Tetanus
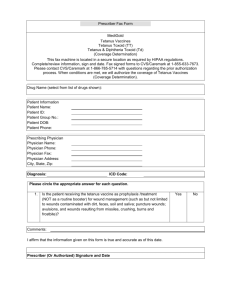
advertisement
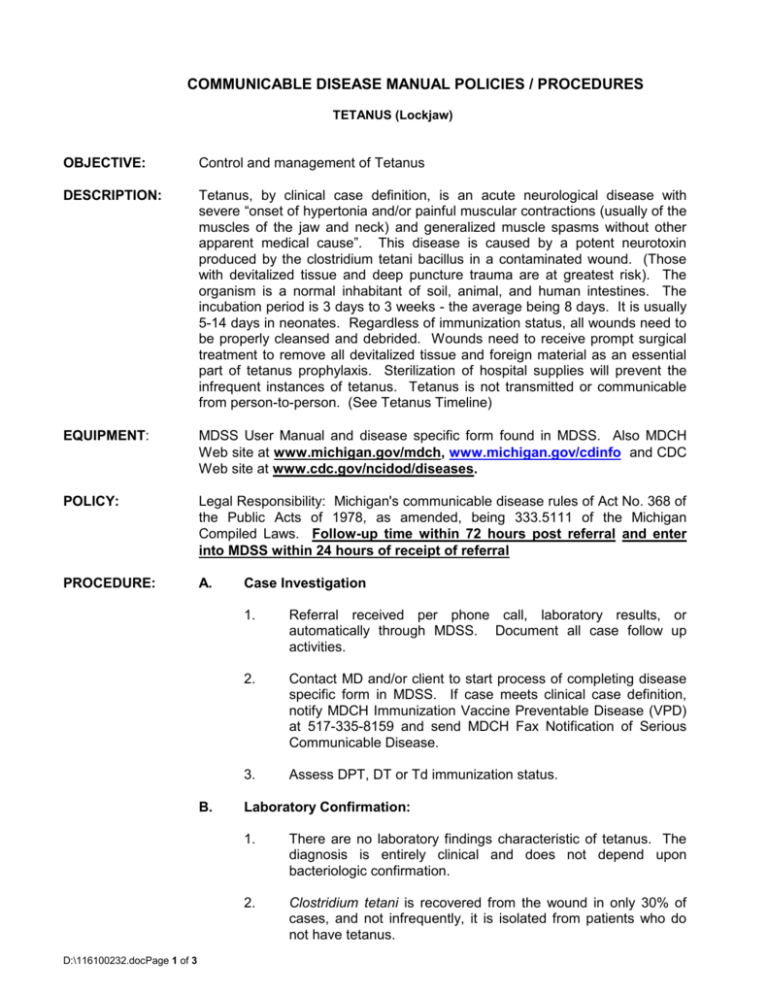
COMMUNICABLE DISEASE MANUAL POLICIES / PROCEDURES TETANUS (Lockjaw) OBJECTIVE: Control and management of Tetanus DESCRIPTION: Tetanus, by clinical case definition, is an acute neurological disease with severe “onset of hypertonia and/or painful muscular contractions (usually of the muscles of the jaw and neck) and generalized muscle spasms without other apparent medical cause”. This disease is caused by a potent neurotoxin produced by the clostridium tetani bacillus in a contaminated wound. (Those with devitalized tissue and deep puncture trauma are at greatest risk). The organism is a normal inhabitant of soil, animal, and human intestines. The incubation period is 3 days to 3 weeks - the average being 8 days. It is usually 5-14 days in neonates. Regardless of immunization status, all wounds need to be properly cleansed and debrided. Wounds need to receive prompt surgical treatment to remove all devitalized tissue and foreign material as an essential part of tetanus prophylaxis. Sterilization of hospital supplies will prevent the infrequent instances of tetanus. Tetanus is not transmitted or communicable from person-to-person. (See Tetanus Timeline) EQUIPMENT: MDSS User Manual and disease specific form found in MDSS. Also MDCH Web site at www.michigan.gov/mdch, www.michigan.gov/cdinfo and CDC Web site at www.cdc.gov/ncidod/diseases. POLICY: Legal Responsibility: Michigan's communicable disease rules of Act No. 368 of the Public Acts of 1978, as amended, being 333.5111 of the Michigan Compiled Laws. Follow-up time within 72 hours post referral and enter into MDSS within 24 hours of receipt of referral PROCEDURE: A. B. D:\116100232.docPage 1 of 3 Case Investigation 1. Referral received per phone call, laboratory results, or automatically through MDSS. Document all case follow up activities. 2. Contact MD and/or client to start process of completing disease specific form in MDSS. If case meets clinical case definition, notify MDCH Immunization Vaccine Preventable Disease (VPD) at 517-335-8159 and send MDCH Fax Notification of Serious Communicable Disease. 3. Assess DPT, DT or Td immunization status. Laboratory Confirmation: 1. There are no laboratory findings characteristic of tetanus. The diagnosis is entirely clinical and does not depend upon bacteriologic confirmation. 2. Clostridium tetani is recovered from the wound in only 30% of cases, and not infrequently, it is isolated from patients who do not have tetanus. 3. C. D. D:\116100232.docPage 2 of 3 Sera collected before TIG is administered can demonstrate susceptibility of a patient to the disease. Immunity/Susceptibility: 1. Susceptibility to tetanus is general. Immunity is conferred by active immunization with tetanus toxoid and persists for ten (10) years after full immunization. Booster doses of tetanus toxoid (given combined with diphtheria toxoid in the form of Td) are indicated every ten (10) years. 