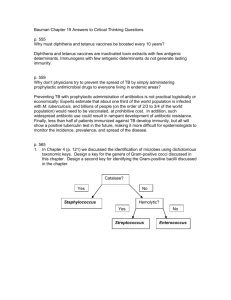
neonates doses
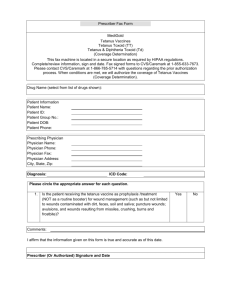
advertisement

Management guideline for tetanus patients in JRRH Childrens’ unit Tetanus is caused by Clostridium tetani, a gram positive anaerobic bacteria found in soil and human and animal intestines It causes muscle spasm by toxin release Generalised tetanus is the commonest clinical presentation It can be fatal Basic management Nurse in quiet, darkened room Minimal handling Clean wounds and remove necrotic tissue Insert IV cannula and nasogastric tube Tetanus causes high energy requirements – ensure patient is fed 2 hourly via NGT, neonates should be fed 1 hourly Specific treatment Neutralise toxin Give tetanus immunoglobulin or anti-tetanus serum as soon as possible Drug Tetanus immunoglobulin Anti-tetanus serum Dose 500 iu in two separate sites (250 iu per site) intramuscularly 1500 units intramuscularly Inhibition of toxin production Give metronidazole 7.5 mg/kg IV 8 hourly for 10 days Neonates require a loading dose of 15 mg/kg IV followed by 7.5 mg/kg IV 12 hourly for 10 days Sedation Survival depends on minimising spasms – it is important that patients receive regular, adequate sedation which should be given IV or via the NGT. Avoid giving im injections. Diazepam 0.3 mg/kg 4-6 hourly Chlorpromazine 0.5 mg/kg 6 hourly Analgesia Tetanus spasms are painful and can be severe enough to cause fractures Prescribe adequate analgesia Paracetamol 15 mg/kg 8 hourly Diclofenac 0.5 mg/kg 12 hourly In severe pain consider morphine: Morphine 0.2 mg/kg 6 hourly –monitor closely for respiratory depression Monitor for signs of superimposed infections especially pneumonia and treat. On discharge Patients who have been managed for tetanus do not develop immunity Tetanus toxoid vaccination should be given on discharge and further doses given 1 month and 2 months after the initial dose. Mothers of neonates with tetanus should also be given tetanus toxoid.