The Road to Endeavour Poster presentation
advertisement
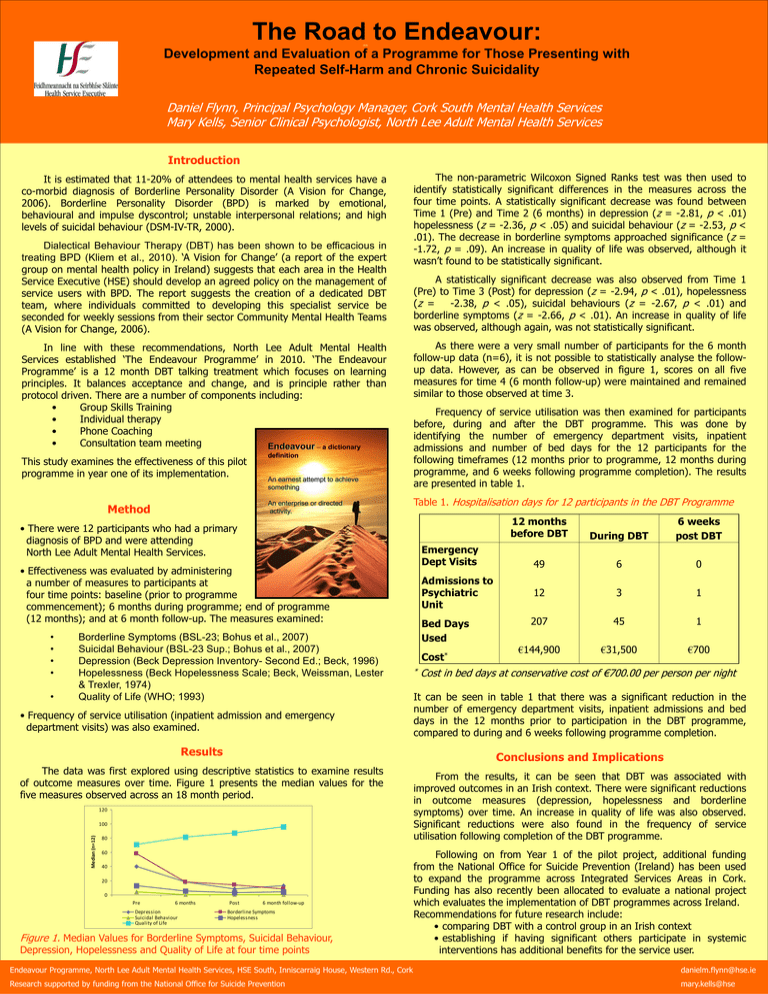
The Road to Endeavour: Development and Evaluation of a Programme for Those Presenting with Repeated Self-Harm and Chronic Suicidality Daniel Flynn, Principal Psychology Manager, Cork South Mental Health Services Mary Kells, Senior Clinical Psychologist, North Lee Adult Mental Health Services Introduction It is estimated that 11-20% of attendees to mental health services have a co-morbid diagnosis of Borderline Personality Disorder (A Vision for Change, 2006). Borderline Personality Disorder (BPD) is marked by emotional, behavioural and impulse dyscontrol; unstable interpersonal relations; and high levels of suicidal behaviour (DSM-IV-TR, 2000). Dialectical Behaviour Therapy (DBT) has been shown to be efficacious in treating BPD (Kliem et al., 2010). ‘A Vision for Change’ (a report of the expert group on mental health policy in Ireland) suggests that each area in the Health Service Executive (HSE) should develop an agreed policy on the management of service users with BPD. The report suggests the creation of a dedicated DBT team, where individuals committed to developing this specialist service be seconded for weekly sessions from their sector Community Mental Health Teams (A Vision for Change, 2006). In line with these recommendations, North Lee Adult Mental Health Services established ‘The Endeavour Programme’ in 2010. ‘The Endeavour Programme’ is a 12 month DBT talking treatment which focuses on learning principles. It balances acceptance and change, and is principle rather than protocol driven. There are a number of components including: • Group Skills Training • Individual therapy • Phone Coaching • Consultation team meeting Endeavour – a dictionary This study examines the effectiveness of this pilot programme in year one of its implementation. definition An earnest attempt to achieve something An enterprise or directed activity. Method The non-parametric Wilcoxon Signed Ranks test was then used to identify statistically significant differences in the measures across the four time points. A statistically significant decrease was found between Time 1 (Pre) and Time 2 (6 months) in depression (z = -2.81, p < .01) hopelessness (z = -2.36, p < .05) and suicidal behaviour (z = -2.53, p < .01). The decrease in borderline symptoms approached significance (z = -1.72, p = .09). An increase in quality of life was observed, although it wasn’t found to be statistically significant. A statistically significant decrease was also observed from Time 1 (Pre) to Time 3 (Post) for depression (z = -2.94, p < .01), hopelessness (z = -2.38, p < .05), suicidal behaviours (z = -2.67, p < .01) and borderline symptoms (z = -2.66, p < .01). An increase in quality of life was observed, although again, was not statistically significant. As there were a very small number of participants for the 6 month follow-up data (n=6), it is not possible to statistically analyse the followup data. However, as can be observed in figure 1, scores on all five measures for time 4 (6 month follow-up) were maintained and remained similar to those observed at time 3. Frequency of service utilisation was then examined for participants before, during and after the DBT programme. This was done by identifying the number