Kent and Canterbury Hospital
advertisement

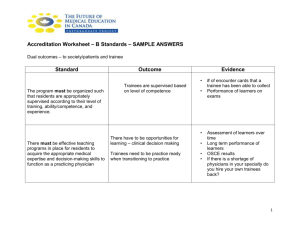
TRAINING PROGRAMME East Kent Hospitals University NHS Foundation Trust (EKHUFT) is one of the Trust largest hospital Trusts in the country, with more than 6,000 staff, including approximately 355 junior doctors, serving a population exceeding 700,000 and provides integrated patient care in East Kent with over 80 clinical specialities. Established on 1st April 1999, East Kent Hospitals University NHS Trust has three acute hospitals at Canterbury, Ashford and Margate, with smaller hospitals in Dover and Folkestone. Plans have been approved for a new state of the art hospital in Dover to replace the existing Buckland Hospital. The Trust achieved University teaching status in 2008. The KSS Deanery introduced the Local Education Provider (LEP) metrics in 2011 and East Kent was one of the top performing Trusts in the region and has annually achieved KSS Deanery Contract Review compliance. In 2010 East Kent Hospitals University NHS Foundation Trust was awarded ‘Trust of the Year 2010’ by healthcare information organisation Dr Foster. Dr Foster measures healthcare across a range of different areas that are important to patients on behalf of the Government. At the end of last year it named EKHUT as the best performing Trust in the country. Recent results show a marked improvement in the national inpatient survey in nine of the ten categories and an impressive 25 percentage point increase in patient satisfaction with regard to waiting lists and planned admissions. There have also been some clear improvements in standards of communication and privacy. A&E/the Emergency Departments have seen a 10 percentage point improvement and discharge has seen a 5 percentage point improvement EKHUFT has a tradition of being a popular and friendly Trust for trainees and 3rd, 4th and 5th year medical students from King’s College London Medical School come on rotation to the Trust as well as students from St George’s, Tooting and overseas including St George’s University Medical School, Grenada. The beautiful coast of East Kent, with its sandy beaches, areas of outstanding scientific interest and beauty and wide range of water-based sports and activities is only 20-30 minutes away by car or by train/bus. In addition, Canterbury's surrounding countryside dips and sweeps through river valleys, woods and hills to the seaside towns of Herne Bay and Whitstable. There is a high speed train with regular trains running every weekday, which makes travel between Kent and central London faster than ever. Dover and Folkestone are also not too far away for visits into France and the rest of Europe. The Trust has recently undertaken a pilot project to revise the model of working in medicine with the introduction of “hot” and “cold” teams with improved cover at weekends. The Better Training Better Care project has had significant outcomes so far in the improvement of training opportunities, multi professional team working and patient care. Data is being collected on patient outcomes in discharge, length of stay and early trends show considerable improvements. Medical Education The Directorate of Medical Education is actively involved with innovative work including A Learning and Information Community for East Kent (A.L.I.C.E.), Doctors and Dentists Advice, Liaison and Support service, presentations at National and International conferences. The Directorate is also actively involved with the Deanery leadership programme for junior doctors as well as encouraging trainees to be involved as trainee representatives, to be a proactive postgraduate doctors’ voice, on specialty local faculty groups and Local Academic Board. Each Education Centre in the Trust has full educational facilities and resources, supported by a dedicated team across the 3 sites. A Trustwide resource for simulation training is based at Devon House, Margate including the latest SimMan 3G. There is a well stocked library at each of the hospital sites (Ashford, Canterbury and Margate), staffed between 9am and 5pm Monday to Friday but accessible 24/7 with a key fob. In addition to the resources available within the trust, the service collaborates with other hospital libraries nationally and in the KSS Deanery and can borrow items from them. A web based catalogue is available for locating books and managing your library account. Electronic journals and databases can be accessed with an Athens password and onsite access to UptoDate is also available. Open access computers connected to the NHS network and Wifi via an independent provider are available for library members. Regular workshops are held on finding the evidence, basic statistics, systematic reviews and critical appraisal skills. A clinical librarian service is available to support learning in clinical areas and journal clubs. The NetVibes system offers free and open access and is now operational, offering tabs for different departments with tables of contents and links to journals. The Trust holds an annual awards event with a range of categories and this year we are holding the first Medical Education Awards Day in July with awards for leadership, teaching and professionalism. Hospital William Harvey Hospital (WHH), Ashford, Kent Four ACCS programmes in total are offered at the Trust. 