Autoantibodies in Connective Tissue Disease
advertisement

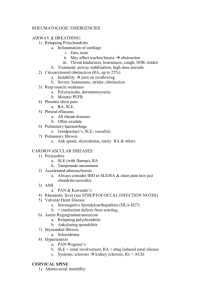
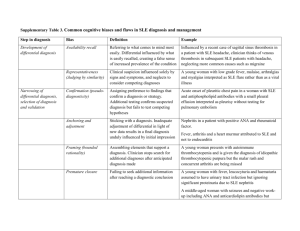
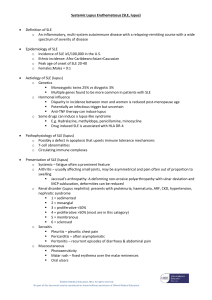
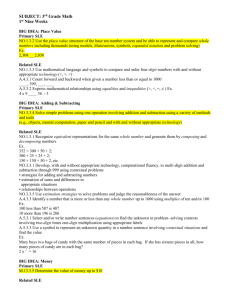
Autoantibodies in Connective Tissue Disease Antibody Associated Disease Interpretation Indication to order Testing Technique DS DNA = nDNA -High level (>2-3 std dev, 1:320) confirms clinical dx of SLE -Low level in RA, Hashimoto, Graves, Waldenstrom, MCTD, SSc, AI liver dx, SS -Low diagnostic value -Increased in childhood linear morphea -+ in many CTDs -+ in only 50-80% of SLE -assoc with renal dz in SLE - high value = specific for SLE -Question of SLE - + in normal people - want > 3 std dev to be significant - Rarely -indirect IF: uses crithidiae mitochondria which only has dsDNA (so + or – only) - elisa: uses calf thymus, increased sensitivity, gives a value - elisa: check by anti-DNA ab that is further extracted to SSDNA from calf thymus - Drug induced SLE (90%+) - SLE (30%+) -SS -SLE -SCLE (70-90%) - Increased with vasculitis - Drug induced SCLE* -same as RO, but incidence 50% less -MCTD (100% by definition) -SLE (30%) -Rarely neonatal LE, SS -SLE (very specific/diagnostic) -Only 15-40% + in SLE - cannot exclude idiopathic SLE if + - if suspect drug induced SLE - correlates with photosensitivity in SCLE - incidence varies with testing technique -w/u for photo-sensitivity -suspicion of neonatal LE, SS -suspicion of SCLE or SLE with negative ANA -IF: uses animal substrate like liver - elisa: uses commercial histone complement fixation -Radial imunodiffusion: high spec, low sens (must contain lg amt to be +, so + = high diagnostic value) -Elisa: low spec, high sens (+ = low diagnostic value unless 2-3 std dev, but gives quantitative value) -90% of pts with +LA have +RO -is to exclusion of other abs in MCTD -majority have SLE b/c SLE > MCTD -same as RO -attempting to confirm MCTD or SLE -same as RO -same as RO -confirms SLE -+ SM = + U1RNP -+U1RNP not = + SM -marker for worse dz (compared to just CREST) -specific for SSc - only 2% SSc have positve -associated with pulmonary sxs in SLE -attempting to confirm SLE -same as RO SS DNA Histones Anti- RO, SSA Anti-LA, SSB U1RNP Anti-SM SCL 70 (aka anti-topoisomerase) Anti-centromere JO-1 (aka anti-histidyltRNA synthase) -SSc (incidence 10-20%) CREST (50-90% positive) -Dermatomyositis, polymyositis -SLE -to distinguish bad SSc from less bad Suspect CREST nDNA, native DNA; SLE, systemic lupus erythematosus; RA, rheumatoid arthritis; MCTD, mixed connective tissue disease; SSc, systemic sclerosis (scleroderma); AI, autoimmune; SS, sjogren’s syndrome; IF, immunofluorescence; *drugs assoc = hydrochlorothiazide, ACE inhibitors, Ca channel blockers, interferons, statins (Archives of Dermatology Jan 2003) taken mainly from JAAD Nov 2000, CME ANA Patterns and their Antigens and Disease Associations ANA Predominant antigen Disease Peripheral Homogenous Nucleolar Centromere Speckled nDNA nDNA, histones Nucleolar RNA Kinetochore Various ribonucleic proteins SLE SLE SSC, SLE CREST SLE, SSc, SS Positive ANA in a healthy population Conditions other than CTDs with positive ANA Titer 1:40 1:80 1:160 1:320 Elderly persons Pregnancy Relatives of patients with CTD Other autoimmune disease (autoimmune thyroiditis, pimary biliary cirrhosis) Chronic infections Prevalence 32% 13% 5% 3% Neoplasms Medications (procainamide, hydralazine) Normal healthy individual