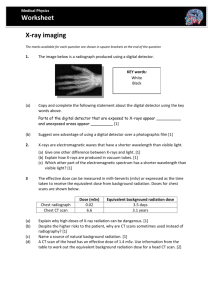
3 Physical and biological phenomena caused by ionizing radiation
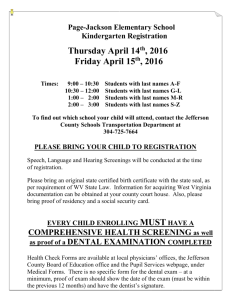
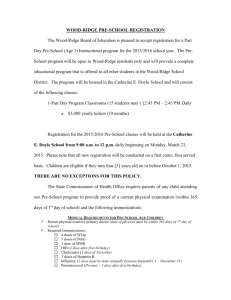
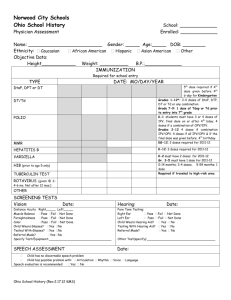
advertisement

Académie des Sciences [Academy of Sciences] - Académie nationale de Médecine [National Academy of Medicine] Dose-effect relationships and estimation of the carcinogenic effects of low doses of ionizing radiation March 30, 2005 André Aurengo1 (Rapporteur), Dietrich Averbeck, André Bonnin1 (†), Bernard Le Guen, Roland Masse2, Roger Monier3, Maurice Tubiana1,3 (Chairman), Alain-Jacques Valleron3, Florent de Vathaire. Executive Summary The assessment of carcinogenic risks associated with doses of ionizing radiation from 0.2 Sv to 5 Sv is based on numerous epidemiological data. However, the doses which are delivered during medical X-ray examinations are much lower (from 0.1 mSv to 20 mSv). Doses close to or slightly higher than, these can be received by workers or by populations in regions of high natural background irradiation. Epidemiological studies have been carried out to determine the possible carcinogenic risk of doses lower than about 100 mSv, and they have not been able to detect statistically significant risks even on large cohorts or populations. Therefore, these risks are at worse low since the highest limit of the confidence interval is relatively low. It is highly unlikely that putative carcinogenic risks could be estimated or even established for such doses through case-control studies or the follow-up of cohorts. Even for several hundred thousands of subjects, the power of such epidemiological studies would not be sufficient to demonstrate the existence of a very small excess in cancer incidence or mortality adding to the natural cancer incidence which, in non-irradiated populations, is already very high and fluctuates according to lifestyle. Only comparisons between geographical regions with high and low natural irradiation and with similar living conditions could provide valuable information for this range of doses and dose rates. The results from the ongoing studies in Kerala (India) and China need to be carefully analyzed. Because of these epidemiological limitations, the only method for estimating the possible risks of low doses (< 100 mSv) is extrapolation from carcinogenic effects observed between 0.2 and 3 Sv. A linear no-threshold relationship (LNT) describes well the relation between the dose and the carcinogenic effect in this dose range where it could be tested. However, the use of this relationship to assess by extrapolation the risk of low and very low doses deserves great caution. Recent radiobiological data undermine the validity of estimations based on LNT in the range of doses lower than a few dozen mSv which leads to the questioning of the hypotheses on which LNT is implicitly based: 1) constancy of the probability of mutation (per unit dose) whatever the dose or dose rate, 2) independence of the carcinogenic process which after the initiation of a cell evolves similarly whatever the number of lesions present in neighboring cells and the tissue. Indeed, 1) progress in radiobiology has shown that a cell is not passively affected by the accumulation of lesions induced by ionizing radiation. It reacts through at least three mechanisms: a) by fighting against reactive oxygen species (ROS) generated by ionizing radiation and by any oxidative stress, b) by eliminating injured cells (mutated or unstable), Membre de l’Académie nationale de médecine Membre correspondant de l’Académie nationale de médecine 3 Membre de l’Académie des Sciences 1 2 through two mechanisms: i) apoptosis which can be initiated by doses as low as a few mSv, thus eliminating cells the genome of which has been damaged or misrepaired, ii) death of cells during mitosis when lesions have not been repaired. (Recent works suggest that there is a threshold of damage under which low doses and dose rates do not activate intracellular signalling and repair systems, a situation leading to cell death.) c) by stimulating or activating DNA repair systems following slightly higher doses of about ten mSv. Furthermore, intercellular communication systems inform a cell about the presence of an insult in neighboring cells. Modern transcriptional analysis of cellular genes using microarray technology reveals that many genes are activated following doses much lower than those for which mutagenesis is observed. These methods have been a source of considerable progress by showing that depending on the dose and the dose rate not the same genes are transcribed. At doses of a few mSv (< 10 mSv), lesions are eliminated by disappearance of the cells; at slightly higher doses damaging a large number of cells (therefore capable of causing tissue lesions), repair systems are activated. They permit cell survival but may generate misrepairs and irreversible lesions. For low doses (< 100 mSv), the extent of mutagenic misrepairs is small but its relative importance, per unit dose, increases with the dose and dose rate. The duration of repair varies with the complexity of the damage and its amount. Several enzymatic systems are involved and a high local density of DNA damage may lower their efficacy. At low dose rates the probability of misrepair is smaller. The modulation of the cell defense mechanisms according to the dose, dose rate, the type and number of lesions, the physiological condition of the cell, and the number of affected cells explains the large variations in radiosensitivity (variations in cell mortality or the probability of mutations per unit dose) depending on the dose and the dose rate that have been observed. The variations in cell defense mechanisms are also demonstrated by several phenomena: initial cell hypersensitivity during irradiation, rapid variations in radiosensitivity after short and intense irradiation at a very high dose rate, adaptive responses which cause a decrease in radiosensitivity of the cells during hours or days following a first low pre-conditionning dose of radiation, etc. 2) Moreover, it was thought that radiocarcinogenesis was initiated by a lesion of the genome affecting at random a few specific targets (proto-oncogenes, suppressor genes, etc.). This relatively simple model, which provided a theoretical framework for the use of LNT, has been replaced by a more complex one including genetic and epigenetic lesions, and in which the relationship between the initiated cells and their microenvironment plays an essential role. This carcinogenic process is counteracted by effective defense mechanisms in the cell, tissue and the organism. With regard to tissue, the mechanisms which govern embryogenesis and direct tissue repair after injury appear to play also an important role in the control of cell proliferation. This is particularly important when a transformed cell is surrounded by normal cells. These mechanisms could explain the lower efficacy of heterogeneous irradiation, i.e. local irradiations through a grid, as well as the absence of a carcinogenic effect in humans or experimental animals contaminated by small quantities of -emitter radionuclides. The latter data suggest the existence of a threshold. This interaction between cells could also help to explain the difference in the probability of carcinogenesis according to the tissues and the dose, since the death of a large number of cells disorganizes the tissue and favors the escape of initiated cells from tissue controls. 3) Immunosurveillance systems are able to eliminate clones of transformed cells, as is shown by tumor cell transplants. The effectiveness of immunosurveillance is also shown by the large increase in the incidence of several types of cancers among immunodepressed subjects (a link seems to exist between a defect in DNA repair (NHEJ) and immunodeficiency). 2 All these data suggest that the lower effectiveness of low doses, or the existence of a practical threshold which could be related to either the failure of a very low doses to sufficiently activate cellular signalling and thereafter DNA repair mechanisms or to an association between apoptosis error-free repair and immunosurveillance.. However on the basis of our present knowledge, it is not possible to define the threshold level (between 5 and 50 mSv?) or to provide the evidence for it. The stimulation of cell defense mechanisms, in particular to cope with reactive oxygen species. Indeed, a meta-analysis of experimental animal data shows that in 40% of these studies there is a decrease in the incidence of spontaneous cancers in animals after low doses. This observation has been overlooked so far because the phenomenon was difficult to explain. These data show that it is not justified to use the linear no-threshold relationship to assess the carcinogenic risk of low doses observations made for doses from 0.2 to 5 Sv since for the same dose increment the biological effectiveness varies as a function of total dose and dose rate. The conclusion of this report is in fact in contradiction with those of other authors [43,118], which justify the use of LNT by the following arguments. 1. for doses lower than 10 mGy, there is no interaction between the different physical events initiated along the electron tracks through the DNA or the cell; 2. the nature of lesions caused and the probability of error prone or error free repair and the elimination of damaged cells by cell death is neither influenced by the dose nor the dose rate; 3. cancer is the direct and random consequence of a DNA lesion in a cell apt to divide and the probability of the initiated cell to give rise to cancer is not influenced by the damage in the neighbor cells and tissues; 4. the LNT model correctly fits the dose-effect relationship for the induction of solid tumors in the Hiroshima and Nagasaki cohort; 5. the carcinogenic effect of doses of the order of 10 mGy is proven for humans by results from in utero irradiation studies . The first argument concerns the initial physico-chemical events which are proportional to dose; however, the nature and efficiency of cellular defense reactions that are activated vary with dose and dose rate. The second argument is contradicted by recent radiobiological studies considered in the present report. The third argument does not take into account recent findings on the complexity of the carcinogenic process and the particular role of intercellular relationships and the stroma.. Regarding the fourth argument, it can be noted that besides LNT, other types of dose-effect relationships are also compatible with data concerning solid tumors in atom bomb survivors, and can also satisfactorily fit epidemiological data that are incompatible with the LNT concept, notably the incidence of leukemia in these same A-bomb survivors. Furthermore, taking into account the latest available data, the dose-effect relationship for solid tumors in Hiroshima-Nagasaki survivors is not linear but curvilinear between 0 and 2 Sv. Moreover, even if the dose-effect relationship were demonstrated to be linear for solid tumors between, for example, between 50 mSv and 3 Sv, a generalization would not be possible because of experimental and clinical data show that the dose effect relationship considerably varies according to type of tumor and age of individuals at the time of irradiation. The global annd empirical relationship observed for solid tumors corresponds to the sum of relationships which can be quite different according to the type of cancer, for example, some being linear or quadratic, with or without threshold. Finally, with regard to in utero irradiation, whatever the value of the Oxford study, some inconsistencies between the availbable data sets call for great caution before concluding the existence of a causal relationship from data showing simply an association. Furthermore, it is highly questionable to extrapolate from the fetus to the child and adult, particularly, since 3 the developmental state, cellular interactions and immunological control systems are very different. In conclusion, this report raises doubts on the validity of using LNT for evaluating the carcinogenic risk of low doses (< 100 mSv) and even more for very low doses (< 10 mSv). The LNT concept can be a useful pragmatic tool for assessing rules in radioprotection for doses above 10 mSv; however since it is not based on biological concepts of our current knowledge, it should not be used without precaution for assessing by extrapolation the risks associated with low and even more so, with very low doses (< 10 mSv), especially for benefit-risk assessments imposed on radiologists by the European directive 97-43. The biological mechanisms are different for doses lower than a few dozen mSv and for higher doses. The eventual risks in the dose range of radiological examinations (0.1 to 5 mSv, up to 20mSv for some examinations) must be estimated taking into account radiobiological and experimental data. An empirical relationship which has been just validated for doses higher than 200 mSv may lead to an overestimation of risks (associated with doses one hundred fold lower), and this overestimation could discourage patients from undergoing useful examinations and introduce a bias in radioprotection measures against very low doses (< 10 mSv). Decision makers confronted with problems of radioactive waste or risk of contamination, should re-examine the methodology used for the evaluation of risks associated with very low doses and with doses delivered at a very low dose rate. This report confirms the inappropriateness of the collective dose concept to evaluate population irradiation risks. Résumé et conclusions Les risques cancérogènes d’une exposition aux rayonnements ionisants ont été estimés par de nombreuses études épidémiologiques entre 0,2 et 5 Sv4. Mais le domaine des doses qui concerne la santé humaine est généralement beaucoup plus faible : les doses délivrées par la plupart des examens radiologiques sont inférieures à une dizaine de mSv4.Les irradiations auxquelles sont exposés les travailleurs ou les personnes habitant les régions où l’irradiation naturelle est élevée, sont également de cet ordre ou légèrement supérieures. Or les études épidémiologiques disponibles ne décèlent aucun effet pour des doses inférieures à 100 mSv, soit qu’il n’en existe pas, soit que la puissance statistique des enquêtes ait été insuffisante pour les détecter. Comme certaines enquêtes portent sur un grand nombre de sujets, ces résultats montrent déjà que le risque, s’il existe devrait être très faible. Il est peu vraisemblable que de nouvelles enquêtes parviennent, dans un avenir proche, à estimer ces risques éventuels et encore moins à les exclure. En effet, le suivi de cohortes, même de plusieurs centaines de milliers de sujets n’aura sans doute pas la puissance statistique suffisante pour mettre en évidence un excès d’incidence ou de mortalité très petit venant s’additionner à une incidence de cancer qui est très grande dans les populations non irradiées et qui fluctue en fonction des conditions de vie. Seules des comparaisons entre des régions géographiques à haute et faible irradiation naturelle, et dans lesquelles les conditions de vie sont semblables pourraient apporter des informations pour cette gamme de dose et de débit de 4 Voir glossaire pour les grandeurs et les unités caractérisant la dose. Il n’y a pas de consensus sur les doses correspondant aux « faibles » ou « très faibles » doses. Selon les auteurs, les faibles doses sont celles inférieures à 200 ou à 100 mSv, les très faibles doses celles inférieures à 20 ou à 10 mSv. Dans le cadre de ce rapport nous admettons que les doses faibles sont inférieures à 100 mSv et très faibles à 10 mSv. 4 dose. Il faut donc suivre attentivement les résultats des enquêtes en cours au Kerala (Inde) et en Chine. Les méthodes d’évaluation directe étant insuffisantes, on est contraint pour estimer les risques éventuels des faibles doses (< 100 mSv) d’extrapoler à partir des effets cancérogènes observés entre 0,2 et 3 Sv. Une relation linéaire décrit convenablement la relation entre la dose et l’effet cancérogène pour les doses supérieures à 200 mSv où on a pu la tester. Ceci a paru justifié l’utilisation d’une relation linéaire sans seuil (RLSS) pour estimer le risque des faibles doses. Cependant dans le domaine des doses inférieures à quelques dizaines de mSv, les données radiobiologiques récentes jettent un doute sur la validité de cette procédure, car elles sont en désaccord avec les deux hypothèses sur lesquelles la relation linéaire sans seuil est implicitement fondée à savoir : 1) la constance de la probabilité de mutation (par unité de dose) quels que soient la dose et le débit de dose. 2) le processus de cancérogenèse, après avoir été initié dans une cellule, évolue indépendamment des lésions éventuellement présentes dans les cellules environnantes. En effet, les données récentes mettent en évidence l’existence de mécanismes de défense contre les altérations du génome à l’échelle de la cellule du tissu et de l’organisme et qui limitent la prolifération d’une cellule « initiée » dans un tissu ou un organisme multicellulaire : 1. Les progrès de la radiobiologie ont montré que la cellule ne subit pas passivement l’accumulation des lésions causées par les rayonnements. Elle se défend et réagit par au moins trois mécanismes : - En mettant en œuvre des systèmes enzymatiques de détoxification dirigés contre les espèces actives de l’oxygène apparues à la suite du stress oxydatif, - En éliminant les cellules lésées (mutées ou instables), grâce à deux mécanismes : l’apoptose (qui peut être déclenchée par des doses de l’ordre de quelques mSv afin de tuer les cellules dont le génome a été altéré ou présente des dysfonctionnements) et la mort au moment de la mitose des cellules dont les lésions n’ont pas été réparées. Or, des travaux récents indiquent qu'il existe un seuil au-dessous duquel les faibles doses et débits de dose ne déclenchent pas l’activation des systèmes de signalisation intracellulaire qui gouvernent la réparation, ce qui entraîne la mort de ces cellules. - En mettant en œuvre des systèmes de réparation de l’ADN qui sont stimulés ou activés par des doses de l’ordre d’une dizaine de mSv. Il existe, de plus, des systèmes de signalisation intercellulaire qui informent chaque cellule sur le nombre de cellules environnantes ayant été lésées. Les méthodes modernes d’analyse de la transcription des gènes cellulaires montrent que pour de nombreux gènes, celle-ci est modifiée par des doses beaucoup plus faibles (de l’ordre du mSv) que celles pour lesquelles on observe une mutagenèse. Ces méthodes ont été la source de progrès considérables en montrant que selon la dose et le débit de dose ce ne sont pas les mêmes gènes qui sont transcrits. Il apparaît ainsi que pour les très faibles doses (<10 mSv), les lésions sont éliminées par la disparition des cellules ; pour des doses un peu plus élevées et endommageant un nombre notable de cellules (donc susceptibles de causer des lésions tissulaires), les systèmes de réparation de l’ADN sont activés ; ils permettent la survie cellulaire mais peuvent générer des erreurs. Aux faibles doses (< 100 mSv), le nombre de réparations 5 fautives mutagènes est petit mais son importance relative, par unité de dose, croît avec la dose et le débit de dose. Cette modulation des réactions de défense de la cellule en fonction de la dose, du débit de dose, de la nature et du nombre de lésions, des conditions physiologiques de la cellule et du nombre de cellules atteintes explique les fortes variations de radiosensibilité (mortalité cellulaire, ou probabilité de mutation, par unité de dose) qui sont observées en fonction de la dose et du débit de dose: hypersensibilité cellulaire initiale au cours d’une irradiation quand la dose est faible, puis au delà de 200 mSv apparition d’une radiorésistance induite avec diminution de la mortalité cellulaire (par unité de dose), variations brutales de la radiosensibilité après une irradiation intense et brève, radio-adaptation c’est-à-dire diminution temporaire de la radiosensibilité dans les heures ou jours qui suivent une première irradiation à faible dose, etc. 2. D’autre part, on pensait que la radiocancérogenèse était initiée par une lésion du génome atteignant de façon aléatoire quelques cibles spécifiques (proto-oncogènes, gènes suppresseurs, etc.). A ce modèle relativement simple, qui avait donné un substrat théorique à l’utilisation de la RLSS, s’est substitué celui d’un processus complexe, que l’on commence à identifier, où s’associent lésions génétiques et épigénétiques et surtout dans lequel les relations entre la cellule initiée et les cellules environnantes jouent un rôle essentiel. Ce processus de cancérogenèse se heurte à des mécanismes efficaces de défense à l’échelle du tissu et de l’organisme. Au niveau du tissu, les mécanismes qui interviennent dans l’embryogenèse et pour diriger la réparation tissulaire après une agression, semblent jouer un rôle pour contrôler la prolifération d’une cellule, même quand celle-ci est devenue autonome. Ce mécanisme pourrait expliquer l’absence d’effet cancérogène après contamination par de faibles quantités de radioéléments émetteurs (phénomène dans lequel un petit nombre de cellules ont été fortement irradiées mais sont environnées par des cellules saines) avec l’existence, dans ce cas, d’un seuil chez l’homme comme chez l’animal. Il pourrait aussi contribuer à expliquer la grande différence de probabilité d’un effet cancérogène selon le tissu et selon la dose, puisque la mort d’un grand nombre de cellules désorganise le tissu et favorise l’échappement aux contrôles tissulaires d’une cellule initiée, comme le suggèrent aussi les irradiations locales au travers de grilles. 3. Enfin, les systèmes de surveillance mis en œuvre par les cellules saines de l’organisme sont capables d’éliminer des clones de cellules transformées, comme le montrent, les échecs des greffes de cellules tumorales ainsi que la forte augmentation de la fréquence de certains cancers chez les sujets immunodéprimés (un certain lien semble exister entre une déficience du système de réparation NHEJ et l’immunodéficience). Toutes ces données suggèrent une moindre efficacité des faibles doses, voire l’existence d’un seuil qui pourrait être lié soit à l’absence de mise en œuvre des mécanismes de signalisation et de réparation pour les très faibles doses, soit à l’association apoptose + réparation non fautive + immunosurveillance, sans qu’il soit possible, en l’état actuel de nos connaissances, de fixer le niveau de ce seuil (entre 5 et 50 mSv ?) ou d’en démontrer l’existence. Ces réactions peuvent aussi expliquer l’existence d’un phénomène d’hormesis5 dû à la stimulation des mécanismes de défense, notamment à la lutte contre les formes actives de 5 effet d’un agent, physique ou chimique, qui provoque un effet à forte dose et un effet inverse à faible dose (voir glossaire). C’est le cas pour de nombreux agents, toxiques à fortes doses, mais qui à faible dose ont un effet favorable protecteur. 6 l’oxygène. De fait, la méta-analyse qui a été faite des résultats de l’expérimentation animale montre dans 40 % de ces études une diminution de la fréquence spontanée des cancers chez les animaux après de faibles doses, observation qui avait été négligée car on ne savait pas l’expliquer. Globalement, ces résultats montrent qu’il n’est pas justifié d’utiliser une relation linéaire sans seuil (RLSS) pour estimer le risque cancérogène des faibles doses à partir des observations effectuées pour des doses allant de 0,2 à 5 Sv, puisqu’un même incrément de dose a une efficacité variable en fonction des conditions d’irradiation notamment de la dose totale et du débit de dose. La conclusion de ce rapport est, de ce fait, en contradiction avec celles d’autres auteurs [43,118] qui justifient l’utilisation de cette relation sur les arguments suivants : 1. aux doses inférieures à 10 mSv il n’y a pas d’interaction entre les différents événements physiques initiés le long des différentes trajectoires des électrons ; 2. la nature des lésions ainsi causées et la probabilité de réparation fidèle ou fautive et d’élimination par la mort des cellules lésées ne dépendent ni de la dose ni du débit ; 3. le cancer est la conséquence directe et aléatoire d’une lésion de l’ADN dans une cellule apte à se diviser et la probabilité pour qu’une cellule initiée donne naissance à un cancer n’est pas influencée par les lésions dans les cellules voisines et les tissus ; 4. la relation linéaire sans seuil rend compte de manière correcte de la relation dose-effet pour l’induction de tumeurs solides dans la cohorte d’Hiroshima et Nagasaki ; 5. l’effet cancérogène de doses de l’ordre de 10 mSv est prouvé chez l’homme par les résultats des études sur l’irradiation in utero. Le premier argument concerne les phénomènes physico-chimiques initiaux qui sont proportionnels à la dose ; cependant la nature et l’efficacité des mécanismes de défense qu’ils déclenchent varie avec la dose. Le deuxième argument est donc en opposition avec les travaux récents de radiobiologie que nous venons d’examiner. Le troisième argument ne tient pas compte de la complexité du processus de cancérogenèse qui a été révélée au cours de la dernière décennie et qui souligne en particulier le rôle des relations intercellulaires et du stroma. Pour le quatrième, on doit remarquer que d’autres types de relation dose-effet (quadratiques ou avec seuil), tout aussi compatibles que la RLSS avec les données concernant les tumeurs solides chez les survivants des explosions atomiques, ont l’avantage de rendre compte d’autres données épidémiologiques non compatibles avec la RLSS, notamment l’incidence des leucémies chez ces mêmes survivants. De plus, les dernières données disponibles montrent que la relation dose-effet pour les tumeurs solides chez les survivants d’Hiroshima–Nagasaki n’est pas linéaire mais curvilinéaire entre 0 et 2 Sv. Enfin, même si la linéarité de la relation dose-effet était démontrée pour certains cancers entre, par exemple 50 mSv et 3 Sv, sa généralisation ne serait pas possible car l’expérimentation et l’observation clinique montrent que la relation dose effet varie considérablement selon le type de tumeur et l’âge lors de l’irradiation. La relation empirique globale observée pour l’ensemble des tumeurs solides correspond à l’addition de relations qui peuvent être très différentes selon le type de cancer, par exemple linéaires ou quadratiques, avec ou sans seuil. Enfin, en ce qui concerne les irradiations in utero, quelle que soit la valeur de l’étude d’Oxford, certaines incohérences entre les données disponibles imposent une grande prudence avant de conclure qu’il existe une relation causale à partir de données montrant une association. De plus, il est très discutable d’extrapoler du fœtus à l’enfant ou à l’homme, en particulier parce que le niveau de développement, les relations intercellulaires et les systèmes d’immunosurveillance sont très différents. En conclusion, le présent rapport émet des réserves sur l’usage de la RLSS pour évaluer le risque cancérogène des faibles doses (< 100 mSv). La RLSS peut constituer un outil 7 pragmatique utile pour fixer les règles de la radioprotection pour des doses supérieures à une dizaine de mSv ; mais, n’étant pas fondée sur des concepts biologiques correspondant à nos connaissances actuelles, elle ne peut pas être utilisée sans précaution pour estimer par extrapolation l’effet des faibles et surtout des très faibles doses (< 10 mSv), notamment dans l’évaluation du rapport bénéfice-risque, imposée au praticien dans le cadre de la pratique radiologique par la directive européenne 97-43. Les mécanismes biologiques sont différents pour des doses inférieures à quelques dizaines de mSv et pour des doses supérieures. Les risques éventuels dans la gamme de dose des examens radiologiques (0,1 à 5 mSv ; jusqu’à 20 mSv pour certains examens) doivent être estimés en tenant compte des données radiobiologiques et de l’expérimentation animale. L’usage d’une relation empirique qui n’est validée que pour des doses supérieures à 200 mSv pourrait, en surévaluant les risques faire renoncer à des examens susceptibles d’apporter au malade des informations utiles ; elle pourrait aussi en radioprotection conduire à des conclusions erronées. Les décideurs confrontés au problème des déchets radioactifs ou au risque de contamination doivent réexaminer la méthodologie utilisée pour évaluer les risques des très faibles doses et des doses délivrées avec un très faible débit. Enfin ce rapport confirme qu’il n’est pas acceptable d’utiliser le concept de dose collective pour évaluer les risques liés à l’irradiation d’une population. 