1) depressed mood most of the day, nearly every day, as
advertisement

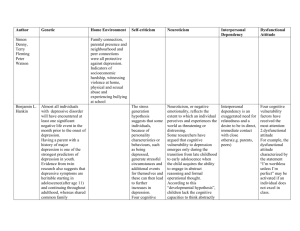
It Just Depression Scam This a moot point because with the deterioration seen in the dorsolateral prefrontal cortex as a result of chronic pain, the mood problems could just a secondary phenomenon. abstract here Damage to that area can be induced through Interferon drug therapy; half the cases will develop depression. It has been suggested that those more “predisposed” to depression seem more susceptible to depression from this brain damage. This does not discount its role anymore than a thin boned person getting a hip fracture from a fall just because his/her bones are thin. There has been much debate over the fact much so called depression in chronic pain is actually just what you would expect – distress over an illness pain sufferers are ill equipped to handle. This is reflected by a review of the following article: Fishbain DA, Cutler R, Rosomoff HL, Steele Rosomoff R. Chronic pain associated depression: antecedent or consequence of chronic pain? A Review. Clin J Pain 1997;13(2):116±136. “Fishbain et al. (1997) recently reviewed the pain-depression literature in order to determine whether depression precedes or follows the development of chronic pain. Forty-one studies were found which supported the concept of pain leading to depression and many of these studies indicated that depression improved following improvement in pain. Pain may, therefore have a very powerful `state' effect in terms of leading to and modulating depression.” It would make sense that chronic pain would wear someone down, but that does not necessarily stop insurers trying to conclude it is all in claimant’s head. The usual tests scales for depression were never designed to be used in chronic pain cases. The concern is articulated here: “All the reviews describe difficulty in accurate and appropriate measurement of negative mood in pain patients. Whether research uses self-report questionnaires or clinician-administered inventories and diagnostic interviews; whether depression or anxiety is the sole subject of the questionnaire or constitutes a subscale within a generic questionnaire; and whether the scale was developed in psychiatric or medical populations, there is still no measure (a) designed for (non-psychiatric) pain populations and (b) which measures emotional well-being, in the form of positive affect, alongside negative mood. In addition, many self-report instruments contain somatic items, which are known to inflate scores in pain populations (Bradley, 1994; Morley et al., 2002; Pincus and Williams, 1999; Pincus et al., 1996; Vahle et al., 2000).”….” As with depression questionnaires, anxiety questionnaires have been developed and validated on normal and psychiatric populations and their application in pain populations may be misleading.” “the widely used Beck Depression Inventory (BDI: Beck et al., 1961) suffers from all the problems outlined in our introduction (Morley et al., 2002): it contains items on sleep, fatigue, appetite, weight, and health concerns, and on work and sexual activity, which may be more related to pain problems than to mood (Wesley et al., 1991, 1999; Williams and Richardson, 1993); it was developed in psychiatric populations from which those with physical illness were explicitly excluded; and respondents can score no better than not depressed.” Asking Psychological Questions that people will have just because they are in pain is called “criterion contamination”. This will lead to erroneous diagnoses or worse psychological labeling of someone who is just sick. Some questions in depression with questionable accuracy from: Pain 109 (2004) 181–188 The development and testing of the depression, anxiety, and positive outlook scale (DAPOS) Tamar Pincusa, Amanda C. de C. Williams, Steven Vogel, Andy Field abstract here Beck Depression Score Inaccurate questions: Weight loss Lack of appetite Difficulty sleeping Feeling Irritable Feeling Tired Uncontrolled crying Concerns about health Loss interest in sex Able to work Loss of Interest in others Answering high positive to all these “questionably accurate” questions would place someone in a severely depressed range where it may only mean they are in severe pain. The Official Criteria for depression cannot be easily applied to someone in chronic pain: For a proper diagnosis one is required to have: 1) must have either answer 1 or 2 below and 2) five items altogether They include: 1) Depressed mood most of the day, nearly every day (2) Markedly diminished interest or pleasure in all, or almost all, activities (3) Significant weight loss NOT VALID (4) Sleep disturbance NOT VALID (5) Psychomotor agitation or retardation nearly every day (6) Fatigue NOT VALID (7)Feelings of worthlessness or excessive or inappropriate guilt (8) Diminished ability to think or concentrate, or indecisiveness (9) Recurrent suicidal ideation With 3 of the 9 criteria invalid, one is left with 6 items of which 5 are needed for a diagnosis. A similar problem was encountered with cancer patients where items concerning weight loss and fatigue had to be automatically eliminated. There are a few caveats required in interpreting the remaining depression criteria questions. 