To test the hypothesis that CD25 expressing memory B cells are a
advertisement

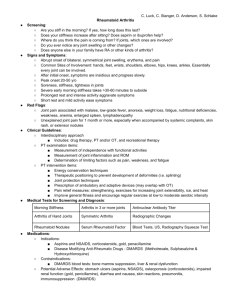
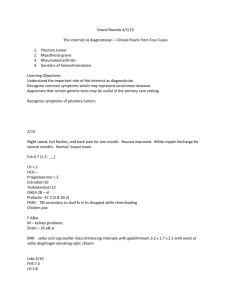
Mikael Brisslert (740528-5136) Research program 1 The role of B-lymphocytes and the newly discovered CD25+ Blymphocyte in the pathogenesis of rheumatoid arthritis The overall goal of this project is to define the importance of B-lymphocytes in the pathogenesis of rheumatoid arthritis with emphasis on a newly discovered CD25+ B cell subset. SPECIFIC AIMS: Rheumatoid arthritis (RA) is characterized by infiltration and proliferation of inflammatory cells in joints. B-lymphocytes are present in joints of RA patients and recent studies show that treatment with rituximab (a drug that gets rid of B cells) improves disease phenotypes. These data implicate B cells as drivers in the pathogenesis of RA. However, the precise role of B cells in RA is unclear. It is also unclear why RA patients undergoing B cell depletion therapy with rituximab are still responsive to vaccinations. B cell depletion is a very crude therapy and it would be highly desirable to identify which B cell subsets are involved in RA so that more specific therapies can be designed. We have earlier identified a new B cell subset expressing the cell surface marker CD25. These CD25+ B cells seem to be part of a hitherto unknown B cell memory population. In this project we will define the importance of B cells in general, and CD25+ B cells in particular, for the pathogenesis of RA and also their role in acquired immune responses. To accomplish this we will use a unique and well-characterized patient material that includes bone marrow (BM), synovial fluid and blood. Importantly, this material is collected at different time points – at diagnosis and before, under and after B cell depletion therapy – making it possible to define spatial and temporal regulation of B cell subsets. Our specific aims are: Specific aim 1: To define the ontogeny of B cells and CD25+ B cells by analyzing BM, blood and synovial fluid from RA patients during B cell depletion therapy. Specific aim 2: To test the hypothesis that B cell depletion therapy in RA patients will impair the response of B cells and CD25+ B cells to protein and carbohydrate antigens in vivo and in vitro. Specific aim 3: To test the hypothesis that CD25+ B cells contribute to the pathogenesis of RA by differentiating into plasma cells that secrete autoreactive antibodies recognizing antigens in the joint. Specific aim 4: To generate mice lacking the CD25+ B cell subset and assess their response to immunisations, bacterial infections and arthritis. BACKGROUND B cells are important mediators of rheumatoid arthritis development RA is an autoimmune disease affecting 1% of our population. RA is more common in women and is characterized by inflammation and joint destruction. The disease increases comorbidity and mortality [1] and comes with enormous economic and health consequences to society. The demand for new therapies to treat RA is urgent. In the past, RA was believed to be mediated by T cells and macrophages, but recently, B cells have come in focus as key mediators of RA [1]. Indeed, it is now believed that B cells play an important role in the initiation as well as maintenance of RA via antigen presentation and production of cytokines and autoreactive antibodies. The autoreactive antibodies such as rheumatoid factor and antibodies recognizing citrullinated peptides and collagen type II are thought to directly contribute to the pathogenesis of RA. In addition, B cells migrate to a zone of the joint where the synovial membrane connects with the cortical bone and there they mount an inflammatory response that leads to pannus formation and cartilage and bone destruction. Mikael Brisslert (740528-5136) Research program 2 B cells may also contribute to the pathogenesis of RA by presenting antigens to autoreactive T cells, secrete chemokines that induce leukocyte infiltration, and produce factors that initiate and sustain angiogenesis and granulation tissue formation. Very little is known about which subsets of B cells contribute to the different pathogenic processes in RA. Subsets of B cells are defined by distinct expression of cell surface markers B cells produce