2 programmes are based entirely at the William Harvey Hospital for both years. The third programme involves the trainee rotating to the Kent and Canterbury in the first year and is then based at the Queen Elizabeth the Queen Mother Hospital for the whole of the second year. The fourth programme involves the trainee rotating to the Kent and Canterbury Hospital in the first year and returning to the William Harvey Hospital for the second year. 3 trainees are based at the William Harvey at any one time. The William Harvey is a busy District General Hospital with full Accident and Emergency services provided 24 hours a day, 365 days per year, intensive care unit, neonatal intensive care unit, acute stroke services, state of the art imaging facilities with endoscopy unit, in-patient general surgery and day surgery unit. • • • • • Plastic surgery/Burns (East Grinstead) Cardio-thoracic and Neurosurgery (London) All types of patients are treated including major trauma (trauma unit) Helicopter site for HEMS and Police helicopter at night Vascular and urology at Kent & Canterbury In recent years the hospital has undergone considerable expansion of its services to include: Extension to Accident and Emergency to include dedicated facilities for gynae emergencies, ENT/ eye emergencies and paediatric resus. New gynaecology ward and expansion of children’s ward. Refurbishment of delivery suite and addition of midwife led birthing unit. Modernisation of pharmacy services with state of the art robotics dispensary. Satellite renal dialysis unit to allow patients to be treated nearer to home. Installation of tele-medicine service to allow 24/7 assessment of stroke patients for life-saving and life-enhancing thrombolysis treatment. Establishment of Kent and Medway Primary PCI service. The William Harvey was chosen as the pPCI centre for Kent offering a pioneering new treatment for patients who have suffered a particular type of heart attack. New Head and Neck facility to enable the centralisation of in-patient maxillofacial services. Major upgrade to the CT and MRI facilities. Kent and Canterbury Hospital There is one CT1 Acute Medicine post at the Kent and Canterbury Hospital with trainees rotating with the A&E post at the William Harvey after 6 months. The Emergency Care Centre (ECC) provides a new model of care in the NHS and was established in 2005 as a result of reconfiguration of patient services within the East Kent Hospitals NHS Trust and takes acute admissions for medicine, vascular surgery and urology as well as providing a minor injuries unit. The focus of the ECC is to deliver effective high quality patient centred care through an integrated team led by senior medical and nursing staff. Patients are assessed rapidly by introducing the concept of a single clerking proforma. KCH provides patient access to critical care, non-interventional coronary care, diagnostic radiology, laboratory services and other specialties (such as renal, neurology, haematology, oncology, rheumatology and dermatology). Queen Elizabeth the Queen Mother Hospital There is one CT2 post at the Queen Elizabeth the Queen Mother Hospital covering 6 months in Anaesthetics and 6 months in Intensive Care Medicine. Currently the in-patient surgical specialists provided include lower G.I, orthopaedics, spine and trauma, gynaecology and obstetrics. Additionally, the Day Care Surgery Unit provides ENT, ophthalmics and maxillo facial. Acute and chronic pain services are also provided on site. And there is great emphasis regional block for orthopaedic & trauma surgery and a there is a stand alone bronchoscopy list supervised by Respiratory Physicians. There are some paediatric lists that encompass dental, maxillo facial, orthopaedic, general surgery, ENT and trauma. This hospital has 24hr A&E and as such experience will be gained in emergency general surgical and trauma lists. There is a separate Obstetric anaesthetic list. The ITU is recognised for core training. There is a separate ITU and HDU with critical