2. Because of waning antitoxin titers, most individuals have antitoxin levels below optimal levels ten (10) years after the last dose of tetanus antitoxin. 3. Serologic studies of the U.S. population demonstrate an excellent correlation between vaccination coverage and immunity to tetanus among children. However, antibody levels decline over time, and one-fifth of older children (10-16 years of age) do not have protective antibody levels. Immunity levels are lowest among the elderly. A national population-based seroprevalence survey found that 72% of adults > 70 years of age lacked protective levels of tetanus antibodies (>0.15 IV/ml) [Gergen PJ, et al. A population-based serologic survey of immunity to tetanus in the United States. N Engl J Med 1995:332:761-6.] Control Measures: 1. Prompt recognition of tetanus is important because hospitalization may be required. Prompt administration of tetanus toxoid and TIG may decrease the severity of the disease. Because tetanus is a rare disease, public health authorities may be consulted on clinical management issues. 2. If clinical case definition is met (clinically compatible, reported by a health care professional), regard as true tetanus case. 3. Provide case treatment information, if needed, to care provider. Follow current Red Book guidelines. 4. Assure household members that tetanus is not transmissible person-to-person. 5. Educate household members and general public in managing future wounds. An excellent Question and Answer Tetanus Information Sheet from the Immunization Action Coalition is included with your Fact Sheets in this policy. 6. Promote immunization of Td for adolescent girls and women of childbearing age and other adults when Td vaccine is indicated. Utilize current immunization schedule for children. E. Complete case investigation using disease specific forms located in MDSS. (See MDSS User Manual for entry instructions.) 1. Follow-up with the case or provider one (1) month after the onset of disease to determine clinical outcome/patient status (Recovered, Convalescing, or Died). Also collect any previously missing information for the Tetanus Surveillance Worksheet, with special attention to the following: 2. Number of days hospitalized; Number of days in ICU; Number of days received mechanical ventilation; Post-wound therapy (Tetanus toxoid and Tetanus Immune Globulin); Age at onset; Circumstances of any antecedent injury; Tetanus toxoid vaccination history. In the event of death, obtain and send copies of hospital discharge summary, death certificate, and autopsy report to MDCH Immunization Division. Address: D. D:\116100232.docPage 3 of 3 Michigan Department of Community Health Immunization Division Attn: Immunization Coordinator 201 Townsend Street PO Box 30195 Lansing MI 48913 Refer to current Red Book, current Control of Communicable Diseases Manual, current Epidemiology and Prevention of Vaccine Preventable Diseases, and VPD Guidelines at www.michigan.gov/immunize.