Y.: The McGraw-Hill Companies; 2008.
http://www.accessmedicine.com/content.aspx?aid=2958607. Accessed Sept. 13, 2010.
MacNeal RJ. Urticaria. The Merck Manuals: The Merck Manual for Healthcare
Professionals.
http://www.merck.com/mmpe/sec10/ch109/ch109e.html?qt=urticaria&alt=sh#sec10ch109-ch109e-101c. Accessed Sept. 14, 2010.
Bingham CO. New onset urticaria: Diagnosis and Treatment.
http://www.uptodate.com/home/index.html. Accessed Sept. 29, 2010.
Atkinson JP. Diagnosis of hereditary angioedema.
http://www.uptodate.com/home/index.html. Accessed Sept. 29, 2010.
Bingham CO. New onset urticaria: Epidemiology, clinical manifestations and etiology.
http://www.uptodate.com/home/index.html. Accessed Sept. 29, 2010.
Urticaria and angioedema. In: Wolff K, et al. Fitzpatrick's Color Atlas and Synopsis of
Clinical Dermatology. 6th ed. New York, N.Y. The McGraw-Hill Companies; 2009.
http://www.accessmedicine.com/content.aspx?aID=5187962. Accessed Sept. 14, 2010.
Initial evaluation of all patients with urticaria. In: Habif TP. Clinical Dermatology: A Color
Guide to Diagnosis and Therapy. 5th ed. Edinburgh, Scotland. Mosby/Elsevier; 2010.
http://www.mdconsult.com/books/page.do?eid=4-u1.0-B978-0-7234-3541-9..00015-8-s0180&isbn=978-0-7234-3541-9&type=bookPage&sectionEid=4-u1.0-B978-0-7234-35419..00015-8--s0180&uniqId=220753099-3#4-u1.0-B978-0-7234-3541-9..00015-8--s0180.
Accessed Oct. 1, 2010.
Treatment of urticaria. In: Habif TP. Clinical Dermatology: A Color Guide to Diagnosis
and Therapy. 5th ed. Edinburgh, Scotland. Mosby/Elsevier; 2010.
http://www.mdconsult.com/books/page.do?eid=4-u1.0-B978-0-7234-3541-9..00015-8-s0290&isbn=978-0-7234-3541-9&type=bookPage&sectionEid=4-u1.0-B978-0-7234-35419..00015-8--s0290&uniqId=220753099-3#4-u1.0-B978-0-7234-3541-9..00015-8--s0290.
Accessed Sept. 13, 2010.
Acute urticaria: Evaluation and management. In: Habif TP. Clinical Dermatology: A
Color Guide to Diagnosis and Therapy. 5th ed. Edinburgh, Scotland. Mosby/Elsevier;
2010. http://www.mdconsult.com/books/page.do?eid=4-u1.0-B978-0-7234-35419..00015-8--s0185&isbn=978-0-7234-3541-9&type=bookPage&sectionEid=4-u1.0-B9780-7234-3541-9..00015-8--s0185&uniqId=220753099-3#4-u1.0-B978-0-7234-35419..00015-8--s0185. Accessed Oct. 1, 2010.
Bingham CO. An overview of angioedema: Clinical features, diagnosis and
management. http://www.uptodate.com/index/home.html. Accessed Oct. 1, 2010.
Delves PJ. Angioedema. The Merck Manuals: The Merck Manual for Healthcare
Professionals. http://www.merck.com/mmpe/sec13/ch165/ch165b.html. Accessed Oct. 1,
2010.
FDA licenses for marketing new drug for rare genetic disease. Food and Drug
Administration.
http://www.fda.gov/NewsEvents/Newsroom/PressAnnouncements/ucm161477.htm.
Accessed Oct. 1, 2010.
Cinryze. Food and Drug Administration.
http://www.fda.gov/BiologicsBloodVaccines/BloodBloodProducts/ApprovedProducts/Licen
sedProductsBLAs/FractionatedPlasmaProducts/ucm150480.htm. Accessed Oct. 6, 2010.
Nolte H, et al. Overview of skin testing for allergic disease.
http://www.uptodate.com/index/home.html. Accessed Oct. 2, 2010.
Berinert. Food and Drug Administration.
http://www.fda.gov/BiologicsBloodVaccines/BloodBloodProducts/ApprovedProducts/Licen
sedProductsBLAs/FractionatedPlasmaProducts/ucm186264.htm. Accessed Oct. 15,
2010.
Kalbitor. Drugs @FDA.
http://www.accessdata.fda.gov/scripts/cder/drugsatfda/index.cfm. Accessed Oct. 15,
2010.
Gibson LE (expert opinion). Mayo Clinic, Rochester, Minn. Oct. 13, 2010.
DS00313 Dec. 21, 2010
© 1998-2011 Mayo Foundation for Medical Education and Research (MFMER). All rights reserved. A single copy
of these materials may be reprinted for noncommercial personal use only. "Mayo," "Mayo Clinic,"
"MayoClinic.com," "EmbodyHealth," "Enhance your life," and the triple-shield Mayo Clinic logo are trademarks of
Mayo Foundation for Medical Education and Research.
StumbleUponDiggdel.icio.usFacebookMySpace
We comply with the HONcode standard for trustworthy health
information: verify here.