Toilet Training for Children - LNNM
advertisement

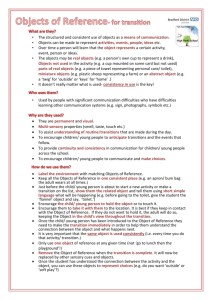
Toilet Training for Children with Special Needs Toilet Training for Children with Special Needs Project Report By Rachel Muncey, Paediatric Special School Nurse 1 Toilet Training for Children with Special Needs Abstract One of the most important skills an individual can learn is how to use the toilet successfully and independently (Wheeler, 2007). Similarly, elimination, washing and dressing have been identified by Roper, Logan and Tierney (2000) as fundamental activities of daily living that increase independence and quality of life. Typically developing children establish control of their bowel at age two and control of their bladder at age three. Thus toilet training is performed by parents or guardians in the home setting, and/or carers in the nursery setting. Researchers have reported that children with an autistic spectrum disorder (ASD) are the most challenging to toilet train and their difficulties often arise from a problem called Sensory Processing Disorder (SPD) which affects almost all who have ASD (Wheeler, 2007). In addition, some children with physical disabilities have limited ability to perform skills such as sitting, flushing, and washing hands and are therefore unlikely to reach full toileting independence. Correspondingly Bhupendra, Masey and Morton (2006) state that a severe impairment in mobility could delay toilet training. Thus children with ASD and physical disabilities commonly present in school with incontinence. There are no standardised guidelines that state who is best qualified to support children with learning difficulties to attain continence (Harris, 2004) however Education and Resources for Improving Childhood Continence (ERIC) (1999) state that the approach should be interprofessional. Therefore this project aims to develop toilet training in Special Needs Schools for the aforementioned children, using expertise and input from parents and professionals across different disciplines. Background - National The Royal College of Nursing (2006), state that continence support, advice and information should be available to all children and their families. Continence should be promoted though the main aim is to ensure bladders and bowels are healthy. They state that all children should have a trial of toilet training, however there are a number of children who will not achieve full continence. There are no national guidelines for toilet training for children with special needs though there are many accessible resources available that will be utilised in this project. Background - Local In March 2013 there were four Special Needs Schools in the borough of Islington in which the need for specialist toilet training was becoming increasingly apparent. This was due to the range and complexity of children that attend the schools, and the large proportion of them who had not achieved bladder and bowel continence. A successful bid was made for funding from the Florence Nightingale Foundation in order to support more 2 Toilet Training for Children with Special Needs children with special needs to achieve their potential with regard to toileting independence. A budget of £3,500 was provided. There are a variety of health professionals who work with children and their families who provide input towards toilet training. These include School Nurses, Occupational Therapists (OTs), Speech and Language Therapists (SLTs) and Teaching staff. Additionally, Support Workers provide toileting care to some of the children who access specialist respite and after school clubs. The professionals listed above are employed by a variety of agencies including the National Health Service, Local Education Authority, Charities and Government funded schemes. Toilet training had been initiated in the past by different workers and in a variety of settings, however little progress was made and the training had been given up on. It was a challenge for the many service providers to keep to a structured programme, and often there was not a named lead professional for distributing a plan and problem solving when new issues presented. As a result, a primary aim for this project was to designate lead professionals, and empower all who work with and care for these children to adapt and follow a scheduled plan for toileting, as this increases the effectiveness of training (Wheeler, 2007). Current Local Service Bladder and Bowel Care Team – No Specialist Paediatric Continence Advisor, however these are present in other NHS Trusts Nursing assessments performed annually or when conditions change or when different continence products are required. Referrals are made for issues such as constipation and overflow diarrhoea. No specialist training provided for professionals Continence pads provided up to a maximum of 5 per day (unless special circumstances). No padded pants/trainer pants/ car seats available. These must be purchased by parents. School staff performs toilet training. There is therapy input such as PECS/communication boards from SLTs and toilet assessments done by OTs however this is not joined up. The financial cost of continence products provided for individuals in Islington borough is approximately £1,000,000 per year. Project Aims o To increase children’s independence with toileting o To empower parents and staff to implement and develop toilet training plans Method o To increase the knowledge of all those in the multidisciplinary and multiagency teams regarding continence and toilet training (Timeline) o Towith saveexplanation money by reducing use of continence products 3 Toilet Training for Children with Special Needs Participants Children were identified to be participants who were displaying signs of readiness for