A Simple and Rapid Approach to Hypokalemic Paralysis in
advertisement

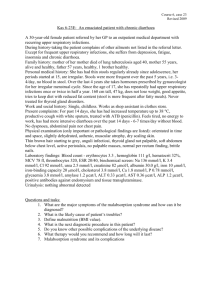
A Simple and Rapid Approach to Hypokalemic Paralysis in Emergency Department -Three Cases Report 急診之簡單和快速評估低血鉀麻痺症-三病例報告 許金旺 1 林石化 2 陳建生 1 朱士傑 1 劉敏英 1 三軍總醫院急診部 1 三軍總醫院內科部腎臟科 2 Introduction Acute muscle weakness with severe hypokalemia is not unusually encountered in the emergency department. The first step is to clarify two different etiologies. The one is hypokalemic periodic paralysis(HPP), which is due to an acute shift of K+ into cells without total body K+ deficit. The other is non-HPP, primarily due to excessive excretion of K+. Failure to clarify these two different etiologies may give to improper management. The therapy of HPP requires only small doses of potassium replacement to avoid rebound hyperkalemia. As the clinical presentations between them are almost similar, the use of spot urine for K+ excretion rate and evaluation of blood acid-base status may be clinically beneficial in the diagnosis and management. Case reports Case 1: Hypokalemia, weakness, and a normal acid-base state A 32-year-old male presented with sudden onset of general muscular weakness of all extremities and inability to ambulate upon awakening. No significant findings were found on his medical and family history. On physical examination, his blood pressure was high(168/84 mmHg), as was his heart rate(128 beats/min). The principal findings were diffusely enlarged thyroid gland and total paralysis of all extremities. Biochemical studies are shown in table 1. He did not have an acid-base + disorder and K excretion was low and transtubular potassium gradient(TTKG) of 1.9. He was treated with intravenous KCL at a rate of 10 mmol/hr. However, hyperkalemia 6.2 mmol/L was observed two hours after recovery.His T3 and T4 levels were elevated while TSH was suppressed. His hyperthyroidism was treated with oral propylthiouracil and propranolol. His thyrotoxic periodic paralysis did not recur and he has remained clinically euthyroid through the following half an year follow up. Case 2: Hypokalemia, weakness , and metabolic acidosis A 29-year-old female was brought to the emergency room because of an inability to ambulate for several hours. She noticed mild weakness of her lower extremities for one week. She denied anorexia, nausea, vomiting, or diarrhea. There were no significant findings on physical examination except total paralysis of her lower extremities with absent reflexes.The biochemical studies are shown in Table 1. Although her Uk was low, the spot urine UK/UCr of 2.8 was higher than expected, suggesting renal K+ wasting. She had metabolic acidosis(pH 7.27) and a normal plasma anion gap. A diagnosis of RTA was established. Aggressive replacement therapy with KCL(mmol/hr) was given to treat her HP. Immunologic surveys revealed elevated rheumatoid factor, positive anti-Ro and La antibodies, and positive Schimer”s test for dry eyes.She proved to have Sjogren syndrome. She was placed on oral potassium citrate, active vitamin D3 and steroid therapy. Case 3: Hypokalemia,weakness, and metabolic alkalosis A 20-year-old male presented to emergency department with muscular weakness that progressed to paralysis involving all extremities; he was unable to walk for hours. He denied nausea, vomiting, diarrhea, or use of diuretics. There were no significant findings on physical examination except a symmetric flaccid paralysis with areflexia in the upper and lower extremities. Hypokalemia was the most striking biochemical abnormality(1.8 mmol/L); it was accompanied by metabolic alkalosis(Table 1). Urinary excretion of K+ was considering his hypokalemia(Uk 11mmol/L, UK/UCr 2.8). A Bartter”s-like syndrome was tentatively diagnosed. Aggressive replacement therapy with KCL(20 mmol/hr) was initiated to treat his HP. Intravenous magnesium sulfate 8 gm for his accompaqnying hypomagnesium was also administered over four hours. Table 1. Biochemical investigations on admission Case 1 2 3 Plasma Sodium (mmol/L) Potassium (mmol/L) Chloride (mmol/L) HCO3¯ (mmol/L) pH Inorganic phosphate(mmol/L) 141 2.0* 106 24 7.39 0.5* 135 1.8* 114* 12* 7.27* 0.5* 141 1.7* 99 30* 7.46* 1.3 Magnesium BUN Creatinine (mmol/L) (mg/dl) (mg/dl) 0.7 11 0.7 0.8 16 1.0 0.5* 14 0.8 Urine Sodium