lokal otojen osteokondral greft uygulamalari: köpeklerde di̇z
advertisement

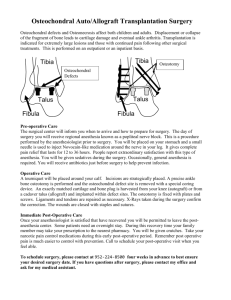
Doğu Anadolu Bölgesi Araştırmaları; 2008 Ali Said DURMUŞ, Yesari ERÖKSÜZ *LOCAL AUTOGENOUS OSTEOCHONDRAL GRAFT APPLICATIONS: AN EXPERIMENTAL STUDY IN DOGS KNEE JOINTS *Ali Said DURMUŞ, **Yesari ERÖKSÜZ *Firat University, Veterinary Faculty, Surgery Department– ELAZIG **Firat University, Veterinary Faculty, Pathology Department– ELAZIG __________________________________________________________________________________________________________________________________________________ ABSTRACT The aim of this study was to investigate applicability of local autogenous osteochondral grafts for the repairment of osteochondral defects in knee joints of dogs. The material consisted of 18 healthy adult mongrel dogs. Osteochondral defects in standard cylindrical shape (0.5 cm x 0.5 cm) were created on both lateral and medial femoral condyles.The defects were filled with autogenous osteochondral grafts harvested from upper surface of lateral and medial labium of femoral trochlea in treatment group (9 dogs). Nine dogs were kept as control group. Clinical and radiographical evaluations were carried out at the 15 days intervals. Histopathological examinations were carried out at the 15th, 30th and 60th days in each group. Consequently, the results indicated that autogenous osteochondral grafts harvested from upper surface of lateral and medial labium of femoral trochlea could be applied in treatment of osteochondral defects in knee joints of dogs. Keywords: Autogenous Osteochondral Graft, Dog. __________________________________________________________________________________________________________________________________________________ LOKAL OTOJEN OSTEOKONDRAL GREFT UYGULAMALARI: KÖPEKLERDE DİZ EKLEMİNDE DENEYSEL ÇALIŞMA ÖZET Yapılan bu çalışmanın amacı köpeklerde diz eklemindeki osteokondral defektlerin onarımında lokal otojen osteokondral greftlerin uygulanabilirliğini araştırmaktı. Çalışmada 18 adet sağlıklı, yetişkin melez köpek kullanıldı. Osteokondral defektler, standart silindir biçiminde (0.5 cm x 0.5 cm) femurun lateral ve medial kondyluslarının her ikisinde de oluşturuldu. Oluşturulan defektler 9 köpekte (tedavi grubu) femoral trochlea’nın lateral ve medial kısımlarının üst yüzeylerinden elde edilen otojen osteokondral greftlerle dolduruldu. Dokuz köpek ise kontrol grubu olarak tutuldular. Klinik ve radyolojik kontroller 15 gün aralıklarla gerçekleştirildi. Histopatolojik kontroller ise 15, 30 ve 60. günlerde gerçekleştirildi. Sonuç olarak, bulgular köpeklerin diz eklemindeki osteokondral defektlerin, lateral ve medial femoral trochlea’nın üst kısımlarından elde edilen otojen osteokondral greftlerle sağaltımlarının gerçekleştirilebileceğini göstermiştir. Anahtar Kelimeler: Otojen Osteokondral Greft, Köpek. *II. Ulusal Küçük Hayvan Hekimliği Kongresi'nde (10-13 Nisan 2003, Bursa) Sözlü Bildiri Olarak Sunulmuştur. __________________________________________________________________________________________________________________________________________________ 1. INTRODUCTION Articular cartilage is a unique tissue with a limited ability to respond to injury (Karataglis et al., 2006; Yaylaoğlu et al., 1999). Mature articular cartilage has minimal regenerative ability owing to its intrinsic properties, such as low chondrocyte mitotic rate and numbers (Hangody et al., 1997; 2008; Mahadev et al., 2001). It has been generally accepted that cartilage defects cannot be repaired by the chondrocytes adjecant to the lesion. However when the defect reaches the subchondral bone, repair is initiated by “creeping substition” similar to that of bone healing (Yaylaoğlu et al., 1999). Several materials, including autogenous (Marcacci et al., 1999; Sammarco and Makwana, 2002), fresh or conserved osteochondral grafts (Desjardins et al., 1991; Hurtig, 1988), autogenous osteochondral grafts harvested ribs (Oka and Ikeda, 2001), sternum (Stover et al., 1989), lateral trochlear rim of talus (Huber et al., 1992), autogenous cartilage grafts harvested sternum (Vachon et al., 1992), autolog condrocyte transplantation (Yıldız et al., 2001), and autogenous periosteal grafts (Vachon et al., 1991) were used for reconstruction of osteochondral defects. 