1 TREATMENT The Treatment of Borderline Personality Disorder
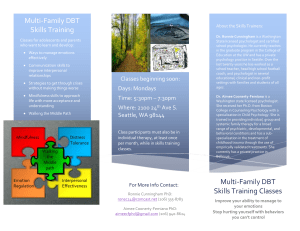
advertisement

TREATMENT The Treatment of Borderline Personality Disorder with Dialectical Behavior Therapy Catherine DuPuy HSJ 5620.2 John F. Kennedy University Spring 2012 TREATMENT 1 The term Borderline was originally coined as a descriptive for a disorder considered to be on the ‘borderline’ between neurosis and psychosis. These clients are notoriously difficult to treat in part because many display suicidal tendencies, are often in crisis, and are emotionally dysregulated. They have a desire to seek help yet find it difficult to commit to staying in therapy long enough for a treatment plan to work. In addition, they are extremely sensitive to anything they perceive as criticism, making working with this population often frustrating. For the therapist, it can lead to burned out and at times, resentment toward the client. Dialectical Behavior Therapy was developed to work to address these issues for both the therapist and client, and to date, is one of the most effective modalities therapists have for working with this populations and the issues they present, for themselves, and in the therapeutic environment. Marsh Linehan developed dialectical Behavior Therapy, or DBT for short, in the early 1980’s. She created what she termed the biosocial theory of emotional dysregulation, proposing that BPD develops from a biological vulnerability and a subsequent invalidating environment. According to Linehan, people who are biologically vulnerable experience emotions more intensely than others, reacting more frequently and with a higher sensitivity to their emotions. Lastly, they experience a longer lasting arousal than others not so vulnerable. These are also the characteristics of a someone suffering from PTSD. Affect dysregulation is the hallmark of those suffering with Borderline Personality Disorder. This is the inability to control one’s emotions, and those emotions then overwhelm a BPD’s ability to think and reason. Emotions are often expressed in an intense way, with little to no ability to moderate them. BPD’s suffer from a host of other TREATMENT 2 issues, including identity problems, unstable relationships, poor impulse control, and feelings of emptiness and little to no sense of self, frequenting leading to self-harming behavior and suicide attempts. They fear abandonment and will go to any lengths to avoid it, yet their emotional instability guarantees rocky and problematic relationships. Relationship difficulty extends to all areas of their lives, including interpersonal, love or work relationships. Research has been ongoing into the etiology of this disorder, and many believe (van Dijke, Ford, J.D., van Son,M., Frank,L., van der Hart, O. ,2012) that for many people with BPD, early childhood trauma is the root. Trauma can include the following; dysfunctional family dynamics, caregivers (mom usually) depressed and erratic, absent fathers or fathers with major character problems, and early losses (Rathbun). Child sexual abuse plays a large part in the development of BPD, as victims are at a higher risk for developing BDP, “childhood abuse and neglect are extremely common among borderline patients: up to 87% have suffered childhood trauma of some sort, 40–71% have been sexually abused and 25–71% have been physically abused (Winston, para. 4, 2000). For Linehan, environment plays as much a part in the development of BPD as a biological vulnerability. And the evidence supports her in this, as it clearly indicates that children who have been traumatized, be it sexual or physical abuse, or in repeated hospital stays and operations, or other early childhood trauma, are at a much higher risk to develop BPD. In a recent study of female inmates, it was found that trauma played a critical role in the development of BPD. “Bpd has been linked to elevated rates of trauma among female offenders” (Blonigen, D. Sullivan, E., Hicks, B., Patrick, C., para. TREATMENT 3 7, 2012). Further, “ the majority… experienced at least one form of abuse in their lifetimes” Blonigen, D. Sullivan, E., Hicks, B., Patrick, C., para. 12, 2012). Perhaps one of the more tragic components of childhood trauma is it’s effect on the developing brain. Research has shown that “chronic trauma interfers with neurobiological development and the capacity to integrate sensory, emotional and cognitive information in a cohesive whole” (van der Kolk, para. 7). It is a setup for the development of many disorders, including BPD. Research based on attachment theory is beginning to elucidate the links between childhood trauma and the capacity to think about oneself and others. Borderline patients are usually preoccupied with their disturbed early relationships