toilet training. These included some of the following: 1. Mental age of more than two years 2. Awareness of being wet or dirty 3. Ability to stay clean and dry for 1-2 hours at a time 4. Ability to stay clean and dry during naps 5. Physical ability to sit on the toilet 6. Ability to cooperate and assist with dressing and undressing 7. Not having any medical conditions that may affect toilet training (Fleming and MacAlister 2013). The multi-disciplinary team (MDT) identified prospective participants based on the above criteria. Furthermore, details of the projects were entered into the school newsletters and some parents expressed an interest and put their children forward to participate. In total, 28 children were involved in the project. Use of Funding A large proportion of the grant provided was used to host a 3 hour training session in order to increase the knowledge and skills regarding toilet training. The session was provided by a Paediatric Continence Nurse, employed by the leading continence organisation; Education and Resources for Improving Childhood Continence (ERIC). 45 staff members from the following disciplines attended: o School Nurses o Occupational Therapists o Speech and Language Therapists o Teachers o Teaching Assistants o Respite Support Workers o Midday Supervisors o Nursery Nurse o Clinical Psychologist o Therapy Assistant o Healthcare Assistant The information was then presented to parents and caregivers at a parent support group meeting at each school. Providing training to parents is a vital component to successful continence training (Kroeger and Sorensen 2010). The presentations were given by the School Nurses, using the resources provided by the ERIC Nurse. The Lead Nurse for Bladder and Bowel Care attended and opened the floor to questions and answers. During this time some of the assessments listed below in the method were conducted with parents. 4 Toilet Training for Children with Special Needs The remaining funding was used for: o Purchase of the highly recommended book: ‘Toilet Training for Individuals with Autism or other Developmental Issues’, by Maria Wheeler o Purchase of continence products including washable pads and seat covers o Nursing agency cover for the special schools in order for assessments and follow up to be conducted by the School Nurses Method Once children had been identified they then underwent a formal assessment of readiness. The method performed coincides with recommendations from the RCN (2006) on ‘Supply of paediatric continence products’ (page 6). The vast majority of assessments utilised were already available, produced by the local Bladder & Bowel care service and in use by the School Nursing team. Firstly, a Paediatric Assessment (see Appendix 1) was completed by the School Nursing Team with parents. This included the following key features: o Fluid Intake and Diet o Bowel Habit and the use of medications o Development Stage o Communication and Behaviour o Mobility, Dexterity o Environment The assessment enabled any underlying medical conditions affecting toileting to be identified, such as constipation. Children could then be referred to the School Doctor or General Practitioner for review and treatment if required. Secondly, a Toileting Chart (see Appendix 2) was provided both to school and to parents in order to track and record when a child opens their bowels or passes urine. This chart was adapted from the locally produced chart, and its suitability verified by the Bladder & Bowel Lead Nurse prior to use. By requesting both school staff and parents to monitor toileting, it promoted the concept of shared care and joint responsibility, something that had been identified as lacking in previous attempts at toilet training. Once this was completed, a Toilet Skills Assessment (see Appendix 3) was completed. Again, this enabled assessment of readiness for toileting as it helped to determine: 1. A maturing bladder that can hold urine for 1½ - 2 hours. 2. A healthy bowel that is not constipated 3. The ability to sit on the toilet for sufficient time. It was at this stage that some children were identified as unsuitable to commence toilet training as they either could not sit for an adequate length of time, had constipation that needed treatment or their urinary frequency was too high. For these children we were still able to create small targets, 5 Toilet Training for Children with Special Needs such as to work at encouraging the child to sit on the toilet for longer by using distraction or a favourite toy. This enabled teachers and parents to contribute to development of toilet training, even if it was small progress in very early stages. For these children a Reassessment Checklist (see Appendix 4) was completed whereby current provision of continence products was reviewed. The Reassessment Checklist was also completed for children deemed ready to commence training. Changes to products could be made to support toilet training, such as changing supply of pads with side tabs, to pull-up pads. For some children, the series of assessments were completed over the summer holidays, as part of a joint School Nurse and OT home visit. This again promoted the theme of shared care and enabled the OT to assess the need for specialised adaptive equipment at home and similar equipment in school, for example foot stools and grab rails. It was possible to ascertain the methods of communication used and relay this to the child’s allocated SLT in school in order to create communication aids used during toileting. For example some children used a makaton sign for toilet, whilst others pointed to a symbol. It was also useful to discuss a reward system for correct use of the toilet that could be developed as a fun incentive. During these visits a good rapport was built