Term Paper- DBT
advertisement

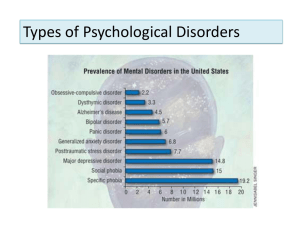
Professor Goldberg PSY 101 October 25, 2011 Treatment of Borderline Personality Disorder With Dialectical Behavior Therapy Borderline personality disorder (BPD) is a chronic and severe mental illness that is becoming more common among teens and young adults. It is estimated that about 25% of the general population are affected by this disorder (Selby, Joiner 219). Frequently patients with borderline personality disorder meet the DSM criteria for other psychiatric illness as well, such as major depression, anxiety disorders, post-traumatic stress disorder, and eating disorders (Lieb et al. 454). This usually makes it more challenging to diagnose BPD and the illness remains untreated. The American Psychiatric Association defines BPD as “a pervasive pattern of affective instability and identity disturbance characterized by frantic efforts to avoid loss and diminish chronic feelings of emptiness that often takes the form of impulsivity and recurrent suicidal or self-mutilating behaviors” (Sneed, Balestri, Belfi 265). These persistent suicidal thoughts and behaviors along with self-mutilation are often referred to as parasuicidal and are most often associated with borderline personality disorder. Other common forms of impulsivity associated with BPD include substance abuse, disordered eating, spending sprees, verbal outbursts, and reckless driving. Along with impulsivity other criteria for borderline personality disorder include affective disturbance, disturbed cognition, and intense unstable relationships (Lieb et al. 453). There are several factors that can cause borderline personality disorder to develop. Genetics has been said to play a role in the onset of BPD, most particularly in twins. BPD can also be inherited from a parent who has borderline personality disorder. Events during childhood can also induce the onset of BPD, especially ongoing experiences of abuse or neglect. It is reported that “the most frequent of these is childhood sexual abuse, which is reported by 40-71% of inpatients with borderline personality disorder” (Lieb et al. 454). In 1993, Marsha Linehan, who later created dialectical behavior therapy, proposed a theory stating that individuals who are surrounded by an invalidating environment are more susceptible to developing BPD. When communication of emotional experience is met by erratic, inappropriate, judgemental, and extreme responses by others, individuals with BPD then develop an emotional vulnerability that results in heightened sensitivity to emotional stimuli, experiences emotions as extremely intense and a slow return to emotional baseline (Selby, Joiner 219). Linehan also pointed out that This development of emotion dysregulation resulted in the development of subsequent behavioral dysregulation (defined as behaviors that are difficult to control and result in impairment in the affected individuals functioning) …, these behaviors provide a way for an individual to shift attention away from unpleasant emotional states.” (Selby, Joiner 219) Because individuals with BPD constitute for a large group among suicide attempters and they tend to repeat their self-destructive behaviors, it is necessary for them to seek treatment. It is evident that because of the high risk behaviors associated with borderline personality disorder, psychotherapy is a necessity. Unfortunately many medical professionals are unaware of the challenges presented by this disorder. Joan Wheelis, M.D., who graduated from the Boston Psychoanalytic Society and Institute, stated that “My psychoanalytic training led me to focus on a patient’s resistances to insight rather than on the patient’s maladaptive responses to overwhelming affect..., When I felt ineffective at helping my patients I sought consultation and I was relieved and excited to learn about dialectical behavior therapy.” (325). Dialectical behavior therapy (DBT) focuses on manipulation the contingencies, which maintain problematic behavior in the present, which they may have been learned in the past. Like Cognitive behavior therapy (CBT), DBT does not recognize dynamic unconscious meanings or forces. Instead these theories try to understand behavior by studying its occurrence over time, what events precede and what follows a particular behavior. When Dr. Marsha Linehan developed DBT she added three important components to the standard CBT protocol. 1. A dialectical philosophy and methodology of treatment emphasizing the importance of acceptance and validation of behavior while promoting its change. 2. Mindfulness as a set of skills to focus attention as well as a philosophy borrowed from the Zen tradition to stay connected to the present 3. Significant attention is focused on the development and on the maintenance of a working therapeutic alliance. (Wheelis 328) Dialectical behavior therapy is currently the most frequently used psychotherapy for borderline personality disorder. The DBT program consists of multiple forms of therapy including individual therapy twice a week, a skills group once weekly, telephone coaching and case management, and supporting therapists’ motivation and skills with a consultation team once weekly. Individual therapy is focused on “promoting the motivation for change by detailed chain analyses, [teaching] validation strategies, and management of reinforcement contingencies” (Kliem, Kröger, Kosfelder 936). DBT therapists use a treatment target hierarchy to help determine the problem focus for each session. The reduction of suicidal gestures and self-injurious behaviors