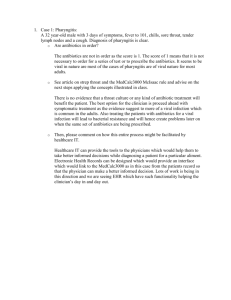
Clinical aspects of Pharyngitis

Clinical aspects of Pharyngitis
Signs and symptoms
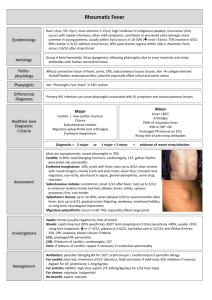
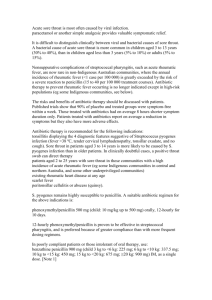
Pharyngitis is related to the inflammation of the mucous membrane that lies at the back of the throat and then it becomes sore, when the throat is inflamed. This type of infection is most common in children and young adults and is caused by a many viral infection. GAS Pharyngitis is often associated with children and young adults. Nearly all acute pharyngitis is caused by viruses where GAS is the significant cause of bacterial cause. GAS pharyngitis is common in ages from 5 – 15 and occurs in climate changes during the winter and spring periods. (Micheal A. Gerber. 2005)
The clinical signs and symptoms shows clear relation to pharyngitis but evidence is required to support the data, that this patient is suffering from GAS pharyngitis although symptoms are closely associated to GAS pharyngitis but it could also refer to upper respiratory tract infection. The symptoms that this patient possessed was sore throat that is common with young children who have GAS pharyngitis. In addition the patient had fever of 38ºC which is triggered by pharyngitis as well as swollen glands upon physical examination. (Michael A. Gerber, Robert S. Baltimore, Charles B.
Eaton, Michael Gewitz, Anne H.Rowley, Stanford T. Shulman and Kathryn A.
Taubert. 2009). The patient had other common symptoms such as headache nausea but important sign was the yellow exudates on his tonsils and multiple, enlarged cervical lymph nodes. There is extremely strong evidence suggesting that the patient has GAS pharyngitis and is often common in children with identical signs and symptoms. Test should be carried out to verify if the patient has pharyngitis and the type of pharyngitis it could be, if proven positive. (Stanford T. Shulman. 2003,
Micheal A. Gerber. 2005)
Table 1
Features suggestive of GAS as causative agent
Sudden-onset sore throat
Pain on swallowing
Fever
Scarlet fever rash
Headache
Nausea, vomiting, and abdominal pain
Tonsillopharyngeal erythema
Tonsillopharyngeal exudates
Soft palate petechiae (“doughnut” lesions)
Beefy, red, swollen uvula
Tender, enlarged anterior cervical nodes
Patient 5 to 15 years of age
Presentation in winter or early spring (in temperate climates)
History of exposure
Features suggestive of viral origin
Conjunctivitis
Coryza
Hoarseness
Cough
Diarrhea
Characteristic exanthems
Characteristic enanthems
Adapted from Michael A. Gerber, Robert S. Baltimore, Charles B. Eaton, Michael
Gewitz, Anne H. Rowley, Stanford T. Shulman and Kathryn A. Taubert. 2009.
Circulation Prevention of Rheumatic Fever and Diagnosis and Treatment of Acute of
Streptococcal Pharyngitis: A Scientific Statement From the American Heart
Association Rheumatic Fever, Endocarditis, and Kawasaki Disease Committee of the
Council on Cardiovascular Disease in the Young, the Interdisciplinary Council on
Functional Genomics and Translational Biology, and the Interdisciplinary Council on
Quality of Care and Outcomes Research. J of American heart association 119:1541-
1551
Diagnosis
Test that will be required to carry out due to the swelling of the pharynx and fever symptoms is the Rapid strep test and Throat culture, bacitracin disk or PYR test.
Rapid strep / rapid antigen detection test (RADT) is performed, whereby this test identifies specific carbohydrates on the cell wall of GAS. This test generate high-level of specificity and can indicate negative or positive for GAS pharyngitis. Despite the fact that RADT may provide a false positive result throat culture is required to be taken to support the result as often in many RADT can be incorrect. (Roberta B Carey,
2008)
Throat culture can only take place if GAS pharyngitis is present; the GAS sample is taken from the patient’s throat using a throat swab. To attain adequate specimen a double swab should be used to carry out the test this is to gain quality results from the test carried. The sample will need to be kept overnight in incubation, this develop the growth of GAS pharyngitis and should prove positive this determines that the patient has GAS pharyngitis. To make sure that you have accurate results a double swab should be used on both tonsils and pharyngeal area so you gain adequate sample and accurate testing can be performed to gain high quality results. The throat culture should be plated on a blood sheep agar, in addition to distinguish the type of GAS pharyngitis or other β-haemolytic streptococci by using a bacitracin disk. The bacitracin test only requires 1 day of incubation to be carried out. It is crucial that no contact with other areas of the mouth and throat should occur to avoid contamination and accuracy of that specific specimen. If throat culture is proving to be positive continuously this may mean that the chronic colonization is GAS and another viral maybe the cause. If RADT provides negative result for accuracy the test may need to be performed again as well as a throat culture to be carried out, newer tests have been made so that it is more sensitive than RADT’s and more efficient and sensitive in comparison to the blood agar plates. (Roberta B Carey, 2008)
PYR test is used as alternative method and used in clinical laboratories this test provides instant result it helps to detect a specific enzyme known as Lpyroglutamylaminopeptidaseit only takes a few minutes and only using a single βhaemolytic colony, if the test is proven positive it means GAS pharyngitis. (Micheal
A. Gerber. 2005)
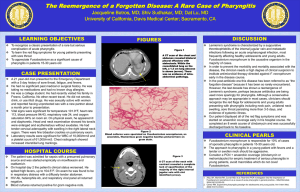
CT scans can assist to diagnose the disease if there is visual complication of pharyngitis such as swelling (abscesses) or sinusitis (inflammation of membrane lining). (Micheal A. Gerber. 2005)
The common sort of testing used is the RADT, however if there is any negative results present a throat culture is required to support the result and if the findings differ it maybe likely that the result might have to retested. The advantages and disadvantage is that most RADT findings are accurate but expensive, whilst with throat culture contamination is likely to affect the result but is less time consuming.
(Stanford T. Shulman. 2003)
References
Roberta B Carey, 2008. Boy with Acute Pharyngitis. Medical Microbiology for the new curriculum: A case based approach, Pg 1-11
Micheal A. Gerber. 2005. Diagnosis and Treatment of Pharyngitis in children.
Paediatrics clinics North America 52:729-747
Michael A. Gerber, Robert S. Baltimore, Charles B. Eaton, Michael Gewitz, Anne H.
Rowley, Stanford T. Shulman and Kathryn A. Taubert. 2009. Circulation Prevention of Rheumatic Fever and Diagnosis and Treatment of Acute of Streptococcal
Pharyngitis: A Scientific Statement From the American Heart Association Rheumatic
Fever, Endocarditis, and Kawasaki Disease Committee of the Council on
Cardiovascular Disease in the Young, the Interdisciplinary Council on Functional
Genomics and Translational Biology, and the Interdisciplinary Council on Quality of
Care and Outcomes Research. J of American heart association 119:1541-1551
Stanford T. Shulman. 2003. Acute Streptococcal Pharyngitis in Paediatric medicine,
Current issue in diagnosis and treatment. Paediatric Drugs 1:13-23