1) People with chronic pain don’t enjoy life like the used to. Life can be very boring without money, and energy; and the pain can prevent many prior pleasurable activities. With poverty, they are often can no longer afford a car so getting out becomes a major undertaking. Depression scores finding lack of enjoyment need to take that into account. 2) If you were to take normal subjects and deprive them of 15% of their sleep a day, within a short time, their optimism and sociability lessen and irritability increases. I am always amazed how much “depression” can disappear with proper sleep. 3) Concentration does decline in chronic pain. Pain, lack of sleep, and medications can all majorly impact of this. One anticonvulsant used in chronic pain has been nicknamed by some “the stupid pill” because it can blunt mental functioning. Finding decreased concentration has to take that into account. 4) The life of someone with pain is one of victimization. It is called the “invisible disability”; they look fine but suffer. This causes considerable scorn from friends, co-workers, employers, insurers, physicians and family. Life in effect can be hell. Workman’s Compensation Victims were followed for 1 year in this Ontario study called: “Victims twice over” – not only are they victims of an injury, they are victims of a punitive process. “Interviewees believed that the process victimizes them and renders them powerless and dependent on others.” Qual Health Res. 2005 Jan;15(1):30-48. Victims twice over: perceptions and experiences of injured workers. Beardwood BA, Kirsh B, Clark NJ. abstract here This in itself is going to be distressing and this can erroneously interpreted as depression. This cannot help but also engender feelings of guilt. I had one lady state, that with her religious background, she does not feel she can allow herself to enjoy life until she is well enough to go back to work. Attitudes to chronic pain and the inability to work create feelings of guilt so it can be difficult to know what the guilt question is actually measuring. 5) It has been documented that the KEY cause of depression in chronic pain is the “subjective future” that is - future dread European Journal of Pain (1999) 3: 221-233 Subjective future as a mediating factor in the relation between pain, pain-related distress and depression Christina Hellstrijm, Bengt Jansson and Sven G. Carlsson “Helping patients to establish more positive thinking about the future would lead to therapeutic gains.” – a future in which a WCB victim deals with employers who only want him/her back if s/he is 100%, and case workers whose only real interest it seems is to contain costs by any means – which means getting him/her off WCB by any trick they can muster. This engendered future dread cannot help but thoroughly perpetuate any depressive distress symptoms One finding demonstrating how inaccurate diagnosis of depression in chronic pain stems from the finding that a negative view of the future is considered very important, particularly in the Beck Depression Inventory. Surprisingly, may chronic pain patients however, do not necessarily share that idea. This has lead to new scales that strip out many of the useless questions that are used in grading depression. abstract here I think it is pretty obvious that 100% of chronic pain patients can be diagnosed depressed if you so wish, using criteria not designed for that population. Hence it is not valid to ever terminate coverage on a patient just because someone found them “depressed”. The most elegant of scans uses the combination of lack of objective findings and depression to legitimize termination. The former is now an illegal maneuver, the latter immaterial. Neither can be used legitimately. Anxiety Diagnostic Testing Unreliable - Anxiety questionnaires can rely heavily on “somatizations” – body pains and symptoms: headaches chest pains - stomach pains constipation tight tense muscles dizzy, off balance (side effect of opioids) tired, weak palpitations (side effect of Amitriptyline used for chronic pain) These can be invalid and can result from the medications the patient is on. Using above criteria, 100% of people with pain can be diagnosed as anxious. This problem arises from the fact these tests were not designed to be used on chronic pain patients – they were only normalized for use in psychiatric populations. Anxiety is a common finding in the “normal population”. It does not render them chronic pain patients. Studies that have found anxiety in chronic pain populations have still had to face the fact the number one issue was still the level of pain. Personality Typing Unreliable Personality type-fitting is another tactic used to discredit claimants. Yet. early analysis demonstrated chronic pain sufferers had relatively normal personality structure: abstract here The largest personality test is the MMPI. The biggest joke was findings on MMPI psychological test which showed elevations of depression, hysteria, and hypochondriasis - “triple V profile”. Its presence in Rheumatoid Arthritis is just caused by extent of disease: Arthritis Rheum. 