Clinical Guidelines - Family Health Care Clinic
advertisement

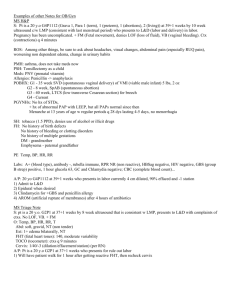
Family Health Care Clinic, Inc. Clinical Guidelines Approved 08 /09 FAMILY HEALTH CARE CLINIC, INC. CLINICAL GUIDELINES Services that would be appropriate to treat in a primary care clinic: Localized infections Medication administration or refills Musculoskeletal pains not associated with recent trauma Needle sticks or puncture wounds Otitis media unless associated with a temperature over 104° or ear drainage Paronychia Sinusitis Sore throat Stye Sublungual hematoma Suture removal Toothache without facial swelling or lymphadenopathy Urinary burning, frequency Notwithstanding the above, the emergency room is the appropriate level of service for the following conditions: Abnormal or unstable vital signs Abnormal motor, sensory,, <w tendon functions of recent onset Eye pain or redness in the presence of contact lenses, foreign body, or trauma Inability to be transferred into a wheelchair for transport Laceration of eyelids, vermillion border of the hp or other complex facial laceration Nose bleeding unable to be controlled by conservative measures Psychiatric loss of control, intoxication, significant confusion or disorientation, or if mere is a high probability of a need for security Vaginal bleeding or pain in pregnancy or in any woman with a late or missed period Diabetes Mellitus The Primary Care Provider Recommended Guidelines: Metabolic diseases characterized by hyperglycemia from defects in insulin, secretion, insulin action, or both. I. Coordinate Care and Anticipate Needs = Risk Factors II. Pathogenesis and etiologic classification of DM A. B. Type I usually results in absolute insulin deficiency 1. Occurs in 10% of diagnosed diabetics 2. Acute onset of polydipsia, polyphagia, polyuria, weight loss, blurred vision, frequent infections 3. Can occur at any age, but usually highest incidence in childhood and adolescence. a. Morbidity and mortality greatest in infants b. Fatigue, weakness, and listlessness c. Nocturnal enuresis d. More infections and sick days e. Ketoacidosis may occur Type II characterized by resistance to the action of insulin and a relative or predominant impairment of insulin secretion 1. Occurs mainly in adults ≥ 30 years of age 2. Obesity and increased abdominal fat 3. Gradual onset with slow progression of symptoms 4. Fatigue 5. 50% of patients will eventually need insulin 6. Ketoacidosis rarely occurs 7. Hyperglycemic hyperosmolar nonketotic coma predominant a. Blood glucose ≥ 600 mg/dl b. Often precipitated by drugs such as steroids and diuretics, therapeutic procedures, chronic disease, and acute stress 8. At risk for cardiovascular disease 9. Type 2 diabetes in children a. Obesity C. b. Family history c. Acanthosis nigricans in 90% of children, velvety hyperpigmented patches in intertriginous area d. Polycystic ovarian syndrome e. Hypertension and dyslipidemia may occur Other specific types of diabetes 1. Genetic defects 2. Exocrine pancreas 3. Endocrinopathies 4. Drug or chemical induced 5. Infections 6. Immune-mediated diabetes 7. Other genetic disorders D. Gestational DM E. Impaired glucose tolerance F. 1. Asymptomatic, at risk for developing DM and cardiovascular disease 2. Associated with insulin resistance syndrome Macrovascular and microvascular complications 1. 2. 3. Retinopathy a. Prevalence is related to duration and type of DM b. Occurs in most Type 1 patients after 20 years and in ≥ 60% of type 2 DM Nephropathy a. Develops in 35 – 45% of type 1 DM and 20% in type 2 DM b. Diabetes in most common cause of ESRD in US Neuropathy a. Peripheral, symmetric sensorimotor neuropathy which is usually only minimally uncomfortable b. May have lancinating or burning pain c. Cardiovascular disease d. III. Care in office or rapid treatment site – Diagnostic Criteria A. Family history of diabetes, hypertension, cardiovascular impairment, and renal manifestations 1. 2. 3. 4. 5. B. C. Polydipsia, polyuria, and weight loss Fasting plasma glucose of ≥ 126/mg/dl 2 hour plasma glucose of ≥ 200/mg/dl during an oral glucose tolerance test Fatigue Infections Physical Examination 1. 2. 3. 4. 5. 6. 7. 8. 9. 10. D. Hx of gestational DM Prior of previous pharmacological, nutritional, and self-management treatment plans Dietary habits History of smoking, hypertension, and obesity Psychological, sociological and economic factors that may impact DM management Symptoms of DM 1. 2. 3. 4. 5. Compare height and weight with norms Vital Signs Examine skin Ophthalmoscopic examination Mouth and dental exam Thyroid Cardiovascular Abdomen Extremities including feet Neurological Diagnostic Tests 1. 2. 3. 4. 5. 6. 7. 8. 9. 