with the child and family, and support was offered by telephone if needs arose in the future. Following completion of assessments, toileting plans were discussed with class teachers and then implemented both in the school and home setting to maintain consistency. Some parents decided to delay beginning toilet training due to circumstances, for example the birth of a new child in the family. This coincides with advice from the Trust’s Clinical Psychologist who recommended delaying training during stressful times. Each plan created was child specific and some of these are described in Appendix 5. Parents were encouraged to regularly inform their child’s teacher of progress using their home-school communication book, and to telephone the school nurse, OT or SLT with any queries. The school nurse provided up to three follow-up telephone calls to troubleshoot further problems and adapt plans as progress was made. 6 Toilet Training for Children with Special Needs Results Of the 28 children that were identified to participate…. 1 Child became continent of urine in the daytime prior to beginning a formal plan. (Number 1 on chart) 3 Children became fully continent during the daytime. (Number 2 on chart) 11 Children developed some new toileting skills but are not fully continent of urine in the daytime. (Number 3 on chart) 8 Children did not have thorough assessments and plans created as parents decided not to participate. Progress made is unknown. (Number 4 on chart) 1 Child could not commence training due to changes with medication. (Number 5 on chart) 3 Children’s parents felt their child was too young or not yet ready. (Number 6 on chart) 1 Child left the borough and therefore we were unable to continue to monitor. (Number 7 on chart) 0 Child did not make any visible progress. (Number 8 on chart) Results 12 11 Number of Children 10 8 8 6 4 2 3 3 1 1 1 0 0 1 2 3 4 5 6 7 8 For the three children who have achieved continence, a total of £6,400 per year will be saved by the NHS in continence pads that are no longer required. 7 Toilet Training for Children with Special Needs Case Study Luke (pseudonym used to maintain confidentiality) When original assessments were performed with Luke and his Mother in summer 2013 it became apparent that Luke was very fearful of the toilet environment and would not even enter the toilet in his home. He wore pads supplied by the continence team and would not use the toilet. He had had a previous frightening experience where he had locked himself in the toilet and then was unable to unlock the door. Luke was displaying many signs of readiness, such as staying dry for up to 2 hours and indicating when he was wet. A specific toileting plan was created for Luke that included: Removal of the bathroom door at home to alleviate fear of becoming trapped again Mum to change Luke’s pad initially just inside the bathroom, and gradually take him closer to the toilet each time. Once Luke felt comfortable enough, Mum encouraged Luke to sit on the toilet at regular intervals; after snack and meal times. She would stand in the doorway encouraging and praising him when he urinated or opened his bowels in the toilet. Whilst toilet training Luke would wear trainer pants so that he had the sensation of being ‘wet’ if he had an accident. School staff also took Luke to the toilet at regular intervals and created a reward chart for him in school. He was able to use a favourite toy whilst he sat on the toilet and was rewarded each time he used the toilet to urinate or open his bowels. Luke’s Mother said that she identified a big change once Luke felt secure in the bathroom environment. It took approximately 8 months for Luke to become continent during the daytime and required both school and his Mum to provide lots of encouragement, use social stories and reward charts. Mum says he now goes by himself and sometimes will inform her that he is going by using the word ‘toilet’ Mum commented that it is brilliant that he can now go independently and she is very happy. 8 Toilet Training for Children with Special Needs Quotes from Teachers, Health Staff and Parents Quote from a Mother: o I think it’s wonderful because I was afraid he would have all his life in a nappy so it’s amazing that now he doesn’t! Quotes from Teaching Staff: o He is now much more independent and we see his confidence (TA) o He's generalised his understanding and ability to follow instructions in toilet training to other situations in class, and he's moved from a single PODD page that he used for the toilet to a PODD book. (TA) o The toilet training made him more determined to communicate his needs. (Teacher) o We would never be able to do it unless we worked as a team with parents. (TA) o It's been such a lovely experience working together with parents to see what their child can achieve. (Teacher) o The experience has shown us all never to underestimate what a child can achieve. (TA and Teacher) o Unless you give the opportunity, you will never know what a child can achieve independently. (Teacher and TA) o I never expected that he would be completely out of pads (day and night) after 3 months. (Teacher) o I found the training really helpful and have passed on information to family and friends too. It’s useful to know correct positioning and for boys to aim at something floating in the toilet like a ping pong ball. (TA) o Having training meant that an informed discussion could be had between staff and parents. There were different expectations between a parent and staff regarding a child’s readiness and we were able to explain this to parents based on knowledge gained. (TA) o It would have been helpful for parents to attend the same training session to enable an open discussion. (TA) 9 Toilet Training for Children with Special Needs Results of Training Sessions A questionnaire was compiled to assess parents’ views on the usefulness of the information session (See Appendix 6). The results are displayed in graphs: Number of parents Was this session relevant to you and you child? 