8 Glossary Apoptosis Programmed cell death. Apoptosis plays an important part in embryogenesis, in tissue regeneration following an insult, and can eliminate cells whose DNA has been damaged and not repaired with a high fidelity. Carcinogenesis Process that leads to the formation of a cancer. It involves several stages (resulting from successive alterations of the genome). The first stage is that of initiation (this may, for instance, be due to the mutation of a protooncogene into an oncogene). For a normal cell to be “transformed” i.e. for it to become preneoplasic, its genome has to undergo several modifications (appearance of an oncogene, inactivation of both copies of a suppressor gene, immortalization i.e. acquisition of an unlimited capacity to proliferate, changes affecting the apoptosis system, etc.). A transformed cell can give rise to an invasive cancer at the end of the second stage, known as “promotion”, which is associated with the proliferation of the descendants of the initiated cell, and the escape of one of them from the control of the normal surrounding cells and of the body. Cytokines Chemical agents that are secreted by certain cells and act on other cells (such as the lymphocytes). Several hundreds have been identified. They bind to specific receptors in the type of cell to which they are destined. Alongside hormones, antibodies etc., they play an important role in intercellular communication. Two of them are mentioned in the report: Transforming growth factor (TGF ), and tumor necrosis factor (TNF ). Dose The concept of dose is used to measure the effect of ionizing radiations, it involves three different quantities: the absorbed dose: the energy absorbed per unit mass. The unit used for the dose absorbed is the gray (Gy). The equivalent dose: the absorbed dose multiplied by a “biological weighting factor” which expresses the relative harmfulness of the various types of radiation. The biological effect of radiations depends on the nature of the particles involved; for an equal dose (in Gy) it is greater for radiations that have a high ionization density along the track of the particles (i.e. a high linear energy transfer, or LET). The biological weighting factor is, for example, equal to 1 for photons and electrons, but equal to 20 for particles. The unit used for the equivalent dose is the Sievert (Sv). The equivalent dose is used, for the purposes of radioprotection, for adding doses delivered by various types of radiations (X-rays and neutrons, for instance). The effective dose: the equivalent dose multiplied, for each tissue, by a “tissue weighting factor”, which expresses the relative risk of carcinogenesis. The tissue weighting factor for the thyroid is, for example, equal to 0.05. The unit used for the effective dose is the Sievert (Sv). The effective dose was introduced for the purposes of radioprotection, because it makes it possible to add the doses received on different areas of the body (on a limb and the thyroid for instance). The units used for the equivalent dose and the effective dose, although these are in distinct quantities, are called by the same name (the Sv), which can give rise to confusion if it is not clearly stated which is being referred to. If the whole body has been exposed uniformly, then the equivalent dose is equal to 9 the effective dose. In the case of exposure to X- or gamma rays, the doses in Gy and in Sv are equal. To make this report easier to follow, we have generally used Sv. Unless otherwise specified, it is used as a unit of equivalent dose. Magnitude of doses Natural irradiation: is that to which all living beings are exposed: cosmic rays, radioactive substances present in the earth’s crust, potassium 40 present in the body, etc. In France, this natural dose averages 2.5 mSv/year with geographical variations ranging between 1 and 6 mSv/year. Worldwide, it ranges from 1 to 80 mSv/year. X-ray examinations: depending on the type of examination, they deliver an equivalent dose of 0.1 to 20 mSv. On average, in France, they deliver 1 mSv/year per person, but this exposure varies widely, concentrated in a small number of individuals. Radiotherapy: the doses used for a treatment range from 60 to 80 Gy to the tumor and the target volume (and from a few Gy to a few mGy to the rest of the body). Nuclear energy: this leads to the exposure of workers directly assigned to work under radiation to 2 mSv/year on average, and to exposure of the general public to less than 0.015 mSv/year (effective dose). Dose rate: Dose per unit time (Gy/min or Sv/min, for example) Low doses There is no consensus about the doses described as being “low” or “very low” doses. Depending on the author, low doses may be less than 200 or less than 100 mSv, and very low doses those that are below 20 or 10 mSv. In the context of this report we take low doses to be less than 100 mSv, and very low doses to be less than 10 mSv. Suppressor genes: genes that oppose the continuous proliferation of cells. They are also known as “tumor suppressor genes”. Genome the full set of DNA molecules present in the cell nucleus. Gray (Gy) unit used for the absorbed dose. A tissue is said to have received a dose of 1 gray (Gy) when the energy transferred by the radiation to the tissue is 1 joule/kg. Hormesis Some physical or chemical agents have one effect at high doses and the reverse effect at low doses. This phenomenon is known as hormesis. It probably results from the activation of defense mechanisms. Hormesis is observed with several drug molecules that are toxic at high doses, but which can have a beneficial protective effect at low doses. ICRP International Commission on Radiological Protection Proto-oncogene gene generally active in the embyo and fetus, and during proliferation processes. A mutation can result in the permanent activation of a protooncogene, which then becomes an oncogene. Dose-effect relationship Linear no-threshold relationship effect) Linear-quadratic relationship Quadratic relationship 10 E = d (where d is the dose and E the E = d + d2 E = d2 Curvilinear relationship: quadratic or quadratic. non-linear function, such as linear- DNA repair Error-free repair: the molecule is reconstituted with a high fidelity, i.e. without loss of information. Misrepair or error prone repair: reconstitution with a loss of information (for instance, deletion due to the loss of a fragment of the molecule, or mutation or translocation). Sievert (Sv) unit used for the equivalent dose and the effective dose. It is equal to the dose in Grays multiplied by a weighting factor. Oxidative stress. Formation of reactive oxygen species (ROS) in and outside cells, such as those resulting from the lysis of water molecules induced by ionizing radiation. This stress can not only damage cellular constituants and generate inflammatory processes but also activate several enzyme systems and modify the transcription of genes. These reactions are known collectively as oxidative stress. TGF TGFß (Transforming Growth Factor beta) is a cytokine which regulates many of the biological processes essential for embryo development and tissue homeostasis, and therefore plays a role in the healing of a tissue and carcinogenesis. The effects of TGFß may differ depending on the tissue concerned. For instance, TGFß inhibits the proliferation of epithelial cells, but stimulates that of fibroblasts. TNF TNF (Tumor Necrosis Factor alpha) is classified as a cytokine. It is a mediator of natural immunity, because it can be secreted without the involvement of any antigen. UNSCEAR United Nations Scientific Commission on Effects of Atomic Radiation 11 1 Introduction 1.1 The risk of low doses of ionizing radiations cannot be assessed directly. The only way to evaluate them is therefore by extrapolating from the effects of high doses. Depending on the dose-effect relationship used for this extrapolation, the risk attributed to low doses may range from zero (or even a negative value in hormesis) to a value proportional to the dose (or even supralinear). The evaluation of the cancer risk of low doses is of great importance in medicine, as illustrated by three examples: - Approximately 70 million radiological examinations are performed in France every year, delivering an average of 1 mSv per year to every French person. Depending on the dose-effect relationship used, it can be deduced from this, either that these exams. could be leading to about three thousand cases of cancer a year, or that they do not represent any hazard. - Nuclear energy delivers about 0.001 mSv/year to each person in France; in the vicinity of power stations, the dose can reach 0.015 mSv/year. People working in the nuclear industry receive on average 2 mSv/year. The impact on health varies widely, depending on how it is estimated, between zero impact and several dozen lethal cancers cases per year for the entire French population, and between zero and a few lethal cancers per year for workers. - An erroneous estimation of the risk associated with exposure to radon at home could lead either to overlooking a serious public health problem’s, given the number of people exposed, or conversely, to incurring considerable pointless expense in order to limit such exposure. 1.2. In 1995, the Académie des Sciences published a report discussing the effects of low doses [4], and subsequently organized a symposium on this topic [5]. The Académie de Médecine has issued several statements on this subject [2,3]. These documents pointed out that following exposure to low doses, epidemiological studies have not evidenced any significant effect: because either there is no effect, or the effect is too small to be detected by such studies. These results, which are sometimes described as “negative results”, are useful, because they help to assess the upper limit of the potential risk, and can be included in the meta-analyses. Over the past decade, new epidemiological data have been published. Some important new facts have emerged, such as the feasibility and value of studies comparing the morbidity and mortality in regions with high and low levels of natural irradiation but similar lifestyles, the questioning of the linear relationship between dose and the incidence of solid tumors among survivors of atom bombs [224,291], the fact that risk factors calculated from the survivors of atom bombs cannot be applied to medical irradiations (notably to fractionated irradiation or low dose rates). Nevertheless, despite their interest, they have not yielded to any conclusive data. With regard to the dose-effect relationship, the main contribution to progress has come from biological research: the new data have revealed the complexity and efficacy of defense mechanisms against genotoxic (physical and chemical) agents at the level of the cell (DNA repair and apoptosis), of the tissue (role of neighboring cells) and of the whole body (immunosurveillance). It has now been established that the cell reacts to low doses of irradiation, by stimulating defense mechanisms and possibly by inducing apoptosis of cells whose DNA has been damaged. The rapidity and effectiveness with which the cell reacts to irradiation had been previously considerably under-estimated, and these reactions depend on the dose and dose rate. Consequently the impact of a given dose of radiation can vary markedly depending on the 12 conditions of irradiation. 1.3 The effect of low doses is usually estimated by extrapolation using a linear, no-threshold dose-effect relationship (LNT). This method of assessing the carcinogenic risks of low doses was introduced in the 1960s by the International Commission on Radiological Protection (ICRP [117] for simplifying the collect and interpretation of the data. The LNT relation indeed makes it possible to add the various doses received by a worker during his/her working life, irrespective of dose rate, of exposure or type of radiation. Understandably, this led to the use of LNT for pragmatic purposes to estimate the effect of low doses by extrapolation in order to help decision making [133]. This use was subsequently justified by postulating that doses always accumulate, and that no matter how low they are, they all have the same radiocarcinogenic potential per unit dose, since each directly or indirectly ionizing particle crossing a cell or its nucleus acts independently and has the same efficacy. This postulate was supported when, during the 1970s, the link between DNA damage and carcinogenesis was established, and it was accepted that carcinogenesis is caused by stochastic mechanisms. This made it logical to assume that all irradiation, however low the dose, could cause irreversible DNA damage likely to develop into cancer, and therefore that the LNT model was valid, even for the lowest measurable doses. LNT therefore acquired the status of a scientific model, without any detailed discussion of its validity for estimating the risks of very low doses [133]. This validity has now been challenged [1,84,272,273], particularly in the light of recent demonstrations of the existence of mechanisms for safeguarding the genome (essentially involving DNA repair [10,15,56,192,251,298,302] and the elimination of cells whose DNA has been damaged via death. In themselves, these defense mechanisms would not have been sufficient to challenge the validity of LNT if their efficacy per unit dose had been constant irrespective of dose and dose rate. However, it is now clear that it is erroneous to assume such constancy. We knew that the repair effectiveness was greater at a low dose rate, but recent studies [60,73,241], by demonstrating the extent of these differences, have removed any scientific justification for extrapolations from high doses to low doses. The purpose of this report is, therefore, to update the multidisciplinary data (biological, biophysical, epidemiological) which make it possible to identify more clearly the quantitative and qualitative differences between low and high doses and their carcinogenic effects. 1.4 In order to take into account the variation in the probability of genotoxic effect per dose unit according to the dose rate in mammalian cells adjustments were introduced by ICRP, which implicitly recognize that LNT overlooks clinical and biological data. A dose, dose rate, effectiveness factor (DDREF) has therefore been introduced to describe the effects arising from exposure to a low dose of photons at a low dose rate. There is no consensus about the validity of this concept, either at UNSCEAR, or within ICRP Committee 1, which is responsible for evaluating risks. UNSCEAR had suggested a DDREF range of 2 to 10 to take the experimental data into consideration [281,282]. Somewhat arbitrarily, and conservatively, the ICRP [117] has adopted a DDREF of 2: the validity of this choice has been challenged [118]. 1.5 Improved understanding of the defense mechanisms of cells and tissues against low doses of IR suggests that their effect per unit dose must be much lower than in the case of high doses, but does not allow us to assess the respective carcinogenic risk. This is why the choice of the dose-effect relationship (linear, linear-quadratic -- i.e. both linear and quadratic -- or quadratic; with or without a threshold), in particular for the assessment of the risks of low doses, has to be based on knowledge of the genotoxic effects, the carcinogenic mechanisms, experimental and clinical data. The quantitative discrepancy between the results of the various epidemiological and animal 13 experimental studies supports the view that there are several dose-effect relationships rather than only one, and that their parameters depend upon the type of cancer, the type of ionizing particles, radiation dose, dose rate, fractionation of irradiation, species, breeding line within the same species, target tissue, volume irradiated, age, individual sensitivity factors and, possibly, co-factors interacting with radiation, such as exposure to other carcinogens. There is still controversy about whether a threshold exists [36,86,108,111,118,134,226]. A threshold could be due to the elimination of lesions from the genome by mechanisms including the absence of intracellular signalling, and therefore the lack of activation of DNA repair systems at very low doses or dose rates, and the combination of error-free DNA repair with the death of the cells of which the DNA has not been repaired [60,92,134,144,241]. 1.6 We shall examine subsequently the mechanisms of radiocarcinogenesis, the physical and biological phenomena caused by the exposure of cells, tissues and organisms to ionizing radiation, the experimental data on radiocarcinogenesis, and the epidemiological data. These topics are covered in more detail in the appendices. Finally, in the light of this data, we shall discuss the validity of the LNT relationship, and envisage the practical implications of these discussions. 2. The mechanisms of carcinogenesis 2.1 The process leading to the transformation of a normal cell into a tumor cell is interpreted as a Darwinian selection process determined by a series of genetic or epigenetic events, each of which gives the initiated cell a selective advantage in terms of survival or proliferation within the tissue to which it belongs. The main steps in this transition are analyzed in Appendix 1. First of all, the cell must be able to divide autonomously, i.e. it must autonomously produce growth factors or be able to proliferate without them, and it must have become insensitive to suppressor genes. Other events, such as impairment of the mechanisms of apoptosis and immortalization, are also necessary [100,101]. The conventional model acknowledges that, by a series of stages, modifications of the genome confer a selective advantage on the cell, during carcinogenesis [9]. We now know that these phenomena cannot be described by a linear process, during which successive genome damages accumulate at random. Carcinogenicity is a phenomenon that cannot be reduced to a series of mutations due to independent stochastic lesions occurring in the same cell. Indeed it affects all aspects of genome function [100,101]. The association of genetic and epigenetic mechanisms is now well-established [20,81,127,139,212,262]. 2.2 The cell, the tissue and the body all have defenses against carcinogenic processes, and these must be successively overcome for carcinogenesis to occur. 2.2.1 There are intracellular systems of proliferation control (suppressor genes), mechanisms involving the death of initiated cells that tend to eliminate or prevent the proliferation of cells in which a proto-oncogene has mutated into an oncogene, with damaged DNA, which do not obey systems regulating proliferation, or which are no longer receiving the growth factors required for their growth. Cell death therefore appears to be a main safeguard mechanism, in particular programmed death or apoptosis. The loss of a cell’s ability to kill itself may result from changes in the genes involved in this process [106] Ionizing radiation is likely to induce, at different levels depending on the tissues, apoptotic responses, which are the consequence of intra- and 14 intercellular signalling. However, IR can also induce mutations, which interfere with apoptosis and which therefore permit the survival of damaged cells, which in turn constitutes one of the steps in carcinogenesis [105]. 2.2.2 At the tissue level, we must emphasize the control exerted by neighboring cells (contact inhibition of proliferation, exchange of signalling and regulation molecules via intercellular junctions, bystander effect, secretion of regulation factors by neighboring cells and stroma). There are multiple interactions between a cell, in which a potentially oncogenic genetic event has occurred, neighboring cells of the same type, the extra-cellular matrix and the stroma. These interactions between cells play a crucial role in embryogenesis, in growth, in cell turnover of certain tissues in adults and in the regeneration of injured tissues. They are involved in the carcinogenic process, either inhibiting or promoting it. The exchange of information between the cell undergoing malignant changes and its microenvironment, the cytokines, (notably TGF-, which plays a crucial role in regulating cell proliferation) can, depending on the context, either slow or accelerate the carcinogenic process [19,26,29,151,299]. The microenvironment can either stop or stimulate the proliferation of clones of cells undergoing neoplastic transformation and affects the genetic instability [71,94,231]. Pathology studies had in fact already shown that tissue disorganization almost always preceeds the appearance of invasive cancer [57]. At low doses and low dose rates of ionizing radiation, the pro-apoptotic effect dominates and the damaged cells, of which there are only a few, can be eliminated or controlled. But at doses in excess of 0.5 Gy with a high dose rate, the greater number of mutant cells and the accumulation of mutations, the tissue disruption and above all the proliferation of the surviving cells to compensate for the death of a high proportion of the cells allow some cells to escape from these controls, which are intended to maintain tissue integrity and to regulate proliferation. These escape processes vary considerably depending on the tissues, the type of initiated cells (stem cells or progenitor cells) and the type of tumor as, for example, has been shown in the analysis of the carcinogenesis of multiple myelomas [71] and colo-rectal cancer [137]. In animals that have received chemical carcinogens, irradiation has little influence on the emergence of cancer [124], whereas, following X-ray irradiation, UV irradiation promotes the appearance of cancers. 2.2.3 At the whole body level, escape from the immune surveillance responsible for eliminating tumor cells is based on selection of cells that are capable of escaping from it [210], for instance by the loss of expression of the components of the major histocompatibility complex. Carcinogenesis may be facilitated by a reduction in immune defenses when a large segment of the body has been irradiated. 3 Physical and biological phenomena caused by ionizing radiation 3.1. Reactive oxygen species, formed by water radiolysis induced by irradiation, damage some cell constituents and produce oxidative stress. This oxidative stress stimulates enzyme systems that detoxify active species of oxygen formed and induces the synthesis of enzymes that destroy them. In parallel, oxidative stress also activates numerous signalling pathways [53,54,85,305]. 