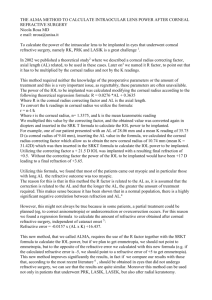
Post-LASIK
advertisement

doctor-hill.com IOL Calculations Determining Corneal Power Following LASIK and PRK The following information contains an outline of several popular central corneal power calculation methods that can be used following the various ablative forms of keratorefractive surgery for myopia, such as LASIK and PRK. As a general rule, IOL power calculations following keratorefractive surgery should not be carried out using popular 2-variable third generation theoretic formulas, such as SRK/T. Instead, the Holladay 2 formula (contained in the Holladay IOL Consultant) should be used in this setting. If your office does not have this software package, a trial version can be downloaded from the Internet at: http://www.docholladay.com/iolprogram.html Most 2-variable formulas such as SRK/T, assume that the anterior and posterior segments of the eye are proportional and use the axial length and keratometric corneal power to estimate the postoperative location of the IOL, known as the effective lens position (ELPo). Unless a correction is made for this situation, the artifactually flattened Ks following keratorefractive surgery have these formulas incorrectly assume a falsely shallow post-operative ELPo.5 The end result is that without a special correction, following LASIK, these formulas will often recommend less IOL power than is actually required. This is a second, and little recognized, source of unanticipated post-operative hyperopia following keratorefractive surgery for myopia. Using the Holladay 2 formula, and the methods listed on the following pages, you and your staff should now be able to do these calculations. For the sake of illustration, we will run through the corneal power estimation and IOL power calculation for an actual patient in our office. Clinical history method 3,4 The clinical history method for corneal power estimation was first described by Holladay and later by Hoffer as: Kp + Rp - Ra = Ka Kp Rp Ra Ka = = = = Where … the average keratometry power before keratorefractive surgery, and … the spherical equivalent before keratorefractive surgery, and … the stable spherical equivalent after keratorefractive surgery, then … the estimate of the central corneal power after keratorefractive surgery. Central corneal power by keratometry will be referred to in diopters (D), even though it is better termed keratometric diopters. This is due to the fact that the cornea has a different index of refraction than manual keratometers or corneal topographers (1.3333 vs. 1.3375).7 Corrected for an estimated vertex distance of 13 mm, the historical estimation of the central corneal power of the right eye following LASIK would be carried out as follows: If the Ks before LASIK were 44.25 D / 45.50 D, and … The refraction before LASIK was -7.50 +1.50 x 123, and … The stable refraction after LASIK was -0.50 +0.50 x 150, then … Kp + Rp - Ra = Ka (49.9) + (-6.21) - (-0.25) = 38.92 D Corrected for an estimated vertex distance of 13 mm, the historical estimation of the central corneal power of the left eye following LASIK would be carried out as follows: If the Ks before LASIK were 44.00 D / 45.25 D, and … The refraction before LASIK was -8.75 +0.75 x 064, and … The stable refraction after LASIK was -1.25 +1.00 x 060, then … Kp + Rp - Ra = Ka (44.6) + (-7.55) - (-0.74) = 37.82 D Using this technique for estimating central corneal power, the following IOL powers are recommended by the Holladay 2 formula: Right Left SA60AT +21.50 D +23.00 D Target Refraction -0.50 D -0.50 D Feiz and Mannis IOL power adjustment method 1 Another method that I like to use when good historical data is available is the IOL power adjustment method of Feiz and Mannis. This is the method that is least likely to result in a post-operative hyperopic surprise. As you will see on the last page, we use this method to set an upper limit of possible IOL powers. Using this technique, first the IOL power is calculated using the pre-LASIK corneal power as though the patient had not undergone keratorefractive surgery. This pre-LASIK IOL power is then increased by the amount of refractive change at the spectacle plane divided by 0.7. The calculation is for a -0.50 D result. This approach is outlined as follows: IOLpre + (∆D 7) = IOLpost Where … IOLpre = the power of the IOL as if no LASIK had been performed, and … ∆D = the refractive change after LASIK at the spectacle plane, then … IOLpost = the estimated power of the IOL to be implanted following LASIK. The Feiz and Mannis IOL power adjustment method for the right eye following LASIK would be carried out as follows: If the Holladay 2 calculated IOL power before LASIK is +12.50 D, and … The change in refractive power at the spectacle plane is +6.50 D, then … IOLpre + (∆D / 0.7) = IOLpost +12.50 D + (+6.50 / 0.7) = +21.78 D The Feiz and Mannis IOL power adjustment method for the left eye following LASIK would be carried out as follows: If the Holladay 2 calculated IOL power before LASIK is +13.00 D, and … The change in refractive power at the spectacle plane is +7.63 D, then … IOLpre + (∆D / 0.7) = IOLpost +13.00 D + (+7.63 / 0.7) = +23.90 D Using this technique, the following IOL powers are recommended by the Holladay 2 formula: Right Left SA60AT +22.00 