antibodies, secrete cytokines and chemokines, and present antigens [3-6]. B cells develop in the BM, enter the blood stream and end up in immunocompetent sites in the body. B cells are found at different maturation stages depending on where in the body they are located [naïve B cells (BM, circulation), memory B cells (synovial and other peripheral tissues), plasma cells (BM and circulation)] [3-6]. There are several different subtypes within each of the different B cell populations. Presently the different subsets are defined with respect to their expression of cell surface antigens (Table 1). We have recently defined a new B cell subset that expresses CD25, which at least in humans, appears to belong to the B cell memory compartment. CD25 is a part of a receptor complex that binds interleukin 2 (IL-2). When CD25 interacts with the complex the receptor undergoes a conformational change resulting in a high affinity for IL-2. In B cells IL-2 induces proliferation. CD25 and IL-2 may be important in RA: the levels of IL-2 in the joint and in the circulation of RA patients are very high. The CD25+ B cells differ substantially from their CD25– counterparts [7]. For example, we have shown that CD25+ B cells are better at presenting antigens than CD25– cells. Based on this finding we have hypothesized that antigen presentation by B cells might be mediated by CD25, in addition to MHC class II. Along those lines, inhibition of CD25 on these B cells abolished antigen-induced T cell responses [7]. In physiological conditions CD25+ B cells secrete lower levels of immunoglobulins compared to CD25– B cells. Phenotypically, CD25+ B cells display a mature memory phenotype with increased expression of IgG and IgA, the memory marker CD27, and the costimulatory molecules CD80 and CD86 [7, 8]. A clinical study on RA and systemic lupus erymatosus patients (SLE; another autoimmune disorder) showed that CD25+ B cells display a more activated and mature phenotype than cells from healthy controls [9]. To understand the ontogeny and function of the CD25+ subset we have also analyzed mice. During B cell development in mice CD25 is expressed on pre-B cells in the bone marrow [10]. We have also identified CD25+ B cells in secondary lymphoid organs (spleen 1%, lymph nodes 2%, peritoneal cavity 16 %) [11] but not in blood or Peyer’s patches. Our phenotypic analyses show that CD25+ B cells displayed a more mature and activated phenotype compared to the CD25– B cells [11]. It will now be important to define the role of CD25+ B cells in the development of autoimmune diseases in mice. In this project, we will address this issue. Table 1: B cell subsets in humans Subset Surface expression Pre-B cells (in BM) CD19+, CD20+ IgD–, CD38++, CD24++ Transitional, T1 (in BM) CD19+, CD20+, IgD+/–, CD38+, CD24+ Mature Bm2 (in BM) CD19+, CD20+, IgD+, IgM++, CD27–, CD38+, CD24+/– Naïve B cells CD19+, CD20+, IgD–, CD27-, CD38+++ Mature B cells CD19+, CD20+, IgD+, IgM+, CD27-, CD38++ Memory B cells* CD19+, CD20+, IgD–, IgM+, IgA+ or IgG+, CD27+, CD38+ Plasma blasts CD19+/–, CD20–, IgD–, IgM+, IgA+ or IgG+, CD27+, CD38+++ Plasma cells CD19–, CD20–, Ig–, CD27–, CD38+++, CD138+ * Our hypothesis is that the CD25+ B cells is a subset of the memory B cell fraction Mikael Brisslert (740528-5136) Research program 3 B cell depletion therapy can help patients with autoimmune diseases A monoclonal antibody (such as rituximab) that recognizes the B cell surface molecule CD20 results in depletion of B cells. In a mouse model of RA (mice engrafted with synovial tissue from RA patients) treatment with anti-CD20 antibodies resulted in a total dissociation of Bcell follicular structures of the implanted synovial tissue [12]. Also, circulating levels of the inflammatory cytokines IL-1 and interferon gamma (IFN-) were reduced dramatically suggesting that B cells have profound effects on T-cell differentiation in the implant. RA patients are now successfully treated with anti-CD20 antibodies that deplete B cells [1316]. The depletion of B cells in RA patients results in a remarkably decreased disease activity and increased quality-of-life [17, 18]. However, we don’t yet know why they are getting better! Neither do we know which B cell subsets are responsible for the reduced disease phenotypes. Several