3.2 In the case of low Linear Energy Transfer (LET) radiations, such as photons or electrons, when the whole body is exposed to 1 mGy, each cell is on average crossed by one electron. Each electron induces on average 2 DNA lesions, including one single-strand break (SSB) 15 and 4 x 10-2 double-strand breaks (DSB) of the DNA molecule, and 10-4 chromosome aberrations. This initial effect is proportional to the dose as, in general, a DSB is not the result of two SSBs located opposite each other on the 2 strands and caused by different particles, but is the direct or indirect consequence of a high transfer of energy within or alongside a DNA molecule, mainly by means of radiation-induced reactive oxygen species [44,97,199,201]. The first physico-chemical events trigger a series of signals and reactions that can profoundly alter the fate of the DNA lesions. It is not the initial physico-chemical events that change, but their outcome. The defense mechanisms induced in a cell depend on the number and nature of cellular damages. The number of DSBs caused by a 1 Gy dose has been estimated to be 40 [44] and 30 by Vilenchik [290]. In contrast, the number of DSBs of endogenous origin, produced in each cell by the oxygen metabolism, remains controversial; it has been estimated to be 8 per day [44] and 50 per cell cycle by Vilenchik [290], who estimates that about 1% of SSBs turn into DSBs (there are about 3000 SSBs per day). In the light of theoretical considerations and in-vitro experimental studies, it has been proposed that ionizing radiations could induce multiple localized lesions, consisting of SSBs, oxidative damage to bases and clusters of DSBs, located within a distance of less than 20 base pairs within the DNA [96,115,200,201]. These very complex lesions are considered to be responsible to a large extent for the genotoxic effects of radiation. However, the number of such lesions induced in a cell and their impact have not yet been clearly established. With regard to the oxidative damage of bases and DSBs from endogenous sources, the variability of the published values suggests that all experimental variables are not entirely under control, in particular the degree of oxidative stress during the extraction of the DNA [46,232]. Furthermore, their number varies considerably depending on the rate of proliferation, as almost all of these endogenous DSBs are produced during the S phase. Moreover, the comparison between the number of DSBs due to cell metabolism and to irradiation is of limited significance, because the proportion of error-free repairs seems to be greater for endogenous DSBs than for those caused by irradiation. The dose rate at which the number of DSBs caused by irradiation is equal to the number produced during the same period of time by cellular metabolism in proliferating cells (endogenous DSBs) is 5 mGy /min; in both cases 0.14 DSBs occur per minute [290]. Note that at a dose rate of 1.5 mGy/min, the signalling systems are not activated, whereas they are at a dose rate of 5 mGy/min or more [60], a dose rate that approximately doubles the number of DSBs, from one DSB per cell every 7 minutes (basic rate) to 1 every 3.5 minutes. If it takes approx. 5 minutes to repair most DNA lesions, as some data suggest, lesions could then accumulate. It therefore appears plausible that the additional DNA lesions caused by low dose rate irradiation do not significantly modify the basic function of the constitutive repair systems (and the RBE), whereas irradiation delivered at higher dose rates activates other repair systems [60,289]. The rate of error free repair of DSBs caused by irradiation, and the time taken for repair vary considerably according to dose and dose rate [240,289], for example from 5 mGy/min. to 1 Gy/min. This leads to considerable variations in the yield of mutations. For very low doses (a few mSv), the numbers of DNA lesions (and therefore the biological response) may vary considerably from one cell to the other because of statistical fluctuations; nevertheless the absorbed dose absorbed remains the only parameter to which one can refer to. The DSBs caused by natural irradiation of 2 to 25 mSv/year only corresponds to a very small fraction of the total number of DSBs (less than 1‰) [44,86,289]. 16 Mitotic cell death or chromosomal aberrations seem to result from error prone rejoining when two chromosome breaks were generated close to each other in space (< 0.1 µm [225,227]) and in time on the same chromosome or on two neighboring chromosomes [62]. Thus, it is understandable that the probability of simple or complex chromosome exchanges is influenced by the dose rate [63,160] and that in addition to the linear component, the doseeffect relationship has a quadratic component [80] which disappears at very low dose rates [63]. 3.3 The irradiation of a cell causes several types of responses which modify the effects of irradiation, and therefore the radiosensitivity: 3.3.1 Oxidative stress (see §3.1) induces the transcription of many genes implicated in the signalling that activates cell defenses [70,85,142,305]. The efficacy of the defenses against reactive oxygen species decreases at high dose rates. 3.3.2 Different signalling systems are activated in yeast [168] and mammalian cells [15,16,70,302], after passage of an electron: cytosol (MAP kinases), mitochondria, nucleus (protein kinases). In addition, in the nucleus, different levels of damages lead to the activation of different families of genes [7,27]. 3.3.3 DNA damages or modifications of the chromatin are detected by signalling proteins. Their activity is modulated by the number of lesions (and therefore by the dose, the dose rate and LET) and by messages from neighboring cells. These proteins activate phosphokinase transmitters, in particular the protein encoded by the ATM gene (which is mutated in ataxiatelangiectasia) [138,215,251,302]. In turn, these transmitters modulate the action of proteins involved in cell cycle control (the interruption of which promotes repair), DNA repair [82,298], or in triggering apoptosis [172]. Studies carried out with the DNA micro-array technique in yeast show that continuous irradiation, at a dose rate of 20 mGy/h, i.e. lower than the level of irradiation that causes a detectable (lethal, mutational) biological effect, is enough to change intracellular signalling without modifying the genome [168] and to activate or inhibit numerous genes involved in the general metabolism and in defenses against ionizing radiation [7,37,53,177]. Such mechanisms bring into play defenses at doses of the same order as those due to natural irradiation, which makes it possible to reduce or prevent its potentially harmful effects. 3.3.4 For exposures greater than 1 mGy to photons or electrons, each cell is traversed by several tracks separated by time intervals inversely proportional to the dose rate. Some SSBs are quickly repaired with a half-time of approx. 5 minutes. DSBs are repaired more slowly and sometimes imperfectly [73,145]. As regards DSBs, we should distinguish between two situations: on the one hand, when the dose [241] or the dose rate [60] is very low, intracellular signalling and detection systems are not triggered below a certain threshold, therefore repair systems are not activated, and the damaged cells die. The elimination of these cells protects the organism against cells potentially undergoing malignant transformation [205]. On the other hand, at doses exceeding this threshold, repair systems are activated, which expose cells to a risk of misrepair, which is small at low doses but increases with dose and dose rate [73,147,240,289,290]. 3.3.5 The dose rate determines the average time interval between physical hits; it has a major effect on the cellular response. In general, the biological effects of irradiation (lethality, mutagenesis, chromosomal aberration etc.) decrease as the dose rate decreases [10,283]. The biological effect of the irradiation depends on two distinct factors: the greater efficacy of the DNA repair at low dose rates, and the probability of damaged cells to be eliminated by death. A very low dose rate can damage the DNA without activating the repair system and the 17 damaged cells die [60]. There is indeed a dose and dose rate threshold below which the intracellular signalling systems and therefore some DNA repair systems are not activated [60,241]. When the dose rate is low, the number of lesions simultaneously present in the cell is limited. Conversely, a high dose rate leads to the simultaneous presence of a large number of lesions. This high local density of lesions interferes with the coordinated action of repair systems, and also increases the probability of error prone endjoining [63] due to the presence of several DSBs in a restricted volume. 3.3.6 These conclusions regarding differences in the efficacy of the protection system are supported by various experimental or clinical data, which highlight the impact of repair on the biological consequences of irradiation: - the lack of any reduction in the mutagenic and lethal effect as the dose rate decreases in the cell lines in which the signalling or the DNA repair systems are impaired [207] or blocked, for example, in hereditary diseases with defects in repair systems (reparatoses). This lack of repair is also observed when yeasts or mammalian cells are exposed to gamma rays at 0°C (a temperature that inhibits the repair enzymes), the number of DNA double strand breaks is then identical at high and low dose rates, whereas at room temperature, it is much smaller at lower dose rates. - A dose of 80 Gy delivered over 14 days (at a dose rate of approx. 4 mGy/min.) does not cause the same rearrangement of the genome as that caused by DSB misrepair. However, when mutant cells deficient in non-homologous endjoining (NHEJ) are irradiated under the same conditions, rearrangement of the genome can be observed in approx. 10% of the cells [240]. Note that the technique used in this study (pulsed field gel electrophoresis) does not allow to detect small deletions or point mutations. 3.4 Variation of mutagenesis and lethality depending on the dose and timing of the irradiation. At equal doses, the mutagenic effect varies markedly with the dose rate [160,241,289,290]. When the dose rate increases , the mutation frequency after having passed through a minimum (hormesis?) increases strongly [289]. If the number of lesions which are present simultaneously is small, repair is generally more effective; thus it is more effective at a low dose rate than at a high dose rate. A limited number of lesions induces a reversible arrest of the cell cycle which enhances repair. A high amount of lesions prolongs the cell cycle arrest which can lead to apoptosis [82,205]. The time taken by repair depends on the complexity of the lesions and the repair system operating. A high local density of lesions reduces the repair efficacy [303]. 3.4.1 The lower lethality following fractionated irradiation cannot only be explained by the repair of DNA lesions between sessions. Recent data also show that the effectiveness and rapidity of repair depend on the time, the type of tissue and its proliferative status. 3.4.2. Initial hypersensitivity. For some cell types, mortality is very high (per dose unit) at the onset of irradiation (during the first two hundred mGy), then falls to a very low level before subsequently increasing again. This low dose hypersensitivity [53,54,60,126,165,176,241,253] is observed in many cell types (leading to a high mortality rate per unit dose) for doses of less than a few hundred mGy of low LET irradiation. An induced radioresistance is observed at doses of over 0.5 Gy; and the mortality rate per unit dose then becomes very low before increasing again [126]. These variations in the mortality rate (per unit dose) indicate that the cellular defense mechanisms against lethality, which initially show little efficacy, becomes more effective during irradiation. These rapid changes 18 in the mortality rate (per unit dose) are not correlated with either the cell’s capacity to undergo apoptosis or the defect in cell cycle arrest caused by irradiation. Conversely, stimulation of the activity of certain enzyme systems (PARP) by hydrogen peroxide, abolishes it [164], and inversely, a toxic substance, aminobenzamide, a PARP inhibitor, increases it [53], which demonstrates the role played by the induction of the enzyme systems in these variations of radiosensitivity. This initial hypersensitivity eliminates damaged cells with mutagenic potential after low doses of radiation[126]. 3.4.3. After high dose rate irradiation of short duration, sudden changes in radiosensitivity can be observed (increased mortality rate), which seem to depend on the activity of the PARP-1 enzyme [88,218]. 3.4.4 The existence of an adaptive response is now well established [173,297]: a first low dose of radiation leads to a reduction in the mortality of organisms in vivo [267], the number of mutations and the rate of neosplastic transformations [25,47,83,178,233,235,236,246] caused by a second irradiation carried out during subsequent hours or days. This inducible and transient protective effect seems to occur also in humans [93,265], and appears to result from a stimulation of cell defense and DNA repair systems. At the cellular level, an increase in lethality may be observed as a result of apoptosis and delayed mortality due to a bystander effect. Genotoxic physical agents (solar ultraviolet and ionizing radiation) were present when life appeared on earth, and very likely, at that time irradiation was generally more intense than today. Recent work has revealed the efficacy and multiplicity of defense mechanisms which developed during evolution. Many of these systems are targeted against reactive oxygen species produced by irradiation. 3.4.5 Some DNA repair systems are activated by low doses of ionizing radiation. DNA repair systems differ in terms of velocity and efficacy; in particular, the repair kinetics for DSBs and the probability of repair vary with dose and dose rate [240]. They are associated with apoptosis, that also varies with dose and dose rate [37,98,172,206]. Thus, although the number of lesions, in particular, that of DSB, is proportional to dose even at very low doses, at doses of a few dozen mGy, no damaged cells are found during the following days. The disappearance of damaged cells seems to result from the lack of activation of repair systems, which leads to an absence of repair and to cell death [60,241] or from high fidelity repair by constitutive systems [240]. When only a few cells are damaged, this elimination strategy seems to be optimal, because repair systems are sometimes error prone and can potentially lead to the emergence of pre-cancerous and subsequently cancerous cells. When a large number of cells in the same tissue are killed or damaged, repair and proliferation mechanisms are triggered, which are intended to protect the integrity and functions of the tissue. By means of intercellular communication systems the reaction of a cell to irradiation therefore seems to be influenced by the number of cells affected. Hence, the cell reacts to irradiation by a global and integrated response that involves several enzyme systems [22] which govern the efficacy of DNA repair and the probability of cell death eliminating damaged cells. Albeit although DNA induced damage is constant (per unit dose), the probability of mutation is modulated within a framework of what could be called a strategy of least cost. 3.4.6 Schematically, one can distinguish between four dose ranges. - At doses of a few mGy or low dose rates, no damage can be detected because the damaged cells die [60,241]. At these doses, the signalling systems are not triggered. Only constitutive repair systems, which are constantly active, operate (such as BER). 19 The doses or dose rates above which apoptosis is stimulated are lower than those that activate the repair systems. - For doses of less than about 100 mGy or those deliveredat low dose rates, damaged cells are eliminated or whenever possible, repaired by high fidelity mechanisms. When this elimination/repair mechanism has been induced by irradiation, it also acts upon the cells damaged by oxidative metabolism. In combination with the detoxification mechanisms induced by oxidative stress, these defenses can also explain the hormesis effect which is observed in experimental animals [11,25,50,79,84,87,174,233,244]. However, radiation-induced cell damage induced by low LET radiation differs from the damage induced by cell metabolism i) by a higher proportion of double strand breaks, ii) by the presence of clustered lesions (caused by the attack by hydroxyl radicals) and iii) by the more heterogeneous (non-compartmentalized) distribution of impacts at the cellular level. Another mechanism that could be responsible for a hormesis effect has been evidenced by in-vitro experiments: the selective death of cells that have been predisposed to neoplastic transformation. This seems to be dose related [235,236]. - At higher doses, over approx. 200 mGy, the concentration of damaged cells increases and the DNA repair systems supposed to avoid cell death and tissue injuries are associated with a risk of misrepair, which is greater when the number of lesions inside the cells is high [73,240]. In the absence of apoptosis, these errors lead to mutations. When apoptosis predominates, the risk of cancer is very low, but the tissue loses cells. When repair predominates, the risk of cancer increases. This is a phenomenon that is also observed during ultraviolet irradiation of the skin [78,273]. Because of these variations in effectiveness of DNA repair and in the probability of apoptosis (in relation to dose or dose rate), the carcinogenicity of irradiation increases more rapidly than the dose, leading to a curvilinear relationship. - Above 500 mGy, also a stimulated proliferation, in order to compensate for cell deaths, is observed. Cell divisions interfere with repair and increase the likelihood of errors[59,136]. The cell response therefore seems to depend on the dose, the dose rate and the cell type, and, without doubt, on the concentration of damaged cells. It varies over time. This strategy of defense that the organism raises against cellular lesions induced by ionizing radiation is distinct from, but somewhat similar to the strategy observed after ultraviolet irradiation. Once again, the accumulation of lesions hinders and delays repair, and therefore increases harmful effects per unit dose of exposure. 3.4.7 One can also draw a parallel between dose effect relationships for ionizing radiation and the numerous experimental data that reveal major differences between the toxicities of chemicals depending on dose, and that have shown very small (if any) carcinogenic effects of low concentrations [6]. However, these variations are also partly linked to changes in metabolism, which may contribute to non-linearity [50,238]. 3.5 Role of neighboring cells, bystander (or “abscopal”) effect and genetic instability. 3.5.1 In multi-cellular organisms, in particular vertebrates, the fate of an irradiated cell depends upon signals emitted by neighboring cells (gap junction, bystander effect, contact inhibition, proliferation control mechanisms by means of cytokines). Normal cells appear to be capable of inhibiting the development of potentially malignant clones [19,29,71,231]. 20 Many experimental data support this concept in the context of radiocarcinogenesis, for example, the influence of the volume irradiated on the likelihood of a carcinogenic effect [263], and the lower efficacy of heterogenous irradiation [167], in particular of irradiation through a grid [45]. Conversely, non irradiated cells can become cancerous in the vicinity of highly irradiated cells [19,41,42]. Besides an inhibitory effect (such as contact inhibition), or a stimulation of cell division, intercellular relationships can also elicit damage in neighboring cells, which have not been irradiated; this is known as the bystander effect. The influence of intercellular interactions on low dose hyperradiosensitivity suggests that there is a link between this phenomenon and the bystander effect [54] The bystander effect originates from potentially genotoxic signals sent to neighboring cells. There are at least two different mechanisms. The first is based on the production by cells exposed to low LET radiation, of “clastogenic” plasmatic factors, which can cause chromosome aberrations in neighboring or remote cells. This mechanism is independent from p53. Clastogenic factors can persist for years after irradiation, as has been shown in earlier studies on plasma of patients who have received radiotherapy [249], or of survivors of Hiroshima Nagasaki [209]. More recently, another mechanism has been initially demonstrated after high LET irradiation [193], which involves inter-cellular gap junctions [12,17,28] through which free radicals, likely to play a role in the bystander effect, can pass [28]. It is dependent upon p53 [122]. This mechanism causes a bystander effect in the immediate environment of the irradiated cells, which decreases as the dose increases [41,247]. This effect is considerably reduced when alpha irradiation is preceded by a low dose (20 mGy) of low LET radiation [178]. It therefore appears to be modulated by adaptive responses. Similar effects have been observed after localized irradiation of the cytoplasm, and the bystander effect has been compared to an inflammatory-type reaction. Various mechanisms are therefore involved in the so-called bystander effects (intercellular signalling, clastogenic factors, passage of active oxygen species and other molecules through gap junctions, stimulation of the production of reactive oxygen species). This “bystander signal” has many consequences for the unirradiated cells (apoptosis, induction of genetic instability, delayed cell death, mutations that are in 90% of cases point mutations and seldom deletions, which sugests that they are induced by reactive oxygen species). These effects depend upon many factors, which are still poorly identified. Mothersill [188,189] suggested that the bystander effect could induce in the neighboring cells an adaptive response similar to that induced by pre-irradiation (see §3.4.4.). These effects on the neighboring non-irradiated cells could therefore, depending on the context, have either protective or harmful effects; they are not proportional to the dose, but on the contrary appear to diminish with increasing doses [58,191]. The bystander effect is mainly expressed at low doses of alpha radiation [17,42]. After exposure to low-dose X-rays, it leads to the death of cells in which the repair of DNA damage is defective [190]. 3.5.2 It has been shown both in vitro and in vivo that approx. 10% of the descendants of irradiated cells display an abnormally high frequency of genome modifications, sometimes persisting after several tens of generations. This effect, which is known as “genetic instability”, was first observed in bacteria and yeasts [61], then in cultures of human cells and in mouse embryos after high LET irradiation (alpha particles) and after high doses of low LET irradiation (over 2 Gy) [129]. Instability can be induced in a cell when it is traversed by a single alpha particle (micro-beam)) [128]. Radiation-induced genetic instability varies 21 according to cell line, but does not seem to be caused by specific genetic lesions [129]. The bystander effect also induces an increase in genetic instability [153]. Since mutations also exist in non-irradiated cells, it is difficult to find out whether there is a threshold. Nevertheless, some experiments do demonstrate the existence of a threshold in some cell lines [166], but it is difficult to say whether there is a threshold in all cases [255]; what is clear is that the maximum effect is reached at relatively low doses (150 to 500 mGy) and that between 2 and 12 Gy, the incidence of genetic instability tends to remain at a plateau [152]. Various genetic abnormalities are observed in the descendants of irradiated cells: rearrangements and chromosome aberrations, gene amplification, aneuploidy, formation of micronuclei, microsatellite instability, mutations [152,153,237,255]. Several mechanisms can cause this instability, which can be interpreted as genomic changes that only become apparent in the descendants, as is suggested by the following: - the importance of the induction of genetic instability when there are changes in p53 gene [149]. - the reduction of genetic instability by the elimination of free radicals or when the cells are confluent (contact inhibition), which permits the repair of potentially-lethal lesions [150]; In most cases, this genetic instability appears to be the prelude to cell death, and there are proteins, such as clusterin which induce the death of such unstable cells by attaching themselves to the ends of the chromosome breaks [301]. This research area is developing rapidly [140,220]. The aim of this research is to find out whether this instability could play a part in the onset of late arising radio-induced cancers [154,227]. Some experiments suggest that this is the case, such as for instance the fact that the instability in mouse bone-marrow stem cells leads to non-specific mutations seen in radiation-induced leukemia [162]. However, other experiments do not support this hypothesis, and in the mouse, genetic instability does not seem to be involved in the initiation of leukemia [39]. Some strains of mice show high predisposition for the induction of genomic instability, whereas others show a high predisposition for radiation-induced leukemias and lymphomas: however, these strains are unrelated [40], which implies different mechanisms. In contrast, in other strains of mice, in which the predisposition for the induction of genetic instability is due to a DNA repair defect, one observes also a predisposition for the induction of breast cancers [207,219,278,279,304]: it thus would appear that in that case the susceptibilities to the induction of a breast tumor and to the induction of genetic instability are genetically co-determined, and a deficiency in the repair of DSBs (linked to a defect of DNA PKcs) may lead to permanent instability of the genome. There could also be a link between a deficiency in DNA repair, the instability of the genome and the integrity of the telomeres, however, it is not known which of these phenomena is the cause of the other [13,38]. These findings should be considered in relation to the studies that have revealed links between telomere dysfunction, impaired DNA repair and tumorigenesis [158,171] In this context, two human studies provide some interesting data. In the leukemias that occurred in elderly survivors of the atomic bomb explosions, an excesss of complex chromosome aberrations with translocations have been reported [195]. This supports the hypothesis according to which irradiation would trigger an early onset of genetic instability associated with telomere shortening [158]. In studies of a group of patients suffering from Hodgkin’s disease, M’Kacher et al. [179] have made interesting observations: 22 i) before treatment a notable increase (compared both to normal individuals and to patients suffering from solid tumors before treatment) in the frequency of simple and complex (with translocation and deletions) chromosome aberrations in circulating lymphocytes. The telomeres are shorter than in normal subjects or in patients suffering from other cancers. There is a correlation between telomere shortening and the rate of simple and complex chromosome aberrations. ii) After treatment (radiotherapy chemotherapy): there is a marked increase in the incidence of simple and complex aberrations, but this increase is not influenced by the dose and extent of the treatment (radiotherapy or chemotherapy). Hypermutability is present, which suggests a DNA repair defect, and which seems to be correlated with the high frequency of aberrations before treatment and the shortening of the telomeres. iii) There is a considerable increase in complications, in particular in second cancers in subjects who, before treatment, had a high incidence of chromosomal aberrations and after treatment displayed a marked increase in this incidence, whereas, on the contrary, second cancers seem to be rare in subjects with a small number of aberrations. The increase in this incidence and hyper-radiomutability are therefore risk factors that can be used to identify subjects who are likely to be susceptible to radiocarcinogenicity, although at present it is still not possible to identify the mechanism by which these factors contribute to radiocarcinogenesis. This may involve a genetic defect in DNA repair, since it is observed in both tumor tissues and in circulating lymphocytes, but viral infection is also a possibility. Active proliferation of EBV and papilloma virus is observed in these patients. The effects of irradiation and viral infection may therefore be associated. This study demonstrates both the possible role of genetic instability in radiocarcinogenicity when it is combined with other disorders, and the extreme complexity of the phenomena involved. As shown by these studies, cancer cells may involve [Fouladi 2000] genetic instability. Theoretically, instability might be transmitted via the parental germ cells to children. which would have lead to an increase in the cancer incidence in the children of parents who have been irradiated; however, this has not been observed in humans and can thus be ruled out [123]. Overall therefore, at the experimental level, the existence of direct link between carcinogenic effects and genetic instability remains hypothetical, in particular after low doses of low LET radiation [129]. However, genetic instability could be an indicator, cause, or consequence of cellular defects, such as impaired DNA repair. The most convincing evidence against the bystander effect and genetic instability playing arole in inducing human cancers is provided by studies on subjects contaminated by radium or thorium and followed-up until their death [52,91,229] over more than fifty years after contamination, and in whom no cancer was detected when the dose was below about 10 Gy, whereas there were many cancers at higher doses (see §5.5). If present in these individuals, the bystander effects or genetic instability would have shown up as a long term effect in the form of an increased cancer incidence. 