1986 Dec;29(12):1456-66. Elevated MMPI scores for hypochondriasis, depression, and hysteria in patients with rheumatoid arthritis reflect disease rather than psychological status. Pincus T, Callahan LF, Bradley LA, Vaughn WK, Wolfe F. abstract here This Triple profile can, however, label someone a personality case. Importantly, it has been demonstrated it is possible for this profile to disappear after successful treatment of the patient’s pain condition. This means that finding these personality factors cannot be reliably used to discount a patient’s pain. Personality characteristics do not change over time – they are supposed to be stable. Yet, chronic pain sufferers personality profiles do change, again suggesting these evaluations are not valid. This study showed how abnormal personality characteristics and depression normalized after treatment was one involving pain relieving whiplash injuries with burning of neck nerves. Wallis BJ, Lords SM, Bogduk N. Resolution of psychological distress of whiplash patients following treatment by radiofrequency neurotomy: a randomized, double-blind, placebo-controlled trial. Pain 1997;73:15 - 22. psychological gone with RX here Another arduous 20 year study found that personality abnormalities in chronic back pain started after the injury: Spine. 1995 Dec 15;20(24):2716-20. Minnesota Multiphasic Personality Inventory profiles in persons with or without low back pain. A 20-year follow-up study. Hansen FR, Biering-Sorensen F, Schroll M. “The results indicated that low back pain is preceded by elevated Minnesota Multiphasic Personality Inventory scales was not supported.” abstract here Another found psychological factors included STAI anxiety scores in head pain disappeared with pain treatment: Head pain normalization MMPI here Cephalalgia. 1994 Oct;14(5):368-73; discussion 319. Personality characteristics before and after treatment of different head pain syndromes. Mongini F, Ibertis F, Ferla E. “Clinical improvement leads to normalization of MMPI profiles and STAI scores in women. The psychometric data before treatment were not predictive for treatment outcome.” Again here is a study showing successful treatment of pain removes the psychological problems: With pain reduction here Pain. 1975 Jun;1(2):177-81. Personality changes associated with reduction of pain. Sternbach RA, Timmermans G. “The results support the hypothesis that the neuroticism associated with chronic pain is the result of it, and may be reversible when the pain is reduced or abolished.” Women seem to get the worst appraisals that their problems are psychological. The worse would have had to be pelvic pain. Blaming the victim - The psychologizing of endometriosis Ballweg ML OBSTETRICS AND GYNECOLOGY CLINICS OF NORTH AMERICA 24 (2): 441- 444 JUN 1997 abstract here Yet a recent study demonstrates that proper pelvic pain treatment can make “psychological problems” improve. J Am Assoc Gynecol Laparosc. 1998 Nov;5(4):389-95. Changes in personality profile associated with laparoscopic surgery for chronic pelvic pain. Duleba AJ, Jubanyik KJ, Greenfeld DA, Olive DL abstract here The biggest joke have to be genital skin pain. This has been extensively discussed as psychological, yet now found potentially curable by Botox injects, or by treating a previously unrecognized external infection. Lichen abstract here Vestibulitis abstract here The depression of Fibromyalgia, a primarily woman’s disease, improves with successful treatment as well, again suggesting it is pain that drives the symptoms. Efficacy and adverse effects of intravenous lignocaine therapy in fibromyalgia syndrome JH Raphael et al 2002 abstract here CONCLUSION A review of MMPI results in chronic pain makes the following very clear: Clinical Psychology Review, Vol. 20, No. 5, pp. 533–559, 2000 THE MINNESOTA MULTIPHASIC PERSONALITY INVENTORY CHRONIC PAIN: A CONCEPTUAL ANALYSIS OF A LONG-STANDING BUT COMPLICATED RELATIONSHIP Alexander A. Vendrig “it has simply been applied inappropriately (i.e., for determination of pain etiology or underlying personality structure “explaining” the chronic pain).” Given that this is the most comprehensive psychological profiling tests, its comments are very chilling: Psychological testing is inappropriate for determining if “personality” is the cause of pain. It must be clear from above that: 1) Personality, depression and anxiety issues are much more likely to be caused by chronic pain. 2) The diagnosis of anxiety, depression, or personality disorders cannot be used to discredit someone with chronic pain. Nor can they be used to terminate coverage. 3) As reiterated earlier, the most elegant of scans uses the combination of lack of objective findings and depression (or “personality disorder”) to legitimize termination. The former is now an illegal maneuver, the latter immaterial. Neither can be used legitimately.