D +24.00 D Target Refraction -0.50 D -0.50 D Modified Maloney method 2,9 Another method of post-LASIK corneal power estimation is one that was originally described by the well-known refractive surgeon Robert Maloney and subsequently modified by Doug Koch and Li Wang. The advantage of this method is that it requires no historical data and has a very low variance when used with either the Holliday 2 formula or the 2-variable formula double K correction nomogram published by Koch and Wang. 2 Using this technique, the central corneal power is obtained by placing the cursor at the exact center of the Axial Map of the Zeiss Humphrey Atlas topographer. This value is then converted back to the anterior corneal power by multiplying the Axial Map central topographic corneal power by 376.0/337.5, which is the same as 1.114. An assumed posterior corneal power of 6.1 D is then subtracted from this product. (CCP x 1.114) - 6.1 = Post-LASIK adjusted corneal power Where … CCP = the corneal power with the cursor in the center of the Refractive Map Of the Zeiss Humphrey Atlas topographer. The Modified Maloney method for the right eye following LASIK is carried out as follows: If the Refractive Map central corneal power is 40.00 D, then … (CCP x 1.114) - 6.1 = Post-LASIK adjusted corneal power (40.00 D x 1.114) - 6.1 = 38.46 D The Modified Maloney method for the left eye following LASIK is carried out as follows: If the Refractive Map central corneal power is 39.90 D, then … (CCP x 1.114) - 6.1 = Post-LASIK adjusted corneal power (39.90 D x 1.114) - 6.1 = 38.35 D Using this technique for estimating central corneal power, the following IOL powers are recommended by the Holladay 2 formula: Right Left SA60AT +22.00 D +22.50 D Target Refraction -0.50 D -0.50 D Postoperative regression method 8 Yet another method of post-LASIK corneal power estimation is the postoperative regression method that has been shared with us by Doug Koch and Li Wang. Using this technique, the 0 mm, 1 mm and 2 mm annular rings of the Numerical View of the Zeiss Humphrey Atlas topographer are averaged together. This topographic-based averaged central corneal power is then multiplied by 1.23 and then 10.41 is then subtracted from this product. The advantage of this method is that it requires no historical data. (CCP x 1.23) - 10.41 D = Post-LASIK adjusted corneal power Where … CCP = the averaged values of the 0 mm, 1 mm and 2 mm annular rings. The postoperative regression method for the right eye following LASIK would be carried out as follows: If the averaged topographic central corneal power is 40.07 D, then … (CCP x 1.23) - 10.41 D = Post-LASIK adjusted corneal power (40.07 D x 1.23) - 10.41 D = 38.88 D The postoperative regression method for the left eye following LASIK would be carried out as follows: If the averaged topographic central corneal power is 39.40 D, then … (CCP x 1.23) - 10.41 D = Post-LASIK adjusted corneal power (39.40 D x 1.23) - 10.41 D = 38.05 D Using this technique for estimating central corneal power, the following IOL powers are recommended by the Holladay 2 formula: Right Left SA60AT +21.50 D +23.00 D Target Refraction -0.50 D -0.50 D Topographic central corneal power adjustment method 2,9 The last method of post-LASIK corneal power estimation was originated by Doug Koch and Li Wang and is based on determining the central power of the cornea using either the Zeiss Humphrey Atlas topographer or the adjusted effective refractive power (EffRPadj) of the Holladay Diagnostic Summary of the EyeSys Corneal Analysis System. Using this technique, the 1 mm and 2 mm annular power rings of the Numerical View of the Zeiss Humphrey Atlas topographer are averaged together, or the adjusted effective refractive power (EffRPadj) is determined, and that figure is reduced by 19% for every diopter of myopia corrected by LASIK. CCP - (∆D x 0.19) = Post-LASIK adjusted corneal power Where … CCP = the EffRPadj, or the averaged Zeiss Atlas central corneal power, and … ∆D = the refractive change after LASIK at the spectacle plane. The topographic central corneal power adjustment method for the right eye would be: If the averaged topographic central corneal power is 40.06 D, and … The change in refractive power at the spectacle plane is +6.50 D, then … CCP - (∆D x 0.19) = Post-LASIK adjusted corneal power 40.06 D - (+6.50 x 0.19) = 38.83 D The topographic central corneal power adjustment method for the left eye would be: If the averaged topographic central corneal power is 39.36 D, and … The change in refractive power at the spectacle plane is +7.63 D, then … CCP - (∆D x 0.19) = Post-LASIK adjusted corneal power 39.36 D - (+7.63 x 0.19) = 37.91 D Using this technique for estimating central corneal power, the following IOL powers are recommended by the Holladay 2 formula: Right Left SA60AT +21.50 D +22.50 D Target Refraction -0.50 D -0.50 D Hard contact lens method 3, 6 Following all forms of ablative keratorefractive surgery (LASIK, PRK, etc.) a review of the literature now suggests that the hard contact lens method may be less accurate than originally thought. For this reason it is not recommended in this clinical setting. Higher order optical aberrations following keratorefractive surgery The higher order optical aberrations that often accompany the various