is given the highest priority, considering that these behaviors predict completing suicide. Therapyinterfering behaviors such as skipping appointments or lying are addressed next, followed by reduction in quality-of-life interfering behaviors, such as drug/alcohol use, and binge eating (Kliem, Kröger, Kosfelder 936). The primary goal of the weekly skills group is to increase target-oriented and appropriate behavior by teaching over 50 skills grouped into four separate modules, each designed to target a different area of skills deficits in BPD. (Neacsiu et al. 564). To aide the DBT therapist in helping the patient during individual session diary cards are used to monitor urges to engage in target behaviors as well as what skills the client practiced throughout the week. They are then reviewed in therapy each week and are used to determine the targets to be addressed in that session. Diary cards are also kept on file throughout treatment as a guide to the therapist on progress being made (Neacsiu et al. 566). During individual sessions, skills from the four modules are also reviewed to help reinforce them with the client. The four modules consist of core mindfulness, distress tolerance focusing on acceptance, interpersonal effectiveness focusing on change and finally emotion regulation (James et al. 149). Perhaps the most important module of skills in DBT is mindfulness. Marsha Linehan added mindfulness to the program because she believes that “an important element is the attention the therapists pay to the dialectic between validation and acceptance of the patients as they are, and at the same time helping them change” (James et al. 149). Mindfulness helps the individual be more in control of their thoughts and actions because it emphasizes staying in the present and focusing attention in the moment (Wheelis 329). This helps facilitate the experience of validation as well as tolerance and acceptance of change. The skill of validation is also focused on during DBT skills groups, which is “the process by which patients are given support for their experiences as their therapists convey their understanding of a patients behavior in view of a current situation or past experience” (Wheelis 329). Validation does not mean agreement, it simply states that you understand where the person is coming from or they are being heard. An example of this could be used with an individual who suffers from recurrent self-injurious behaviors. The therapist may validate this behavior by saying “I can understand how you could get to point” or “It must be really difficult to deal with those feelings so I can see why you would want to cut yourself”. Although dialectical behavior therapy was originally developed for treatment of borderline personality disorder, it has now been conceptualized as a useful treatment for a wider range of difficult to treat or multiple disordered patients. These include but are not limited to paranoid personality disorder, obsessive-compulsive personality disorder, avoidant personality disorder, non-BDP anorexia-nervosa, and chronic depression (Lynch, Cheavens 155). In general, “Dialectical behavior therapy is the most empirically supported treatment available for suicidal behaviors and nonsuicidal self-injury” (Harned et al. 421). Works Cited Harned, Melanie S.Jackson, Safia C.Comtois, Katherine A.Linehan, Marsha M. "Dialectical Behavior Therapy As A Precursor To PTSD Treatment For Suicidal And/Or Self-Injuring Women With Borderline Personality Disorder." Journal Of Traumatic Stress 23.4 (2010): 421-429. Psychology and Behavioral Sciences Collection. Web. 4 Nov. 2011. James, Anthony C.Taylor, Annie Winmill, Louise Alfoadari, Kielly. "A Preliminary Community Study Of Dialectical Behaviour Therapy (DBT) With Adolescent Females Demonstrating Persistent, Deliberate Self-Harm (DSH)." Child & Adolescent Mental Health 13.3 (2008): 148-152. Psychology and Behavioral Sciences Collection. Web. 4 Nov. 2011. Kliem, Sören, Christoph Kröger, and Joachim Kosfelder. "Dialectical Behavior Therapy For Borderline Personality Disorder: A Meta-Analysis Using Mixed-Effects Modeling." Journal Of Consulting And Clinical Psychology 78.6 (2010): 936-951. PsycARTICLES. Web. 4 Nov. 2011. Lieb, Klaus Zanarini, Mary C.Schmahl, ChristianLinehan, Marsha M.Bohus, Martin. "Borderline Personality Disorder." Lancet 364.9432 (2004): 453-461. Psychology and Behavioral Sciences Collection. Web. 4 Nov. 2011. Lynch, Thomas R.Cheavens, Jennifer S. "Dialectical Behavior Therapy For Comorbid Personality Disorders." Journal Of Clinical Psychology 64.2 (2008): 154-167. Psychology and Behavioral Sciences Collection. Web. 4 Nov. 2011. Neacsiu, Andrada D.Rizvi, Shireen L.Vitaliano, Peter P.Lynch, Thomas R.Linehan, Marsha M. "The Dialectical Behavior Therapy Ways Of Coping Checklist: Development And Psychometric Properties." Journal Of Clinical Psychology 66.6 (2010): 563-582. Psychology and Behavioral Sciences Collection. Web. 4 Nov. 2011. Selby, Edward A., and Thomas E. Jr. Joiner. "Cascades Of Emotion: The Emergence Of Borderline Personality Disorder From Emotional And Behavioral Dysregulation." Review Of General Psychology 13.3 (2009): 219-229. PsycARTICLES. Web. 4 Nov. 2011. Sneed, Joel R., Massimo Balestri, and Brian J. Belfi. "The Use Of Dialectical Behavior Therapy Strategies In The Psychiatric Emergency Room." Psychotherapy: Theory, Research, Practice, Training 40.4 (2003): 265-277. PsycARTICLES. Web. 4 Nov. 2011. Wheelis, Joan. "Mending The Mind." Psychoanalytic Dialogues 20.3 (2010): 325-336. Psychology and Behavioral Sciences Collection. Web. 4 Nov. 2011.