studies have examined the repopulation pattern of B cells that occur at different time points after depletion therapy [19-21]. None of them have thoroughly investigated the effect of anti-CD20 on the BM B cell population [22]. This compartment is important since this is a place of B cell formation and of plasma cells receding. Therefore it will be essential to clarify how B cells regulate disease activity, and how the different B cell subsets, and in particular CD25+ B cells, contribute in this process, and how the immune response is affected after B cell depletion therapy. In this way, we could direct the therapy to a specific B cell subset and limit the sometimes severe side effects associated with rituximab therapy (i.e., immunosuppression and severe bacterial and viral infections). MATERIAL AND METHODS Patient description Inclusion criteria Diagnosis RA according to the standard ACR-criteria [26]. Both RF+ and RF– as well as antiCCP+ and anti-CCP– patients Patient population Patients with established therapy-resistant RA Sex Material will be recruited according to a ratio of 1:3 (male:female) as disease prevalence is distributed in our population. Previous treatment Metotrexate is a requirement, however combinations of DMARDs and Metotrexate are allowed. For the depletion studies, a history of anti-TNF-failure is required. Exclusion criteria Infections, Malignancies, Pregnancy Laboratory analyses All included patients will be monitored according standard procedures at the Rheumatologic clinic at Sahlgrenska University Hospital Control groups RA patients treated with metotrexate monotherapy Healthy subjects recruited from the blood donor central RF, rheumatoid factor; anti-CCP, antbodies to citrullinated peptides; DMARD, disease modifying anti-rheumatic drugs Experimental setup RA patients will be recruited and asked to donate blood and BM, before, during and after rituximab treatment for evaluation of the effect on the B cell population and the effect on the ability to mount an immune response following immunization. Mikael Brisslert (740528-5136) Research program 4 WORK PLAN Specific aim 1: To define the ontogeny of B cells and CD25+ B cells by analyzing BM, blood and synovial fluid from RA patients during B cell depletion therapy. In peripheral blood, BM and synovial fluids from RA patients receiving/received B cell depletion therapy the B cell phenotype and B cell subsets will be analysed using flow cytometry. Samples will be collected at different time points (day 0, +1 month, +3 months as well as before second treatment (see experimental setup depletion study)) to follow the changes in the B cell compartment. We will use monoclonal antibodies revealing maturation stages, activity, and immunoglobulin repertoire (i.e. CD19 for B cells in combination with IgA, IgM, IgD, IgG, CD10, CD24, CD25, CD27, CD38, CD71, CD80, CD86, CD95, CD138, BAFF-R and TACI). Preliminary data suggest, that one and three months following rituximab treatment, BM retained up to 30% of B cells while peripheral blood was depleted of B cells. Analysis of the remaining BM B cells indicated a prevalence of immature pre-B (CD38++CD24++) and CD27+IgD- memory cells. IgD+ cells were depleted (Figure 1). A significant reduction of CD27+ cells in BM and in peripheral blood was observed long after anti-CD20 treatment (mean 22 months) (p=0.003). Naive B cells were the dominant population in the BM (p=0.02) and circulation (p=0.003). Figure 1: FACS analysis of the BM B cell phenotype in RA patients following short-term or long-term rituximab treatment. Lower left quadrant in each plot represents immature B cells (IgD -CD27-), lower right quadrant represents naïve B cells (IgD+CD27-), and upper right quadrant represents unswitched memory B cells (IgD+CD27+). The upper left quadrant represents switched memory B cells (IgD-CD27+). A) Rituximab naïve Mikael Brisslert (740528-5136) Research program 5 patient is shown at day 0, 1 month and 3 months following treatment. B) Rituximab-treated patient is shown at day 0, 1 month and 3 months following 2 nd treatment. Arrow indicates population that was found to be depleted during rituximab treatment. Expected outcome: We believe we will be able to demonstrate a B cell subset that escapes rituximab depletion even