Improving Cancer Therapy: Triggering Chemotherapy Using
advertisement
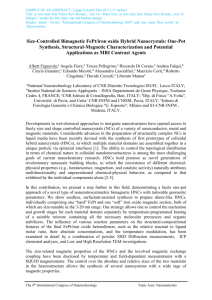
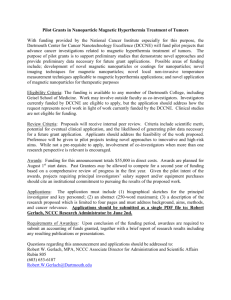
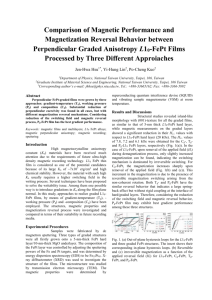
Improving Cancer Therapy: Triggering Chemotherapy Using Temperature Responsive Polymers Mary Kathryn Sewell Christopher S. Brazel, Ph.D. Professor of Chemical and Biological Engineering, The University of Alabama Abstract: A combination cancer treatment platform that combines hyperthermia and chemotherapy was investigated. By including magnetic nanoparticles in a thermally responsive hydrogel, a smart drug delivery system was created. Drug delivery was triggered using in vivo experiments to simulate hyperthermia treatment. The combination of treatment methods could improve cancer therapy efficacy and decrease negative side effects currently associated with cancer treatments. To create an even heating profile, nanomagnets must be uniformly dispersed within a hydrogel. The size of agglomerations of FePt nanoparticles was dependent on the initial concentration of nanomagnets. Drug diffusion coefficients were determined for a model drug, theophylline, when released from thermallysensitive poly(N-isopropyl acrylamide-coacrylamide) gels. From these experiments, the effects of temperature and FePt concentration on diffusion coefficients were determined. Increased nanomagnet concentrations did not obstruct theophylline diffusion, therefore drug carriers can be designed without concern about altering their microstructure due to the nanoparticles. Increasing temperature above the normal human body of 37oC to simulate hyperthermia, however, caused slower release rates in gels that had been dried before the release studies. Introduction and Background: The most common forms of cancer treatment include chemotherapy, radiation, and surgery, and to a lesser extent, hyperthermia. Hyperthermia is a heating therapy in which the cancerous tissue is heated between 43oC and 45oC (Kim et al.). The higher temperatures kill tumor cells because the cancerous tissue cannot cool itself as quickly or efficiently as healthy tissue. Hyperthermia is usually used in combination with other therapies to increase treatment efficiency (NCI). Localized hyperthermia is limited to the affected area of a patient’s body; the heating source may be external or internal (NCI). Chemotherapy involves treating patients with anti-cancer drugs; these drugs can either destroy the cancerous cells or slow their growth (NCI). The high concentrations of anti-cancer drugs used in chemotherapy can harm healthy cells as well, causing hair loss, nausea, and other negative side effects (NCI). Radiation treatment uses ionizing radiation to shrink tumors and destroy cancer cells (NCI). This treatment is often used in combination with surgery or chemotherapy (NCI). Surgery is another common treatment method in which the tumor is removed from the patient; however not all tumors can be safely removed. A metastasis occurs when cancerous cells spread from the primary affected region to another region or system in the body (NCI). Often these metastatic cells cannot be detected until other tumors have formed (NCI). A unique solution to the challenge of effective cancer therapy with minimal side effects is proposed. Our approach to combine hyperthermia with chemotherapy utilizes magnetic nanoparticles in thermally responsive hydrogels. The nanoparticles are designed so that an externally administered AC magnetic field will heat them, causing the thermal response of the gel. The mesh network of the hydrogel will change, releasing a controlled amount of anti-cancer agent at a specific location. The inclusion of adenoviruses or other biological agents would allow for targeting of the treatment. The combination of hyperthermia and chemotherapy should increase treatment efficacy (Ito et al.). The targeting and triggering of the therapy should localize both the heating and chemotherapeutic agent to help decrease negative side effects associated with current cancer treatment options. This research project is focused on synthesis and characterization of magnetic nanoparticlecontaining hydrogels to determine their thermal and diffusive behavior. One objective is to create an even dispersion of magnetic nanoparticles into the hydrogel. This will allow for even heating profiles during hyperthermia treatment. Another objective is to determine the effect of temperature and nanoparticle concentration