outreach service. There are acute and chronic pain services. Introduction The ACCS programme covers a two year period and encompasses four specialties including new posts for this year at Kent and Canterbury Hospital and the Queen Elizabeth the Queen Mother Hospital. The four two year programmes at East Kent are: Programme 1 CT1 Acute Medicine (WHH) and Emergency Medicine (WHH) CT2 Anaesthetics (WHH) and Intensive Care Medicine (WHH) Programme 2 CT1 Emergency Medicine (WHH) and Acute Medicine (WHH) CT2 Intensive Care Medicine (WHH) and Anaesthetics (WHH) Programme 3 CT1 Emergency Medicine (WHH) and Acute medicine (KCH) CT2 Anaesthetics (QEQM) and Intensive Care (QEQM) Programme 4 CT1 Acute Medicine (KCH) and Emergency Medicine (WHH) CT2 Intensive Care Medicine (WHH), Anaesthetics (WHH) All trainees rotate every 6 months. Terms of Business Include terms of business and information on workfinding service Distinction between training programme offer and employment contract Post details Specialty Grade Location within programme ACCS CT1 & CT2 Depending on rotation:William Harvey Hospital Kent and Canterbury Hospital Queen Elizabeth the Queen Mother Hospital Type of Work CT1 year The first year (CT1) consists of six months of Emergency Medicine and six months of AM or vice versa, based at either the William Harvey or the Kent and Canterbury Hospital. The Accident and Emergency unit at the William Harvey provides a full 24 hour a day 365 day service receiving major trauma and all emergency patients from the area in conjunction with the A & E department at QEQM. Both sites have a helipad. At WHH all major specialties are on site except: - Plastic surgery/Burns (East Grinstead) - Cardio-thoracic and Neurosurgery (London) - Vascular and urology at Kent and Canterbury Hospital During the Acute Medicine (AM) placement the trainee is based on the Acute Medical Unit (AMU) and Ambulatory Care Unit. In both settings patients are assessed, diagnostics performed and treatment commenced following referral from A&E / GP. Ambulatory care facilitates rapid assessment and treatment of those patients well enough to go home on the same day who can return for early reviews as required. Patients admitted to the AMU are either discharged or transferred to an appropriate specialty ward within 48 hours of admission. AMU is the centre for unscheduled care for Medicine. The AMU comprises 4 areas, each with it’s own maximum length of stay and admission criteria: - Emergency Assessment Unit (EAU : maximum length of stay 4 hours - Clinical Decision Unit : maximum length of stay 12 hours - Short Stay Ward : maximum length of stay 2 nights - Ambulatory Care Unit (urgent care without overnight stay) : urgent Ambulatory pathways, medical review, elective procedures This part of the rotation gives the trainee experience of assessing and managing all types of medical patients in the acute stage, as well as having many opportunities to undertake practical procedures under supervision. CT2 year The second year (CT2) consists of 6 months of Anaesthetics and 6 months of Intensive Care (ICM) or vice versa in either the William Harvey or the Queen Elizabeth the Queen Mother Hospital. There are 7 operating theatres in the main suite at the William Harvey including a dedicated emergency theatre staffed 24 hours a day. There is a Consultant present for emergencies continually from 8.30am to 10.00pm Monday to Friday. The Intensive Care Unit has 9 beds receiving approximately 700 high dependency and intensive care patients per year. There is also a separate obstetric theatre which is staffed 24 hours a day and a mobile theatre next to the gynaecological ward. There is also a stand alone day surgery unit with 3 operating theatres and a minor operations theatre. ST3 onwards Completion of the 2 year ACCS programme is followed by further training at ST3 level in either Emergency Medicine (the ACCS programme is the first 2 years of this curriculum) or Medical specialties with an emphasis on the acute management). Shift Practice and Rota 1. Emergency Medicine – William Harvey Hospital The department is staffed at senior level by 5 consultants and by 8 specialty doctors and 2 specialty trainees, with the speciality doctors and HST’s taking responsibility for 24 hour cover. The consultants are available for shop floor cover from Monday to Friday from 8.00am to 7.00pm. The CT1 ACCS post covers a rolling rota with a varying shift pattern over an 8/10 day block covering morning, afternoon, evening and night shifts followed by time off and also one weekend off in four. 2. Acute Medical Unit (AMU) – William Harvey Hospital The acute physician provides day to day