Potassium Chloride Creatinine Osmolality K+/creatinine (mmol/L) (mmol/L) (mmol/L) (mmol/L) (mosm/Kg.H2O) mmol/mmol 166 12 158 11 894 0.7 44 9 46 2.8 164 2.8* 90 11 80 3.7 241 2.4* 2.1 - -.. TTKG *denotes abnormal values Conclusions A severe degree of hypokalemia with paralysis is a potential life-medical emergency. The causes of hypokalemia paralysis are usually not evident from the history. Emergency physicians should first evaluate whether renal wasting is contributing to the hypokalemic paralysis. Three measurements including Uk(<15-20 mmol/L,might be misleading), UK/UCr ratio(>2), and TTKG(>3) may indicate renal wasting. The UK/UCr reflects a corrected K+ excretion at the time. The TTKG is a semi-quantitative index for Uk that adjusts for the Pk and for water reabsorptionin the medullary collecting ducts. At ER, a simple approach is necessary to clarify its etiologies and subsequently can give correctly rapid potassium replacement and management. We can differentiate hypokalemic paralysis simply based on the patient”s acid-base status on presentation to emergency department.(Table 2 and Figure 1) Table2 常見低血鉀癱瘓之原因 自細胞之間轉移(HPP) 急性鉀離子缺乏(non-HPP) (全身鉀離子有缺乏) (全身鉀離子並未缺乏) 甲狀腺高能症週期性癱瘓 (thyrotoxic periodic paralysis) 家族性週期性癱瘓 (familial periodic paralysis) 偶發性週期性癱瘓 (sporadic periodic paralysis) 高血鈉低血鉀癱瘓 (hypernatremic hypokalemic paralysis) 鋇中毒 (barium poisoning) 有低血氯代謝性鹼中毒 嚴重嘔吐 礦物皮質酮過量 有高血氯代謝性酸中毒 低 NH4+ 分泌 遠端腎小管酸中毒 (primary &secondary (medullary sponge kidney, aldosteronism ,licorice Sjogren’s syndrome) ingestion ,glucocorticoid excess) 腎小管疾病 近端腎小管酸中毒 (Liddle’s syndrome ,Batter’s or Fanconi syndrome Gitelman’ syndrome) 利尿劑 (diuretics) 高 NH4+ 分泌 異位性 ACTH 症候群 腹瀉 (diarrhea state) 輸尿管分流 (ureteral diversion) 濫用甲苯 (toluene abuse) In patients with HPP, there is no obvious acid-base disorder and the UK/UCr ratio is less than 2, while in non-HPP there is associated with abnormal acid-base disorder and the UK/UCr ratio is more than 2. When treating patients with HPP, the dose of KCL should be as small as possible to avoid rebounding hyperkalemia. In contrast, non-HPP due to excessive renal K+ excretion requires large doses of KCL to correct the deficit in total body K+. Finally, close monitoring the plasma potassium, ECG and muscle strength is absolutely necessary in the management of patient with HP. 參考文獻 1.Dunlap HF,Kepler EJ. A syndrome resembling familial periodic paralysis occurring in the course of exophthalmic goiter. Endocrinology 1931;15:541-6. 2.Stedwell RE, Allen KM, Binder LS. Hypokalemic paralyses: A review of the etiologies, patholphysiology, presentation , and therapy. Am J Emerg Med 1992; 10:143-8. 3.McFadzean AJS, Yeung R. Periodic paralysis complicating thyrotoxicosis in Chinese. Br Med J 1967; 1:451-5. 4.Manoukian MA, Foote JA, Crapo LM. Clinical and metabolic features of thyrotoxic periodic paralysis in 24 episodes. Arch Intern Med 1999; 159:601-6. 5.Lin SH, Lin YF, Halperin ML. Hypokalaemia and paralysis. QJM 2001; 94:133-9. 6.Ahlawat SK, Sachdev A. Hypokalaemic paralysis. Postgrad Med J 1999;75:193-7. 7.Ko GTC, Chow CC, Yeung VTF, Chan HHL, Li JKY, Cockran CS. Thyrotoxic periodic paralysis in a Chineses population. QJM 1996; 6:463-8. 8.Lin SH, Chiu JS, Hsu CW, Chau T. A simple and rapid approach to hypokalemic paralysis. Am J Emerg Med 2003 (In Press) 9.Lin YF, Lin SH, Tsai WS, Davids MR,Halperin ML. Severe hypokalaemia in a Chinese male. QJM 2002 10:695-704. 10.Lin YF, Wu CC, Pei D, Chu SJ, Lin SH. Diagnosing thyrotoxic periodic paralysis in the ED. Am J Emerg Med 2002 (In Press) 11.Lin SH, Lin YF. Propranolol rapidly reverses paralysis,hypokalemia,and hypophosphatemia in thyrotoxic periodic paralysis. Am J Kidney Dis 2001; 3:620-23. Figure 1 Clinical algorithm for the approach to patients with hypokalemic paralysis Abbreviation: TPP: thyrotoxic periodic paralysi; FPP: familial periodic paralysis; SPP: sporadic periodic paralysis; RTA: renal tubular acidosis; GS; Gitelman”s syndrome; BS:Bartter”s syndrome Hypokalemia and Paralysis Shift Deficit Low K+ excretion and normal acid-base High K+ excretion and abnormal acid-base Acid-base state TPP FPP Barium poisoning SPP Metabolic acidosis Metabolic alkalosis Blood pressure Normal Toluene abuse Profound diarrhea High RTA GS or BS Diuretics Vomiting Mineralocorticoid excess