on diffusion of a model drug from hydrogel systems. A final objective is to investigate the parameters of magnetic fields that can successfully heat hydrogels containing magnetic nanoparticles. Environmentally responsive polymers have been studied for some time as a way to increase the efficacy of pharmaceutical administration, improve drug delivery platforms, reduce administration frequency, and decrease side effects (Ankareddi and Brazel, Brazel and Peppas 1999, Schmaljohann). The unique characteristics of these materials allow for engineering of desired responses. This technology has been in use for some time in the form of enteric coatings on many drug capsules. These coatings only dissolve in the basic pH of the intestines, rather than in the acidic pH of the stomach. Polymers may be responsive to a change in temperature, pH, concentration, or a combination of these factors (Schmaljohann). When stimulated by a change in one of these conditions, an environmentally responsive polymer will undergo a phase transition. This changes the conformation of the system, causing the desired release behavior. In order to exploit the thermal behavior of temperature-responsive hydrogel systems, the lower critical solution temperature (LCST) needs to be known. The LCST is the temperature at which a polymer will undergo phase transition and exhibit a change in volume or conformation. An example of this behavior can be seen in poly(N-isopropyl acrylamide), P(NIPAAm). Below 32oC, a PNIPAAm gels are hydrophilic and swell with water. When the sample is heated above this temperature, it becomes hydrophobic, effectively “squeezing” the water out of the sample. The inclusion of hydrophilic or hydrophobic comonomers changes the chemical structure of the gel and alters the LCST (Ankareddi and Brazel, Feil et al.). This paper explores the use of PNIPAAmbased hydrogels to characterize drug diffusion and heating. Because our system will utilize hyperthermia to trigger drug release, a copolymer that has an LCST in the range of 42-45 oC is desirable. An LCST of approximately 45oC can be achieved by using16.6 mol% acrylamide (AAm) to increase the hydrophilicity of PNIPAAm (Ankareddi and Brazel). These copolymers are termed P(NIPAAm-co-AAm). Another parameter that can be altered to control drug diffusion is the polymer mesh size. This can be controlled to some degree by changing the amount of cross-linking agent or comonomer used during synthesis. Materials and Methods: Hydrogel synthesis was carried out via freeradical solution polymerization. Quantities of reactants and solvents were based on the amount of NIPAAm used in synthesis; all other values were calculated based on this number. NIPAAm and AAm were dissolved in a 50:50 weight percent methanol and water solution, which was used as the solvent. Methylene bisacrylamide (MBAAm) at 1mol% was used as a cross-linking agent. Ammonium persulfate at 1wt% was used as the free-radical initiator. Tetramethylethylenediamine (TEMED) was used at 1wt% as the reaction accelerator. For the heating experiments, poly(2hydroxyethyl methacrylate) or PHEMA was used instead of PNIPAAm, but it was synthesized similarly to the P(NIPAAm-co-AAm) samples. Instead of TEMED, sodium metabisulfite was used as an additional initiator at 1wt% total monomer weight. Samples were synthesized by first adding measured amounts of NIPAAm, AAm, and MBAAm to a beaker. Water and methanol were added, and the solution was mixed on a magnetic stir plate. For 15 minutes, nitrogen gas was purged through a balloon into the solution. This removed any oxygen that could act as a free radical scavenger during the polymerization. After the gas purge, the initiator and accelerator were added. After stirring for 1-2 minutes, the solution was then pipetted between two siliconized glass plates that were separated by a Teflon gasket and secured with clamps. The thickness of the gasket controlled the thickness of the resulting polymer sample. Polymerization of a P(NIPAAm-co-AAm) sample usually took 24 hours. For some samples, a model drug, theophylline, was added at 1 wt% of the monomer amount, to the mixture with the monomers prior to polymerization. If magnetic nanoparticles were included in a sample, the synthesis procedure varied. In this study, FePt magnetic nanoparticles, also synthesized at UA, were used. The average size of the particles was 6nm, dispersed in water with mercaptoundeconoic acid. After the NIPAAm, AAm, and MBAAm were