and are unable to give a coherent account of them. Severe childhood trauma in these patients appears to result in a specific inability to think about their own thoughts and feelings, as well as those of others. (Winston, para. 7, 2000). Children who are lucky enough to be raised by a ‘good enough’ caregiver are able to model their behavior after hers, and when the child becomes emotionally distraught and dysregulated, Mom is there to calm and soothe the child, and help them to restore a sense of safety and control, over both themselves and their environment. They grow up trusting themselves and trusting that the environment will meet their needs. These early patterns of attachment will affect the quality of information processing throughout the child’s life (van der Kolk, para. 9) and allow the child to learn to trust what they feel and what they think in any given circumstance. However, for children raised in what Marsha Linehan calls an invalidating environment, an environment that can be dismissive, neglectful, violent, inconsistent or abusive, the child can become very distressed with no sense that their external environment can or 4 TREATMENT will provide relief. “As a result, they experience feelings of anxiety, anger and the strong desire to be taken care of” (van der Kolk, para. 15), note the Borderlines need for relationship and fear of abandonment. She does not learn safety and she cannot control herself as it is not being modelled for her. Under these conditions, the child does not learn to moderate her arousal and she is unable to process, integrate and understand what is happening. Children who grow up under these conditions experience an insecure attachment and this same emotional instability is the foundation for Borderline Personality Disorder. Like the suicide attempts of the teen ager and later adult, for the child, their problems and their reaction to them can be seen as an attemp to minimize the objective threat and regulate their emotional distress (van der Kolk, para. 16). For children like this, emotional dysregulation leads to a poor sense of self, poor impulse control and agrression towards themselves or others. They have not been given, by appropriate modelling, the tools to understand the cause and effect of their behavior and/or what their relationship to their behavior and the environment around them is. “Without internal maps to guide them, they act, instead of plan, and show their wishes in their behaviors, rather then asking for what they want” (van der Kolk, para. 22). A traumatic childhood can be, and often is, a set up for the development of Borderline Personality Disorder. The DSM–IV ‘s diagnostic criteria for borderline personality disorder is as follows: At least five of: Intense and unstable personal relationships Frantic efforts to avoid real or imagined abandonment TREATMENT 5 Identity disturbance or problems with sense of self Impulsivity that is potentially self-damaging Recurrent suicidal or -suicidal behavior Affective instability Chronic feelings of emptiness Inappropriate intense or uncontrollable anger Transient stress-related paranoid ideation or severe dissociative symptoms DSM–IV (American Psychiatric Association, 1994) Dialectical Behavior Theory proposes that people with BPD are attempting to regulate their behavior, even if we see it as dysregulated, problematic and disordered. Further, it states that invalidating behavior helps to further it and that common patterns develop in attempting to both live and regulate behavior. These patterns become problems unless treated (Koerner, p. 12, 2012). The theoretical framework for DBT is dialectics, which is “both a view about the nature of reality and a method of persuasion. It is an essential idea that any one position contains its antithesis” (Koerner, p 15, 2012). It is in simpler terms, a “way to achieve balance” (Linehan, 1995). Clients are both accepted for who they are, where they are, and at the same time, encouraged to change behavior that does not work for them. Validation is critical to DBT, as it sees behaviors like suicide attempts as the best the client can do for now. In the film Girl, Interrupted, Winona Ryder says to her therapist “I wasn’t trying to kill myself, I was trying to make the shit stop” (Girl, Interupted, 2008). The “shit” in this case is an emotional life out of control. DBT is based on Cognitive Behavior Therapy, which is a therapy geared toward change oriented strategies. DBT adds the element of mindfulness, as well as TREATMENT 6 acceptance strategies, because, borderlines are so sensitive to criticism and negative feedback, that simply working from a change strategy will meet with great resistance and the client will likely leave therapy. Understanding that borderlines are coming