forms of keratorefractive surgery, and the multifocal nature of some of these corneas, will remain unchanged following cataract surgery. Understandably, some patients mistakenly expect that cataract surgery will alleviate these symptoms. Unfortunately, this is not the case. It is important to discuss this fact with these patients prior to surgery so that their expectations will be realistic. For example, the third and fourth order higher order aberrations produced by radial keratotomy can be as much as 35 times normal values. Significantly elevated third and fourth order aberrations are also seen following some of the early forms of LASIK that employed a large spot size and a non-Gaussian distribution strategy. Also, the change from a prolate (steep central cornea) to an oblate (flattened central cornea) ocular system produced by lowering the central corneal power may result in decreased discrimination at higher spacial frequencies. This will not change after cataract surgery, Accuracy of intraocular lens power calculations following LASIK It is important to explain to your patient that intraocular lens power calculations following all forms of keratorefractive surgery are, at best, problematic. You should also discuss the fact that in spite of our very best efforts, the final refractive result may end up more hyperopic, or more myopic than expected. The fact that multiple methods are in use is eloquent testimony to how far we still have to go in this area. It is a disappointment to all of us that given available technology, there is simply no single reliable method to accurately determine the net central power of these unusual eyes. Intraocular lens exchange or secondary piggyback implantation after all forms of refractive surgery, are important parts of informed consent prior to cataract surgery. Given the limitations of available technology, this fact must be clearly understood by every patient as a well-recognized consequence of prior keratorefractive surgery. Below is a summary of IOL powers, generated by several forms for central corneal power estimation. Some have certain characteristics, which we can use to better understand what the correct IOL power may be. By effectively bracketing, it is possible to modestly improve the accuracy of an inherently inaccurate exercise. However, when refractive surgery results in a highly multifocal cornea, or there is unaccounted for lenticular myopia, this system can show variable and unexpected results. When this system of bracketing breaks down, one or more pieces of the mathematical puzzle are either missing, masked, or inaccurate. Often, the calculations may be influenced our inability to determine the true post-LASIK refractive state (without the influence of lens-induced myopia). It is generally accepted that IOL power calculations following keratorefractive surgery are always placed on the myopic side and are typically for -0.50 D. This helps to prevent unexpected post-operative hyperopia. Calculation method Feiz and Mannis IOL Power OD +22.00 D IOL Power OS +24.00 D Often higher limit correct IOL power - - - - - - - - - - - - - - - - - - - - - - - - - - - - - - - - - - - - - - - - - - - - - - - - - - Clinical history +21.50 D +23.00 D Modified Maloney +22.00 D +22.50 D Correct IOL power is often in this Topo central power adjust +21.50 D +22.50 D area between upper and lower limits Postoperative regression +21.50 D +23.00 D - - - - - - - - - - - - - - - - - - - - - - - - - - - - - - - - - - - - - - - - - - - - - - - - - - Flattest measured K +20.50 D +22.00 D Often lower limit correct IOL power Sim Ks by topography +18.50 D +20.00 D Usually below correct IOL power Measured Ks +20.00 D +21.00 D Usually below correct IOL power - - - - - - - - - - - - - - - - - - - - - - - - - - - - - - - - - - - - - - - - - - - - - - - - - - SA60AT Right Eye Recommended power Target refraction +21.50 D +22.50 D -0.50 D -0.50 D MTA4UO Right Eye Recommended power Target refraction SA60AT Left Eye MTA4UO Left Eye +18.50 D +19.50 D -0.50 D -0.50 D Best overall estimate of IOL power References 1. Feiz V., Mannis M.J. Garcia-Ferrer F. Intraocular lens power calculation after laser in situ keratomileusis for myopia and hyperopia a standardized approach. Cornea 2001; 20:792–797. 2. Koch, D., Wang I. Calculating IOL power in eyes that have had refractive surgery. J Cataract Refract Surg 2003 29(11) 2039-2042. 3. Holladay JT. Consultations in refractive surgery. Refract Corneal Surg 1989; 5:203 4. Hoffer KJ. Intraocular lens power calculation for eyes after refractive keratotomy. J Refract Surg 1995; 11:490–493 5. Aramberri J. Intraocular lens power calculation after corneal refractive surgery: Double K method. J Cataract Refract Surg 2003; 29: 2063–2068. 6. Haigis W. Corneal power after refractive surgery for myopia: contact lens method. J Cataract Refract Surg 2003 29 (7) 1397-1411. 7. Seitz B. Intraocular lens power calculation in eyes after corneal refractive surgery. J Refract Surg 2000; 16:349–361 8. Personal communication, April, 2004. Douglas D. Koch, MD, Cullen Eye Institute, Baylor College of Medicine, Houston, Texas. 9. Wang L, Booth MA, Koch DD. Comparison of intraocular lens power calculations methods in eyes that have undergone LASIK. Ophthalmology 2004 111(10) 18251831.