though they express CD20 and that this population will be CD25 positive. Regardless of CD25 status, we would next analyse the T cell population and the cross talk between B- and T cells that might be of importance for activation of autoreactive B and T cells during RA. Specific aim 2: To test the hypothesis that B cell depletion therapy in RA patients will impair the response of B cells and CD25+ B cells to protein and carbohydrate antigens in vivo and in vitro. RA patients will be immunized with carbohydrate and protein vaccines (Pneumo23, SanofiPasteur MSD and Afluria, ZLB Pharma GmbH) at different time points before or after B cell depletion. Blood and BM will be collected and analysed for antigen-specific antibody secreting cells using ELISPOT. In addition, the phenotypic properties of CD25+ B cells will be analysed using flow cytometry and the same panel of surface markers described in Specific Aim 1. Preliminary data indicates that 6 days after vaccination, 9 of 10 rituximab-treated patients and 13 of 13 methotrexate-treated patients had B cells producing influenza specific antibodies. The number of cells producing influenza specific IgM and IgG was significantly lower in rituximab-treated patients as compared to those treated with methotrexate (p=0.009, and 0.02). Pneumococcal polysaccharide–specific responses developed in 2 of 10 rituximabtreated patients compared to 12 of 13 of the methotrexate-treated. No significant differences were observed between the groups with respect to immunoglobulin secretion in response to Pneumococcal polysaccharides. Expected outcome: We predict that B-cells in rituximab-treated RA patients will exhibit reduced ability to mount a proper immune response following vaccination. In the unlikely event that immune responses to vaccination is normal that would suggest that vaccine induced B cells already in the lymph nodes down regulate CD20 expression and therefore are insensitive to treatment on their way to the bone marrow. If the preliminary data hold up in extended analyses, we will define the optimal time for vaccination of RA patients prior to rituximab treatment. We will also delineate how it is possible to establish an immune response with no circulating B cells (or with only a small subset of B cells). Specific aim 3: To test the hypothesis that CD25+ B cells contribute to the pathogenesis of RA by differentiating into plasma cells that secrete autoreactive antibodies recognizing antigens in the joint. Blood, BM and synovial fluid from RA patients and blood from healthy controls will be sorted (Figure 2) into CD25+ and CD25– B cells and cultured at defined conditions that promotes differentiation into plasma cells. Immunoglobulin production from differentiated cells will be analysed using ELISPOT, and the phenotype will be determined using a fivecolour flow cytometry panel including antibodies recognizing CD20, CD27, IgD, CD38 and CD138. Since increased numbers of B cells are found in the joints of RA patients we will compare the migration and the expression of homing receptors on CD25 + and CD25– B cells. Migration studies will be performed using a Transwell-system [11, 27, 28]. During maturation of B cells into plasma cells, immunoglobulin genes undergo somatic hypermutations. We will analyze mutations in these genes in maturating CD25+ and CD25– B cells in collaboration with Prof. Thomas Dörner (Berlin, Germany). Preliminary data suggests that CD25+ B cells more efficiently differentiate into plasma cells compared to CD25– B cells as judged by ELISPOT and surface marker analysis. This was shown by an increased expression of CD27, CD38, and CD138 and down regulation of the expression of CD20 and IgD on the CD25+ B cell population (indicating a plasma blast/cell phenotype). In addition, cells originating from the CD25+ population secreted far more immunoglobulins compared to CD25– cells. This finding is in contrast to our data using un- Mikael Brisslert (740528-5136) Research program 6 stimulated cells from healthy subjects where the CD25– B cells secreted more immunoglobulins. Interestingly, in RA patients this difference is lost, again suggesting that CD25+ B cells may be involved in the pathogenesis of RA. Expected outcome: We expect that we will be able to document that CD25+ B