4.5 4 3.5 3 2.5 2 1.5 1 0.5 0 1 2 3 4 5 1 - Not very relevant 6 7 8 9 10 - Very relvant 10 Number of parent Did the presentation have the right amount on information for you? 3.5 3 2.5 2 1.5 1 0.5 0 1 2 3 4 1 - to little 5 6 7 5 - just right 8 9 10 10 - too much Number of Parents Did the session help with your understand of toilet training 3.5 3 2.5 2 1.5 1 0.5 0 1 2 3 4 5 1 - No 6 7 8 9 10 10 - Yes 10 Toilet Training for Children with Special Needs Number of parents Did you find the questions and answer session with the continence nurse useful? 8 6 4 2 0 1 2 3 4 5 1 - No 6 7 8 9 10 2 - Yes Number of parents Would you recommend this session to other parents? 10 8 6 4 2 0 1 2 3 4 5 6 7 1 - No 8 9 10 10 - Yes A different questionnaire was also created to assess staff members’ response to the training (see appendix 7). The results are: Can think of children and families in class or on caseload who are ready for developing toilet training 1 1 or 2 children – 47% 3 or more children – 53% 0 1 or 2 3 or more 11 Toilet Training for Children with Special Needs Feel that prioritising toilet training as a functional skill is an appropriate focus during school time No Not Sure Yes Feel we have sufficient toilet seats/equipment at school to support children with toilet training Yes – 27% No – 40% Not Sure – 33% Yes No Not Sure Understand w hat m y role is as part of the MDT supporting children w ith toilet training Yes – 73% No – 0% Not Sure – 27% Yes No Not Sure 12 Toilet Training for Children with Special Needs Have appropriate communication tools and rewards to support childrn with toilet training Yes – 50% No – 25% Not Sure - 25% Yes No Not Sure Limitations There were numerous factors that limited the ability of children to develop continence and toileting skills. These include: Not enough time for the School Nurse, SLT and OT to perform joint home visits for all children Some follow up phone calls for parents were not performed due to parents missing calls and calling back when School Nurse was unavailable School holidays disrupted routines causing some children delays in their progress. There were differing levels of parent motivation. Some parents were enthusiastically implementing plans and following recommendations whereas some parents struggled to implement plans as they felt that their child was unable to achieve continence or develop skills in this area. Differing levels of teachers’ motivation. Some teachers placed high importance on developing toileting skills, especially if it was one of the child’s targets. Some teachers did not see this as a priority. Some family circumstances meant that it was not appropriate to begin toilet training at that time, for example a new baby or a brereavement. Staff shortages affected ability to implement plan in school setting. Teachers who did not attend training did not feel as confident to implement plans. Recommendations To provide adequate training for both staff and parents regarding toilet training for children with special needs. If there is a paediatric continence advisor in the borough then they could provide this. If not, then funding should be allocated for this to be delivered by an external company such as ERIC. 13 Toilet Training for Children with Special Needs To perform initial assessments jointly ideally with parents, School Nurse, OT, SLT and Teacher. To create a toileting plan that everybody working with the child is aware of and can be delivered both at home, school and at respite/play centres. To provide regular telephone follow up, support and advice. All recommendations fit within the proposed model of care that has been developed and is displayed below. Proposed Model of care for use in Special Needs Schools London wide 14 Toilet Training for Children with Special Needs Future Plans The proposed model will continue to be used within the current setting. It can be developed as services develop and include new assessments as these are continually updated by the Bladder and Bowel care team. The model will be used locally in the Special Needs Schools, especially when new starters begin in September each year The model can potentially be distributed further through publication in relevant journals, presentation at conferences and via network groups such as the Royal College of Nursing School Nursing forum. Observations made Personal observations have been made since the training session in June 2013. Parents and teaching staff appear empowered to continue with the original plans, updating and adapting them as necessary following discussions with the MDT. Some teachers have used their newly gained knowledge to take the lead in developing toilet training plans which they have verified with the School Nurse before implementing and sending to the family. At one school site the School Nurse left the post so the teachers took the lead in developing and implementing plans. For the children that made most progress, they had been identified as ready when initially assessed. For those who were not showing signs and whose parents wanted to continue regardless, they gained some skills however did not achieve continence. Parents’ motivation played a big part. Even if a child was assessed as ready to begin toilet training and plans were put in place in school, if they were not followed at home and the parents did not provide much input then very little progress was made. Related research, guidelines and articles The Whittington Health Librarian kindly conducted a literature search regarding ‘toilet training’ and ‘children with special needs’. Two relevant National Institute for Health and Care Excellence guidelines were identified and taken into account. Databases searched included: CINAHL, Medline, BNI, EMBASE & PsycInfo and this produced 7 highly relevant articles, and 17 more general articles some of which have been quoted within this report. The results are in Appendix 8 and can be utilised for further reading. 