from a place of skills deficits – they do not know how to do things any other way, goes a long way in working with them. If they are met where they are, if they are accepted for what they have attempted in the past (even when it fails) and when the therapist understands how hard it has been for them, and expresses that, then agreement to work toward change becomes a possibility (Linehan, 1995). This is the philosophical difference between DBT and other theoretical perspectives, the notion of direct acceptance. Within the seed of that idea, comes the notion of change. Hence the dialectic. Saying to a client “people who meet criteria for borderline have skills deficits or capability deficiency, that they don’t have the ability to engage in the behaviors that they need to dissolve their problems. What I’m thinking is that what we have to do, is teach you something new to do, what do you think?” (Linehan, 1995) is a welcoming and understanding perspective, one that encourages possibilities. From here is possible to bring the client on board in the treatment, by asking if they then want to learn something new. DBT is based on a hierarchical structure with 4 primary components; individual therapy, group skills therapy, telephone consults and therapist group therapy/support. These 4 modes of treatment have been one of the most effective modalities for treating those with Borderline Personality Disorder. Individual Therapy TREATMENT 7 Individual therapy begins with what is termed the ‘pretreatment stage, where the client and the therapist agree (contract) to the essential goals and the methods of treatment. The therapist explains (to the extent they can in this initial session) what DBT is all about. The contract may not be written down, but it is essential that both parties understand and agree to it. This agreement will take into consideration what precisely is the current problem(s) for the client, and will include expected and set time frames for treatment results as well as when scheduled sessions are, what they cost, etc. The therapist will also include what he/she is agreeing to, which might include needing extra training, abiding by the highest ethical standards and that they will be participating in a BDT consult group. When this agreement is in place, formal treatment begins. DBT has 4 stages, not all of which any one patient may go through. The first stage is for the most critical clients, though given a borderlines resistance, most clients, even if not suicidal, will start here. This stage targets behaviors that the client is doing that are life threatening, for instance, suicide attempts, and cutting behaviors, or burning themselves with cigarettes. DBT defines treatment goals as the desired end point for a stage of treatment, for example, in Stage 1, a treatment goal would be choosing not to kill oneself (or do other self-injurious behaviors). A ‘target” is defined as behaviors that have been identified (by the therapist, therapist consult team, or the client) as needing to change. That change may be either increasing the behavior (for example, learning to sit with ambiguity) or decreasing behaviors (tolerating distress without blowing up or raging at someone). Stage 1 decrease life threatening behaviors TREATMENT 8 Decrease therapy-interfering Decrease quality of life interfering behaviors (this can include Axis 1 disorders as well as issues around housing, relationships, work, or legal problems. Increase behavioral skills (some of these are taught in skills groups) o Mindfulness o Distress Tolerance o Interpersonal effectiveness o emotional regulation o self-management (Koerner, p. 25, 2012) It should be no surprise that DBT starts targeting self-harm behaviors right away, as DBT was created to deal with suicidal borderlines. Like many therapies, DBT expects the client to commit to a no suicide pact, but in DBT, the contract is usually for a year, and unlike most other therapeutic interventions, DBT therapists are available to their clients (regardless of the stage) by telephone for consultation when the need arises. In a 2003 study done in Sweden, borderline clients found the therapeutic contract beneficial and supportive. The contract “postulates progress in therapy as a criterion to continue”, pushing them to work on their issues. One (unnamed) study participant said “If I’ve signed a paper it feels like more of a commitment not to let myself or the therapist down” (Perseius, para. 23, 2003). Identifying behaviors that can or do interfere with therapy is the second in this hierarchy. DBT recognizes that borderlines have a tendency to shoot themselves in the foot, and drop out of therapy when it’s gets hard, and this is where the acceptance and TREATMENT 9 change model comes into play. Clients are