72 Doğu Anadolu Bölgesi Araştırmaları; 2008 Ali Said DURMUŞ, Yesari ERÖKSÜZ Autogenous osteochondral graft has gained in clinical popularity because of its technical feasibility and cost effectiveness. However only a few series have been reported in the literature, many of them are case reports (Dew and Martin, 1991; 1992; Hangody et al., 1997; 2008; Karataglis et al., 2006). recipient sites by press-fit technique in treatment group (9 dogs) (Figure 2). Special attention was paid to avoid fracture or breakage of the osteochondral plugs during the course of transplantation. Nine dogs were kept as control group. The purpose of this study was to investigate applicability of local autogenous osteochondral grafts harvested from upper surface of lateral and medial labium of femoral trochlea for the repairment of osteochondral defects and evaluate the incorporation of autogenous osteochondral graft in osteochondral defects in knee joint of dogs. 2. MATERIAL AND METHODS Animal experiments were conducted in the Animal Hospital of Veterinary Faculty of the Firat University of Turkey in accordance with usual guidelines. Eighteen adult mongrel female clinically healthy dogs aged between 2 and 4-y-old (mean 3-yold) were used in this study. General anaesthesia was induced in animals by intramuscular administration of Xylazine hydrochloride 3 mg/kg (Rompun, Bayer, 23.32 mg/ml), and ketamine hydrochlorur 15 mg/kg (Ketalar, Parke-Davis, 50 mg/ml). Dogs were divided into two equal groups. Figure 2. Autogenous osteochondral plugs were transplanted into the defect in condylus by press-fit technique. Operation wounds were closed in a routine manner (Piermattei and Greeley, 1979). The related limbs were supported with a bandage reinforced by plastic casts, and the bandages were kept for two weeks by renewing every week. Postoperative medications included procaine peniciline G (22.000 IU/kg, IM, q 12 h) administered for 5 days. Skin sutures were removed 10 days after the surgery. Clinical and radiographical evaluations were carried out at 15 days intervals. Three dogs in each group were sacrificed by overdose sodium penthobarbital at 15th, 30th, and 30th days. At postmortem, the articular surfaces were evaluated for color, homogenity, and amount and demarcation of repair tissue. Each speciemen, a block consisting of repair area and surrounding tissues, was bisected centrally through the defect. The samples was fixed in 10% neutral buffered formalin for 5 days and decalcifed in a decalcification solution (15 ml HNO3+10 ml 10% neutral buffered formalin+85 ml distilled water). The samples were cut into 5 µm sections after complete decalcification and stained with Hematoxylin and Eosin (H&E) and examined by light microscopy. Figure 1. Autogenous osteochondral plugs were harvested from the upper surface of lateral labium of femoral trochlea. Surgically, the knee joints was exposed using lateral parapatellar approach as reported by Piermattei and Greeley (1979). Osteochondral defects in standard cylindrical shape (0.5 cm x 0.5 cm) were created on both lateral and medial femoral condyles. Then autogenous osteochondral plugs of the same length were harvested from the upper surface of lateral and medial labium of femoral trochlea (Figure 1), and were transplanted into the 3. RESULTS In this study, clinical, radiographical and histopathological results were evaluated at the 15th, 30th, and 60th days postoperation. Clinical examinations showed the occurrence of lameness in all cases at the 15th day of experi73 Doğu Anadolu Bölgesi Araştırmaları; 2008 Ali Said DURMUŞ, Yesari ERÖKSÜZ ment. Whereas, lameness was completely resolved, and