3.5.3 Current studies highlight similarities between the adaptive response, the bystander effect and genetic instability [36,140,159]. These phenomena underline the importance of intra- and intercellular signaling in the biological effects induced by low dose radiation. It could be speculated that these phenomena could either increase or decrease carcinogenic risks. The bystander effect could induce an adaptive response in unirradiated cells leading subsequently to radioresistance [188]. Activation of enzyme systems are involved in the phenomenon of low dose hypersensitivity followed by an induced radioresistance (see 23 §3.4.2.), and in the W variations in radiosensitivity (§3.4.3). The mechanisms induced by irradiation, even at very low doses, therefore appear to be very complex, and arejust starting to be analysed. What is already clear, is that cells and tissues defend themselves by multiple and effective mechanisms against radiation-induced stress [69,74,84,111,216,300] The cell response is based on a complex network of intra-and inter-cellular signaling, and may be expressed in several ways, including the repair of damage, apoptosis, delayed death or prolonged quiescence of initiated cells. Very importantly, the modalities of the response are adapted to the context and vary according to the dose, fractionation, dose rate, LET, cellular redox-state, cell status before irradiation (in particular, whether or not integrity is conserved of the genes involved), and presence of signals emitted from neighboring cells and, possibly, of other toxic agents. 3.6 The subject of this report is ionizing radiation. However, it is apparent that most of its conclusions can also be applied to other physical (U.V. radiation) and chemical (genotoxic) carcinogenic agents, for which often, for administrative reasons there is also a tendency, to apply a linear no-threshold relationship. It seems that time has come to challenge this trend, whose scientific bases are questionable [1,6] and which can provoke unjustified fears and expenses. The problem is more complex for chemicals than for physical agents, because two aspects of the products studied have to be considered: their genotoxicity and their metabolism, which may include detoxification. Any toxic effect is the result of numerous biochemical reactions. Like X-rays, some agents are genotoxic by inducing directly or indirectly DNA lesions as a result of the production of highly-reactive chemical species (free radicals, potent electrophils, reactive species of oxygen), whereas others induce defense reactions. For each toxic effect, there are specific defense mechanisms. For instance, glutathione captures free radicals and electrophils, in the same way that metallothioneines trap heavy metals, whereas superoxide dismutases degrade the superoxide anion. The outcome depends on the balance between these two types of reaction. If the dose is low and defenses are sufficient, there will be no toxic effect. If the dose is high, and defense reactions are overwhelmed, like buffers when exceeding the pH , a toxic effect emerges and becomes proportional to the dose. It is likely that there are threshold doses or even hormetic effects, and many arguments have been put forward in the last decade suggesting that this is the case for chemical agents [125,148, 238]. In fact, the distribution of the results around a threshold is not random (if it were, there would be the same frequency of positive and negative effects), and the negative effects are more frequent, which is in favor of the hypothesis of hormesis [49]. This has been observed in approx. 40% of toxicological studies [50], i.e. a proportion similar to that observed in Duport’s meta-analysis [79] concerning experimental radiocarcinogenesis. 3.7 Overall, the genotoxicity of ionizing irradiation varies considerably, depending on the dose rate, the dose already received, and the time interval following the last exposure. These facts show that the cell’s reactions and its defense capacities are to a large extent determined by these factors. The cell is not passive, its response to an irradiation depends on intra- and intercellular signaling mechanisms, the characteristics of radiation and the state of the tissue. Elimination of damaged cells by death is effective when there are only a few damaged cells around; but it challenges survival of the organism when there is a high number of such cells. In this case, it is necessary to repair the DNA damage even if it may include error-prone repair and the induction of mutations. Mutations rise proportionally more rapidly than the dose and with the dose rate [240,289,290]. The efficacy of cellular defense mechanisms is very high in the dose range corresponding to natural irradiation (1 to 20 mSv/year), but it declines at higher doses. The question is above which dose it declines. Furthermore (see §2), the likelihood that an initiated cell escapes from cell and tissue control increases with the number of cells killed and 24 the tissular disorganization. More data are given in Appendices 1 and 2. 4 Experimental animal data Animal experimentation has made a major contribution to our understanding of the carcinogenic effects of ionizing radiation, and has confirmed the efficacy of DNA repair mechanisms from the simplest to the most complex organisms. In multicellular organisms, there are also additional mechanisms that can eliminate mutant and potentially carcinogenic cells or control their proliferation. Nevertheless, when the dose is high enough carcinogenic effects have been reported in all species [116]. However, the proportions of radiocancers vary, depending on the species, age, sex and tissues concerned and the dose-effect relationships are very variable. It has been possible to carry out numerous experiments regarding settings for which there was no epidemiological data available, and to assess the role of the following: - the type of radiation: X, gamma, beta, alpha, neutrons, protons, fission fragments [198], - the dose rate,dose fractionation and less uniform dose distributions as they may occur after internal contamination [281], - concomitant exposures to other genotoxic agents [283] and the size of irradiated volume [263]. Few studies have evidenced an effect of low doses. Animal experiments benefit from specific, potentially favorable conditions such as the control of exposure conditions and thegenetic homogeneity of laboratory animals, the short life span of rodents, making it possible to replicate studies, routine histopathological examinations, the relatively large number of animals included in the studies (a few tens of thousands of rats and mice and a few thousand Beagle dogs). Despite these favorable conditions, it has neither been possible to establish a statistically significant carcinogenic risk for doses less than 100 mSv, nor to exclude its existence, which is obviously much more difficult. With only few exceptions, no excess tumors is observed below 500 mGy for low LET radiations [283]. Animal experiments, notably in the mouse, allow to study dose-effect relationships for cancer induction over a large range of external exposure levels [95,275,276,277,284]. A large number of data is compatible with a linear-quadratic model [116,282]. However, some data are not satisfactorily fitted with this model. In properly conducted studies in the mouse, some data are better fitted by a quadratic relationship without a linear component [183,245] or by relationships with a threshold [64,74,163,300 ] than by a model with a linear, no-threshold component. In rats, a considerable reduction in the carcinogenic effects has been observed with low LET, low dose and low dose rate radiation. This attenuation is particularly obvious after contamination of the lungs by beta and gamma emitters [14] and after exposure to radon [21,184]. Attenuation is observed for all the tumors induced by external low LET irradiation [186]. This observation explains why the RBE (Relative Biological Effectiveness) of neutrons increases constantly as an inverse function of the square root of the neutron dose without ever levelling off [135,296]. This suggests that photons exhibit dose-effect relationships that either have a threshold, or are purely quadratic. Threshold relationships have also been established for pulmonary tumors induced by alpha radiation in rats [246,247], and for bone tumors in dogs [230]. However, in 25 the case of thyroid tumors after exposure to iodine131 the diminution due to dose rate remains open to question [197]. In general, heterogeneous irradiation, in particular following internal contamination by radionuclides, shows major reduction of the low dose rate effects, with a quasi-threshold, in most cases [196,217]. This lower efficacy compared to the same dose of uniform irradiation seems to be associated with the control exerted by neighboring cells [19]. This same phenomenon is also observed in human beings (see §5.5). Among the experimental studies in which the incidence of cancer was sufficiently high in control animals, a reduction of this incidence was observed following low dose irradiation in 40% of them, an observation which is consistent with the concept of hormesis. This finding does not justify generalization of this concept [286], however, it does confirm its existence [79,174,244]. Appendix 3 provides more detailed information. 5 Epidemiological data For doses above approx. 200 mSv, epidemiological data permit to establish with fair accuracy the relationship between dose and carcinogenic effect. However, for low doses (below 200 mSv) and a fortiori below 20 mSv generally encountered within the context of radioprotection, epidemiology can neither confirm nor refute the existence of an increased incidence of cancer. In order to estimate the effects of these low doses, three conditions need to be satisfied: - hundreds of thousands of subjects must be included and monitored for a sufficiently long time; this is stressed in the article by Brenner [43] that is discussed below. - the absence of any correlation between the dose received and all the other potential risk factors (such as tobacco) should be established. If such factors are present, they must be taken into account by appropriate statistical methods. This point is particularly important with regard to the study of low doses, because the specific effect of the confounding factors can be much greater than the effect of radiation. It is not enough to postulate that such a correlation has no logical reason to exist; it is necessary to establish that it did not appear by chance in the sample studied. For example, in a study investigating the risk of lung cancer due to radon in homes, not taking smoking into account would make the results impossible to interpret [66]. - accurate information must be available about all exposures to ionizing radiation, including those unrelated to the source of irradiation being investigated. This is difficult, given the frequent and possibly repeated exposures to small doses of radiation: natural irradiation (differences of natural irradiation can reach 20 mSv/year), X-ray examinations, air travel. Often these exposures are not controlled or integrated into the calculation of the dose studies. They may introduce biases even when they are smaller than the irradiation investigated. 5.1 Many epidemiological studies on cohorts that are often very large have been performed in order to quantify the carcinogenic risk associated with exposure to ionizing radiation. These studies, listed in Appendix 4, cover a wide range of conditions: age and gender of subjects, pathological conditions (patients treated by radiotherapy or apparently normal individuals), type and duration of exposure, dose and dose rate. These studies encounter so many methodological and logistic difficulties that it is justified to 26 perform a rigorous analysis of the conditions under which each of them has been conducted. The main problems are as follows: - Solid tumors and leukemia have a spontaneous incidence which is high and which varies according to lifestyle. Moreover, the possible increase in this incidence following irradiation is relatively low, so the studies must have sufficient statistical power, which requires large cohorts. - The difficulty of obtaining accurate dosimetry is encountered in many studies. Collective dosimetric determinations are imprecise and individual determinations are sometimes difficult to obtain. Usually, it is only in medical studies (diagnostic or therapeutic irradiation) that doses can be estimated with accuracy on the basis of medical records. Dosimetry is also reliable in workers wearing dosimeters. - The variability of the conditions of exposure of the population studied and in dosimetric accuracy make meta-analyses difficult to perform although not impossible. However, hopefully, they can be more powerful from a statistical point of view than single studies. - For doses lower than 100 mSv, almost all studies do not evidence a significant effect. Nevertheless, they could provide an upper boundary to the possible carcinogenic effect, though they cannot rule out the existence of a small risk. Since the time of Aristoteles, we learned that it is impossible to prove the absence of a risk. 5.2 In the field of low doses, the available data can be classified into three groups: A-bomb survivors who received a low level of irradiation during the explosions (high dose rate); data obtained in residential or working environments (low dose rate irradiations); data obtained after diagnostic or therapeutic procedures (high dose rates and fractionated irradiation). 5.2.1 In the analysis of the incidence of cancers in the survivors of the Hiroshima and Nagasaki bombs (HN), leukemias and solid cancers have been distinguished. With regard to radiation-induced leukemias, the dose-effect relationship is statistically incompatible with an LNT relationship and shows a threshold at approx. 150 mSv and a decrease in spontaneous risk (hormesis?) at doses lower than 100 mSv [155,156]. There has been considerable controversy about the dose-effect relationship for solid tumors; the latest analysis reveals that the dose effect relationship is not linear but curvilinear, possibly linear quadratic with a fairly similar value for the parameters [224]. This new data benefited from a longer follow-up and from the revision of the dosimetry in 2002 [132]. At low doses, the excess risk of death due to solid cancers per Sv (ERR/Sv) is now estimated to be 0.19 (95%CI: 0.03-0.37) [224], i.e. less than half of the previous estimation [223]. Preston et al. limit the scope of this relationship for evaluating the risks, by invoking anomalies in the distribution of the excess relative risk for the lowest doses; it is difficult to accept this reasoning, particularly, because the RBE of the neutrons can, at very low doses, have values very much greater than 10, about 30 or more [291]. Such high RBE value would lead to a revision of some of the high excess relative risk (ERR) in the range of very low doses which presently cause these doubts. The linearity of the first part of the curve (linear component of the linear quadratic relationship) should be reconsidered, and the contribution of low LET irradiation to solid tumor excess in the range of low doses should be reassessed. Incidence data have not yet been revised; the ERR seems to be similar in the ranges 5-50, 50150, 50-500 mSv and 50-4000 mSv, and the dose-effect relationship is compatible with an LNT model but also with a model with a threshold that could be up to 60 mSv or with a quadratic relationship [213]. The correction of the RBE for neutrons should reinforce the hypothesis of a threshold for the photon contribution. A possible influence on the risk of 27 cancer of injuries sustained during the bombings has also been reported [260]. 5.2.2 Several other studies have shown that low doses, delivered at low or high rates, either have no statistically significant effect on the increase in mortality or the incidence of cancers, or have significantly lower effects than those predicted on the basis of the risk coefficients calculated on the basis of the HN data. For example, the data obtained for the 21,500 workers at the Mayak complex show an excess relative risk of death of 0.15 for solid cancers (90%IC: 0.09-0.20), lower than that observed in the HN cohort; however, the dosimetry (external and internal) for plutonium remains quite imprecise [250]. Similarly, a recent study on 8600 people involved in cleaning up after the Chernobyl accident, who had received a mean dose of 50 mSv, shows an incidence of all cancers which is 12% lower than that of the general Russian population. There is no dose-effect relationships [121]. Similarly, the analysis of the incidence of leukemias in these workers did not reveal any significant dose effect relationship [146]. The IARC’s meta-analysis relating to 96,000 workers in the nuclear industry [51] had shown a risk of death by leukemia with doses higher than 400 mSv (the risk is, however, half of that of the HN estimations) and no significant increase in deaths from solid tumors. An extension of this meta-analysis to 600,000 workers is under way. It includes 9 other studies conducted on workers in the nuclear industry (Japan involving 171,000 workers, USA 125,000, United Kingdom 106,000 and 13,000, France 58,000 and 22,400, Finland 16,000, Russia 11,000, Slovakia 2,700). Amongst radiologists and radiology technicians who started work in the 1960s (or 1970s in China) and who received annual doses in the region of 10 to 50 mSv, and therefore cumulative doses of several hundred mSv, studies of large cohorts have shown that the cancer risk is not significantly increased (USA 87,000 [180,181,254] and 117,000 [76], China 17,000 [292], England 1,400 [23]. In all these studies, no excess risk was observed for particularly sensitive organs such as the breast, thyroid and hematopoietic tissue. Airline flight crews receiving exposures of 1.5 to 6 mSv per year have been studied. No increase in the total number of cancers or of cancers in the most radiosensitive organs has been detected in 44,000 members of flight crews [31,306] or in 2,740 Canadian pilots [18]. An excess of melanomas was observed in these populations, and this can be explained by their more frequent exposure to the sun. 5.2.3 As the epidemiological studies including hundreds of thousands of people who have been occupationally exposed to tens of mSv are not powerful enough to detect or exclude a statistically significant risk for doses below 100 mSv, it appears that only comparisons of populations exposed to different natural levels of irradiation could provide quantitative information about the effect of low doses (< 20 mSv/year) administered at very low dose rates, but they have to be carried out on sufficiently large populations. Currently, the studies carried out in regions where the natural natural irradiation is markedly higher than in France do not evidence any correlation between the level of natural irradiation and cancer mortality, although chromosomal aberrations in the circulating lymphocytes confirm the high level of irradiation [268]: the Indian State of Kerala (up to 70 mSv per year [194]); the Chinese region of Yangijang, (comparative monitoring for ten years of 100,000 inhabitants of zones at 6, 4 mSv and 2 mSv per year [262,264,293,294]); Japan (irradiation due to radon [169,202,256]). In all cases, the dose rates are very low. Studies are in progress to confirm these initial findings, their updating should bring interesting information. Within the framework of medical diagnostic irradiation (high dose rate), none of the studies 28 including a reconstitution of the exposure based on medical records or on another reliable dosimetry has shown an increase in the risk of leukemia after radiological examinations, even if repeated, for doses lower than 100 mSv [32,35,67,258]. The only study showing an excess risk was based on non-verifiable case studies and witness interviews, bias could therefore been introduced [228]. With regard to thyroid cancer,there is no data showing that they can be caused by frequent radiological examinations in children or adults [90.120]. Three cohort studies have shown an increase in the risk of breast cancer after repeated radiodiagnostic examinations, with a linear dose-effect relationship from 100 mSv upward; relative risk decreases markedly with age at the time of exposure [32,77,109,114,170,222]. None of these studies has shown any increase in risk below 100 mSv. A meta-analysis of doses of less than 100 mSv, in particular between 50 and 100 mSv would be very useful, Appendix 4 shows that this could be done. In this context, it is important to point out that, although fractionated doses of the order of 10 mGy lead to an increase in the risk of breast cancer, for a cumulative dose of the order of one Gy [113] (the breast is the only organ for which this has been demonstrated), it does not seem justified to conclude that a single dose of 10 mGy is carcinogenic as the recent draft report by the ICRP does [118]. In fact, the study of women followed up for pneumothorax is informative only for doses above 500 mGy: below this dose, the excess risk is virtually nil, 9%, and not significant. It would also be interesting to check whether these women, who were suffering from tuberculosis, had the same other breast cancer risk factors as the general Canadian population, in particular, with regard to age at the first pregnancy and the number of children. In radiotherapy, the doses are much higher and are administered at a high dose rate. Tissues not located in the target volume receive doses ranging from several mGy to several Gy. This risk has been assessed in several studies including several thousand to one hundred thousand patients, and it varies considerably with the dose and age of the irradiated subjects. For example, an increased risk of cancer has been found in 160,000 women cured of cervical cancer and treated by radiotherapy, but without any carcinogenic effect on organs that had received less than 50 mGy [34]. In children for a same given dose, the excess of cancers induced is greater, and the types of cancers induced are different. A signficant excess in the relative risk of breast cancer (2.25 with IC: 0.59-5.62) was found in women treated during childhood with radiotherapy for hemangioma, with mean doses of 1.5 Gy on the breast [161]. A purely quadratic dose-effect relationship, without a linear component, has been observed in a cohort of 7700 women treated by radiotherapy at the Institut Gustave Roussy for breast cancer [243]. The risk in this case is much lower that that observed in the HN cohort and is negligible for doses lower than several Gy. The relative risk is 0.003 for a dose of 1 Gy. Is this because the irradiation is delivered during 5 sessions per week and the dose per session can vary from 2 Gy per session in tissues located in the target volume to very much lower doses per session in tissues located outside the target volume? This hypothesis has led to analyze the influence of the dose per session; the data show that no carcinogenic effect is observed for doses per session of less than 160 mGy (even though the total dose can reach 5 Gy), whereas a significant carcinogenic effect is observed for high doses per session. This effect of fractionation has been confirmed by the study of the number of sessions. The data suggest that doses administered by fractions of 150 mGy or less, delivered at intervals of 24 hours, do not cumulate their carcinogenic effect, which could be due to the elimination of damaged cells or the repair of lesions (see §3)). These results would be worth confirming. It has been possible to make comparisons between patients treated by external radiotherapy at high dose rate (1 Gy/minute) or by implantation of radioactive sources (1 Gy/hour). The reduction in carcinogenic effect in the latter case is in accordance with what is observed in 29 animals. Metabolic radiotherapy with iodine131 results in much lower dose rates than with external radiotherapy. The administration of iodine-131 does not increase the risk of thyroid cancer in adults (10,000 patients treated for hyperthyroidism [110] and 36,800 subjects who have had scintigraphies [72]. No effects were observed in children, the numbers of children studied were limited (1900 under 20 and 800 under 18 years of age [99]), and their average age was higher than that of the children of the former USSR who developed thyroid cancer following Chernobyl. Amongst the 2000 thyroid cancers observed after Chernobyl, 80% of patients were under 5 years old at the time of the accident. These children, who were generally deficient in iodine, were exposed to iodine-131 but also to iodines with shorter half-lives (in particular 132I), responsible for high dose rates. Note that amongst the 2 million children whose thyroids were irradiated as a result of Chernobyl, some received doses higher than 1 Gy. No excess thyroid cancer has been observed outside the former USSR, even in Poland. A study is being carried out by the IARC, on the evaluation of doses received by children suffering from thyroid cancer in Russia and Belarus. 