15 Toilet Training for Children with Special Needs Conclusion This project was originally embarked upon as there was no integrated approach to toilet training within four Special Needs Schools in London. The aims were to ultimately increase children’s independence with toileting, empower parents and staff to implement plans and save money by reducing use of continence products. A grant of £3,500 from the Florence Nightingale Foundation was used in order to meet the project aims. 28 children participated and were assessed using adapted resources from the local Bladder and Bowel care service. Training was provided to the multidisciplinary team and a parent information session was held prior to commencement of toilet training. Questionnaire results proved that staff and parents found the training relevant, helped with their understanding and they would highly recommend it to others. The toilet training results were extremely positive with some children achieving full continence and many others developing new skills. Many of the staff members were pleasantly surprised at the children’s’ ability to develop new skills when they worked together with parents as a team. For the three children who have achieved continence, a total of £6,400 per year will be saved by the NHS in continence pads that are no longer required. There were some limitations to the success of the project including time, differing levels of motivation, holidays interrupting routines and staff shortages. As a result of this project a proforma has been developed as a model for use across other London Special Needs Schools. This could be distributed to other schools through a variety of methods and adapted for use in the local area. 16 Toilet Training for Children with Special Needs References ERIC, 1999. Bowel and Bladder Management in Children with Special Physical Needs, A Guide for Parents. Bristol: ERIC. Fleming, E. and MacAlistair, L., 2013, Learning to wee and poo in the right place – Continence problems in children with autism, PowerPoint presentation, National Autistic Society, London. Harris, A., 2004. Toilet training children with learning difficulties: What the literature tells us. British Journal of Nursing,13(13), pp.773-777. Kroeger, K. and Sorensen, R., 2010. A parent training model for toilet training children with autism. Journal of Intellectual Disability Research, June, 54(6), pp.556-567. Roper, N., Logan, W. W. and Tierney, A. J., 2000. The Roper-Logan-Tierney Model of Nursing: Based on Activities of Living. Churchill Livingstone Royal College of Nursing, 2006. Paediatric assessment of toilet training readiness and the issuing of products. London: Royal College of Nursing. Singh, B.K., Masey, H. and Morton, R., 2006. Levels of continence in children with cerebral palsy. Paediatric Nursing, June, 18(4), pp.23-26. Wheeler, M., 2007. Toilet training for individuals with autism and other developmental issues. Texas: Future Horizons. 17 Toilet Training for Children with Special Needs Appendices 1. Paediatric Assessment Bladder & Bowel Care Service Paediatric Assessment Form Patients Details Name: DOB: Parents Name: Child's position in the Family: GP Contact details: NHS No: M/F: Address: Professionals involved in Care : Postcode: Phone: Mobile: Ethnicity: Patient’s Borough: Camden School: Assessment completed by: Medical Diagnosis: i. ii. iii. Brief Medical History: Islington School Nurse: Assessment date: Medication, including complimentary medication: Allergies: Fluid intake How many drinks in 24 hours? Diet Any special diet eaten? What do they drink? Do they eat fruit? Is intake restricted and if so when? Vegetables? Beaker bottle cup with straw bottle sports Cereals? Any dietary problems? 18 Toilet Training for Children with Special Needs Enteral Feeding Feed: hours: Quantity in 24 Water: Flushes: Food Allergies? Bowel Habit Daily: Alternate Days: Less Often: Laxatives: Yes No Suppositories: Yes Constipated: Diarrhoea: Enemas: Yes Where it occurs: Anywhere Hides Development Stage Has your child ever been dry? Can they use a potty/toilet? No Soiling: Yes Type (Bristol Stool Chart): No Yes No No Has potty training ever been attempted? Yes No If yes, when did they stop? Can they reach the potty/toilet in time? Yes No Does your child know if they are wet/soiled? Yes No Are they able to indicate that they are? Yes Are they afraid to sit on the toilet? Yes No Are they dry at night? Yes Wears: nappies No Do they refuse to sit on the toilet? Yes No No pull ups underwear How many times is the nappy changed in 24 hours? Communication How does your child communicate? Normal speech Yes No Limited Speech Yes No Sign language Yes No No Communication Yes No Other form Yes No Behaviour Does your child have any behavioural problems related to incontinence? Yes How does your child manage his/her incontinence at school? No How does your child manage his/her incontinence at home? Any other problems related to incontinence i.e. Change of school/home: 19 Toilet Training for Children with Special Needs Birth of brother/sister: Death or illness in the family: Marital breakdown: How bothersome is the wetting/soiling problem (please tick the appropriate number - 1 being no bother and 10 being very bothersome) To your child 1 2 3 4 5 6 7 8 9 10 To you as a parent carer 1 2 3 4 5 6 7 8 9 10 Brothers/sisters 1 2 3 4 5 6 7 8 9 10 Mobility Walks unaided: Yes No If no, give details: Buggy/wheelchair Yes No Able to transfer unaided Yes No Any other problems? Physio: Occupational Therapy: Orthotics: Dexterity Does your child need help pulling down clothes? Yes No Does your child need help cleaning/wiping? Yes No Does your child need help readjusting clothes? Environment Toilet location and At Home: distance: Yes No At School: Special equipment i.e. footstool/Ring Reducer/Potty Chair? Does your child share a room? Yes No Are the family in temporary accommodation? 