the joints were stabilized and there were not limitation of movement, crepitation and muscular atrophy in the further examination. Radiographical examinations indicated that grafted regions were determined slightly after surgery (Figure 3). Periarticular tissue thickness and articular space width were in normal ranges, and incorporation of grafts was completely fulfilling in the treatment group at the 60th day postoperation (Figure 4). The fulfilling of defects continued in the course of time but could not completed in the control group (Figure 5, Figure 6). Figure 5. Radiographic appearence of a case of the control group after surgery. Figure 3. Radiographic appearence of a case of the treatment group after surgery. Figure 6. Radiographic appearence of the former case at postoperative 60th day. Macroscopical evaluations revealed that the grafts determined surrounding tissue at the 15th day, morphologic zones could not be discerned, the grafted defects had healed with congruent, smooth and intact surfaces at the 30th day. The grafted defects had healed with congruent and smooth surfaces of the same colour and texture as the adjacent normal cartilage at the 60th day of postoperation. All ungrafted defects had irregularity in the femoral condyle. Histopathologic evaluations, at the 15th day of postoperation, revealed that graft was alive and regenerative attempts were initated in osseous and cartilaginous components in treatment group (Figure 7). At 30th and 60th days of postoperation, reperation Figure 4. Radiographic appearence of the former case at postoperative 60th day. 74 Doğu Anadolu Bölgesi Araştırmaları; 2008 Ali Said DURMUŞ, Yesari ERÖKSÜZ in osseous component of graft was not completed, and cartilaginous component of the graft included fibrous cartilago (Figure 8). Eburnation and synovial membrane proliferation were detected as the main complications in all the control group animals. 1993). The goal was to penetrate the subchondral zone of vascularization within the cartilage defect, allowing a conduit and site for clot formation containing mesenchymal stem cells capable of forming fibrocartilage repair tissue. In this study, the model of defect and methods were the same as reported by other investigators (Delcogliano et al., 2002; Kold and Hickman, 1986; Marcacci et al., 1999; Yıldız et al., 2001). Osteochondral grafting or mosaicloplasty is a technique in which dowels of bone and cartilage are taken from a non weight-bearing portion of the femoral trochlea or condyle and press-fit into a recipient hole made by removing the cartilage defect with its underlying bone (Delcogliano et al., 2002; Marcacci et al., 1999). In this study, we preferenced osteochondral grafts harvested from the upper surface of lateral and medial labium of femoral trochlea, non weight-bearings portion in the knee joint to eliminate to donor site morbidity. In addition, donor region is neighborhood to the lesion, and required no second operation and additional anaesthesia for harvesting of osteochondral grafts. Figure 7. Histopathologic appearence of a case of the treatment group at postoperative 15th day. N: Normal cartilage, G: Grafted cartilage, R: Resorbed bone, K: Callus. (H.E.x 40). In this study, a bandage reinforced by plastic casts was placed on the releated limb for 15 days the same as reported by Fallon (1990). This application was useful for success of the treatment. Some investigators (Desjardins et al., 1991; Hurtig et al., 1988; 2001; Oka and Ikeda, 2001; Scranton and McDermott, 2001; Stevenson, 1986; Sullins et al., 1989; Vachon et al., 1991), reported that postoperatively the knee is often painful when the dog walked. In this study, lameness was observed in all dogs in the first 15 days, but it was completely resolved later examination. It is reported that crepitus (Fallon, 1990), and limitation of movement (Dew and Martin, 1992; Howard et al., 1994; McIIwraith et al., 1994) may be present in the patients with