5.3 Medical irradiation in utero has been the subject of a large-scale cohort study known as the “Oxford Study” [75]. This study concluded that cancer risk was increased at doses of about 10 mSv. Although conducted rigorously, this study is not without weaknesses, and is not consistent with some other data. 5.3.1 In the 807 children exposed in utero in Hiroshima and Nagasaki and monitored until 1992, the upper boundary of the excess relative risk was 0.6% for 1 mGy [68], a value only one tenth of that obtained [30] in the Oxford study (5.1%, with a confidence interval of 2.8 to 7.6). Furthermore, the Oxford studies on the one hand, and the studies by Monson and McMahon [185] on the other, did not find any increased risk for children who died before the age of 10 years, whereas the Hiroshima Nagasaki study covers a longer follow-up. No increase in the incidence of the various types of leukemia following irradiation in utero was detected in a Swedish study (198 bis)The very limited number of cases in these studies makes it difficult to put a value on the risk, and some authors [33,208,269] feel that the positive findings of the Oxford study might be linked with a memory bias, or to underlying maternal disorders which required X-rays during pregnancy, rather than the irradiation itself. 5.3.2 The excess risk found in the Oxford study is similar for almost all cancer sites (leukemias, lymphomas, neuroblastomas…), whereas in all the other populations studied, the dose-effect relationships are very different depending on the tissues and organs: in the survivors of the HN cohort, who were exposed when very young, one observes, for example, an excess relative risk of about 17 per Gy for leukemias, but of only 2 per Gy for other cancers. 5.3.3 For doses of over 100 mSv, animal experiments have shown that there is indeed a carcinogenic risk in dogs, rats and mice, after irradiation in utero during the late stages of development [116]; however, they do not demonstrate that the embryonic tissues have a greater susceptibility to carcinogenesis or radiosensitivity than tissues of young animals, except in a few tissues, such as the nerve tissue in the rat [187] and the ovary in the mouse [280]. 5.3.4 Twin pregnancies are monitored more closely than other pregnancies. For this reason, in the past, they were submitted to approx. twice as many diagnostic radiological examinations [282]. Comparisons between the incidence of cancers in populations of twins with the incidence observed in the general population has therefore provided an opportunity to evaluate the effects of irradiation on the subsequent cancer risk. Studies of twins avoid the potential bias of other studies, because the reason for having more X-ray examinations is not 30 associated with problems occurring during the pregnancies (which could be linked to a pathology that itself, and irrespective of any irradiation, involves a subsequent risk of cancer for the unborn infant). Apart from a single case-control study (with regard to which a case history bias cannot be ruled out, as cases tend to remember the details of exposure better than controls) [102], these studies do not show excess cancers in twins [239], with some showing a considerable reduction in the incidence of cancers [119.182]. It therefore appears that the data on the carcinogenic effect of in utero irradiation has not sufficient robustness to be the basis for evaluating the risk of low doses in children and adults. 5.4 Overall, with the possible exception of the results of in-utero irradiation, no correctly conducted epidemiological cohort or case-control study has been able to detect any carcinogenic effect for doses of ionizing radiation of less than approx. 100 mSv in adults. Some of these surveys have studied populations of large size, their total being much larger than the population of survivors of Hiroshima and Nagasaki. Although some sources of information suffer from shortcomings, such as the absence of individual dosimetric estimations for radiologists (which decreases the power of the studies), others do not. In several of these studies, the dosimetry is of high quality and is based on fewer non-verifiable hypotheses than that for the Hiroshima and Nagasaki survivors. The epidemiological data do not therefore provide any convincing argument in favor of a LNT relationship at doses lower than 200 mSv, but they do not rule out the possibility that there could be a carcinogenic effect within this dose range. The search for the relationship most closely matching the available data should be continued. However, it should be emphasized that the dose-effect relationship probably varies markedly with the tissue, the age at irradiation and above all, with the dose rate. There is no scientific justification for assuming that only one type of relationship exists. Given the specificity of the body’s defense mechanisms at low doses, the epidemiological studies can only provide information about the carcinogenic effect by specifically studying populations that have received doses likely to cause similar biological effects (for example, between 30 and 80 mSv as a single dose), rather than including much higher or lower doses. This procedure should avoid incorrect conclusions. However, given the smallness of the effects (if they exist) the confidence intervals are likely to be large, which make it hard to reach any conclusions. This explains the interest of studying natural irradiation, which can involve very large numbers of subjects. 5.5 Carcinogenesis by long half-life -emitting radionuclides When an -particle crosses a nucleus, the dose received by the cell is approx. 370 mGy and from 1 to 20 events can occur in the DNA molecules, causing important damage. Most cells are killed, but not all because cancers do occur. However, relatively few cells are affected, and they are surrounded by normal cells; Painters of luminous dials contaminated with radium-226 and 228 have been subjected to several investigations covering over fifty years of monitoring [52,91,242,257,266]. Other investigations have studied patients who had received thorotrast, a thorium-based contrast product used in the past in vascular radiology [8,203,270,271,287]. They have also been monitored for more than 50 years. Painters of luminous dials have presented a high frequency of osteosarcomas, but no excess cancers have been observed for absorbed doses of less than 10 Gy [52], contrasting with a 31 marked increase for doses of more than 20 Gy. Patients who have received thorotrast have presented hepatomas. In this case also, a threshold is observed: at about 2 Gy for hepatomas. Several non mutually-exclusive hypotheses have been put forward to explain the lack of effect with lower doses, which contrasts with the very high incidence with larger doses [273]: 1. It might be necessary for several alpha-particles to cross the cell to trigger carcinogenesis. 2. The process triggered in a cell can lead to cancer only if the adjacent cells are nonfunctional (which, in the case of -particles would necessitate high doses) and so no longer exercise normal tissue control on the proliferation of the initiated cell. 3. If there are few cells damaged, these are eliminated by apoptosis, this elimination would not take place when there are large numbers of damaged cells. 4. Cells that cause cancers may not be induced directly but by a bystander effect. This mechanism is effective only at high doses. On the basis of present knowledge, it is difficult to choose between these hypotheses but these data show that, with this type of irradiation, the bystander effect and radiation-induced genomic instability do not cause cancer when the number of damaged cells is small. Moreover, none of these hypotheses is compatible with the postulates on which the LNT relationship is based. 6 Validity of the linear no-threshold (LNT) relationship The LNT model used in 1956 by Russell to evaluate the radio-induced mutations in the germ cell line in the mouse, was introduced between 1960 and 1980 for the purposes of regulation in radioprotection with regard to all mutagenic and carcinogenic effects in Man. At that time, this was a convenient pragmatic relationship but not a model based on data [133]. A predictive value was subsequently attributed to this linearity at a time when people were unaware of the complexity of carcinogenesis, and the diversity and effectiveness of the responses of a cell to irradiation. The rapidly growing knowledge in the last decade should lead us to reconsider the validity of the hypotheses on which the use of LNT has been based for assessing the carcinogenic effect of low doses (< 100 mSv) and a fortiori of very low doses (< 10 mSv) on the basis of that observed in the range of doses of 0.2 to 3 Sv. 6.1 The LNT model postulates that the cell reacts in the same way regardless of dose rate and dose, which implies that the probabilities of death and mutation (per unit dose) and the contribution to carcinogenesis of each physical event remains constant irrespective of the number of lesions in the cell and in the neighboring cells. This constancy implicitly admits several hypotheses: 1. In the range of the doses and dose rates under consideration, there is no physical, chemical or biological interaction between the effects caused by the various tracks of ionizing particles in a cell. 2. Any absorbed dose of energy in a cell nucleus leads to a proportional probability of mutation. The probabilities of successful repair or misrepair (per unit dose) are always the same. Similarly, the probability of apoptosis does not vary with dose. 32 3. Any DNA lesion has the same probability of giving rise to a cancer, irrespective of the number of other lesions in the same cell and the neighboring cells. 6.2 These hypotheses are not consistent with current radiobiological knowledge that could be tentatively summarized as follows (see §3): 6.2.1 The oxidative stress induced by the irradiation induces defense mechanisms against the reactive oxygen species; the effectiveness of these defenses varies with dose. 6.2.2 The dose rate influences the effectiveness of DNA repair and of mutagenesis (see §3). The signaling systems are not activated for dose rates of less than about 5 mGy/min, apoptosis is triggered by doses of over 5 mGy and the repair system (and therefore the possibility of misrepair) is triggered from about 10 mSv. These figures are only indicative and far from being definit. Moreover, within this range of very low doses, they can vary considerably from one cell to another, depending on the damage produced in DNA [86]. They also vary depending on the cell line and tissues. Despite these fluctuations, the data show that the safeguard mechanisms and their effects (elimination by death of damaged cells, and the probability of error free and error-prone repair) vary with dose and dose rate (see §3.4.6). 6.2.3 The radiation-induced cell mortality (per unit dose) varies during the cell cycle, although the probability of DNA damage is the same; the change in the mortality is therefore mainly attributable to differences in the probability of error-free repair depending on the cell cycle phase. 6.2.4 The probability of DNA misrepair increases with the dose rate and dose. Similarly, the lethal or mutagenic effects (per unit dose) vary considerably with dose and dose rate. In particular, from about 0.5 Gy, the initial hyperadiosensitivity (see §3.4.2.) decreases and then disappears, as a result of the activation of repair systems. 6.2.5 Most of the cells with unrepaired DNA lesions are eliminated either by death, when these lesions are not repaired, or by triggering apoptosis. In vitro, the damaged cells disappear at very low dosesbut this is not the case at doses above about 10 mSv (see §3.3.4 & 3.4.6). The efficacy of the elimination of potentially mutant cells varies with the dose, the cell line, and the tissue [206, see §3.4.5.]. In the work of Hendry [104,105], concerning the apoptosis of intestinal crypt cells after gamma irradiation, apoptosis reaches a plateau at doses of 200 to 400 mGy. The experiments of Rothkamm [241] have shown that after a low dose, 24 h after the irradiation no cell with a DSB can be detected; this disappearance can be due either to cell death caused by the absence of repair, or to a combination of error-free repair and apoptosis. The lower the dose or the dose rate [60], the more effectively lesions are eliminated (see §3.4.5). At doses above a few tens of mSv, the larger dose rate or dose by fraction diminish the efficacy of the safeguard mechanisms probably linked to the increased number of intracellular lesions (see §3.3.3., 3.3.1, 3.3.5, 3.3.6, and 3.4) 6.2.6 The adaptive response (see §3.4.4.) results in a temporary induction of the defense mechanisms, which proves that their mobilization reduces the mutational effect. 6.2.7 No excess of chromosome aberrations has been reported for doses of less than 20 mSv for low LET radiations, despite the attempts made to evidence them [283]. Thus, there may be a threshold for this effect. The generally accepted form of the dose-effect relationships for chromosome aberrations is linear-quadratic. This makes it possible to reliably determine the dose for chronic irradiation, and for the dose reconstitutions after accidents. However, although the linear-quadratic relationship forecasts a small level of aberrations, at low dose 33 and dose rates no effect is detectable below 20 mSv, either because the initial slope of the linear component is less steep than that calculated from doses over 100 mSv, or because there is a practical threshold (see §3.2), and perhaps even a hormetic effect. This is an important problem because chromosome translocations and deletions play a fundamental role in carcinogenesis. The lack of validity of the LNT relationship for chromosome aberrations at low doses with low LET radiation is not surprising [62] since the occurrence of a chromosome aberration is observed when there are two or more DNA double-strand breaks in the same chromosome or neighboring chromosomes, and that the rejoining of the fragments either does not restore the molecule to its initial condition (inversion or translocation within the same chromosome), or even rejoins fragments that do not belong to the same chromosome. The probability of such error-prone endjoining therefore depends on the number of breaks simultaneously present in a limited volume, and therefore decreases markedly with dose rate and is not proportional to dose but to the square of the dose. LNT cannot be used to predict chromosome aberrations for very low doses (see §6.5.3). 6.2.8 The dose-effect relationship for cell lethality is not linear but linear-quadratic. The phenomenon of initial hyperadiosensitivity shows that it is necessary to introduce a correction into the linear-quadratic relationship for doses of less than 200 mGy. All data clearly show that the efficacy of defense mechanisms against the lethal effect and the mutagenic effect of ionizing radiations, varies with the cell line. This efficacy appears to be in all cell lines very high at low doses and dose rates such as those delivered by the natural irradiationbut it declines at higher doses. These variations in the efficacy with dose is not surprising since these mechanisms have emerged during evolution to protect procaryote cells against the lethal effect of the natural ionizing (or U.V) radiation. After the appearance 600 million years ago of multicellular organisms the aim of defense mechanisms was also to protect multicellular organisms against the appearance of mutant cells. 6.3 The process of carcinogenesis (see §2) As discussed earlier, mechanisms exist to protect multicellular organisms against the cells that have escaped the systems that controls cell proliferation within the tissues. The effectiveness of these mechanisms can be overcome or impaired by high doses (mutation of the genes responsible such as p53). 6.3.1 In animals, depending on the species (and strain in mice), the tissue and type of cancer, the dose-effect relationship for carcinogenesis is extremely variable and is seldom linear. In animal, not only does a threshold seem to exist, but also in 40% of experiments, there is even a hormesis [79]. Dose rate has a major influence. Furthermore, heterogeneous irradiation is less effective than homogenous irradiation, and the size of the irradiated volume is important, which would not be the case if only damage to the DNA in the initiated cell were involved. 6.3.2 In vitro, in studies of the neoplastic transformation of hybrid cells (hela-fibrostart) the incidence of transformation is not increased at doses between 0.5 mGy and 220 mGy, and there is even a reduction in the incidence of spontaneous transformations at doses between 0.5 mGy and 11 mGy [141]. According to UNSCEAR [283], no cellular neoplastic transformation is observed at doses of less than 100 mSv. Other data show that low-dose irradiation can reduce the number of transformations [233,234,235,236]. 6.3.3 Carcinogenesis does not seem to be attributable to a simple, random accumulation of independent DNA lesions. Some cancers are caused by a specific translocation, whose frequency is too high to be explained by stochastic phenomena [272] and which cannot be 34 attributed to lesions induced directly by the radiation [273]. The epigenetic mechanisms (which seem likely to have a threshold) play a notable role. 6.3.4 In Man, carcinogenesis is a complex process that varies depending on the tissues and types of cancer involved, and in which genetic and epigenetic mechanisms are associated (see §2). The extreme susceptibility to radiocarcinogenesis in some human diseases with DNA repair disorders shows the essential role played by repair systems in this process. The efficacy of these systems is modulated by various factors, in particular, by the dose and dose rate (see §3). 6.3.5 During carcinogenesis, the micro-environment and the interactions between the initiated cells and the normal cells, as well as the mechanisms regulating proliferation linked to the tissue organization play a capital role (see §2.2.2 and 4). The proliferation of the initiated cell is controlled by the neighboring cells within the tissue (see §2.2.2). Tissue disorganization often heralds the emergence of a cancer [57]. Possibilities of escape certainly do exist but these are increased after a dose that has killed a high proportion of cells (> 0.5 Gy), and has therefore disorganized the tissues. The acceleration of the proliferation induced by a high dose (> 0.5 Gy) could interfer with the repair of lesions, and allow cells to escape from control mechanisms. 6.3.6 At the level of the whole organism, immunosurveillance has an important role (see §2.2.3). The impairment of immunosurveillance mechanisms after irradiation of a large segment of the organism could account for the increase in the carcinogenic effect in this case [263]. The high incidence of cancers in immunodepressed patients (AIDS, patients treated with immunodepressive drugs after an organ transplant) confirms their efficacy. It is difficult to imagine that phenomena that are as complex and as variable from tissue to tissue, and which depend on the nature of the initiated cell (stem cell or progenitor cell [48]) and the volume irradiated [263], depend solely on the lesions produced in the initiated cell. The hypothesis that the incidence of radiocancers can be predicted by simple proportionality with the dose received by the cells also conflicts with the absence of radiocarcinogenicity of -emitting radionuclides at low doses (see §5.5). The concept that radiocarcinogenesis is a stochastic phenomenon must be revisited [272]. 6.3.7 That a cancer could be induced by very low doses is a possibility which cannot be excluded, but all the available biological data indicate that at very low doses the combination of the failure to repair the DNA damage [60,241] leading to cell death ( apoptosis) and errorfree DNA repair should make this risk minimal or non-existent [143]. These phenomena, and the effort to counteract reactive oxygen species may account for a hormesis effect [49,50,79,86,87,125,130]. Hormesis could also be explained in part by stimulation of immune mechanisms [157,286]. Some preliminary data suggest that a hormesis effect can be observed in humans [55,131,155,285]. 6.3.8 The hypothesis has been made that the bystander effect (see §3.5.1) and the induction of genomic instability could cause a significant number of cancers at low doses, and that they could even lead to a supralinear dose-effect relationship at low doses. However, this hypothesis does not seem plausible (see § 3.5). In humans (see § 5.5) and in animals (see §4), the existence of a threshold after contamination by αalpha-emitting radionuclides makes it possible to exclude a significant contribution of a bystander effect when only a few cells are affected in an undamaged tissue. The animal data (see §4) demonstrate a hormesis effect, highlighting the implausibility of this hypothesis. 6.3.9 Epidemiology (see §5) cannot exclude one of the two following hypotheses: i) the absence of a detectable carcinogenic effect at doses of less than 100 mSv is due to the 35 insufficient statistical power of the surveys or ii) it is attributable to the lack of any carcinogenic effect due to the existence of a threshold. The data relating to contamination by -emitting radionuclides (radium, thorium) in animals and humans does definitely demonstrate the existence of a threshold in some situations. Scientific rigor demands that when looking for a universal model we should first analyze all the epidemiological data for doses between 50 and 100 mSv, and then look for a model compatible with all radiobiological and epidemiological available data. Assuming linearity is a precautionary not a scientific attitude. It is not consistent with the recent data regarding solid tumors in survivors of Hiroshima-Nagasaki [224, 291]. Using LNT to estimate the carcinogenic effect at doses of less than 20 mSv is not justified in the light of current radiobiologic knowledge. 6.4 Article by Brenner et al. 2003. In 2003, several well-knownradiobiologists and epidemiologists published an article that puts forward arguments in favor of a linear nothreshold relationship (LNT). Their conclusions differ from those in this report. 6.4.1 – Biological arguments This article considers that a carcinogenic effect occurs in humans after acute irradiation with a dose of 10 mSv. At this dose, approx. 10 electrons cross the nucleus, and the authors rightly state that there is no interaction between the physical events caused by each electron. They deduce from this that a single electron (1 mSv) causes a carcinogenic effect equal to a tenth of the effect caused by 10 electrons. This reasoning ignores the defense reactions triggered in the cell, it only considers physical events and overlooks defense reactions caused by initial cell damage. The physical events caused by each electron are identical, but the cell defenses induced by doses of a few mSv (when the nucleus is crossed by several electrons) activates detoxification by enzymatic systems of reactive oxygen species and signaling mechanisms (see §3). 