helped (through individual, group and phone calls) in their commitment to their own process. The therapy will target any of these behaviors with specific goals to stop their occurrence. The therapist is also involved in helping the client resolve life issues they may be having, usually as a result of their skills deficit. To a borderline, a job interview may seem overwhelming, and with the help of the therapist and the skills group, the client can begin to try out new behaviors, because a critical component of DBT is the ability to translate what one has learned in the rooms, to the outside world. This is where Linehan sees other treatment modalities as failing the borderline. “Treatment programs fail because they don’t pay enough attention to getting the behaviors learned in therapy into the real world, where they have got to have them” (Linehan, 1995). Lastly, the therapist and client begin to identify and work on a set of skills that will help the client begin to be a bit more comfortable in the world. It is this step in the stage one hierarchy that also sets DBT apart from other evidence based methods. Here mindfulness is introduced. Linehan is not talking about asking a client to learn to sit in meditation, though she is a student of Zen herself. Rather, what is asked of the client is that they begin to inculcate an awareness into their lives that they begin to question, in the moment, what they are feeling or doing. As the therapist has worked in the room on acceptance of the client where they are, so now the client begins that same process of acceptance “by practicing mindfulness skills, clients become increasingly able to willingly and nonjudgmentally engage with their immediate experience” (Koerner, p. 20, 2012). Because this population can be difficult and triggering to work with, DBT expects that it’s therapists are practicing all the elements itself, including mindfulness. TREATMENT 10 Stage 1 can last for a year or more, depending entirely on the client, therapist and the peer consult group. Below is a diagram of how DBT views the development of BPD. AN ETIOLOGICAL MODEL OF BORDERLINE PERSONALITY DISORDER (Winston, 2000) The next stage, Stage 2, is completely dependent on the stability of the client. It is possible that the client will move in and out of this stage as their work with their own trauma begins. Stage 2 involves a good deal of exposure therapy, and for many borderlines, that can be quite difficult. Starting small and building on successes is the best way to approach this and understanding that the client may move back to stage one (anywhere on the hierarchy) is critical. Continuing to meet the client with acceptance (validation for the difficulties they are experiencing) and change (giving them the skills they need to work through their trauma) is what this stage entails. Estimates are that 36-58% of people with borderline personality disorder are also suffering from PTSD. Because of the reactivity of clients with BPD, assessing the readiness of the client is critical at this stage. Stage 2 is not hierarchical, but is TREATMENT 11 prioritized based on the individual client needs, and it is about decreasing symptoms like emotional dysregulation, invalidating the self, and avoiding situations or feelings that have been troublesome in the past. Clients may or may not stay in therapy for the last 2 stages and Linehan herself has written and researched little about them. In stage 3, she sees the therapist helping the client to synthesize all the work that has gone before, helping the client to begin to take her place in the world, to develop a sense of respect for herself and her process and to work on any remaining issues around living. Stage 4 dips down again into the client’s inner world, focusing on “the sense of incompleteness” (Koerner, p. 24, 2012) that many people with BPD experience. Mindfullness continues to be helpful at this stage, and for clients reaching stage 4, developing a spiritual life becomes possible as they begin to work with and perhaps give up, notions about the ego. Dialectical Behavior Therapy is not an easy methodology, especially for the new trainee. There are fail points within it, not the least is the notion of ‘peer group support’. The theory is that a team of experienced DBT therapists meets once a week to support each other in working with their borderline patients. However, this presupposes a number of things; that a therapist needing help will speak up in the group, and speak up consistently. But what happens if the therapist feels they are taking up too much of the group time, week after week, or if the therapist is simply unwilling to speak up for fear of being judged (some may have a supervisor in this group) or just not wanting to appear ignorant? And