New Patient Medical History Form
advertisement

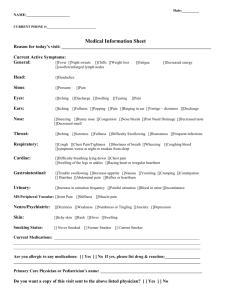
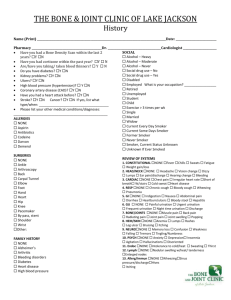
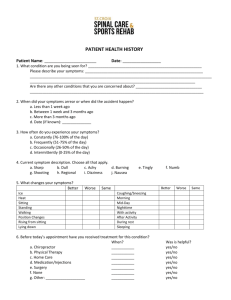
RIVERWOOD FAMILY MEDICINE NEW PATIENT-MEDICAL HISTORY FORM Please complete this form and bring it to your appointment. You may also mail it back to the office prior to your appointment date. Date: _____________________ Full-legal name___________________________________ Date of Birth: ____________________________________ Allergies or drug reactions (list drug and reaction): Please list the conditions you are currently being treated for: Please list any other doctors who are also currently treating you: Past medical history (Please list all hospitalizations, major illnesses and surgeries): Event Date of Occurrence 1 Who lives in your home with you? (Spouse, children, in-laws, significant others, etc.) Your occupation: Do you get regular exercise? (Describe) Do you wear seatbelts? Always Usually Occasionally Never Smoking history: (please check) ____ never smoked ____previous smoker x ____years; quit _____ (when?) ____current smoker x ______years; _____ packs per day Do you use other forms of tobacco such as chewing tobacco, pipe, cigars? If yes, how often? Alcohol Screen: Do you drink beverages that contain alcohol? How often do you have alcoholic beverages? 1/month More than 1/week Have you ever had a drinking problem? 1/week More than 1/month How many cups of coffee or caffeinated drinks do you drink daily? Do you use marijuana, cocaine, any street drugs or prescription drugs that were not prescribed for you? Family History: Age, if living Mother Age at death Health problems or cause of death Father Siblings Children 2 Medications: (Please list all the medication you are taking, including over-the-counter medications, vitamins, herbs and other treatments.) Name of Prescribed by Dosage When is the Purpose Will you be in medication medication taken need of refills at your visit? Vaccinations: Vaccine Tetanus (Td, TdaP, Dtap, Tetanus Toxoid) Influenza Pneumonia Hepatitis B Shingles (Zostavax) Others (please list) Date of last one 3 History of Tests/Exams: Exam Colonoscopy Bone Density Mammogram Pap Smear PSA Eye exam Others (please List) Date last completed Check whether or not you have or have had these conditions: Yes Fatigue Fever or chills Recent weight change Headache Vision changes Eye itching Eye pain Ringing in ears Runny nose Nose bleeds Nasal congestion Snoring Hoarseness Sore throat Mouth sores Breast lump or pain Chest pain Irregular heart beat Pounding heart beat Shortness of breath Cough Wheezing Decreased appetite Difficulty swallowing Heartburn Nausea 4 No Vomiting Abdominal pain Black tarry stools Rectal bleeding Diarrhea Constipation Blood in urine Urinating too often Pain with urination Excessive thirst Weakness Easy bruising Muscle aches Joint pain or stiffness Swelling in arms or legs Dizziness Fainting Memory problems Numbness Anxiety Depression Trouble sleeping Hallucinations Dry skin Itching Lump or spot on skin Rash Stress Other (please list) Do you have any specific concerns for your first visit? (Describe) 5