6.4.2 The induction of carcinogenesis after irradiation of the fetus at a dose of about 10 mSv is still open to question (see §5.3). Furthermore, extrapolating from the fetus to the child or adult is debatable. For many tumor sites in the range of doses between 50 and 500 mSv the carcinogenic effect varies markedly with age. There are grounds for thinking that the differences might be even greater between a fetus and a child, even a young child. 6.4.3 Studies carried out on survivors of atom bombs 6.4.3.1. All authors agree that there is no significant increase in the incidence of cancers (for all ages and both sexes) below 100 mSv. However, as at lower doses, there is a nonsignificant increase, but with a similar excess relative risk (ERR), Brenner et al. [43] deduce from this that one can consider all subjects who have received between 5 and 125 mSv together as they constitute a homogenous group and that there is a significant increase for this whole population. This conclusion is questionable from a methodological point of view. The significant excess observed for this whole group could indeed be due to a simple increase in power due to the greater number of subjects in the 5-125 group than in the 5-100 group, as the authors postulate. However, it is also compatible with the existence of a threshold at a few tens of mSv or a non-linear relationship. Therefore, this excess cannot be used as an argument in favor of LNT. 6.4.3.2 In fact, studies have shown that the HN data are compatible with a threshold of about 60 mSv [155,156,213]. Brenner et al. [43] have over-interpreted the findings suggesting a linear relationship with a consistent slope between 0 and 125 mSv. They overlooked the unreliability of that apparent constancy of the slope and did not take into acount the large confidence intervals of each point. Indeed, the new data published by Preston [224] now correspond to a curvilinear relationship. The nonlinearity of the new data would be even 36 greater if a higher value of the RBE had been used for the neutrons at low doses [291], in accordance with the experimental data. There is therefore no convincing evidence that casts doubt on the traditional conclusion (an increase above 100 mSv, no significant increase for doses due to low LET radiation below 100 mGy) (see § 5.2.1). This conclusion has the advantage of concurring with other epidemiological data and with the leukemia data from Hiroshima and Nagasaki. 6.4.4. The other studies used in this publication to support the carcinogenic effect of doses lower than 100 mSv seem to have been selected arbitrarily. The study of thyroid cancers after irradiation of the scalp for treatment of childhood ringworm suffers from a dosimetric methodological bias, and it is the only study to draw the conclusion of an increased risk at doses this low, whereas several similar studies on the same topic did not find the same result. Two other investigations quoted on leukemia in children in areas contaminated by the fall-out from Russian and American nuclear tests [65.259] are based on geographical correlations, which suffer from the limitations of this type of study. Their results are in disagreement with those of other studies of the same type conducted on the consequences of the Chernobyl accident [211] and with the results of all the cohort or case-control studies carried out on leukemias after irradiation in childhood, including studies on survivors of Hiroshima and Nagasaki. 6.4.5 Altogether, therefore, the article by Brenner et al. [43] does not prove the validity of a linear no-threshold relationship, or even the existence of a significant excess of cancers at doses of less than 100 mSv. This conclusion is not surprising, because the authors themselves state that a much larger number than in the HN cohorts would be necessary in order to show the possible effect of low doses. This discussion underlines the importance in this area of a multidisciplinary approach, combining epidemiology and biology. 6.5 A draft report of an ICRP task group was posted on the Web in December 2004 [118]. It discusses the problems raised by the choice of the relevant dose-effect relationships. This document, of high scientific quality, analyses recent radiobiology data. However, and sometimes surprisingly, the conclusions of the various sections and the general conclusion although recognizing that one cannot rule out the hypothesis of a threshold, which is described as being very plausible, do advocate the use of the LNT, at least on a provisional basis. The main arguments advanced in favor of this position are as follows: 6.5.1 At the epidemiological level, the authors feel that it is very likely that there is a carcinogenic effect in Man of a dose of 10 mSv, given the effect on the fetus in utero and the breast cancers observed after repeated fluoroscopies to monitor pneumothorax. They also consider that the findings of other surveys, despite being statistically without significance, do suggest that there is a carcinogenic effect between 10 and 100 mSv. In reply, we can say that: 1. the data from the Oxford study of in-utero irradiation are too unreliable to provide scientific validation for LNT (see §5.3 and §6.4.2), and that furthermore, they concern the fetus. Extrapolation to a child or adult calls for caution. Finally, even if this effect were to be confirmed, it would not justify extrapolation to doses of less than 10 mSv since we know that a dose of about 10 mGy activates repair systems that could cause misrepair, whereas these systems are not activated by lower doses [60,241]. 2. the carcinogenic effect of repeated X-ray examinations is only observed when the cumulative dose exceeds 0.5 Gy. Indeed, very few women in the cohort investigated in the publication cited by the ICRP task group [113] had received doses of less than 500 mSv. This publication does not provide any information about the effect of these 37 doses. This study therefore demonstrates that doses of the order of ten or a few tens of mSv can have an additive effect, if the cumulative dose reaches 500 mSv or more, but not that ten mSv are carcinogenic [113]. 3. A study showing a non-significant increase cannot be used to deduce that a risk exists. At the very least, what needs to be done is to review all the studies carried out after such doses and to compare the frequencies of positive, negative and nul effects. Until this preliminary work has been done, no indication can be drawn from data that are not statistically significant. 6.5.2 At the radiobiologcal level, the authors indicate that a high proportion of the lesions induced by ionizing radiation are complex and difficult to repair, and so cannot be compared to lesions of endogenous origin. In addition, they also stress that apoptosis is an effective mechanism but there is nothing to indicate that its is totally effective, and so, it is conceivable that some damaged cells could survive, avoid the control and give rise to a clone of initiated cells. These comments are pertinent, but in reply, we could point out: 1. that it is unlikely that the cells with complex lesions that are difficult to repair would avoid being eliminated by death (mitotic death or apoptosis), 2. in fact the problem with regard to LNT does not lie here, it is finding out whether the probability of misrepair is the same if the number of genomic lesions is low or high. The LNT model is based on the assumption that the probability of each DNA damage to transform a normal cell into a neoplastic cell and for this neoplastic cell to give rise to an invasive cancer is constant whether this damage is isolated or is associated with other damages in the same cell and in neighboring cells. Rather surprisingly, this crucial question has not been dealt with in that report. However, all the data available show that this probability in fact varies with dose (see §3). Similarly, the efficacy of apoptosis is not constant, but varies with dose. No apoptosis occurs if the genes implicated, such as p53, have been damaged. 3. the probability that an initiated cell will escape depends on tissue organization. If its tissue structure has not been perturbed, the initiated cell may remain quiescent in the tissue for many decades and possibly until death (see §5). The very rapid fall in the incidence of lung cancers in smokers after smoking cessation (even if they had previously smoked for twenty years of more) demonstrates the prominent role of promotion mechanisms, i.e. the influence of cell proliferation and tissue disorganization in the escape of the initiated cell. This observation also shows that initiated cells can remain quiescent until the death of the subject. Indeed, microcancers are found during autopsy in 10 to 30% of people over 60 years of age. An escape from control regulations is always possiblebut it is unlikely if the tissue has retained its organization undamaged (see §5.5 ). Furthermore the absence of any carcinogenic effect at doses of several hundreds of mSv in some tissues, such as the small intestine, bone, skin, and even the breast and thyroid of adult subjects, highlights the importance of the tissue structure and the safeguard mechanisms since the genome is the same in all cells. For the thyroid and the breast, the difference between the radiocarcinogenicity seen in small children illustrates the role of tissue organization and intercellular relationships. The latter strongly influence carcinogenesis (see §2). 6.5.3 The authors affirm that the frequency of chromosome aberrations is a linear function of the dose. 38 Reply: UNSCEAR report 2000 [283],pointed out that despite the attempts to find them, no aberrations have been detected at doses of less than 20 mSv. Above this dose, the relationship is linear-quadratic for low LET radiations (see §3.2). At very low dose rates (about 1 mGy /min) the relationship is linear for doses of 20 to 100 mGy but the efficacy, estimated in terms of the number of aberrations per unit dose, is much lower (about 20 times lower) than that of doses delivered at a high dose rate [63]. 6.5.4 The authors think that it will be possible to rule out the possibility of a carcinogenic effect due to the genetic instability and to the bystander effect induced by low doses only when the mechanisms of these effects have been elucidated. Reply: It can be noted that much of the data suggests that there is a threshold or a dose-effect relationship for these two phenomen. Moreover, despite the efforts made, no evidence has been found of any carcinogenic effect at low doses (see §3.5.2). The absence of any carcinogenic effect after contamination with -emitting radionuclides (see §5.5) makes it unlikely that these mechanisms contribute significantly to carcinogenesis in humans. 6.5.5 The authors feel that the animal data support a LNT model. Our conclusions disagree on this point (see §4). We feel that the importance of hormesis should not be overlooked. Hormesis has been reported in 40% of the animal experiments [79], moreover, the biological bases of hormesis now seems to be understood [87], and its existence is beyond question [50]. In addition, Tanooka’s meta-analysis [262] shows that there is a practical threshold for virtually all experimental tumors. The viewpoint that simply introducing a DDREF factor will allow these facts to be taken into account does not appear justified. The influence of the dose rate and of fractionation on carcinogenesis in animals shows that the phenomena are too complex to be accounted for by a LNT model. 6.5.7 Conclusion: This very high quality report shows that we cannot rule out the possibility of a carcinogenic effect at doses of the order of 10 mGy. However, when the arguments presented are analyzed, it appears that this effect, if it exists, must be very low for such doses. The authors have not analysed differences in the efficacy of safeguard mechanisms related to dose and dose rate. Their report assumes that the efficacy of the defense reactions is constant which is inconsistent with current data. It does not establish the validity of the LNT model between 10 and 100 mSv. The hypothesis of a carcinogenic effect for doses of less than 5 mGy is implausible, even if it cannot be completely ruled out. Further research is needed. However, in the meantime, it would be detrimental to put too much weight on the very hypothetical risk when balancing cost and benefit of X-ray examinations [274]. Most Xray examinations deliver doses of less than 5 mGy, the estimation of their risk must be based on plausible scientific data; overestimating this risk would have a harmful impact on the health of populations. The LNT model cannot be used to estimate the effect of very low doses, particularly, because it considers all solid tumors together. In this pooled study, the relationship may seem to be linear only because for each of the cancers concerned the doseeffect relationship is different. At the beginning of the preliminary ICRP report [118], it is stated that the concept of a collective dose, which is a direct consequence of the LNT model, assumes that a very low dose administered to a large number of subjects has the same carcinogenic effect as a higher dose administered to a small number of subjects, and that the available data suppport this assumption. The present report comes to an opposite conclusion; it considers that for a given 39 collective dose, the risk is much greater when doses of more than 0.2 Gy are delivered than when the doses are below 20 mGy. 7 Implications of the dose-effect relationship The hypothesis of a linear no-threshold relationship should be considered as a tool which is useful for regulatory purposes because it simplifies the administrative task. However, it is at the price of a probably marked over-estimation of the risk of doses lower than a few dozen mSv. It is not a model validated by scientific data [84,133,272,273]. A dose-effect relationship is used in different contexts: 7.1 For the protection of people occupationally exposed to ionizing radiation. If the irradiations received are considered to be additive and independent, and the dose rate is not taken into consideration, then the reference to a linear, no-threshold relationship is implicit. The limit doses which are recommended seem to have considered industrial possibilities rather than aiming at a scientific assessment of the health risk. With present industrial techniques, they are easy to comply with, except in a few specific cases. On the other hand, in some medical professions (interventional radiology), the annual limits constitute a constraint, the appropriateness of which has not really been assessed, and the consequences of which with regard to some medical professions, and therefore for some patients, might be detrimental. 7.2 The ALARA principle is based implicitly on the concept of a LNT relationship because it postulates that the lowest dose may be harmful when it is given to a large number of individuals. For decades, doses received occupationally were relatively high, and it was justified to aim at reducing them. At present, one may wonder whether the ALARA principle is justified in all circumstances because the values reached are sometimes so low that to reduce them any further would have no meaning in terms of improving public health, since the number of cancers avoided by means of complex and expensive practices would probably be extremely small or zero. The money spent in this sector should be subjected to a rigorous cost-benefit analysis and compared to expenses in other areas of public health. 7.3 The choice of the dose-effect relationship influences the priorities of public health in terms of radiation protection. If the LNT model is selected, a desire for effectiveness would tend to lead to reducing the low doses received by the greater number. On the other hand, if low doses are thought to present very little or no danger, this costly reduction is unnecessary, and efforts should instead be made to reduce the higher doses. This example shows that any prevention strategy is implicitly based on quantitative assessment of the risks [295]. 7.4 In medical practice, one could similarly be led to concentrate efforts on the most common examinations (chest X-rays) rather than focusing on those that deliver the highest doses to the most vulnerable subjects (CT scans in children). We fear that the former strategy would be counter-productive. In medicine, diagnostic or therapeutic procedures using ionizing radiation must, like any medical procedure, be subject to the principle of justification. The legislation explicitly requires the risk of irradiation involved in a procedure to be weighed against the expected benefit to the patient6, thus it is necessary to compare two potential Article R.43.51 of the Code of Health amended by modified by Administrative Order 2003-270 of March 24 2003 concerning the protection of individuals exposed to ionizing radiation for medical and medico-legal purposes and which transposes European Directive 97/43 specifies: 6 40 health risks. A risk assessment based on linear no-threshold dose-effect relationships [24], would lead to an over-estimation of the risks of of X-ray examinations, and would therefore distort comparisons of the benefits and risks of these examinations [274]. - Thus the LNT relationship could lead to the refusal of useful examinations because of a hypothetical risk. Conversely, if we consider that the risk (per unit dose) increases with the dose, then efforts should be focussed on situations in which examinations (for example CT scans for children) or their frequent repetition results in doses of more than a few tens of mSv. This strategy seems to be more pertinent than attempting to reduce the doses for all examinations, which would be more costly and probably be less effective. - In the case of therapeutic irradiation, on the other hand, the doses are much higher, and the risks clearly identified. It is therefore necessary, as with any therapeutic procedure, to evaluate for each patient the benefits of treatment versus its adverse effects, and to look for irradiation techniques, which make it possible to reduce the volume of normal tissue exposed to doses greater than approx. 150 mGy per session( §see 5.2.4). 7.5 Finally, this LNT relationship is often applied incorrectly to large numbers of people, multiplying the effects of trivial doses by large populations on the basis of a LNT model. One example of this erroneous use is to “calculate” the number of deaths induced if millions of people were exposed to a few micro-sieverts. These calculations based on collective doses do not have any meaning, as UNSCEAR and ICRP have pointed out. Nevertheless, some people are still applying them, which leads to inappropriate conclusions (for instance evacuation of a large population after the Chernobyl accident). Without any scientific justification, these calculations propagate the idea that even a very small dose of radiation is dangerous. The debate around radioactive waste and the calculations of risk based on the LNT model show that the form of this relationship and the calculations that are based on it do not contribute to an understanding of the biological and medical problem, and can, on the contrary, make them more obscure. 8 Proposals 8.1 Thanks to new techniques of molecular biology, considerable progress has been made in the past decade in understanding the mechanisms of action of radiation at the sub-cellular and cellular level and the defense reactions of the cell, tissues and the whole organism against the carcinogenic effects of ionizing radiation This ability of living organisms to defend themselves against aggression is not surprising, and was established in the 19 th century (Claude Bernard). Without it, living species would not have survived. Advances in biology have enabled a better understanding of these mechanisms; nevertheless more detailed investigation is possible and should be performed. The efficacy of defense mechanisms, the diversity of the strategies used by the cells, the tissues and the whole organism to reduce or eliminate carcinogenic risk are now better understood. They strongly suggest that a threshold or a practical threshold does exist and even, for some cancer sites, as in animals, so does a hormesis effect. It seems that during For the application of the principle mentioned in §1 of article L. 1333-1 (this concerns the principle of justification. Editor’s note.), any exposure of any individual to ionizing radiation for purposes of a diagnosis, therapy, occupational medicine or screening, must be subjected to a preliminary analysis to ensure that this exposure provides a sufficient direct medical advantage relative to the risk that it may involve and that no other technique is available, which is of comparable effectiveness and involves less risk or does not carry any such risk. 41 three billion years of evolution in a sea of ionizing and ultraviolet radiation living beings have developed systems of defense and repair capable of preventing harmful effects due to doses of the same order of magnitude as those received due to natural radiation (1 to 20 mSv/year). These defenses seem to be overwhelmed at higher doses and the effect of intermediate dose zones should be determined, especially for doses between 20 and 100 mSv at high dose rates and moderate irradiations (< 500 mSv) at low dose rates. In these areas, efforts should be made in epidemiology (meta-analyses, analysis of the frequency of the different types of cancers and the age of the subjects affected) and in cell biology. Determining these risks quatitatively is a main goal [204,295] but one that is difficult to achieve by epidemiology alone, even by comparing geographical regions that receive different doses of natural irradiation. This means that surveys must be associated with biological research. Dose-effect relationships have to be used for estimating the risks, in particular, the carcinogenic effects. Experimental and clinical data show that the shape of the dose-effect relationship varies considerably, notably with regard to its initial part, depending on the type of cancer, the age of the subject and the characteristics of the irradiation. A relationship obtained for all the solid tumors of individuals of various ages may appear to be linear, even if for each of the cancers under consideration it has a very different shape. Such a relationship may be of pragmatic interest with regard to radiation protection within certain dose limits but has no scientific validity for predicting the effect of much smaller doses, given the complexity of radiobiology and carcinogenesis. 8.2 Many attempts are currently being made to improve the modeling of the stages of radiocarcinogenesis by introducing recent cell biology data [48,103,108,214]. Efforts should be made in this field in order to estimate the upper limit of the risks. 8-3 Research is mandatory in several other areas. Here is a non-exhaustive list. 1. Epidemiological studies make it possible to investigate the effect of very low doses (< 20 mSv) notably those comparing the frequencies of cancers and congenital malformations in regions where the natural irradiation is high (> 10 mSv/year). Few studies have been carried out in this field in Iran [93] and Brazil, even though in these countries there are regions with particularly high natural irradiation. However, it is also necessary to develop other epidemiological studies likely to provide information in the 50 to100 mSv dose range and to analyze the histological type of the excess cancers. In epidemiological studies, for instance, we need to find out which types of cancer are in excess and the age of the subjects affected in order to find out whether, between 50 and 150 mSv, these characteristics are different from those of the general population. There are major discrepancies between the data published; we need to find out how to interpret them and envisage meta-analyses. 2. Experimental studies of the reductionof the cancer rate after irradiation or exposure to a genotoxic agent (hormesis). The interest of the dose-effect relationship and possible hormesis effect extends beyond ionizing radiation because of their possible implications for the evaluation of the toxicity of chemical genotoxic agents. It would be proper to coordinate the research carried out in these areas. 3. Research in radiobiology should help us to understand and quantify the effect of low doses (< 100 mSv), and of very low doses (< 10 mSv). The bystander effect, genetic instability and adaptive response deserve more research. In radiocarcinogenesis, the role of the tissue and stroma factors and the control exerted by normal cells need further investigation. Huge progress has been made in recent years in these areas, and 42 they have paved the way for further research. Differences in the dose-effect relationships depending on age and tissue should be investigated. We are beginning to understand why tissues such as the small intestine and the skin are so resistant to radiocarcinogenesis but the influence of age on the predisposition to radiocarcinogenesis of the thyroid or mammary gland deserves further research. We should explore the contribution of genetic factors to radiocancers [248]. 4. On the practical level (radiodiagnosis), major efforts should be made to reduce the doses received during examinations delivering more than 5 mSv, especially, in the case of children. 5. Investigations of the biological mechanisms triggered by exposure to combinations of genotoxic agents (smoking and radon or UV-Xrays, for instance [252]), should be continued. So far, this research has tended to conclude that there is an additive effect rather than a synergistic one, except in the case of radon and smoking, where inframultiplicative synergism is observed [112]. 