osteochondral lesions. In this study, there were not crepitus, muscular atrophy, and limitation of motion of the knee. This results indicated that this treatment method was successful clinically. Radiology is essential for an early diagnosis (Fallon, 1990). Definitive diagnosis is made by radiographic examination of the affected joint (Manley et al., 1990). A standard craniocaudal view usually shows an irregularity in the countour of the femoral condyle. The medial aspect of the lateral condyle is most often affected; the lesion appears as a radiolucent concave defect with sclerotic margins (Fallon, 1990). In the present study, periarticular tissue thickness, joint space, and osteophyte formation evaluated radiographically, and results of the treatment group was satisfactory to control group as reported by Dew and Martin (1991;1992). Figure 8. Histopathologic appearence of a case of the treatment group in postoperative 60th day. R: Resorbed bone, K: Cartilage. (H.E.x 40). 4. DISCUSSION Focal chondral defects of the articular surface of the knee are a complex clinical problem because of the inability of articular cartilage to initiate any clinically appreciable healing response. When indicated, treatment should ideally prevent defect progression, reduce symptoms and restore function. Indications to proceed with options considered palliative, reparative, or restorative are evolving. Although biological resurfacing of a partially damaged joint surface is clinically desirable, it is difficult to achieve consistent and lasting results. Repair of large osteochondral defects, larger than 3 mm in diameter and 3 mm deep, must include support of the bone as well as the articular surface tissue (Shahgaldi, 1998; Messner and Gillquist, 75 Doğu Anadolu Bölgesi Araştırmaları; 2008 Ali Said DURMUŞ, Yesari ERÖKSÜZ In this study, histopathologically, local autogenous osteochondral grafts was useful in osteochondral defects due to grafts was alive and regenerative and reparative attempts were observed in treatment group. In contrast, eburnation and synovial membran proliferation were observed in control group. Consequently, it was indicated that autogenous osteochondral grafts harvested from upper surface of lateral and medial labium of femoral trochlea could be applied in treatment of osteochondral defects in knee joints of dogs. 5. REFERENCES 1. 2. 3. 4. 5. 6. 7. 8. 9. Delcogliano A., Caporaso A., Menghi A., Rinonapoli G. and Chiossi S. 2002. Results of autologous osteochondral grafts in chondral lesions of the knee. Minerva Chirurgica, 57: 273-281. Desjardins M.R., Hurtig M.B., Palmer N.C. 1991. Incorporation of fresh and cryopreserved bone in osteochondral autografts in the horse. Vet. Surg., 20: 446-452. Dew T.L., Martin R.A. 1992. Functional, radiographic, and histologic assessment of healing of autogenous osteochondral grafts and full-thickness cartilage defects in the talus of dogs. Am. J. Vet. Res., 53: 2141-2152. Dew T.L., Martin R.A. 1991. The functional, radiographic and histologic comparison of an autogenous orthotopic osteochondral graft and a full-thickness cartilage defect in the canine talus. Vet. Surg., 20: 334. 10. Hurtig M. Pearce S., Warren S., Kalra M., Miniaci A. 2001. Arthroscopic Mosaic Arthroplasty in the Equine Third Carpal Bone. Vet. Surg., 30: 228-239. 11. Hurtig M.B. 1988. Experimental use of small osteochondral grafts for resurfacing the equine third carpal bone. Equine Vet. J., Suppl, 6: 2327. 12. Karataglis D., Green M.A., Learmonth D.J.A. 2006. Autologous osteochondral transplantation for the treatment of chondral defects of the knee. Knee, 13 : 32-35. 13. Kold S.E., Hickman J. 1986. An experimental study of the healing process of equine chondral and osteochondral defects. Equine Vet. J., 18: 18-24. 14. Mahadev A., Mahara D.P., Chang P., Mitra A.K., Tay B.K., Sim C.S. 2001. Autogenous osteochondral morselised grafts for full thickness osteochondral defects in the knee joints of pigs. Singapore Med. J., 42: 410-416. Fallon K.R. 1990. Osteochondritis Dissecans of the Stiffle. In: M.J. Bojrab (ed.): Current Techniques in Small Animal Surgery, Third Ed. Lea & Febiger, Philadelphia, 721-722. 