Acute sore throat is most often caused by viral infection
advertisement
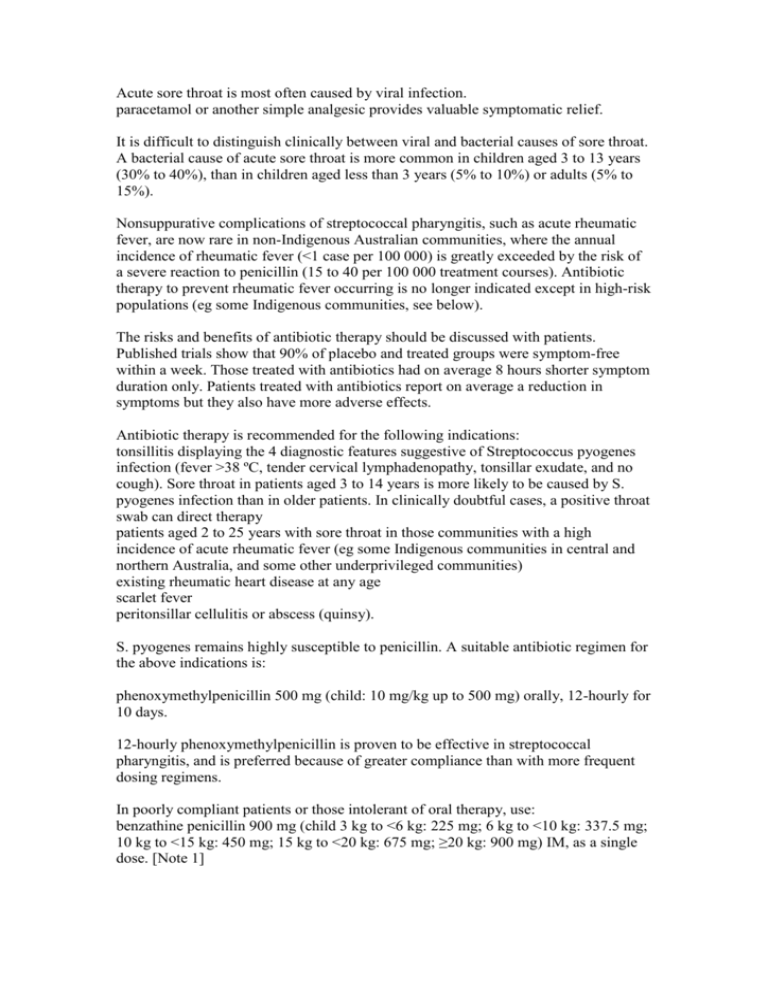
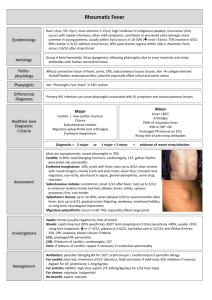
Acute sore throat is most often caused by viral infection. paracetamol or another simple analgesic provides valuable symptomatic relief. It is difficult to distinguish clinically between viral and bacterial causes of sore throat. A bacterial cause of acute sore throat is more common in children aged 3 to 13 years (30% to 40%), than in children aged less than 3 years (5% to 10%) or adults (5% to 15%). Nonsuppurative complications of streptococcal pharyngitis, such as acute rheumatic fever, are now rare in non-Indigenous Australian communities, where the annual incidence of rheumatic fever (<1 case per 100 000) is greatly exceeded by the risk of a severe reaction to penicillin (15 to 40 per 100 000 treatment courses). Antibiotic therapy to prevent rheumatic fever occurring is no longer indicated except in high-risk populations (eg some Indigenous communities, see below). The risks and benefits of antibiotic therapy should be discussed with patients. Published trials show that 90% of placebo and treated groups were symptom-free within a week. Those treated with antibiotics had on average 8 hours shorter symptom duration only. Patients treated with antibiotics report on average a reduction in symptoms but they also have more adverse effects. Antibiotic therapy is recommended for the following indications: tonsillitis displaying the 4 diagnostic features suggestive of Streptococcus pyogenes infection (fever >38 ºC, tender cervical lymphadenopathy, tonsillar exudate, and no cough). Sore throat in patients aged 3 to 14 years is more likely to be caused by S. pyogenes infection than in older patients. In clinically doubtful cases, a positive throat swab can direct therapy patients aged 2 to 25 years with sore throat in those communities with a high incidence of acute rheumatic fever (eg some Indigenous communities in central and northern Australia, and some other underprivileged communities) existing rheumatic heart disease at any age scarlet fever peritonsillar cellulitis or abscess (quinsy). S. pyogenes remains highly susceptible to penicillin. A suitable antibiotic regimen for the above indications is: phenoxymethylpenicillin 500 mg (child: 10 mg/kg up to 500 mg) orally, 12-hourly for 10 days. 12-hourly phenoxymethylpenicillin is proven to be effective in streptococcal pharyngitis, and is preferred because of greater compliance than with more frequent dosing regimens. In poorly compliant patients or those intolerant of oral therapy, use: benzathine penicillin 900 mg (child 3 kg to <6 kg: 225 mg; 6 kg to <10 kg: 337.5 mg; 10 kg to <15 kg: 450 mg; 15 kg to <20 kg: 675 mg; ≥20 kg: 900 mg) IM, as a single dose. [Note 1] For patients hypersensitive to penicillin, use: roxithromycin 300 mg orally, daily (child: 4 mg/kg up to 150 mg orally, 12-hourly) for 10 days. Quinsy usually requires aspiration or drainage in hospital, in addition to parenteral penicillin as for aspiration pneumonia (see Aspiration pneumonia). It is usual to broaden cover by adding metronidazole to penicillin or by substituting clindamycin for penicillin. Diphtheria (Corynebacterium diphtheriae) is very rare in Australia but may occur in recent overseas travellers or their contacts. It presents as gross membranous pharyngitis, with or without airway obstruction, associated with obvious systemic toxicity. Epstein-Barr virus infection should be excluded as it is a much more common cause of this set of symptoms. The mainstay of treatment is diptheria antitoxin. Its use can be associated with acute allergic reactions, and hence it is best given in a hospital setting under expert guidance—see the Australian Immunisation Handbook. Parenteral penicillin is frequently used as adjunctive therapy. Contacts of proven cases should be given oral penicillin or erythromycin. Other infections that may cause exudative pharyngitis include glandular fever and gonococcal infection. Vesicular or ulcerative eruptions may occur with infection due to some types of enterovirus and herpes simplex virus types 1 and 2. Also consider the possibility of secondary syphilis. Note 1: benzathine penicillin 900 mg = 1.2 million units