20 Toilet Training for Children with Special Needs 2. Toileting Chart Bladder & Bowel Care Service Toileting Chart Please follow the individual toilet training plan and complete the chart below so that we can see what your child is doing both at home and school. Record in the 'Nappy column whether the pad/pamts were wet (W) or dry (D), or if the child opened their bowels (B). Record in the 'Toilet' column whether the child did a wee (W) or opened their bowels (B) on the toilet. Each time your child has a drink, record it by putting a tick in the 'Drink' column. Day 1 Day 2 Day 3 Day 4 Day 5 Day 6 Day 7 Date: 7am 8am 9am 10am 11am 12am 1pm 2pm 3pm 4pm 5pm 6pm 7pm 8pm 9pm 10pm 21 Drink 6am Nappy Toilet Drink Nappy Toilet Drink Nappy Toilet Drink Nappy Toilet Drink Nappy Toilet Drink Nappy Toilet Drink Nappy Toilet Time 5am Toilet Training for Children with Special Needs 3. Toileting Skills Assessment Bladder & Bowel Care Service Toilet Skills Assessment Childs Name: Initial assessment completed by: Date of Birth: Date of assessment: Date (a) Bladder Function – if bladder emptied 1 More than once per hour (Shade in area 1) 2 Between one - two hourly (Shade in areas 1 & 2) 3 More than two hourly (Shade in areas 1, 2 & 3) (b) Bowel Function – if 1 has frequent daily soiling (Shade in area 1) 2 Does not always have normal formed bowel movements is subject to constipation or diarrhoea (shade in area 2) 3 Has regular normally formed bowel movements (Shade in areas 1, 2 & Date 1 2 3 1 2 3 (c) If night time wetting occurs 1 Frequently – every night (Shade in area 1) 2 Occasionally – some dry nights (Shade in areas 1 & 2) 3 Never occurs (Shade in areas 1, 2 & 3) 1 2 3 (d) If night time bowel movements 1 Frequently - every night (Shade in area 1) 2 Occasionally – some clean nights (Shade in areas 1 & 2) 3 Never Occurs (Shade in areas 1, 2 & 3) 1 2 3 Independence (e) Sitting on the toilet 1 Afraid or refuses to sit toilet/potty (Shade in area 1) 2 Sits with help (Shade in areas 1 & 2) 3 Sits briefly without help (Shade in areas (1, 2 & 3) 4 Sits without help for long enough to complete voiding/evacuation of bowels (Shade in areas 1, 2, 3 & 4) 1 2 3 4 (f) Going to the toilet 1 Gives no indication of need to go to the toilet (Shade in area 1) 1 2 Gives some indication of need to go to the toilet (Shade in areas 1 & 2) 2 3 Sometimes goes to the toilet of own accord (Shade in areas 1, 2 & 3) 3 (g) Handling clothes at toilet 1 Cannot handle clothes at all (Shade in area 1) 2 Attempts or helps to pull down pants (Shade in areas 1 & 2) 3 Pulls pants down by self (Shade in areas 1, 2, & 3) 1 2 3 22 Date Toilet Training for Children with Special Needs 4 Pulls clothes up & down without help (Shade in areas 1, 2, 3 & 4) 4 other components (h) Bladder control 1 Never or rarely passes urine on toilet/potty (Shade in area 1) 2 Passes urine on toilet sometimes (Shade in areas 1 & 2) 3 Passes urine on toilet every time (Shade in areas 1, 2 &3) 4 Can initiate a void on request (Shade in areas 1, 2, 3 & 4) 1 2 3 4 (i) Bowel control 1 Never or rarely opens bowels on toilet/potty (Shade in area 1) 2 Opens bowels on toilet sometimes (Shade in areas 1 & 2) 3 Opens bowels on toilet every time (Shade in areas 1, 2 & 3) 1 2 3 (j) Behaviour problem that interferes with toileting process (e.g. screams when toileted) 1 Occurs frequently – once a day or more (Shade in area 1) 1 2 Occurs occasionally – less than once per day (Shade in areas 1 & 2) 3 Never occurs (Shade in areas 1, 2 & 3) 2 3 (k) Wears nappies, pull ups or similar 1 Yes (Shade in area 1) 2 No (Shade in areas 1 & 2) 1 2 (l ) Toilet If 1 Requires toileting aids or adaptations (Shade in area 1) 2 Uses normal toilet/potty (Shade in areas 1 & 2) 1 2 (m) Response to basic commands (e.g. sit down) 1 Never responds to commands (Shade in area 1) 2 Occasionally respond to commands (Shade in areas 1 & 2) 3 Always responds to commands (Shade in areas 1, 2 & 3) (n) Diet 1 Refuses/unable to eat fruit/vegetables (Shade in area 1) 2 Will occasionally eat fruit/vegetables each day areas 1 & 2) 3 eats adequate amounts daily e.g. age+5 =grams fibre) in areas 1, 2 & 3) 1 2 3 1 (Shade in 2 (Shade 3 (o) Fluid intake 1 Drinks poor amount - >50ml/kg per day (Shade in area 1) 1 2 Drinks 50ml/kg per day 4 – 5 drinks per day (Shade in areas 1 & 2) 3 Drinks 80ml/kg per day 6+ drinks per day (Shade in areas 1, 2 & 3) 2 3 23 Toilet Training for Children with Special Needs 4. Reassessment Checklist QuickTime™ and a decompressor are needed to see this picture. 24 Toilet Training for Children with Special Needs QuickTime™ and a decompressor eded to see this picture. 25 Toilet Training for Children with Special Needs 5. Examples of Individual Toileting Plans Peter’s Plan (pseudonym to maintain confidentiality) -From 02/12/13 Peter to wear a pair of pants inside his nappy for one week to get the sensation of feeling ‘wet’. School and home to take note of any signs that Peter makes indicating he feels wet. -The school will provide “wet” and “dry” symbols, pants and nappy symbols and a toilet routine visual to use at home and school. -From 09/12/13 Peter to wear washable pants not nappies AND: Be taken to the toilet every 1- 1 ½ hours Peter to sit on the toilet for 10 seconds initially and gradually increase the time and be encouraged to do a wee and/or open his bowels Peter is given a reward for example foamy soap to wash his hands with or a toy after sitting on the toilet or using the toilet. -Parents to request advice and support from teacher and school nurse when required. Nathan’s Plan (pseudonym to maintain confidentiality) Nathan will wear ‘washable pants’ or underwear whilst toilet training Every hour tell Nathan it is time to use the toilet and tell him to sit for up to a minute. Tell him where you are going and that he needs to ‘wee on the toilet’ Use the same language and words, for example ‘wee’, ‘toilet’ and ‘poo.’ Follow the same pattern each time Deal with accidents by saying to Nathan that he is ‘wet’ or ‘dirty’ and he needs to get changed in the toilet/bathroom straight away. (Feeling wet or dirty can desensitise a person to discomfort interfering with training efforts). Use record charts, stick these on the toilet wall Copy the chart onto the one in Nathan’s communication book at the end of the day. 26 Toilet Training for Children with Special Needs 6. Parents Questionnaire Toilet training presentation and workshop Parent feedback form Thank you very much for attending today’s toilet training presentation and workshop. We would value your feedback, and kindly ask for you to complete this questionnaire. Your feedback will enable us to develop these sessions further. 1) Was this session 1 2 3 Not very relevant relevant 2) 7 and 8 your 9 child? 10 Very 4 5 6 7 Just the right amount 8 9 10 Too much 3 4 5 6 7 8 9 10 Yes a Did you find the questions and answer session with the continence nurse useful? 1 2 Not really lot 5) 6 you Did the session help you develop your understanding of toilet training and give you practical tips to help? 1 2 Not really lot 4) 5 to Did the presentation have the right amount of information for you? 1 2 3 To little information information 3) 4 relevant 3 4 5 6 7 8 9 10 Yes a Would you 1 2 No 3 recommend 4 5 this 6 session 7 to 8 other 9 parents? 10 Yes Any other comments. 27 Toilet Training for Children with Special Needs 7. Toilet Training Feedback Analysis from staff - ERIC Toilet Training Including Children with Special Needs 11th June 2013 FEEDBACK ANALYSIS Out of the 40 delegates who attended this seminar 38 completed and returned their feedback questionnaires. All the percentages below have been calculated against the 38 responses. Q.1 The sessions were rated as follows: Session A – Healthy bladders & bowels No. 30 6 2 0 % 79 16 5 0 Option Very useful Useful Quite useful Not at all useful Session B - Skills required for toilet training No. 26 10 2 0 % 68 26 5 0 Option Very useful Useful Quite useful Not at all useful Session C – Why some children struggle with toilet training No. 19 17 2 0 % 50 45 5 0 Option Very useful Useful Quite useful Not at all useful Session D – Equipment & products No. 20 16 2 0 % 53 42 5 0 Option Very useful Useful Quite useful Not at all useful 28 Toilet Training for Children with Special Needs Session E – Developing toileting programs No. 16 21 1 0 % 42 55 3 0 Option Very useful Useful Quite useful Not at all useful Comments included: Q.2 Very interesting and useful training Very interesting with useful information Really useful. Answered all questions very well – everyone excited to put ideas into practice More information about overcoming struggles with toilet training/behavioural issues It would be useful to see some examples (real caseloads and challenging situations Very interesting Clear structure and practical strategies to support toilet training – well presented to cover a variety of diagnoses and needs Handout of resources – Books (available on slide show) More visual and examples Very informative but a times felt bombarded with information, probably good idea to have had a 15 min break not 5 for a chance to refresh More information on communicating with children Very good. Need a break half through though Excellent for our students! Fantastic presentation and info to use straight away Excellent training. Concise, informative with many useful ideas Would you like to receive ERIC catalogues to hand out to patients? No. 26 10 2 Q.3 % 68 26 5 Option Yes No Neither box ticked Do you inform parents about ERIC’s helpline and resources? No. 2 17 19 % 5 45 50 Option Yes No – but all said they would do from now on No comments 29 Toilet Training for Children with Special Needs Comments included: During school support groups, family support worker, medical team, class team Not personally as feel medical team would but will do so now This is all new but will pass info on to parents Didn’t know about it before 8. Literature search results for further reading National Institute for Health and Care Excellence CG99 Constipation in children and young people: NICE guidance Published 26/05/2010 National Institute for Health and Care Excellence CG128 Autism in children and young people: full guideline Published 28/09/2011 1. Title: A parent training model for toilet training children with autism. Citation: Journal of Intellectual Disability Research, 01 June 2010, vol./is. 54/Part 6(556-567), 09642633 Author(s): Kroeger K, Sorensen R Source: CINAHL 2. Title: Completion of toilet training in children with defecation disorders and concomitant symptoms of autism spectrum disorders Citation: Gastroenterology, May 2012, vol./is. 142/5 SUPPL. 1(S381), 00165085 (May 2012) Author(s): Peeters B., Benninga M.A., Noens I. Source: EMBASE 3. Title: A multidisciplinary functional toileting pathway for children with cerebral palsy: Preliminary analysis. Citation: Clinical Practice in Pediatric Psychology, March 2013, vol./is. 1/1(8188), 2169-4826;2169-4834 (Mar 2013) Author(s): Millard, Erin, Benore, Ethan, Mosher, Kathryn Source: PsycINFO 4. Title: Use of parent administered picture activity cards to teach toileting skills in children with autism Citation: European Child and Adolescent Psychiatry, July 2013, vol./is. 22/2 SUPPL. 