leadership of the unit from 9 to 5, liaising with A&E, GPs and on call teams, and ensures that all roles are covered on the unit. The AMU team consists of 1 ST3 (Acute Medicine), 1 CT1 ACCS and 1 F1 supported by the on call team of Duty Medical Registrar, CT1/2, F2 and F1s in HCOOP / Medicine. The CT1 trainee will be expected to attend all ward rounds and Consultant reviews on the AMU and support the assessment and management of A&E / GP referrals under the direction of the AMU ST3 and Medical Registrar , liaising closely with the A&E team. The trainee will work across A&E / AMU/ Ambulatory Care depending on clinical need and be involved in day to day management of all patients on the AMU, including medical and HCOOP patients, and will also be expected to provide support and supervision to the F1s. He/she will work closely with the AcPhysician. The CT1 ACCS post on the ward involves responsibility for clerking patients and supporting ambulatory care procedures and medical reviews. The hours are 9am to 6pm, Monday to Friday with one weekend in four on duty from 9am to 9.30pm (Friday to Sunday). 3. Emergency Care Centre – Kent and Canterbury Hospital The Minor Injury Unit in the ECC is staffed primarily by Emergency Nurse Practitioners (ENPs). The Majors ECC team comprises: Consultant Acute Physician on duty. On-call Consultant Physicians for Medicine and Care of the Elderly. 4 Foundation Year 2 (F2) Doctors. The team is supported by Specialist Registrars, Medical SHOs or F2 doctors on-call. Foundation Year 1 (F1) doctor on-call. Nursing and technical staff. The Acute Physicians in the ECC provide cover Monday to Friday from 9am to 5pm and have 2 regular medical review clinics per week. The Medical and Elderly Care Consultants each lead 3 ward rounds in every 24 hour period. Patients needing a longer period of observation and/or assessment overnight are transferred to the adjacent ward within the ECC under the care of the oncall team and are then either discharged or admitted to appropriate wards in the hospital. Patients are assessed, investigated (including blood tests and Doppler scan) and treated in a single visit. Medical review is constantly available if deemed necessary. The ECC has a wide range of facilities including: A Resuscitation area with 4 beds. A Majors Bay with 12 beds. A Short Stay Ward with 18 beds. An area for the assessment of Deep Venous Thrombosis (DVT). The Minor Injury Unit (MIU). 4. Anaesthetics – William Harvey Hospital This department is staffed at senior level by 20 Consultants, 7 STs, 7 CTs, 1 Associate Specialist and 2 Staff Grades. There is a Consultant present for emergencies continually from 8.30am to 10.00pm, Monday to Friday. Day shifts are from 8.00am to 5.30pm and on-call 1 in 7, day shift 8.00am to 8.00pm and night shift 8.00pm to 8.00am covering emergency theatre, assisting with emergencies in A&E and elsewhere in the hospital. 5. Intensive Care Unit – William Harvey Hospital The critical care unit comprises of nine mixed ITU and HDU bed admitting over 750 patients per annum. The case mix is almost equal mix of medical and surgical patients with well over forty percent being ventilated. This unit is staffed by 5 Consultant Intensivists during the week, on a 1 week in 5 basis and by the Consultant Anaesthetist on-call, out of hours. The daily clinical activities include two daily consultant led ward round with multi-disciplinary participation form allied health professionals, daily consultant microbiology ward round and outreach support. The junior rota constitutes of six resident doctors providing full time shift with internal cover. There is a rolling rota over 6 weeks with a varying shift pattern of days from 8.30am to 5.30pm, lates from 8.30am to 9pm and night shifts from 8.30pm to 9.30am. Handovers are held during ward rounds at 8.30am and 4pm and at 9.00pm. Two of the residents are anaesthetic trainee, one ACCS trainee and one medical rotation trainee. The ACCS CT2 trainees work alongside Critical Care Fellows, usually from a medical background, Anaesthetic trainees and an F1 Doctor. A Foundation Year 1 doctor and medical students support the resident team. There is a 24 hours outreach service which extend the critical care services to the wards. Recent feedback from anaesthesia trainees has been very positive about their experience on the ICU. The Unit has already received positive feedback from the Regional Adviser and Deanery with respect to its teaching. 