6. In the field of public health, it should be useful to discuss when a carcinogenic effect becomes significant for a society and at which level it is pertinent to take it into account. It would be also of interest to define to which extent the representation of a risk may influence the means which are devoted to fight against it. It is impossible to banish all the risks from a society but it is difficult to establish a hierarchy amongst them and to determine the cost and the benefits of every procedure, notably radiological procedure. 7. It is also necessary to carry out research in the field of sociology in order to investigate the perception of the risk of radiocarcinogenesis, the concept of acceptable risk, and more generally the reactions of the society with regard to the medical and industrial use of ionizing radiation [261]. Radiophobia, which did not exist until 1950, i.e. several years after the first atomic explosions, actually became preeminent in the mid-1950s. It would be interesting to investigate its sources and consequences, and more generally to study when the fear of risk becomes an obstacle to scientific and technical progress in our society. Acknowledgements The authors would like to thank Ethel Moustacchi, Elisabeth Robert, Raymond Ardaillou, Pierre-Yves Boelle, Jacques Esteve, Vincent Favaudon, Miroslav Radman and André Rico for their help and advice. 43 References 1. Abelson PH. Risk assessment of low level exposure. Science 1994, 265, 1507. 2. Académie de Médecine - Communiqué « Energie nucléaire et santé ». Bull. Acad. Natl Med. 1999, 183, 1233-1246. 3. Académie de Médecine – Avis : Irradiation médicale, déchets, désinformation, Bull. Acad. Natl. Med. 2001, 185, 1671-1679. 4. Académie des Sciences – (Paris). Problèmes liés aux faibles doses des rayonnements ionisants. Rapport n° 34, 1995 (English translation: Problems associated with the effects of low doses of ionizing radiation. Report n° 38 1997). 5. Académie des Sciences (Paris). Colloque « Risques cancérogènes dus aux rayonnements ionisants » Comptes-Rendus, Série III, Sciences de la Vie, 1999, 322, 81-256. 6. Ames BN, Gold LS. Environmental pollution, pesticides and the prevention of cancer. Faseb J 1997, 11, 1041-1052. 7. Amundson SA, RA Lee, CA Koch-Paiz, ML Bittner, P Meltzer, JM Trent, AJ Fornace, Jr., Differential responses of stress genes to low dose-rate gamma irradiation. Mol Cancer Res, 2003. 1: 445-452. 8. Andersson M ; Storm H.H. Cancer incidence among Danish thorotrast-exposed patiens. J. Natl. Cancer Inst. 1992, 84, 1318-1325. 9. Armitage P., Doll R. The age distribution of cancer and a multistage theory of carcinogenesis. Br J Cancer 1954, 8, 1-12. 10. Averbeck D. Mécanismes de réparation et mutagenèse radio-induite chez les eucaryotes supérieurs. Cancer/Radiother 2000, 4, 1-20. 11. Azzam EI, de Toledo SM, Raaphorat GP, Mitchel EJ. Low-dose ionizing radiation decreases the frequency of neoplastic transformation to a level below the spontaneous rate in C3H 10T1/2 cells. Radiat. Res. 1996, 146, 369-373. 12. Azzam EI, de Toledo S, Gooding MT, Little JB. Intercellular communication is involved in the bystander regulation of gene expression in human cells exposed to very low fluences of alpha particles. Rad Res. 1998, 150, 497-504. 13. Bailey SM, Cornforth MN, Kurimasa A, Chen DJ, Goodwin H. Strand-specific post replicative processing of mammalian telomeres. Science 2001, 293, 2462-2465. 14. Bair WJ Experimental carcinogenesis in the respiratory tract. In Upton AC, Albert RE, Borns FJ, Share RE eds. Radiation carcinogenesis, New York Elsevier Applied Science Publishers 1986. 15. Bakkenist C.J., Kastan M.B. DNA damage activates ATM through intermolecular autophosophorylation and dimer dissociation. Nature 2003, 421, 499-506. 16. Bakkenist CJ, MB Kastan, Initiating cellular stress responses. Cell, 2004;118: 9-17. 17. Ballarini F., Biaggi M., Ottolenghi A., Sapora O. Cellular communication and bystander effects : a critical review for modelling low-dose radiation action. Mutat Res 2002, 501, 1-12. 44 18. Band P, Nhu D, Frang R, Deschamps M, Coldman AJ, Gallagher RP, Moody Joanne. Cohort study of Air Canada pilots : mortality, cancer incidence and leukemia risk. Am J Epidemiol 1996 ; 143 :137-143. 19. Barcellos-Hoff MH, Brooks AL. Extracellular signaling through the microenvironment: a hypothesis relating carcinogenesis, bystander effects, and genomic instability. Radiat Res 2001, 156, 618-627. 20. Baylin S.B., Herman J.G. DNA hypermethylation in tumorigenesis TIG, 2000, 16, 168-174. 21. BEIR IV, Health Risks of Radon and Other Internally Deposited Alpha-emitters, Committee on the Biological Effects of lonizing Radiations, National Research Council (National Academy of Sciences, Washington, DC), 1998, p.602. 22. Bernstein C, H Bernstein, CM Payne, H Garewal, DNA repair/pro-apoptotic dual-role proteins in five major DNA repair pathways: fail-safe protection against carcinogenesis. Mutat Res, 2002. 511: 145-178. 23. Berrington A, Darby SC, Weiss HA, Doll R. 100 years of observation on British Radiologists: mortality from cancer and other causes 1987-1997. Br J Radiology 2001, 74, 507-19. 24. Berrington A., Darby S. Risk of cancer from diagnostic X-Rays, estimates for the UK and 14 ther countries. Lancet 2004, 363, 345-351. 25. Bhattacherjee G., Ito A. Deceleration of carcinogenic potential by adaptation with low dose gamma irradiation. In Vivo 2001, 15, 87-92. 26. Bhowmick NA, Chytil A, Plieth D, et al. TGF-beta signaling in fibroblasts modulates the oncogenic potential of adjacent epithelia. Science 2004, 303, 775-7. 27. Bishay K, Ory K, Olivier MF, Lebeau J, Levalois C, Chevillard S. DNA damage-related RNA expression to assess individual sensitivity to ionizing radiation.Carcinogenesis 2001, 22, 1179-83. 28. Bishayee A, Hill HZ, Stein D, Rao DV, Howell RW. Free radical-initiated and gap junction-mediated bystander effect due to nonuniform distribution of incorporated radioactivity in a three-dimensional tissue culture model.Radiat Res. 2001, 155:335-44. 29. Bissel M.J., Radisky D. Putting tumours in context. Nature Reviews/Cancer 2001, 1, 4654. 30. Bithell JF. Statistical issues in assessing the evidence associating obstetric irradiation and childhood malignancy. In Lengfelder E, Wendhausen H eds, Neue Bewertung des Strahlenriskos : Niedrigdosis Strahlung und Gesundheit, Munich, 1993, 53-60. 31. Blettner M, Zeeb H, Auviven A, et al. Mortality from cancer and other causes among male airline cockpit in Europe. Int J Cancer 2003, 106, 946-52. 32. Boice JD, Preston D, Davis FG, Monson RR. Frequent chest X-ray fluoroscopy and breast cancer incidence among tuberculosis patients in Massachusetts. Radiat Res. 1991; 125: 214-22. 33. Boice JD., Miller R.W. Childhood and adult cancer after intra-uterine exposure to ionising radiation. Teratology, 1999, 59, 227-233. 45 34. Boice JDJ, Engholm G, Kleinerman RA et al. Radiation dose and second cancer risk in patients treated for cancer of the cervix. Radiat Res 1988, 116, 3-55. 35. Boice JDJ, Morin MM, Glass AG et al. Diagnostic x-ray procedures and risk of leukemia, lymphoma, and multiple myeloma JAMA 1991; 265: 1290-4. 36. Bonner WM. Low-dose radiation : Thresholds, bystander effects, and adaptive responses. Proc Natl Acad Sci USA 2003, 100, 4973-5. 37. Boreham DR, JA Dolling, SR Maves, N Siwarungsun, RE Mitchel, Dose-rate effects for apoptosis and micronucleus formation in gamma-irradiated human lymphocytes. Radiat Res, 2000. 153: 579-586. 38. Bouffler SD, Blasco MA, Cox R, Smith PJ. Telomeric sequences, radiation sensitivity and genomic instability. Internat. Journal radiation Biology 2001, 77, 995-1005. 39. Bouffler SD, Haines JW, Edwards AA, Harrison JD, Cox R. Lack of detectable transmissible chromosomal instability after in vivo or in vitro exposure of mouse bone marrow cells to 224Ra alpha particles, Radiation Research 2001, 155, 345-352. 40. Boulton E, Cleary H, Papworth D. Plumb M. Susceptibility to radiation-induced leukaemia/lymphoma is genetically separable from sensitivity to radiation-induced genomic instability. Int. J. Radiat. Biol. 2001, 77, 21-29. 41. Brenner DJ., Little J.B., Sachs RK. The bystander effect in radiation oncogenesis : II. A quantitative model. Radiat Res 2001, 155, 402-408. 42. Brenner DJ, Sachs RK. Do low dose-rate bystander effects influence domestic radon risks ? Int J Radiat Biol 2002 ; 78, 593-604. 43. Brenner DJ., Doll R., Goodhead DT. et al Cancer risk attributable to low doses of ionizing radiation : Assessing what we really know. Proc. Natl. Acad. Sci USA, 2003, 100, 1376113766. 44. Burkart W., Jung T., and Frasch G. Damage pattern as a function of radiation quality and other factors. C. R. Acad. Sci. Paris (Série III, Sciences de la vie) 1999, 322, 89-101. 45. Burns FJ, Albert RE Dose response for radiation induced cancer in rat skin. Pp 5170, in FJ Burns, Upton AC, Silini G eds, Radiation carcinogenesis and DNA alterations. Plenum Press, Life sciences, 1986. 46. Cadet J, D'Ham C, Douki T, Pouget JP, Ravanat JL, Sauvaigo S. Facts and artifacts in the measurement of oxidative base damage to DNA. Free Radic Res. 1998 ;29:541-50. 47. Cai L. Research on the adaptative response induced by low-dose radiation : where have we been and where should we go ? Human Exp. Toxicol. 1999, 18, 419-425. 48. Cairns J. Somatic stem cells and the kinetics of mutagenesis and carcinogenesis. PNAS 2002, 1999, 10567-10570. 49. Calabrese E.J., Baldwyn L.A. Toxicology rethinks its central belief – Hormesis demands a reappraisal of the way risks are assessed. Nature 2003, 421, 691-692. 50. Calabrese EJ. Hormesis: from marginalization to mainstream ; A case for hormesis as the default dose-response model in risk assessment. Toxicol Appl Pharmacol. 2004;197, 125-36. 46 51. Cardis E, Gilbert ES, Carpenter L, et al. Effects of low dose rates of external ionizing radiation : cancer mortality among nuclear industry workers in three countries. Radiat Res 1995, 142, 117-32. 52. Carnes BA., Groer PG., Kotec TJ. Radium dial workers : Issues concerning dose response and modeling. Radiat. Res. 1997, 147, 707-714. 53. Chalmers A, Johnston P, Woodcock M, Joiner M, Marples B. PARP-1, PARP-2, and the cellular response to low doses of ionizing radiation. Int J Radiat Oncol Biol Phys, 2004, 58: 410-419. 54. Chandna S, Dwarakanath BS, Khaitan D, Mathew TL, Jain V. Low-dose radiation hypersensitivity in human tumor cell lines: effects of cell-cell contact and nutritional deprivation. Radiat Res, 2002, 157: 516-525. 55. Chen WC, Luan MC, Shieh ST et al. Is chronic irradiation an effective prophylaxis against cancer ? J Am Phys Surg 2004, 9, 6-10. 56. Christmann M, MT Tomicic, WP Roos, B Kaina, Mechanisms of human DNA repair: an update. Toxicology, 2003. 193: 3-34. 57. Clark W.H. The nature of cancer : morphogenesis and progressive self-disorganization in neoplastic development and progression, Act. Oncologica 1995, 34, 3-21. 58. Coates P.J, Lorimore S.A., Wright E.G. Damaging and protective cell signalling in the untargeted effects of ionizing radiation. Mutation Research 2004, 568, 5-20. 59. Cohen S.M., Ellwein L.B. Cell proliferation in carcinogenesis. Science 1990, 249, 503-504. 60. Collis SJ., Schwaninger JM., Ntambi AJ. et al. Evasion of early cellular response mechanisms following low level radiation induced DNA damage. J. Biol. Chem. 2004, 279, 49624-49632 61. Constantin T., Lartajet R. Mutations différées induites chez une levure par les rayons ultraviolets. Compte-rendus Société de biologie. 1953, 147, 1906-1909. 62. Cornforth MN, Analyzing radiation induced complex chromosome rearrangements by combinatorial painting. Rad. Res. 2001, 155, 643-659 63. Cornforth MN, Bailey SM, Goodwin EH. Dose responses for chromosome aberrations produced in noncycling primary human fibroblasts by alpha particles, and by gamma rays delivered at sublimiting low dose rates. Rad. Research 2002, 158, 43-53. 64. Courtade M, Billote C, Gasset G et al. Life span, cancer and non cancer diseases in mouse exposed to a continuous very low dose of gamma irradiation. Int J Radiat Biol 2002, 78, 845-855. 65. Darby SC, Olsen JH, Doll R et al. Trends in childhood leukaemia in the Nordic countries in relation to fallout from atmospheric nuclear weapons testing Br Med J 1992, 304, 10059. 66. Darby S, Hill D, Auvinen A. et al. Radon in homes and risk of lung cancer : collaborative analysis of individual data from 13 European case-control studies. Brit. Med. J. 2005, 330, 223. 67. Davis FG, Boice JDJ, Hrubec Z, Monson RR. Cancer mortality in a radiation-exposed 47 cohort of Massachusetts tuberculosis patients. Cancer Res. 1989; 49: 6130-6. 68. Delongchamp RR, Mabushi K, Yasuhiko Y et al. Cancer mortality among atomic bomb survivors exposed in utero or as young chidren. Radiat Res 1997, 147, 385395. 69. Dendy PP, Brugmans MJP. Low dose radiation risks. Brit J Radiol 2003; 76:674-677 70. Dent P, A Yacoub, J Contessa, et al. Stress and radiation-induced activation of multiple intracellular signaling pathways. Radiat Res, 2003. 159: 283-300. 71. Derksen PW, Tjin E, Meijer HP, et al. Illegitimate Wnt signaling promotes proliferation of multiple myeloma cells. Proc. Natl. Acad. Sci. USA, 2004, 101, 6122-7. 72. Dickman PW, Holm LE, Lundell GR, Boice JD, Hall P. Thyroid cancer risk after thyroid examination with 131I : a population based cohort study in Sweden. Int J Cancer 2003 ; 106, 580-7. 73. Dikomey E, Brammer I. Relationship between cellular radiosensitivity and non-repaired double-strand breaks studied for different growth states, dose rates and plating conditions in a normal fibroblast line. Int J Radiat Biol 2000, 76, 773-781. 74. Di Majo V, Rebessi S, Pazzaglia S, Saran A, Covelli V. Carcinogenesis after low doses of ionizing radiation. Radiat Res 2003, 159, 102-108. 75. Doll R, Wakeford R. Risk of childhood cancer from fetal irradiation. Br J Radiol 1997 ;70,130-9. 76. Doody MM, Mandel JS, Lubin JH, Boice JD. Mortality among USA radiologic technologists 1926-1990. Cancer Causes Control 1998, 9, 67-75. 77. Doody MM, Lonstein JE, Stovall M, Hacker DG, Luckyanov N, Land CE for the U.S. Scoliosis Cohort Study Collaborators. Breast cancer mortality following diagnostic x rays : Findings from the U.S. Scoliosis Cohort Study. Spine 2000, 25, 2052-2063. 78. Dubertret L, Tubiana M. Soleil et santé. Rapport du groupe de Cancérologie de l’Académie de Médecine. 2004. 79. Duport P. A database of cancer induction by low dose radiation in mammals : overview and initial observations. Int J Low Radiation 2003, 1, 120-131. 80. Edwards AA, Hone PA, Moquet JE, Lloyd DC. Simple chromosome exchanges are not linear with dose. Int. J. Radiat. Biol. 1999, 75, 1113-1117. 81. Esteller M. Epigenetic lesions causing genetic lesions in human cancer, promote hypermethylation of DNA repair genes. Eur J Cancer 2000, 36, 2294-2300. 82. Fei P, WS El-Deiry. P53 and radiation responses. Oncogene, 2003. 22: 5774-5783. 83. Feinendegen LE. The role of adaptive responses following exposure to ionizing radiation. Human and exp. toxicology 1999, 18, 426-432. 84. Feinendegen LE, Pollycove M. Biological responses to low doses of ionizing radiation: detriment versus hormesis. J Nuclear Medicine 2001, 42, 17N-27N. 85. Feinendegen LE. Reactive oxygen species in cell responses to toxic agents. Human & Exp. Toxic. 2002, 21, 85-90. 48 86. Feinendegen LE. Relative implication of protective responses versus damage induction at low dose an low-dose-rate exposures, using the microdose approach. Radiat. Prot. Dosimetry. 2003, 104, 337-346. 87. Feinendegen LE. Evidence for benefical low level radiation effect and hormesis. Brit J Radiology 2005, 78, 3-7. 88. Fernet M. Ponette V., Deniaud-Alexandre E. et al. Poly (ADP-Ribrose) polymerase, a major determinant of early cell response X ionising radiation. Int J Radiat Biol 2000, 76, 73-84. 89. Fouladi B, Sabatier L, Miller D, Pottier G, Murnane JP. The relationship between spontaneous telomere loss and chromosome instability in a human tumor cell line. Neoplasia. 2000, 2, 540-54. 90. Franklyn JA, Maisonneuve L, Sheppard M, Betteridge T, Boyle P. Cancer incidence and mortality after radioiodine treatment for hyperthyroidism: a population based study. Lancet 1999, 353, 2111-2115. 91. Fry SA. Studies of US radium dial workers : An epidemiological classic. Radiat. Res. 1998, 150, S21-29. 92. Fujikawa K, Y Hasegawa, S Matsuzawa, A Fukunaga, T Itoh, S Kondo, Dose and doserate effects of X rays and fission neutrons on lymphocyte apoptosis in p53(+/+) and p53(/-) mice. J Radiat Res (Tokyo), 2000. 41: 113-127. 93. Ghiassi-Nejad M, Mortazavi SMJ, Cameron JR, Niroomand-rad A, Karam PA. Very high background radiation area in Ramsar, Iran : preliminary biological studies. Health Phy 2002, 22, 87-93. 94. Giles RH, Van Es JH, Clevers H. Caught up in a Wnt storm : Wnt signaling in cancer. Biochim. Biophys. Acta. 2003, 1653, 1-24. 95. Grahn D, Lombard LS, Carnes BA ; The comparative tumorigenic effects of fission neutrons and cobalt 60 gamma rays in the B6CF1 mouse. Radiat Res 1992, 129, 1936. 96. Gulston M. Fulford J., Jenner T., De Lara C; O’Neill P. Clustered DNA damage induced by gamma radiation in human fibroblasts (HF19), hamster (V79-4) cells and plasmid DNA is revealed as Fpg and Nth sensitive sites. Nucleic Acids Res. 2002, 30,3646-3672. 97. Gulston M, de Lara C, Jenner T, Davis E, O’Neill P. Processing of clustered DNA damage generates additional double-strand breaks in mammalian cells post-irradiation. Nucleid acids Res. 2004, 32, 1602-1609. 98. Guo M., Hay BA. Cell proliferation and apoptosis. Curr. Op. Cell Biol. 1999, 11, 745752. 99. Hahn K, Schnell-Inderst P, Grosche B, Holm LE. Thyroid cancer after diagnostic administration of iodine-131 in childhood. Radiat Res 2001 ; 156, 61-70. 100. Hahn WC, Weinberg RA. Modeling the molecular circuitry of cancer. Nat. Rev. Cancer 2002, 2, 331-341 101. Hahn WC, Weinberg RA. Rules for making human tumor cells. N. Engl. J. Med. 2002, 347, 1593-1603. 49 102. Harvey EB, Boice JD, Honeyman M, FlanneryJT. Prenatal x-ray exposure and childhood cancer in twins. N Engl J Med 1985; 312:541-545. 103. Heidenreich WF, Brugman MJP, Little MP et al. Analysis of lung tumor risk in radonexposed rats: an intercomparison of multi-step modelling. Radiat Environ Biophys 2000, 39, 253-264. 104. Hendry JH, Potten CA, Chadwick C, Bianchi M. Cell death (apoptosis) in the mouse small intestine after low doses : effects of dose-rate, 14.7 MeV neutrons, and 600 MeV (maximum energy) neutrons. Int. J. Radiat. Biol. 1982, 42, 611-20. 105. Hendry JH, West CML. Apoptosis and mitotic cell death. Their relative contribution to normal tissue and tumour radiation response. Int. J. Radiat. Biol. 1997, 71, 709-719. 106. Hickman J.A. Apoptosis and tumorigenesis. Cur Opin Cell Biol 2002, 12, 67-72. 107. Hoeijmakers JH, Genome maintenance mechanisms for preventing cancer. Nature, 2001. 411: 366-374. 108. Hoel DG, Li P. Threshold models in radiation carcinogenesis. Health Phys 1998, 75, 241-250. 109. Hoffman DA, Bronstein JE, Morin MM. Breast cancer in women with scoliosis exposed to multiple diagnosis X-rays. J Natl Cancer Inst 1989, 81, 1307-1312. 110. Holm LE, Hall P, Wiklund K, et al. Cancer risk after iodine 131 therapy for hyperthyroidism. J Natl Cancer Inst 1991, 83, 1072-7. 111. Hooker AM, Bhat M, Day T.K, et al. The linear No-threshold model does not hold for low-dose ionizing radiation. Radiation Research 2004, 162, 447-452. 112. Hornung R.W. Meinhardt T.J. Quantitative risk assessment of lung cancer in US uranium miners, Health Phys. 1987, 52, 417-30. 113. Howe HL, Johnson TP, Lehnherr M, Warnecke RB, Katterhagen JG, Ford L. Patterns of breast cancer treatment : A comparison of a rural population with an urban population and a Commuity Clinical Oncology Program Sample. Cancer Control. 1995, 2, 113-120. 114. Hrubec Z, Boice JD, Monson RR, Rosenstein M. Breast Cancer after multiple chest fluoroscopies : second follow-up of Massachusetts Women with Tuberculosis. Cancer Research 1989; 49: 229-34. 115. Huels M.A., Boudaiffa B., Cloutier P., Hunting D., Sanche L. Single, double and multiple double strand breaks induced in DNA by 3-100 eV electrons. J. Am. Chem. Soc. 2003, 125, 4467-77. 116. IARC. Monograph on the evaluation of carcinogenic risks to humans. Vol. 75 – Ionizing radiation part I – X and gamma radiation and neutrons. IARC Lyon, France 2000. 117. ICRP Publication 60 : 1990 Recommendations of the International Commission on Radiological Protection. 118. ICRP Draft report of Committee I/Task Group. Low dose extrapolation of radiation related cancer risk. Dec. 10, 2004. 119. Inksip PD, Harvey EB, Boice JD et al. Incidence of cancer in twins. Cancer Cause and Control 1991; 2:315-324. 120. Inskip PD, Ekbom A, Galanti MR, Grimelius L, Boice JDJ. Medical diagnostic x rays 50 and thyroid cancer. J Natl.Cancer Inst. 1995; 87: 1613-21. 121. Ivanov V, Ilyin L, Gorski A, Tukov A, Naumenko R. Radiation and epidemiological analysis for solid cancer incidence among nuclear workers who participated in recovery operations following the accident at the Chernobyl NPP. J. Radiat. Res. (Tokyo), 2004, 45, 41-44. 122. Iyer R, Lehnert BE. Effect of ionizing radiation in targeted and non-targeted cells. Arch Biochem Biophys. 2000, 376, 14-25. 123. Izumi S, Koyama K, Soda M, Suyama A. Cancer incidence in children and young adults did not increase relative to parental exposure to atomic bombs. Br. J. Cancer 2003, 89, 1709-13 124. Jaffe D, Bowden GT. Ionizing radiation as an initiator. Effects of proliferation and promotion time on tumor incidence in mice. Cancer Res. 1987, 47, 6692-6696. 125. Johansson L. Hormesis, an up date of the present position. Eur. J. Nuclear Med. 2003, 30, 921-933. 126. Joiner MC, Marples B, Lambin P, Short SC, Turesson I. Low-dose hypersensitivity: current status and possible mechanisms. Int J Radiat Oncol Biol Phys. 2001, 49, 379-89. 127. Jones P.A., Baylin S.B. The fundamental role of epigenetic events in cancer. Nature Reviews/Genetics 2002, 3, 415-428. 128. Kadhim MA, Marsden SJ, Goodhead DT, Malcolmson AM, Folkard M, Prise KM, Michael BD. Long-term genomic instability in human lymphocytes induced by singleparticle irradiation. Radiat. Res. 2001, 155, 122-126. 129. Kadhim MA.Role of genetic background in induced instability.Oncogene. 2003, 22, 6994-9. 130. Kaiser J. Sipping from a poisoned chalice. Science 2003, 302, 376-379. 131. Kant K, Chauhan RP, Sharma GS, Chakarvarti SK. Hormesis in humans exposed to low-level ionizing radiation. Int. J. Low Radiat. 2003, 1, 76-87. 132. Katayama H, Matsuura M, Endo S, et al. Reassessment of the cancer mortality risk among Hiroshima atomic-bomb survivors using a new dosimetry system, ABS2000D, compared with ABS93D. J Radiat Res 2002, 43, 53-64. 133. Kathren RL. Pathway to a paradigm: the linear non-threshold dose-response model in historical context. Health Phys : 1996, 70, 621-635. 134. Kato F, Dotsumaya A, Nomoto S, Kondo S, Norimura T. Threshold effect for teratogenic risk of radiation depends on dose rate and p53-dependent apoptosis. Int J Radiat Biol 2001, 77, 13-19. 135. Kellerer AM, Rossi HH. The theory of dual radiation action. Cur Top Radiat Res 1972, 8, 85-90. 136. Kennedy A.R., Little J.B. Evidence that a second event in X-ray-induced oncogenic transformation in vitro occurs during cellular proliferation, Radiat. Res. 1984, 99, 228248. 137. Kim PJ, Plescia J, Clevers H, Fearon ER, Altieri DC. Survivin and molecular pathogenesis of colorectal cancer. Lancet 2003, 362, 205-9. 51 138. Khanna KK. Cancer risk and the ATM gene : a continuing debate. J Natl Cancer Inst 2000, 92, 795-802. 139. Klaunig J.E., Kamendulis L.M., Xu Y. Epigenetic mechanisms of chemical carcinogenesis. Hum. Exp. Toxicol. 2000, 19, 543-555. 140. Klokov D., Criswell T., Leskov K.S et al. IR-inducible clusterin gene expression : a protein with potential roles in ionizing radiation-induced adaptive responses, genomic instability, and bystander effects. Mutat. Res. 2004, 568, 97110. 141. Ko SJ, Liao XY, Molloi S et al. Neoplastic transformation in vitro after exposure to low doses of mammographic-energy X Rays : quantitative and mechanistic aspects. Radiat. Res. 2004, 162, 646-654 142. Kojima S, Ishida H, Takahashi M, Yamaoka K. Elevation of glutathione induced by low-dose gamma rays and its involvement in increased natural killer activity. Radiat. Res. 2002, 157, 275-280. 143. Kondo S. Health effects of low level radiation. Osaka-Japan. Madison Wis.: Kinki Univ press (1993). 144. Kondo S. Apoptotic repair of genotoxic tissue damage and the role of p53 gene.Mutat. Res. 1998, 402, 311-9. 145. Kondo S. Tissue misrepair hypothesis for radiation carcinogenesis. J. Radiat. Res (Tokyo) 1991, 32 suppl 2, 1-13. 146. Konogorov AP, Ivanov VK, Chekin SY, Khait SE. A case-control analysis of leukemia in accident emergency workers of Chernobyl. J. Environ. Pathol. Toxicol. Oncol. 2000, 19, 143-151. 147. Kuhne M., Rothkamm K., Lobrich M. Physical and biological parameters affecting DNA double strand break misrejoining in mammalian cells. Radiat. Prot. Dosimety, 2002, 99, 129-132. 148. Lave LB. Hormesis: implications for public policy regarding toxicants. Annu Rev Public Health 2001, 22, 63-67. 149. Liang L, Shao C, Deng L, Mendonca MS, Stambrook PJ, Tischfield JA.Radiation-induced genetic instability in vivo depends on p53 status. Mutat Res 2002, 502, 69-80. 150. Limoli CL, Kaplan MI, Giedzinski E, Morgan WF. Attenuation of radiationinduced genomic instability by free radical scavengers and cellular proliferation. Free Radic Biol Med. 2001, 31, 10-9. 151. Liotta LA., Kohn E.A., The microenvironment of the tumor-host interface Nature 2001 411, 375-379. 152. Little JB, Nagasawa H, Pfenning T, Vetrovs H. Radiation-induced genomic instability : delayed mutagenic and cytogenetic effects of X rays and alpha particles. Rad Res 1997, 148, 299-307. 153. Little JB. Radiation induced genomic instability and bystander effect. Implications for radiation protection. Radioprotection (Paris) 2002, 37, 261-284. 52 154. Little JB. Genomic instability and radiation. J Radiol Prot. 2003, 23, 173-81. 