1(S213-S214), 1018-8827 (July 2013) Author(s): Ramachandram S., Lope R.J.R., Chandran V., Nor N.K., Ismail J. 30 Toilet Training for Children with Special Needs Source: EMBASE 5. Title: Intensive behavioral treatment of urinary incontinence of children with autism spectrum disorders: An archival analysis of procedures and outcomes from an outpatient clinic Citation: Focus on Autism and Other Developmental Disabilities, March 2013, vol./is. 28/1(26-31), 1088-3576;1538-4829 (March 2013) Author(s): Hanney N.M., Jostad C.M., Leblanc L.A., Carr J.E., Castile A.J. Source: EMBASE 6. Title: Investigation of a reinforcement-based toilet training procedure for children with autism. Citation: Research in Developmental Disabilities, September 2002, vol./is. 23/5(319-31), 0891-4222;0891-4222 (2002 Sep-Oct) Author(s): Cicero FR, Pfadt A Source: MEDLINE 7. Title: Levels of continence in children with cerebral palsy. Citation: Paediatric Nursing, 01 May 2006, vol./is. 18/4(23-26), 09629513 Author(s): Singh BK, Masey H, Morton R Source: CINAHL 8. Title: Functional performance in children with Down syndrome. Citation: American Journal of Occupational Therapy, 01 November 2004, vol./is. 58/6(621-629), 02729490 Author(s): Dolva A, Coster W, Lilja M Source: CINAHL 9. Title: Behavioral intervention to eliminate socially mediated urinary incontinence in a child with autism. Citation: Child & Family Behavior Therapy, 01 December 2003, vol./is. 25/4(53-63), 07317107 Author(s): Riccciardi JN, Luiselli JK Source: CINAHL 10. Title: Continence in cerebral palsy. Citation: Health Visitor, 01 September 1990, vol./is. 63/9(301-302), 00179140 Author(s): Shaw J Source: CINAHL 11. Title: Systemic adverse events following botulinum toxin A therapy in children with cerebral palsy. Citation: Developmental Medicine & Child Neurology, 01 February 2010, vol./is. 52/2(139-144), 00121622 Author(s): Naidu K, Smith K, Sheedy M, Adair B, Yu X, Graham HK 31 Toilet Training for Children with Special Needs Source: CINAHL 12. Title: Safety of botulinum toxin type A among children with spasticity secondary to cerebral palsy: a systematic review of randomized clinical trials. Citation: Clinical Rehabilitation, 01 May 2009, vol./is. 23/5(394-407), 02692155 Author(s): Albavera-Hernández C, Rodríguez JM, Idrovo AJ Source: CINAHL 13. Title: Relationship of bladder dysfunction with upper urinary tract deterioration in cerebral palsy. Citation: Journal of pediatric urology, October 2013, vol./is. 9/5(659-64), 14775131;1873-4898 (2013 Oct) Author(s): Gundogdu G, Komur M, Avlan D, Sari FB, Delibas A, Tasdelen B, Nayci A, Okuyaz C Source: MEDLINE 14. Title: Autism spectrum disorders in children with functional defecation disorders. Citation: Journal of Pediatrics, September 2013, vol./is. 163/3(873-8), 00223476;1097-6833 (2013 Sep) Author(s): Peeters B, Noens I, Philips EM, Kuppens S, Benninga MA Source: MEDLINE 15. Title: Clinical and urodynamic spectrum of bladder function in cerebral palsy. Citation: Journal of Urology, October 2009, vol./is. 182/4 Suppl(1945-8), 00225347;1527-3792 (2009 Oct) Author(s): Richardson I, Palmer LS Source: MEDLINE 16. Title: Correlation between motor function and lower urinary tract dysfunction in patients with infantile cerebral palsy. Citation: Neurourology & Urodynamics, 2007, vol./is. 26/2(222-7), 07332467;0733-2467 (2007) Author(s): Bross S, Honeck P, Kwon ST, Badawi JK, Trojan L, Alken P Source: MEDLINE 17.Title: Voiding dysfunction and the Williams-Beuren syndrome: a clinical and urodynamic investigation. Citation: Journal of Urology, April 2006, vol./is. 175/4(1472-6), 00225347;0022-5347 (2006 Apr) Author(s): Sammour ZM, Gomes CM, Duarte RJ, Trigo-Rocha FE, Srougi M Source: MEDLINE 18.Title: Urodynamic findings in children with cerebral palsy. 32 Toilet Training for Children with Special Needs Citation: International Journal of Urology, August 2005, vol./is. 12/8(717-20), 0919-8172;0919-8172 (2005 Aug) Author(s): Karaman MI, Kaya C, Caskurlu T, Guney S, Ergenekon E Source: MEDLINE 19. Title: Behavioral problems in children with Down syndrome. Citation: Indian Pediatrics, July 2005, vol./is. 42/7(675-80), 0019-6061;00196061 (2005 Jul) Author(s): Bhatia MS, Kabra M, Sapra S Source: MEDLINE 20. Title: Functional performance in children with Down syndrome. Citation: American Journal of Occupational Therapy, November 2004, vol./is. 58/6(621-9), 0272-9490;0272-9490 (2004 Nov-Dec) Author(s): Dolva AS, Coster W, Lilja M Source: MEDLINE 21. Title: Development of bladder control in children and adolescents with cerebral palsy. Citation: Developmental Medicine & Child Neurology, February 2001, vol./is. 43/2(103-7), 0012-1622;0012-1622 (2001 Feb) Author(s): Roijen LE, Postema K, Limbeek VJ, Kuppevelt VH Source: MEDLINE 22. Title: Urologic health in children with down syndrome Citation: Journal of Urology, April 2013, vol./is. 189/4 SUPPL. 1(e75-e76), 0022-5347 (April 2013) Author(s): Brown E., Hogan R., Zhang J., Dinh K., Langston S., Roth C. Source: EMBASE 23.Title: Autism spectrum disorders and autism spectrum symptoms in children with functional defecation disorders Citation: Journal of Pediatric Gastroenterology and Nutrition, June 2011, vol./is. 52/(E97-E98), 0277-2116 (June 2011) Author(s): Peeters B., Benninga M.A., Loots C.M., Van Der Pol R.J., Burgers R.E., Philips E.M., Wepster B.W., Tabbers M.M., Noens I.L. Source: EMBASE 24. Title: Psychological differences between children with and without soiling problems Citation: Pediatrics, May 2006, vol./is. 117/5(1575-1584), 0031-4005;02105721 (May 2006) Author(s): Joinson C., Heron J., Butler U., Von Gontard A. Source: EMBASE 33