15. Manley P.A., Howard P.E., Constantinescu G.M. 1990. Surgery for Osteochondrosis of the Canine Shoulder. In: M.J. Bojrab (ed):, Current Techniques in Small Animal Surgery, Third Ed. Lea & Febiger, Philadelphia, 749-756. Hangody L., Kish G., Kárpáti Z., Szerb I., Udvarhelyi I. 1997. Arthroscopic autogenous osteochondral mosaicplasty for the treatment of femoral condylar articular defects. A preliminary report. Knee Surg. Sport Tr. A., 5: 262-267. 16. Marcacci M., Kon E., Zaffagnini S., Visani A. 1999. Use of autologous grafts for reconstruction of osteochondral defects of the knee. Orthopedics, 22: 595-600. Hangody L., Vásárhelyi G., Hangody L. R., Sükösd Z., Tibay G., Bartha L., Bodó G. 2008. Autologous osteochondral grafting-technique and long-term results. Injury, 39, Suppl.1:3239. 17. McIlwraith C.W., Howard R.D., Trotter G.W., Powers B.E., McFadden P.R, Harwood F.L., Amiel D. 1994. Sternal cartilage autografts for repair of large osteochondral defects in horses: long-term fate and effects of exercise. Vet. Comp. Orthopaed., 7: 63-64. 18. Messner K., Gillquist J. 1993. Synthetic implant for the repair of osteochondral defects of the medial femoral condyle. Biomaterials, 14: 513-521. 19. Oka Y., Ikeda M. 2001. Treatment of severe osteochondritis dissecans of the elbow using osteochondral grafts from a rib. J. Bone Joint Surg. Br., 83: 738-739. 20. Piermattei D.L., Greeley R.G. 1979. An Atlas of Surgical Approaches to the Bones of the Dog Howard R.D., McIlwraith C.W., Trotter G.W., Powers B.E., Mcfadden P.R, Harwood F.L., Amiel D. 1994. Long-term fate and effects of exercise on sternal cartilage autografts used for repair of large osteochondral defects in horses. Am. J. Vet. Res., 55: 1158-1167. Huber M.J., Schmotzer W.B., Riebold T.W., Watrous B.J., Synder S.P., Scott E.A., Matthiessen P.C., Von-Matthiessen P.C. 1992. Fate and effects of autogenous osteochondral fragments implanted in the middle carpal joint of horses. Am. J. Vet. Res., 53: 1579-1588. 76 Doğu Anadolu Bölgesi Araştırmaları; 2008 Ali Said DURMUŞ, Yesari ERÖKSÜZ 26. Sullins K.E., Veıt H.P., McIlwraith C.W. 1989. Osteochondral grafts to fill large articular defects in horses. Vet. Surg., 18: 77. 27. Vachon A.M., McIlwraith C.W., Powers B.E., McFadden P.R., Amiel D. 1992. Morphologic and biochemical study of sternal cartilage autografts for resurfacing induced osteochondral defects in horses. Am. J. Vet. Res., 53: 1038-1047. and Cat, 202 pages, WB Saunders Company, Philadelphia. 21. Sammarco G.J., Makwana N.K. 2002. Treatment of talar osteochondral lesions using local osteochondral graft. Foot Ankle Int., 23: 693-698. 22. Scranton P.E., McDermott J.E. 2001. Treatment of type v osteochondral lesions of the talus with ipsilateral knee osteochondral autografts. Foot Ankle Int., 22: 380-384. 28. Vachon A.M., McIlwraith C.W., Trotter G.W., Norrdin R.W., Powers B.E. 1991. Morphologic study of induced osteochondral defects of the distal portion of the radial carpal bone in horses by use of glued periosteal autografts. Am. J. Vet. Res., 52: 317-327. 23. Shahgaldi B.F. 1998. Coral graft restoration of osteochondral defects. Biomaterials, 19: 205213. 24. Stevenson S. 1986. Histomorphometric analysis of massive osteochondral allografts in dogs. Vet. Surg., 15. 135. 29. Yaylaoğlu M.B., Yıldız C., Korkusuz F., Hasırcı V. 1999. A novel osteochondral implant. Biomaterials, 20: 1513-1520. 25. Stover S.M., Pool R.R., Lloyd K.C.K. 1989. Repair of surgically created osteochondral defects with autogenous sternal osteochondral grafts in the horse. Vet. Surg., 18: 76-77. 30. Yıldız C., Bahçe M., Deveci S., Bilgili H., İde T., Tunay S., Başbozkurt M., Gür E. 2001. Autolog condrocyte transplantation (an experimental study in rabbit knee joints). Artroplasti Artroskopik Cerrahi, 12: 75-82. 77