the question must be asked; do all who practice DBT have such a group? It is a major component of practicing BDT, but it seems that that would be dependent on geography and the number of DBT therapists near you. TREATMENT 12 Further, it remains unclear exactly how to help resistant clients. The DBT rule is if you miss 4 sessions you are out, but how do you deal with those clients who show up late, who do not pay, who are disruptive within the session? Clearly getting by in from the client is critical, but that may not be an easy thing to accomplish with borderlines. Telephone support, another critical component of this therapy that helps build essential skills, may also prove difficult. Borderlines by definition have difficulty with boundaries and giving them free access to their therapists, especially new therapists, could be fraught with problems. How does one manage the client who calls in such emotional dysregulation that she/he cries for 20 minutes (Rizvi, 2010)? It may be difficult to validate a client when they are so dysregulated you have trouble understanding what they are saying The phone calls are (according to the manual) to last between 5 – 10 minutes. But if you are concerned the person is going to kill himself or herself, or they are saying they are going to kill themselves, where do you draw the line? And if these calls come once a day or several times per day, how is that to be managed? Which of course can lead to a greater issue, that of remaining (as the therapist) in a positive frame of mind to work with such clients. DBT currently has the best track record for decreasing suicidality among the borderline population, but it is by no means (as is true of all theoretical systems) foolproof. Expanding the model for instance, perhaps simplifying it or integrating it with other models being developed (IFS – internal family systems) might be worth investigating. Keeping an open mind to what works as this disorder becomes more understood, especially from a trauma perspective, seems a good approach. 13 TREATMENT References Blonigen, D. Sullivan, E., Hicks, B., Patrick, C. (2012). Facets of Psychopathy in Relation to Potentially Traumatic Events and Posttraumatic Stress Disorder among Female Prisoners: The Mediating Role of Borderline Personality Disorder Traits. Personality Disorders: Theory, Research, And Treatment , 10. Cassidy, J. S. (Ed.). (2008). Handbook of Attachment. New York, NY: The Guilford Press. Gunderson, J. (2008). Borderling Personality Disorder. Washington, DC: Amercian Psychiatric Publishing. Diagnostic and Statistical Manual of Mental Disorders, Fourth Edition. American Psychiatric Association. 1994. Johnson, S. (1994). Character Styles. New York, NY: W.W. Norton & Company. Kiehn, B. S. (n.d.). An Overview of Dialectical Behavior Therapy in the Treatment of Borderine Personality Disorder. Retrieved from Dialectical Behavior Therapy: www.priory.com/dbt.htm Koerner, K. (2012). Doing Dialectical Behavior Therapy. New York, NY: The Guilford Press. Linehan, M. (1995). Treating Borderline Personality Disorder. The Guilford Press. Perry, B. (2001). Bonding and Ataachment in Maltreated Children. Retrieved May 1, 2012, from www.ChildTraumaAcademy.org: www.ChildTrauma.org Perseius, K. A. (2003). Treatment of Suicidal and Deliberate Self-Harming Patients with Borderling Personality Disorder Using Dialectical Behavioral Therapy: The Patients' and the Therapists' Perceptions. Archives of Psychiatric Nursing , XVII, pp 218-227. TREATMENT 14 Rathbun, J. (n.d.). Borderline Personality Disorder. Retrieved 2012, from BPD Today: www.borderlinepersonalitytoday.com Rizvi, S. (2010). Treatment Failure in Dialectical Behavior Therapy. Retrieved 2012, from ScienceDirect: www.sciencedirect.com Trauma and defense in the etiology of borderline personality disorder. In Borderline Personality Disorder: Etiology and Treatment (ed. J. Paris). Washington, DC: American Psychiatric Press. van der Kolk, B. (n.d.). Develpomental Trauma Disorder. Psychiatric Annals , pp 2 - 8. van Dijke, A., Ford, J., van Son, M., Frank, L., & van der Hart, O. (2012). Association of Childhood-Trauma-by-Primary Caregiver and Affect Dysregulation with Borderline Personality Disorder Symptoms in Adulthood. Psycholgical Trauma: Theory, Research, Practice, and Policy , pp 1-8. van Gelder, K. (2010). the buddha & the borderline. Oakland, Ca: New Harbinger Publications, Inc. Wick, R. Ryder, W. (Producers). Mangold,J. (Director) (1999). Girl, Interrupted [Motion Picture]. United States: Columbia Pictures. Winston, A. (2000, June). Recent Developments in borderline personality disorder. Retrieved May 2012, from Advances in psychiatric treatment: http://apt.rcpsych.org/content/6/3/211.ful#sec-13 Contact Information for Catherine: cdupuy3@me.com