cells are a subset of memory B cells and that these cells are important in the development of RA and perhaps also in other B cell–mediated diseases such as vasculitis and allergy. A 4 10 C 10 5 10 4 62 3 10 99.2 PE-A: CD 25 10 B 5 PE-A: CD 25 10 PE-A: CD 25 10 5 10 3 10 2 10 0 10 2 10 3 10 4 Pacific Bl ue-A: CD 19 10 5 3 10 2 10 2 0 0 36.7 0 4 84.6 0 10 2 3 4 10 10 Pacific Bl ue-A: CD 19 10 5 0 10 2 10 3 10 4 Pacific Bl ue-A: CD 19 10 5 Figure 2: Validation of cell sorting generating CD25+ and CD25– B cells from human blood. (A) The original B cell population is shown. (B) The sorted CD25+ B cell population. (C) The sorted CD25– B cell population. Specific aim 4: To generate mice lacking the CD25+ B cell subset and assess their response to immunisations, bacterial infections and arthritis. Mice lacking the CD25 gene (CD25 knockout) have been generated. However, these mice develop severe disease at a young age that range from lymphoproliferative disorders, haemolytic anaemia and inflammatory bowel disease, making it impossible to define the importance of CD25+ B cells in these mice. In collaboration with Dr. Martin Bergö (Wallenberg laboratory, Sahlgrenska Academy) we will generate mice lacking CD25 exclusively on B cells. For this, we will flank the promoter and exon 1 of the CD25 gene with loxP sites (“flox”) with standard gene-targeting techniques. We will the breed the CD25flox/flox mice (with normal expression of CD25) on with mice expressing Cre-recombinase exclusively in B cells (Cre driven by the CD19 promoter). We will thus obtain mice that lack CD25 expression on B cells. With these mice, we will answer several important questions: Would mice lacking CD25 on B cells exhibit an impaired ability of B cells to present antigens, migrate and respond to immunizations? Would the absence of CD25 on B cells render mice less susceptible or even resistant to autoimmune diseases like collagen-induced arthritis and SLE-models [29, 30]? What about sensitivity to bacterial infections? We hypothesize that CD25 on B cells is important in all these processes. The genetically modified mice are now under construction. SIGNIFICANCE Despite intense research, the role of B cells and B cell subpopulations in rheumatoid arthritis has not been established. A few years ago a cytolytic monoclonal antibody targeting CD20 on B cells (rituximab) was approved by the Swedish Ministry of Health for treatment of RA. The treatment has improved the quality of life for many RA patients. Rituximab is a B cell specific drug, and the successful disease outcome among patients has again implicated that B cells are of great importance for the progression of the disease. Our group has a unique expertise in this field and together with our collaborators we are perfectly positioned to answer all the questions in this application. The design of this project, which includes both a large and defined clinical material as well as a new mouse model, generates excellent tools to answer the proposed questions. In the long run, we hope to be able to identify a subset of B cells (most likely CD25+) that can be targeted in RA therapy and that this strategy will substantially reduce the sometimes severe side effects seen with complete B cell depletion. In addition, our study should allow us to define the efficiency of antigen- Mikael Brisslert (740528-5136) Research program 7 specific vaccination and optimize the conditions for vaccination regimens in RA patients undergoing rituximab therapy. REFERENCES 1. Goronzy JJ, Weyand CM. Rheumatoid arthritis. Immunol Rev 2005;204:55-73. 2. Silverman GJ, Carson DA. Roles of B cells in rheumatoid arthritis. Arthritis Res Ther 2003;5 Suppl 4:S1-6. 3. Carsetti R, Rosado MM, Wardmann H. Peripheral development of B cells in mouse and man. Immunol Rev 2004;197:179-91. 4. Honjo T, Alt F, Neuberger M. Molecular Biology of B cells. San Diego: Elsevier Academic Press, 2004. 5. Lam K-P, Rajewsky K. B-cell development. In: Gallin J, Snyderman R, eds. Inflammation: Basic principles and clinical correlates, Vol. 3rd edition. Philadelphia:Lippincott, Williams, and Wilkins, 1999:151-65. 6. Lopes-Carvalho T, Kearney JF. Development and selection of marginal zone B cells. Immunol Rev 2004;197(1):192-205. 