155. Little MP, Muirhead CR. Evidence for curvilinearity in the cancer incidence doseresponse in the Japanese atomic bomb survivors. Int J Radiat Biol 1996, 70, 83-94. 156. Little MP, Muirhead CR. Derivation of low dose extrapolation factors from analysis of the curvature in the cancer incidence dose response in Japanese atomic bomb survivors. Int J Radiat Biol 2000, 76, 939-953. 157. Liu S.Z. On radiation hormesis expressed in the immune system. Crit. Rev. Tox. 2003, 33, 431-441. 158. Lo AW, Sabatier L, Fouladi B et al. DNA amplification by breakage (fusion, bridge, cycle) initiated by spontaneous telomere loss in a human cell line. Neoplasic 2002, 4, 531-538. 159. Lorimore SA, Wright EG. Radiation induced genomic instability and bystander effects : related inflammatory-type responses to radiation-induced stress and injury ? A review. Int. J. radiat. Biol. 2003, 79, 15-25. 160. Loucas BD, Eberle R, Bailey SM, Cornforth MN. Influence of dose rate on the induction of simple and complex chromosome exchanges by gamma rays. Radiat. Res. 2004, 162, 339-349. 161. Lundell M, Mattsson A, Hakulinen T, Holm LE. Breast cancer after radiotherapy for skin hemangioma in infancy. Radiat.Res. 1996, 145, 225-30. 162. MacDonald D, Boulton E, Pocock D, Goodhead D, Kadhim M, Plumb M. Evidence of genetic instability in 3 Gy X-ray-induced mouse leukaemias and 3 Gy X-irradiated haemopoietic stem cells. Int J Radiat Biol. 2001, 77, 1023-31. 163. Maisin JR, Gerber GB, Vankerkom J, Wambersie A. Survival and diseases in C57BL mice exposed to X rays or 3, 1 Mev neutrons at an age of 7 or 21 days. Radiat Res 1996, 146, 453-460. 164. Marples B, Joiner MC. The elimination of low-dose hypersensitivity in Chinese hamster V79-379A cells by pretreatment with X-rays or hydrogen peroxide. Radiat Res, 1995, 141: 160-169. 165. Marples B., Wouters BG., Collis SJ. et al. Low-dose hyper-radiosensitivity : a consequence of ineffective cell cycle arrest of radiation-damaged G2-phase cells. Radiat. Res. 2004, 161, 247-55. 166. McIlrath J., Lorimore S.A., Coates P.J, Wright E.G. Radiation-induced genomic instability in immortalized haemopoietic stem cells. Internation Journal Radiation Biology, 2003, 79, 37-34. 167. Masse R, Cross F. Risk considerations related to lung modeling. Health Phys. 1989, 57, supp 1, 283-289. 168. Mercier G. Berthault N., Mary J. et al, Biological detection of low radiation doses by combining results of two microarray analysis methods. Nucleic Acids Res. 2004, 32, e12 . 169. Mifune M, Sobue T, Arimoto H, Komoto Y, Kondo S, Tanooka H. Cancer mortality survey in a spa area (Misasa, Japan) with a high radon background. Jpn J Cancer Res 53 1992, 83, 1-5. 170. Miller AB, Howe GR, Sherman GJ et al. Mortality from breast cancer after irradiation during fluoroscopic examinations in patients being treated for tuberculosis. N Engl J Med. 1989; 321: 1285-9. 171. Mills KD, Ferguson DO, Alt FW. The role of DNA breaks: genomic instability and tumorigenesis. Immunol. Rev. 2003, 4, 77-95. 172. Mirzaie-Joniani H, D Eriksson, A Sheikholvaezin, A Johansson, PO Lofroth, L Johansson, T Stigbrand, Apoptosis induced by low-dose and low-dose-rate radiation. Cancer, 2002. 94: 1210-1214. 173. Mitchel REJ, Dolling JA, Misonoh J, Bahen ME and Boreham DR. Influence of prior exposure to low dose adapting radiation on radiation-induced teratogenic effects in fetal mice with varying Trp53 function. Radiation Res 2002, 158, 458-463. 174. Mitchel REJ, Jackson JS, Morrison DP and Carlisle SM. Low doses of radiation increase the latency of spontaneous lymphomas and spinal osteosarcomas in cancer-prone, radiation-sensitive Trp53 heterozygous mice. Radiat Res 2003, 159, 320-327. 175. Mitchel REJ, JS Jackson, SM Carlisle, Upper dose thresholds for radiation-induced adaptive response against cancer in high-dose-exposed, cancer-prone, radiation-sensitive Trp53 heterozygous mice. Radiation Res., 2004 ; 162: 20-30. 176. Mitchell CR., Folkard M., Joiner MC. Effects of exposure to low-dose-rate (60)Co gamma rays on human tumor cells in vitro. Radiat. Res. 2002, 158, 311-8. 177. Mitchell JR., Hoeijmakers JH, Niedernhofer LJ. Divide and conquer : nucleotide excision repair battles cancer and ageing. Curr. Opin. Cell. Biol. 2003, 15, 232-40. 178. Mitchell SA, Marino SA, Brenner DJ, Hall EJ. Bystander effect and adaptative response in C3H 10T1/2 cells. Int J Rad Biol 2004, 80, 465-472. 179. M’Kacher R., Bennaceur-Griscelli A, Girinsky T. et al. Detection of DNA repair abnormalities and telomere shortening in circulating lymphocytes : relevance to predict late complications and secondaries malignancies in Hodgkin lymphoma patients. ASCO 2005, abstract (accepted for presentation). 180. Mohan AK, Hauptmann M, Freedman DM, et al. Cancer and other causes of mortality among radiologic technologists in the United States. Int J Cancer 2003, 103, 259-67. 181. Mohan AK, Hauptmann M, Linet MS, et al. Breast cancer mortality among female radiologic technologists in the United States. J Natl Cancer Inst 2002, 94, 943-8. 182. Mole RH. Antenatal irradiation and childhood cancer: causation or coincidence. British Journal of Cancer 1974: 30:199-208. 183. Mole RH, Papworth D, Corp MJ. The dose response for X ray induction of myeloid leukemia in male CBA/H mice. Brit J. Cancer, 1983, 47, 285-291. 184. Monchaux G, Morlier JP, Altmeyer S, Debroche M, and Morin M. Influences of exposure rate on lung cancer induction in rats exposed to radon progeny. Radiat Res 1999, 152, S137-S140. 54 185. Monson RR, MacMahon B. Prenatal X-ray exposure and cancer in children. pp97-105 In Radiation carcinogenesis: Epidemiology and biological significance. JD Boice and JF Fraumeni eds. Raven Press New York 1984. 186. Morin M, Masse R, Lafuma J. Effets cancérogènes de l’irradiation gamma à faible débit de dose. CR Acad Sci Paris 1990, 311, Serie 3, 459-466. 187. Morin M, Allin F, Altmeyer S, Masse R. Relations entre l’irradiation et l’apparition de tumeurs cérébrales chez le rat. C R Acad Sci Paris Sciences de la vie, 1994, 317, 277-281. 188. Mothersill C, Rea D, Wright E.G. et al. Individual variation in the production of a bystander signal following irradiation of primary cultures of normal human urothelium. Carcinogenesis. 2001, 22, 1465-1471. 189. Mothersill C, Seymour C. Possible implications of radiation-induced « bystander effects » for radiation protection. Int J of Low Radiation. 2003, 1, 34-8. 190. Mothersill C., Seymour RJ., Seymour CB. Bystander effects in repair-deficient cell lines. Radiat Res. 2004 ; 161, 256-63. 191. Mothersill C, Seymour CB. Radiation-induced bystander effects implications for cancer. Nat Rev Cancer. 2004 ; 4, 158-64. 192. Moustacchi E. DNA damage and repair: consequences on dose-responses. Mutat Res 2000, 464, 35-40. 193. Nagasawa H, Little JB. Induction of sister-chromatide exchanges by extremely low doses of alpha particles. Cancer Res. 1992, 52, 6394-6. 194. Nair MK, Nambi KS, Amma NS, et al. Population study in the high natural background radiation area in Kerala, India Radiat Res 1999, 152, S145-S148. 195. Nakanishi M, Tanaka K, Shintani T, Takahashi T, Kamada N. Chromosomal instability in acute myelocytic leukemia and myelodysplastic syndrome patients among atomic bomb survivors. J Radiat Res 1999, 40, 159-167. 196. NCRP N° 46 National Council on Radiation Protection and Measurements. Alpha emitting particles in lungs, 1975. 197. NCRP N° 80. Induction of thyroid cancer by ionizing radiation, 1985 198. NCRP N° 104. National Council on Radiation Protection and Measurements. The relative Biological effectiveness of radiations of different quality, 1990, 218p. 198 bis Naumburg E, Belloco R, Cnattingius S, Hall P, Boice J.D, Ekbom A. Intrauterine exposure to diagnostic X rays and risk of childhood leukemia subtypes. Rad. Res. 2001, 156, 718-723. 199. Nikjoo H, Munson RJ, Bridges BA. RBE-LET relationships in mutagenesis by ionizing radiation. J. Radiat. Res (Tokyo) 1999, 40,85-105. 200. Nikjoo H, O’Neill P, Wilson WE, Goodhead DT. Computational approach for determining the spectrum of DNA damage induced by ionizing radiation. Radiat. Res. 2001, 156, 577-583. 55 201. Nikjoo H, Bolton CE, Watanabe R, Terrissol M, O’Neill P, Goodhead DT. Modelling of DNA damage induced by energetic electrons (100 eV to 100 keV). Radiat. Prot. Dosimetry, 2002, 99, 77-80. 202. Noguchi K, Shimizu M, Anzai Z. Correlation between natural radiation exposure and cancer mortality in Japan (I). J Radiat Res 1986, 27, 191-212. 203. Nyberg U, Nilsson B, Travis LB, Holm LE, Hall P. Cancer incidence among Swedish patients exposed to radioactive thorotrast: a forty-year follow-up survey. Radiat Res. 2002, 157, 419-25. 204. OECD. Nuclear Energy Agency Committee on radiation protection and public health: report on developments in radiation health science and technology and their impact on radiation protection. Paris: OECD (1998). 205. Offer H, N Erez, I Zurer, X Tang, M Milyavsky, N Goldfinger, V Rotter, The onset of p53-dependent DNA repair or apoptosis is determined by the level of accumulated damaged DNA. Carcinogenesis, 2002. 23: 1025-1032. 206. Ohyama H, Yamada T. Radiation-induced apoptosis : a review. In : Apoptosis, its roles and mechanisms. (eds) Yamada T, Hasimoto Y. Business Center for Academic Societies Japan, Tokyo, 1998, pp 141-186. 207. Okayasu R, Suetomi K, Yu Y et al. A deficiency in DNA repair and DNA-PKcs expression in the radiosensitive BALB/c mouse. Cancer Res. 2000, 60, 4342-4345. 208. Oppenheim BE., Griem ML., Meier P. The effects of diagnostic X-ray exposure on the human fetus : an examination of the evidence. Radiology. 1975, 114, 529-34. 209. Pant GS, Kamada N. Chromosome aberrations in normal leukocytes induced by the plasma of exposed individuals. Hiroshima J Med Sci. 1977, 26, 149-154. 210. Pardoll D. T cells and Tumors. Nature 2001, 411, 1010-1012. 211. Parkin DM, Clayton D, Black RJ et al. Childhood leukaemia in Europe after Chernobyl: 5 year follow-up. Br J Cancer 1996, 73, 1006-12. 212. Pelengaris S., Khan M., Evan G. C-myc : More than just a matter of life and death. Nature Review Cancer 2002, 2, 754-776. 213. Pierce DA, Preston DL. Radiation-related risk at low doses among atomic bomb survivors. Radiat Res 2000, 154, 178-186. 214. Pierce DA. Mechanistic models for radiation carcinogenesis and the atomic bomb survivor data. Radiation Res 2003, 160, 718-723. 215. Petrini JH, Stracker TH. The cellular response to DNA double-strand breaks : defining the sensors and mediators. Trends Cell Biol. 2003, 13, 458-462. 216. Pollycove M, Feinendegen LE. Radiation-induced versus endogenous DNA damage : possible effects of inducible protective responses in mitigating endogenous damage. Human Exp Toxicol 2003, 22, 290-306. 217. Poncy JL, Fritsch P, Masse R. Evoluation of sister-chromatid exchanges (SCE) in rat bone marrow cells as a funtion of time after 2 Gy of whole-Body neutron irradiation. Mutat. Res. 1988, 202,45-49. 56 218. Ponette V., Le Pechoux C., Deniaud-Alexandre E. et al. Hyperfast early cell response to ionising radiation. Int. J. Rad. Biol. 2000, 72, 1233-1243. 219. Ponnaiya B, Cornforth MN, Ullrich RL. Radiation-induced chromosomal instability in BALB/c and C57BL/6 mice : the difference is as clear as black and white. Radiat. Res. 1997, 147, 121-125. 220. Ponnaiya B, Limoli CL, Corcoran J, Kaplan MI, Hartmann A, Morgan WF. The evolution of chromosomal instability in Chinese hamster cells : a changing picture ? Int. J. Radiat. Biol. 1998, 74, 765-770. 221. Potten CS, Owen G, Booth D. Intestinal stem cells protect their genome by selective segregation of template DNA strands. J. Cell. Science 2002, 114, 2381-8. 222. Preston DL, Mattsson A, Holmberg E, Shore R, Hildreth NG, Boice JD. Radiation effects on breast cancer risk : a pooled analysis of eight cohorts. Radiat. Res. 2002, 158, 220-35. 223. Preston DL, Shimizu Y, Pierce DA, Suyama A, Mabuchi K. Studies of mortality of atomic bomb survivors. Report 13: solid cancer and noncancer disease mortality: 1950-1997. Radiat Res 2003 ; 160, 381-407. 224. Preston DL, Pierce DA, Shimizu Y et al. Effect of recent changes in atomic bomb survivor dosimetry on cancer mortality risk estimates. Radiation Research 2004, 162, 377-389. 225. Preston RJ. Developing mechanistic data for incorporation into cancer and genetic risk assessment. Health Phys. 2003, 85, 4-12. 226. Preston RJ. The LNT model is the best we can do-today. J. Radiol Prot. 2003, 23, 263-268. 227. Preston RJ. Radiation biology: concepts for radiation protection. Health Phys 2004, 87, 3-14. 228. Preston-Martin S, Thomas DC, Yu MC, Henderson BE. Diagnostic radiography as a risk factor for chronic myeloid and monocytic leukaemia (CML). Br J Cancer 1989; 59: 634-44. 229. Raabe O.G., Comparison of the carcinogenicity of radium and boneseeking actinides, Health Phys 1984, 46, 1241-1248. 230. Raabe OG, Rosenblatt LS, Schlenker RA. Interspecies scaling of risk for radiation-induced bone cancer.Int J Radiat Biol 1990 ;57:1047-1061. 231. Radisky DC, Bissell MJ. Cancer. Respect thy neighbor ! Science, 2004, 6, 303, 775-774. 232. Ravanat JL, Douki T, Duez P, et al. Cellular background level of 9-oxo-7,8dihydro-2'-deoxyguanosine: an isotope based method to evaluate artefactual oxidation of DNA during its extraction and subsequent work-up. Carcinogenesis 2002, 23: 1911-1918. 233. Redpath JL, Antoniono RJ. Induction of an adaptive response against spontaneous neoplastic transformation in vitro by low dose gamma radiation. Radiat. Res. 1998, 149, 517-520. 57 234. Redpath JL, Short SC, Woodcock M, Johnston PJ. Low-dose reduction in transformation frequency compared to unirradiated controls: the role of hyperradiosensitivity to cell death. Radiat Res. 2003 159:433-6. 235. Redpath JL, Lu Q, Lao X, Molloi S, Elmore E. Low dose of diagnostic energy Xrays protect against neoplastic transformation in vitro. Int. J. Radiat. Biol. 2003, 79, 235-240. 236. Redpath JL. Radiation induced neoplastic transformation in vitro : evident for a protective effect at low doses of low LET. Radiation Cancer Metastasis Rev. 2004, 23, 333-339. 237. Reliene R, Schiestl RH. Mouse models for induced genetic instability at endogenous loci. Oncogene 2003, 22, 7000-7010. 238. Rico A. Chemo-defence systems. CR Acad Sc (Sciences de la vie) Paris 2001 324, 97-106. 239. Rodvall Y, Hrubec Z, Pershagen G et al. Childhood cancer among Swedish twins. Cancer Causes and Control 1992; 3:527-532. 240. Rothkamm K., Kuhne M., Jeggo P.A. & Lobrich M. Radiation-induced genomic rearrangements formed by nonhomologous end-joining of DNA doublestrand breaks. Cancer Res. 2001, 61, 3886-93. 241. Rothkamm K, Löbrich M. Evidence for a lack of DNA double-strand break repair in human cells exposed to very low x-ray doses. Proc Natl Acad Sci U S A. 2003, 100, 5057-62. 242. Rowland R.E., Stehney A.F., Lucas H.F., Dose-reponse relationships for radium-induced bone sarcomas, Health Phys 1983, 44 suppl. 1, 15-31. 243. Rubino C, de Vathaire F, Shamsaldin A, Labbe M, Le MG. Radiation dose, chemotherapy, hormonal treatment and risk of second cancer after breast cancer treatment. Br J Cancer 2003 ; 89, 840-6. 244. Sakai K. et al. Suppression of mouse tumour induction by chronic low dose-rate gamma-irradiation. J. Radiat. Res. 2000, 41, 467. 245. Sanders CL, McDonald KE, Mahaffey JA. Lung tumor response to inhaled Pu and its implications for radiation protection. Health Phys. 1988;55:455-62. 246. Sasaki MS, Ejima Y, Tachibana A, Yamada T, Ishizaki K, Shimizy T. Nomura T. DNA damage response pathway in radioadaptive response. Mutat. Res. 2002, 504, 101-118. 247. Sawant S.G., Randers-Pehrson G., Geard C.R et al. The bystander effect in radiation oncogenesis : I. Transformation in C3H 1OT1/2 cells in vitro can be intiated in the unirradiated neighbors of irradiated cells. Radiat Res 2001, 155, 397-401. 248. Schmitz A, Bayer A, Dechamps N, Thomas G. Intrinsic susceptibility to radiation-induced apoptosis of human lymphocyte subpopultions. Int. J. radiat. Oncol. Biol. Phys. 2003, 57, 769-728. 249. Scott D. The effect of irradiated plasma on normal human chromosomes and 58 its relevance to the long-lived lymphocyte hypothesis. Cell Tissue Kinet 1969, 2, 295-305. 250. Shilnikova NS, Preston DL, Ron E, et al. Cancer mortality risk among workers at the Mayak nuclear complex. Radiat Res 2003, 159, 787-98. 251. Shiloh Y. ATM and related protein kinases : safeguarding genome integrity. Nat. Rev. Cancer 2003, 3, 155-68. 252. Shore RE. Radiation-induced skin cancer in humans. Med. Pediatr. Oncol. 2001, 36, 549-54. 253. Short SC, Kelly J, Mayes CR, Woodcock M, Joiner MC. Low-dose hypersensitivity after fractionated low-dose irradiation in vitro. Int. J. Radiat. Biol. 2001, 77, 655-664. 254. Sigurdson AJ, Doody MM, Rao RS, et al. Cancer incidence in the US radiologic technologists health study, 1983-1998 Cancer 2003, 97, 3080-9. 255. Smith LE, Nagar S, Kim GJ, Morgan WF. Radiation-induced genomic instability: radiation quality and dose response. Health Phys 2003, 85, 23-9. 256. Sobue T, VS Lee, W Ye, H Tanooka, M Mifune, A Suyama, T Koga, H Morishima, S Kondo, Residential radon exposure and lung cancer risk in Misasa, Japan: a case-control study. J Radiat Res (Tokyo), 2000. 41: 81-92. 257. Stebbings JH, Lucas HF, Stehney AF. Mortality from cancers of major sites in female radium dial workers. Am. J. Ind. Med. 1984, 5, 435-459. 258. Spengler RF, Cook DH, Clarke EA, Olley PM, Newman AM. Cancer mortality following cardiac catheterization: a preliminary follow-up study on 4,891 irradiated children. Pediatrics 1983; 71: 235-9. 259. Stevens W, Thomas DC, Lyon JL et al. Leukemia in Utah and radioactive fallout from the Nevada test site. A case-control study. JAMA 1992, 264, 585-91. 260. Stewart AM., Kneale GW. A-bomb survivors : factors that may lead to a reassessment of the radiation hazard. Int. J. Epidemiol. 2000, 29, 708-14. 261. Streffer C, Bolt H, Follesdal D. et al. Low Dose Exposures in the Environment, DoseEffect Relations and Risk Evaluation. Reihe : Wissenschaftsethik und Technikfolgenbeurteilung, Band 23, 2004, Springer 470 pages. 262. Sugahara T., Watanabe M. Epigenetic nature of radiation cancinogenesis at low doses. Int. J. Occup. Med. Toxicol. 1994, 3, 129-136. 263. Tanooka H. Threshold dose-response in radiation carcinogenesis : an approach from chronic beta-irradiation experiments and a review of non tumour doses ; Int J Radiat Biol 2001, 77, 541-551. 264. Tao Z, Zha Y, Akiba S, Sun Q, et al. Cancer mortality in the high background radiation areas of Yangjiang, China during the period between 1979 and 1995. J Radiat Res (Tokyo) 2000 ; 41, 31-41. 265. Thierens H, Vral A, Barbe M, Meijlaers M, Baeyens A, and Ridder LD. Chromosomal radiosensitivity study of temporary nuclear workers and the support of the adaptive response induced by occupational exposure. Int. J. Radiat. Biol. 2002, 78, 1117-1126. 59 266. Thomas RG. Tumorigenesis in the US radium luminizers: how unsafe was this occupation? p. 145-148 in: Health Effects of Internally Deposited Radionuclides: Emphasis on Radium and Thorium (G. van Kaick, A. Karaoglou, A.M. Kellerer, eds.). World Scientific, London, Singapore, 1995. 267. Tiku AB, Kale RK. Adaptative response and split dose effect of radiation on the survival of mice. J. Biosci. 2004, 29, 111-117. 268. Tonomura A., Cytogenetic studies in Japanese populations. Report of a research group for biological effects of low-dose radiation for fiscal year 1980 (Chairman : T. Sugahara), Nuclear Safety Research Association, 1980. 269. Totter JR., MacPherson HG. Do childhood cancers result from prenatal x-rays ? Health Phys. 1981, 40, 511-24. 270. Travis LB, Land CE, Andersson M, Nyberg U et al. Mortality after cerebral angiography with or without radioactive Thorotrast: an international cohort of 3, 143 twoyear survivors. Radiat Res. 2001 ; 156, 136-50. 271. Travis L.B., Hauptmann M., Gaul LK et al. Site-specific cancer incidence and mortality after cerebral angiography with radioactive thorotrast. Radiat. Res. 2003, 160, 691-706. 272. Trott K, Roseman M. Molecular mechanism of radiation carcinogenesis and the linear non-threshold dose response model of radiation risk estimation. Radiat. Environ. Biophys. 2000, 39, 79-87.. 273. Tubiana M. The carcinogenic effect of low doses : the validity of the linear nothreshold relationship. Int J Low Radiation, 2003, 1, 1-31. 274. Tubiana M., Aurengo A., Masse R., Valleron AJ. Risk of cancer from diagnostic X rays. Lancet 2004, 363, 1908. 275. Ullrich RL, Storer JB, Influence of gamma irradiation on the developpment of neoplastic disease in mice. Part 1, 2,3, Radiat Res 1979, 80, 303-342. 276. Ullrich RL Tumor induction in BalbC mice after fission neutrons or gamma irradiation, Radiat Res 1983, 93, 506-515. 277. Ullrich RL, Jernigan MC, Satterfield LC, Bowles ND. Radiation carcinogenesis : time-dose relationships. Radiat. Res. 1987, 111, 179-84. 278. Ullrich RL, Bowles ND, Satterfield LD, Davis CM. Strain dependent susceptibility to radiation induced mammary cancer is a result of differences in epithelial sensitivity to transformation. Radiat Res 1996, 146, 353-355. 279. Ullrich RL, Ponnaiya B. Radiation-induced instability and its relation to radiation carcinogenesis. Int. J. Radiat. Bio. 1998, 74, 747-754. 280. Uma Devi P, Hossain M. Induction of solid tumours in the swiss albino mouse by lowdose fœtal irradiation. Int J Radiat Biol 2000, 76, 95-99. 281. UNSCEAR : United Nations Scientific Committee on the Effects of Atomic Radiation. Sources, effects and risks of ionising radiation. Report to the General Assembly, with Annexes. United Nations, E 94 IX 11 New York 1993. 282. UNSCEAR : United Nations Scientific Committee on the Effects of Atomic Radiation. Sources, effects and risks of ionising radiation. Report to the General Assembly, with Annexes. United Nations, E 94 IX 11 New York 1994. 60 283. UNSCEAR : United Nations Scientific Committee on the Effects of Atomic Radiation. Sources, effects and risks of ionising radiation. Report to the General Assembly, with Annexes. United Nations, New York 2000. 284. Upton AC, Randolph ML, Conklin JW, Kastenbaum MA, Slater M, Melville GS Jr, Conte FP, Sproul JA Jr. Late effects of fast neutrons and gamma-rays in mice as influenced by the dose rate of irradiation : induction of neoplasia. Radiat. Res. 1970, 41, 467-491. 285. Upton AC. The linear-non threshold dose-response model: a critical reappraisal. In: Radiation Protection in Medicine: Contemporary Issues. NCR Proceedings 1999, 21, 9-31. 286. Upton AC Radiation hormesis : data and interpretation. Crit Rev Toxicol 2001, 31 , 691-695. 287. Van Kaick G., Wesh H., Luhrs H., Lieberman D., Kaul A., Neoplastic diseases induced by chronic alpha irradiation. Epidemiological, biophysical and clinical results by the German Thorotrast Study Group, J Radiat Res 1991, 32, suppl. 2, 2033. 288. Vathaire F de, Hardiman C, Shamsalidin A., et al. Thyroid carcinoma following irradiation for a first cancer during childhood. Arch Inter Med 2000, 159, 2713-2719. 289. Vilenchik MM., Knudson A.G.. Inverse radiation dose-rate effects on somatic and germ-line mutations and DNA damage rates. Proc Natl Acad Sci U S A. 2000, 97, 5381-6. 290. Vilenchik MM ; Knudson A.G. Endogenous DNA double-strand breaks : production, fidelity of repair, and induction of cancer. Proc. Natl. Acad. Sci. USA. 2003, 100, 12871-6 291. Walsh L., Rhum W., Kellerer A.M. Cancer risk estimates for gamma-rays with regard to organ-specific doses. I all solid cancer combined. Radiat. Environ. Biophysics 2004. 43, 145-51. 292. Wang JX, Zhang LA, Li BX, et al. Cancer incidence and risk estimation among medical x-ray workers in China 1950-1995. Health Phys 2002, 82, 455-66. 293. Wang Z.Y., Boice J.D., Wein L.X. Thyroid nodularity and chromosome aberration among women in areas of high background radiation in China, J. Natl. Cancer Inst. 1990, 82, 478-485. 294. Wei L, T Sugahara, An introductory overview of the epidemiological study on the population at the high background radiation areas in Yangjiang, China. J Radiat Res (Tokyo), 2000. 41 Suppl: 1-7. 295. Whittemore A.S. Quantitative risk assessment p.116-126 in Cancer epidemiology and prevention (D. Schottenfeld, J.F. Fraumeni Edit.) Oxfort Univ. Press 1996. 296. Wolf C, Lafuma J, Masse R, Morin M, Kellerer AM Neutron RBE for induction of tumors with high lethality in Sprague-Dawley rats. Radiat Res. 2000 ;154:41220. 61 297. Wolff S. The adaptive response in radiobiology: evolving insights and implications. Environ Health Perspect 1998;.106: 277-283 298. Wood RD, Mitchell M, Sgouros J. and Lindahl T. Human DNA repair genes. Science 2001, 10, 1284-1289. 299. Xie L, Law BK, Aakre ME, et al. Transforming growth factor beta-regulated gene expression in a mouse mammary gland epithelial cell line. Breast Cancer Res. 2003, 5, R187-98. 300. Yamamoto O, Seyama T, Itoh H, Fujimoto N. Oral administration of tritiated water (HTO) in mouse. Low dose rate irradiation and threshold dose-rate for radiation risk. Int J Radiat Biol 1998, 73, 535-541. 301. Yang C.R., Leskov K., Hosley-Eberlein K, et al. Nuclear clusterin, an X-ray induced Ku 70 – protein that signals cell death. Proc. Natl. Acad. Sc. USA 2000, 97, 5907-5912. 302. Yang J., Y. Yu, H.E. Hamrick, and P. J.Duerksen-Hughes. ATM, ATR and DNA-PK: initiators of the cellular genotoxic stress responses. Carcinogenesis 2003, 24, 1571-1580. 303. Ye N, MS Bianchi, NO Bianchi, GP Holmquist, Adaptive enhancement and kinetics of nucleotide excision repair in humans. Mutat Res, 1999. 435: 43-61. 304. Yu Y, Okayasu R, Weil MM, et al. Elevated breast cancer risk in irradiated BALB/c mice associates with unique functional polymorphisms of the Prkde gene. Cancer Research 2001, 61, 1820-1824. 305. Yukawa O, Nakajima T, Yukawa M, Ozawa T, Yamada T. Induction of radical scavenging ability and protection against radiation-induced damage to microsomal membranes following low-dose irradiation. Int J Radiat Biol, 1999, 75: 1189-1199 306. Zeeb H, Blettner M, Langner I, et al. Mortality from cancer and other causes among airline cabin attentants in Europe : a collaborative study in eight countries. Am J Epidemiol 2003; 158:35-46. 62