6. Anaesthetics – Queen Elizabeth the Queen Mother Hospital The QEQM has 6 main operating theatres, 3 day surgery theatres and an obstetric theatre. Case load includes general surgery, including (laparoscopic) colorectal surgery, trauma and orthopaedics, gynaecology (including major gynaecology oncology) as inpatients. Day surgery includes those mentioned and also ENT, maxillo-facial and ophthalmology. There is a 24 hour emergency theatre with consultant anaesthetist presence from 8am-10pm Monday-Friday. There is a daily dedicated trauma list 1:306pm Monday to Friday and at weekends 10am-4pm. The department is made up of 16 Consultants, 4 Associate Specialists, 6 Specialty Doctors and 12 trainees (including Core Anaesthetics, ACCS and ST doctors). Normal working days are 8am-6pm. On calls covering emergency theatres are from 1pm-11pm with a resident on call Consultant 8am-10pm. Weekend on call is from 9am-10pm. CT doctors do not do theatre on calls overnight. Currently the in-patient surgical specialists provided include lower G.I, orthopaedics, spine and trauma, gynaecology and obstetrics. Additionally, the Day Care Surgery Unit provides ENT, ophthalmics and maxillo facial. Acute and chronic pain services are also provided on site. And there is great emphasis regional block for orthopaedic & trauma surgery and a there is a stand alone bronchoscopy list supervised by Respiratory Physicians. There are some paediatric lists that encompass dental, maxillo facial, orthopaedic, general surgery, ENT and trauma. This hospital have 24hr A&E and as such experience will be gained in emergency general surgical and trauma lists. There is a separate Obstetric anaesthetic list . The ITU is recognised for core training. There is a separate ITU and HDU with critical outreach service. There are acute and chronic pain services. 7. Intensive Care Unit – Queen Elizabeth the Queen Mother Hospital The ICU is a 9 bedded unit which admits both elective and emergency cases and both surgical and medical patients. The unit is staffed by 4 Consultant intensivists during the week daytime and the on call Consultant anaesthetist overnight. The ACCS trainees will also be working with specialist doctors, an FY1 doctor and other CT anaesthetic trainees. Day shifts are 8am-5pm, long days are 8am-8pm and night shifts are 7:30pm-8:30am. Handovers are held during ward rounds at 8:00 AM, 16:00 PM and at 21:00 PM. Education and Study Schedule – William Harvey Hospital A variety of learning approaches are adopted, including web-based learning, ward and theatre based clinical teaching, group learning, private study, courses, reflective practice, audit projects and regular teaching specific to module. It is expected that trainees should attend specific teaching provided while in each rotation, immersing themselves in that specialty, however there will inevitably be some overlap due to the nature of the 4 specialties involved. Emergency Medicine - Weekly teaching sessions in the A & E Resource Room - Fortnightly speciality doctor teaching sessions Acute Medicine - Weekly Medical teaching sessions for all Medical STs and Registrars, the programme is fully mapped against the RCP curriculum and includes clinical scenarios and practical skills sessions - Weekly case discussions and literature reviews for all Medical STs and registrars Intensive Care Medicine - Weekly teaching round between 8.30am and 9.30am on ITU - Weekly tutorial session / Journal Club between 9.30am and 10.30am - Monthly Morbidity and Mortality meeting 12.30pm to 1.30pm (Anaesthetic Dept) Anaesthetics - Weekly tutorial session between 10.30am and 12.30pm - Monthly departmental / Audit meeting Other teaching available - Trauma and orthopaedic teaching every Friday lunchtime - Weekly Tuesday morning Paediatric teaching - Weekly Chest Radiology Seminars - Monthly Grand Rounds Kent and Canterbury Hospital Acute Medicine Weekly lunchtime medical teaching in the Education Centre. Grand round on the last Friday of every month and a medical directorate meeting on the other Fridays. Queen Elizabeth the Queen Mother Hospital Anaesthetics and Intensive Care There is weekly ward round teaching on the ICU on Wednesdays, followed by Anaesthetic Department teaching. There are also intermittent journal club meetings, M&M meetings and primary FRCA exam practice prior to trainees undertaking OSCEs and Vivas. There are also bi-monthly audit meetings. A variety of learning approaches are adopted, including webbased learning, ward and theatre based clinical teaching, group learning, private study, courses, reflective practice, audit projects and regular tutorial teaching . It is expected that trainees should attend specific teaching provided while in each rotation, immersing themselves in that specialty. Intensive Care Medicine/ Anaesthetics Weekly teaching round between 8.30 AM and 9.30 AM on ITU Weekly