7. Brisslert M, Bokarewa M, Larsson P, Wing K, Collins LV, Tarkowski A. Phenotypic and functional characterization of human CD25 B cells. Immunology 2006;117(4):548-57. 8. Amu S, Tarkowski A, Dörner T, Bokarewa M, Brisslert M. The human immunomodulatory CD25+ B cell population belongs to the memory B cell pool Scand J Immunol 2007;66(1):77-86. 9. Amu S, Stromberg K, Bokarewa M, Tarkowski A, Brisslert M. CD25-expressing Blymphocytes in rheumatic diseases Scand J Immunol 2007;65(2):182-91. 10. Rolink A, Grawunder U, Winkler TH, Karasuyama H, Melchers F. IL-2 receptor alpha chain (CD25, TAC) expression defines a crucial stage in pre-B cell development. Int Immunol 1994;6(8):1257-64. 11. Amu S, Gjertsson I, Tarkowski A, Brisslert M. Phenotypic properties of CD25-expressing murine B-cells in primary and secondary lymphoid organs. Scand J Immunol 2006;64(5):482-92. 12. Takemura S, Klimiuk PA, Braun A, Goronzy JJ, Weyand CM. T cell activation in rheumatoid synovium is B cell dependent. J Immunol 2001;167(8):4710-8. 13. Edwards JC, Cambridge G. Prospects for B-cell-targeted therapy in autoimmune disease. Rheumatology (Oxford) 2005;44(2):151-6. 14. Edwards JC, Cambridge G. B-cell targeting in rheumatoid arthritis and other autoimmune diseases. Nat Rev Immunol 2006;6(5):394-403. 15. Park YW, Pryshchep S, Seyler TM, Goronzy JJ, Weyand CM. B cells as a therapeutic target in autoimmune diseases. Expert Opin Ther Targets 2005;9(3):431-45. 16. Tsokos GC. B cells, be gone--B-cell depletion in the treatment of rheumatoid arthritis. N Engl J Med 2004;350(25):2546-8. 17. Leandro MJ, Edwards JC, Cambridge G. Clinical outcome in 22 patients with rheumatoid arthritis treated with B lymphocyte depletion. Ann Rheum Dis 2002;61(10):883-8. 18. Leandro MJ, Edwards JC, Cambridge G, Ehrenstein MR, Isenberg DA. An open study of B lymphocyte depletion in systemic lupus erythematosus. Arthritis Rheum 2002;46(10):2673-7. 19. Leandro MJ, Cambridge G, Ehrenstein MR, Edwards JC. Reconstitution of peripheral blood B cells after depletion with rituximab in patients with rheumatoid arthritis. Arthritis Rheum 2006;54(2):613-20. 20. Roll P, Dorner T, Tony HP. Anti-CD20 therapy in patients with rheumatoid arthritis: predictors of response and B cell subset regeneration after repeated treatment. Arthritis Rheum 2008;58(6):1566-75. Mikael Brisslert (740528-5136) Research program 8 21. Roll P, Palanichamy A, Kneitz C, Dorner T, Tony HP. Regeneration of B cell subsets after transient B cell depletion using anti-CD20 antibodies in rheumatoid arthritis. Arthritis Rheum 2006;54(8):2377-86. 22. Leandro MJ, Cooper N, Cambridge G, Ehrenstein MR, Edwards JC. Bone marrow Blineage cells in patients with rheumatoid arthritis following rituximab therapy. Rheumatology (Oxford) 2007;46(1):29-36. 23. Trollmo C, Sollerman C, Carlsten H, Tarkowski A. The gut as an inductive site for synovial and extra-articular immune responses in rheumatoid arthritis. Ann Rheum Dis 1994;53(6):377-82. 24. Gelinck LB, Teng YK, Rimmelzwaan GF, van den Bemt BJ, Kroon FP, van Laar JM. Poor serological responses upon influenza vaccination in patients with rheumatoid arthritis treated with rituximab. Ann Rheum Dis 2007;66(10):1402-3. 25. Oren S, Mandelboim M, Braun-Moscovici Y, et al. Vaccination against influenza in patients with rheumatoid arthritis: the effect of rituximab on the humoral response. Ann Rheum Dis 2008;67(7):937-41. 26. Arnett FC, Edworthy SM, Bloch DA, et al. The American Rheumatism Association 1987 revised criteria for the classification of rheumatoid arthritis. Arthritis Rheum 1988;31(3):315-24. 27. Brisslert M, Enarsson K, Lundin S, Karlsson A, Kusters JG, Svennerholm AM, Backert S, Quiding-Jarbrink M. Helicobacter pylori induce neutrophil transendothelial migration: role of the bacterial HP-NAP. FEMS Microbiol Lett 2005;249(1):95-103. 28. Gjertsson I, Innocenti M, Matrisian LM, Tarkowski A. Metalloproteinase-7 contributes to joint destruction in Staphylococcus aureus induced arthritis. Microb Pathog 2005;38(23):97-105. 29. Williams RO. Collagen-induced arthritis as a model for rheumatoid arthritis. Methods Mol Med 2004;98:207-16. 30. Tarkowski A, Collins LV, Gjertsson I, Hultgren OH, Jonsson IM, Sakiniene E, Verdrengh M. Model systems: modeling human staphylococcal arthritis and sepsis in the mouse. Trends Microbiol 2001;9(7):321-6.