well mixed with the solvents, the beaker was removed from the stirring plate. The magnetic stir bar was also removed from the solution. The desired amount of FePt solution was added drop wise to the solution in the beaker. The resulting solution was stirred under a nitrogen gas purge. The accelerator and initiator were added, and the solution was stirred with a glass rod for 1-2 minutes and then plated as described before. The drug release studies were completed using a Shimadzu Model UV-2401 spectrophotometer attached to Distek Model 2100C USP type II dissolution cells. A sample was taken from a cell to the spectrometer via a low-flow peristaltic pump and Tygon tubing. The Kinetics setting on UV-Probe software was used to collect drug release data every 10 seconds over the course of the experiments. The release medium was 1L of deionized water kept at 37 or 50oC. Absorbance data were collected at 275nm for 10 hours. Beer’s Law, which shows a linear relationship between absorbance and concentration, was used to determine the amount of theophylline released over time. The experiments were run in triplicate to determine reproducibility. The heating experiments were carried out to determine the rate of termperature rise and steady state temperatures reached using an AC magnetic field. The instrument used for these experiments was a custom designed hyperthermia chamber built by Induction Atmospheres. The six turn solenoid attachment was used with the chamber. The sample was placed in a glass vial, and the vial was inserted into the coils for the experiment. The magnetic field produced in this experiment was 560 Oe, with a resonance frequency of 231 kHz. A FLIR Systems ThermaCAM SC2000 NTSC, with infrared imaging, was used to collect the temperature data at the center, midpoint, and edge of the sample. Each experiment lasted 15 minutes, with temperatures taken every minute. To establish reproducibility, four trials were run for each sample. A 12mm diameter PHEMA hydrogel loaded with 0.75 wt% FePt was used for the experiments. Results and Discussion: At all levels of FePt concentration, agglomerations were seen in the hydrogels. For lower initial nanoparticle concentrations, the size of the agglomerates was smaller than in more concentrated samples (Figure 1). At greater concentrations, the color of the hydrogel is noticeably darker and the agglomerations appear evenly dispersed. An optical microscope was used to verify the size of agglomerations in different samples. a b Figure 1. Microscope image of FePt agglomerations in PHEMA hydrogels with (a) 0.10 wt% and (b) 0.75 wt% FePt. The white line scales to 500 m. Although there are more aggregates in the 0.10wt% FePt sample, they are small in size than those found in the 0.75wt% FePt sample. One sample of P(NIPAAm-co-AAm) at 1.25 wt% FePt was completely non-uniform with millimeter sized aggregates. This suggests there is an upper limit to the inclusion and dispersion of magnetic nanoparticles in hydrogels. Attaining a completely even dispersion of nanomagnets may not be possible. Because the nanoparticle solutions are synthesized in organic solvents, even after ligand exchanges on the nanoparticles, the aqueous nature of the hydrogels may cause aggregates to form at all concentrations. The drug release experiments were used to determine diffusion coefficients for theophylline from the hydrogel systems (Figure 2). These coefficients were determined using the early time approximation of the Fickian equation for diffusion (Brazel and Peppas 2000): Mt Dt 4 2 M 1/ 2 M ,0 t M 0.6 where Mt is the mass of solute released at time t, M∞ is the total mass of solute released, D is the diffusion coefficient in cm2/s, t is the time in s, and is the half-thickness of the dry hydrogel sample in cm. At higher temperatures, the diffusion of theophylline from P(NIPAAm-co-AAm) gels is slowed (Table 1). This was expected because the hydrogel has undergone a phase transition and collapsed in on itself. The inclusion of FePt had little effect on the release of theophylline. At higher concentrations the release rate was marginally slower than at lower concentrations, although the difference is not significant. Future experiments will include magnetically-triggered release studies, using the hyperthermia chamber. Other future studies will examine the release behavior starting from pre-swollen hydrogels kept at 37oC, where a squeezing mechanism is expected to offer higher release rates at