of emergency department visits, inpatient admissions and number of bed days for the 12 participants for the following timeframes (12 months prior to programme, 12 months during programme, and 6 weeks following programme completion). The results are presented in table 1. Table 1. Hospitalisation days for 12 participants in the DBT Programme • There were 12 participants who had a primary diagnosis of BPD and were attending North Lee Adult Mental Health Services. Emergency Dept Visits • Effectiveness was evaluated by administering a number of measures to participants at four time points: baseline (prior to programme commencement); 6 months during programme; end of programme (12 months); and at 6 month follow-up. The measures examined: • • • • • Borderline Symptoms (BSL-23; Bohus et al., 2007) Suicidal Behaviour (BSL-23 Sup.; Bohus et al., 2007) Depression (Beck Depression Inventory- Second Ed.; Beck, 1996) Hopelessness (Beck Hopelessness Scale; Beck, Weissman, Lester & Trexler, 1974) Quality of Life (WHO; 1993) • Frequency of service utilisation (inpatient admission and emergency department visits) was also examined. Results 120 Median (n=12) 100 80 60 40 20 0 6 months Depression Suicidal Behaviour Quality of Life Bed Days Used Cost* * During DBT 6 weeks post DBT 49 6 0 12 3 1 207 45 1 €144,900 €31,500 €700 Cost in bed days at conservative cost of €700.00 per person per night It can be seen in table 1 that there was a significant reduction in the number of emergency department visits, inpatient admissions and bed days in the 12 months prior to participation in the DBT programme, compared to during and 6 weeks following programme completion. Conclusions and Implications The data was first explored using descriptive statistics to examine results of outcome measures over time. Figure 1 presents the median values for the five measures observed across an 18 month period. Pre Admissions to Psychiatric Unit 12 months before DBT Post 6 month follow-up Borderline Symptoms Hopelessness Figure 1. Median Values for Borderline Symptoms, Suicidal Behaviour, Depression, Hopelessness and Quality of Life at four time points From the results, it can be seen that DBT was associated with improved outcomes in an Irish context. There were significant reductions in outcome measures (depression, hopelessness and borderline symptoms) over time. An increase in quality of life was also observed. Significant reductions were also found in the frequency of service utilisation following completion of the DBT programme. Following on from Year 1 of the pilot project, additional funding from the National Office for Suicide Prevention (Ireland) has been used to expand the programme across Integrated Services Areas in Cork. Funding has also recently been allocated to evaluate a national project which evaluates the implementation of DBT programmes across Ireland. Recommendations for future research include: • comparing DBT with a control group in an Irish context • establishing if having significant others participate in systemic interventions has additional benefits for the service user. Endeavour Programme, North Lee Adult Mental Health Services, HSE South, Inniscarraig House, Western Rd., Cork danielm.flynn@hse.ie Research supported by funding from the National Office for Suicide Prevention mary.kells@hse