tutorial session / Journal Club/ case based discussions between 9.30 AM and 12:30 PM in the Anaesthetics department seminar room. Monthly departmental / Audit meeting. Research and audit Opportunities Trainees will be supported if they wish to pursue their audit and research interests and the anaesthetic department takes part in national research initiatives where possible. Name of the position and work needing to be done Qualifications and professional registration required Attach JD Anticipated duration of programme Commencement date Standard rotation details Year 1 - CT (SHO level ) in Emergency Medicine and Acute Medicine – 4 x 6 month rotations Year 2 - CT (SHO level) in Anaesthetics and Intensive Care Medicine – 4 x 6 month rotations Basic Medical Qualification (MBBS, MB ChB) Must be registered with the GMC 2 years – comprising of 6 months in each rotation August 2013 The CT1 trainee will either commence in Emergency Medicine or Acute Medicine (depending on exit specialty), rotating after 6 months in February with the other CT1 trainee. The CT2 trainee will either commence in Anaesthetics or Intensive Care Medicine, rotating after 6 months in February with the other CT2 trainee. Educational Supervisor Our Educational Supervisors in the ACCS programme are:CT1 Acute Medicine Emergency Medicine Acute Medicine CT2 Anaesthetics and Intensive Care Medicine Anaesthetics and Intensive Care Medicine Dr Indrani Chakraborti, Acute Physician, WHH Mr Jalal Maryosh, Emergency Medicine Consultant Dr Hardeep Baht, Acute Physician, KCH Dr Ranjit Dulai, Consultant Anaesthetist, WHH Dr Ravi Ramaiah, Consultant Anaesthetist, WHH Dr Tony Hodgetts, Consultant Anaesthetist QEQM An Educational Supervisor will be allocated to each trainee and will be responsible for overseeing training throughout the year, making sure that the trainee is making the necessary clinical and educational progress. It is the trainee’s responsibility to organise regular meetings with their Educational Supervisor which should take place in the first week or so of the job, at the mid-point and at the end of each specialty placement in order to: - Review progress to date - Ensure all appropriate assessments have been completed - Review which competencies have been met - Review / amend professional development / learning plan - Ensure all relevant documentation has been completed - Provide careers guidance The Educational Supervisor is responsible for: - Bringing together the structured report which looks at evidence of progress in training including assessments. - Undertaking regular appraisals with the trainee - Preparing the annual trainer’s report with the Training Programme Director for presentation to the ARCP panel at the deanery If the Educational Supervisor has any concerns about a trainee’s development / progress this will be raised in the first instance with the trainee and subsequently, if necessary with the Training Programme Director and the Specialty Faculty Group and then through the Local Academic Board to the Deanery. This is to ensure that the appropriate support is provided as it is common for trainees to experience difficulties and should only become a problem if help is not sought at an early stage. Both HEKSS and London Deaneries publish guidelines for ‘Trainees in Difficulty’ which: - Advise on the management of doctors in Deanery funded training posts - Bring together in one place a number of resources and details of relevant national and local initiatives - Covers both trainees in difficulty and those with additional needs - Offers the trainees support and guidance All Educational Supervisors at East Kent are required to participate in the Qualified Educational Supervisor Programme which is a Deanery initiative established to enhance the quality of teaching. The programme consists of two parts: Part 1: Certificate in Teaching Part 2: Certificate in Educational Supervision All of our Educational Supervisors are QESP Part 1 and 2 qualified. Clinical Lead Dr Bandipalyam Prathibha – Director of Medical Education Dr Ravi Ramaiah – Local Faculty Lead, ACCS Dr Scott-Russell – College Tutor, Medicine, William Harvey Dr Mark Fenton – College Tutor Medicine, Kent and Canterbury Dr Christina Schneider-Smith – College Tutor, Anaesthetics, William Harvey Dr Rini Poddar – College Tutor, Anaesthetics, Queen Elizabeth the Queen Mother Hospital Dr Madelaine Coupe – Local Faculty Lead, Anaesthetics Mrs Maggie Batchelor – ACCS Programme Administrator Outcome CCT/CESR/CP/Core Outcome of training programme i.e. core competencies Payments/Policy Salary Scale To achieve the core competencies required for progression on to the next year of training.