higher temperatures. Table 1. Diffusion Coefficients for Theophylline Release from P(NIPAAm-co-AAm) Hydrogels* 37oC 50oC 0 wt % FePt 4.79 ± 0.09 3.28 ± 0.28 0.002 wt % FePt 4.47 ± 0.20 3.37 ± 0.21 0.05 wt % FePt 4.35 ± 0.08 4.09 ± 0.36 0.125 wt % FePt 4.06 ± 0.21 8 3.10 ± 0.24 2 *All values in10 cm /s Figure 2. The effects of temperature and FePt nanomagnet concentration on theophylline release from P(NIPAAm-co-AAm) hydrogels. In the heating experiments, the magnetic nanoparticle agglomerations were shown to have a negligible effect on the overall heating profile (Figure 3). The gels heated to approximately 31oC during each experiment. Despite having an uneven dispersion of FePt in the sample, the heating appears uniform. This suggests that as long as the aggregates are fairly uniform in size, the gel will heat evenly. Future studies will include different polymers, an increased concentration of nanomagnets, and different operating parameters of the hyperthermia unit with the goal of heating the sample to temperature effectively used for hyperthermia (42-45oC). Figure 3. The radial heating profile of PHEMA with 0.75 wt% FePt. The dip in the lines was caused by the camera’s auto-adjust function. References: 1. 2. Figure 4. An infrared thermal image of a PHEMA gel with 0.75wt% FePt during the heating experiments. The outer yellow rings correspond to the coils of the hyperthermia unit surrounding the sample vial (seen from the top). 3. 4. Conclusions: The size of FePt agglomerates in P(NIPAAm-co-AAm) hydrogels can be limited with careful synthesis procedures. Preliminary results indicate that even with aggregation of magnetic nanoparticles, the heating profiles during hyperthermia experiments are uniform. Further work is needed to determine the maximum amount of FePt that can be included in a gel without creating an uneven heating profile. The drug release studies indicate that the increased nanomagnet concentration does not interfere with drug delivery and that temperature offers a way to control the rate of release. Future studies will determine the release rates for gels with different mesh sizes and higher concentrations of FePt. Another set of future studies will be completed to show magnetically-triggered drug release. Acknowledgements: I would like to thank the following people who have supported my project: Dr. Dong Hyun Kim, Dr. David E. Nikles, Hitesh Bagaria, Lauren Blue, Kyle Fugit, Andrei Ponta, and Yhni Thai. I would also like to acknowledge those who funded my research: the McWane Undergraduate Fellowship, the John McKinley Creative Project Award, and the Alton Scott Memorial Fund. 5. 6. 7. 8. D.-H. Kim, S. Lee, K.-N. Kim, K.-M. Kim, I. Shim, and Y.Lee. Temperature changes of various ferrite particles with alternating magnetic field for hyperthermic application. Journal of Magnetism and Magnetic Particles, Volume 293 Issue 1 (2005), pp. 320-327. A. Ito, Y. Kuga, H. Honda, H. Kikkawa, A. Horiuchi, Y. Watanabe, and T. Kobayashi. "Magnetite nanoparticle-loaded anti-HER2 immunoliposomes for combination of antibody therapy with hyperthermia," Cancer Letters, 212 (2004) 167-175. Hyperthermia in Cancer Treatment: Questions and Answers. National Cancer Institute. http://www.cancer.gov. I. Ankareddi and C.S. Brazel .Synthesis and characterization of grafted thermosensitive hydrogels for heating activated controlled release. International Journal of Pharmaceutics, Volume 336, Issue 2 (2004), pp. 241-247. C.S. Brazel and N.A. Peppas. Mechanisms of solute and drug transport in relaxing swellable hydrophilic glassy polymers. Polymer, 40 (1999), pp. 3383–3398. D. Schmaljohann. Thermo- and pH-responsive polymers in drug delivery. Advanced Drug Delivery Reviews ,Volume 58, Issue 15, (2006), pp. 16551670. H. Feil, Y.H. Bae, J. Feijen and S.W. Kim. Effect of comonomer hydrophilicity and ionization on the lower critical solution temperature of Nisopropylacrylamide copolymers. Macromolecules, 26 (1993), pp. 2496–2500. C.S. Brazel and N.A. Peppas. Modelling of drug release from swellable polymers. Eur. J. Pharm. Biopharm, 49 (2000), pp. 47–58. Mary Kathryn Sewell, from Helena, Alabama, is a senior majoring in Chemical and Biological Engineering. For her work with the Magnetic Biomaterials Research Group, Mary Kathryn has received the John McKinley Creative Project Award, a Randall Outstanding Undergraduate Research Award, and two McWane Undergraduate Fellowhips. She is also the Assistant Editor for this issue of JOSHUA.