10. IV. Increased prevalence of infections, cognitive impairment, and contracture of digits (hammer toes and stiff fingers) Screening Random plasma glucose measurement Fasting plasma glucose measurement HbA1C Diabetic retinopathy Fasting lipid profile Annual serum creatinine Urinalysis Microalbuminuria Diabetic ketoacidosis Educate patient, family, and caregiver about: A. Underlying pathologies and management plan 1. 2. 3. 4. 5. 6. 7. Explain long-term complications Patient to wear Medic-Alert tags If applicable, discuss contraception and importance of glucose control before conception and during pregnancy Nutritional recommendations Physical activity Medication regimen Insulin therapy, if applicable B. C. How to recognize signs and symptoms of complications, and when to report to health care professional, including: 1. Hyperglycemia 2. Hypoglycemia 3. Skin breaks including diabetic foot ulcers 4. Change in Blood pressure. 5. Change in Weight 6. Proteinuria 7. Cerebral or visual disturbances. Assess psychosocial factors, including: 1. 2. 3. V. Anxiety and depression. Changes in lifestyle. Changes in social roles. D. Coordinate development of treatment goals and plans with multiple caregivers F. Ensure timely referral to appropriate community resources and applications for public funding. G. Ensure that follow-up appointment is made and transportation is available. Home health care may be suitable for patients who require skilled assessment and management of care A. To minimize out-of-home appointments for patients B. Blood pressure. C. Weight D. Proteinuria E. Cerebral or visual disturbances F. Medication management in home environment utilizing glucose monitoring G. Signs and symptoms of edema, including pulmonary edema. H. Patient is safe at home, with adequate caregiver available as needed Hypertension The Primary Care Provider Recommended Guidelines: I. II. Coordinate Care and Anticipate Needs = Risk Factors A. B. C. D. Family history of hypertension or vascular disease. Personal history of cardiovascular or hypertensive disease Personal history of tobacco use. Diabetes E Renal infections F. Circulatory involvement Care in office or rapid treatment site A. Hypertensive disorders are the most common medical complication B. Medically assess and stabilize preexisting blood pressure or renal disease: 1. 2. 3. 4. 5. III. Educate patient, family, and caregiver about: A.. B. Underlying pathologies and management plan How to recognize signs and symptoms of complications, and when to report to health care professional, including: 1. 2. IV. Assess blood pressure Obtain urinalysis for protein urea. Obtain blood sample for blood urea nitrogen, creatinine, uric acid, platelets and hemoglobin. Assess edema. Assess reflexes. Blood pressure elevation >30 systolic or > 15 diastolic from baseline. Assess home safety, needs, and capabilities Routine Patient Visit Care A.. Monitor progress: 1. 2. 3. 4. 5. 6. 7. B. Blood pressure. Weight Proteinuria Intake and output Cerebral or visual disturbances. Signs and symptoms of edema, including pulmonary edema. Nail beds, observing for cyanosis. Assess psychosocial factors, including: C. 4. Anxiety and depression. 5. Changes in lifestyle. 6. Changes in social roles. 7. Coordinate development of treatment goals and plans with multiple caregivers D. Ensure timely referral to appropriate community resources and applications for public funding. G. V. VI. VII. Ensure that follow-up appointment is made and transportation is available. Home healthcare may be suitable for patients who require skilled assessment and management of care, including: A. To minimize out-of-home appointments B. Blood pressure. C. Weight D. Proteinuria E. Intake and output. F. Cerebral or visual disturbances G. Signs and symptoms of edema, including pulmonary edema. IH Nail beds, observing for cyanosis. I. Patient is safe at home, with adequate caregiver available as needed Educate patient, family, and caregiver about care requirements. Clinical Indications for Inpatient Admission A. Uncontrolled hypertension (systolic >=160 mm Hg or diastolic >=010 mm Hg) with (any one of the following): 1. 2. 3. 4. 5. 6. 7. 8. Proteinuria > 100 mg/L on urine dipstick or > 1 g/24 hours Rapid increase in serum creatinine to > 1.2 mg/dL Platelet count <100,000/mm3 Evidence of microangiopathic hemolytic anemia Elevated hepatic enzymes (alanine aminotransferase or aspartate aminotransferase) Epigastric pain Significant edema Evidence of acute and progressing target organ disease (any one of the following): a. Hypertensive encephalopathy b. Cerebral infarction c. Intracerebral hemorrhage d. Myocardial ischemia, myocardial infarction e. Acute pulmonary edema f. Aortic dissection g. Seizures h. Acute renal insufficiency i. Papilledema j. Optimal Recovery Course 9. Day 1: Admit patient for blood pressure out-of-control, hypertensive symptoms, or failure to respond to outpatient antihypertensives. Bed rest. Frepuent vital signs. Urinalysis, CBC, platelet count, chemistry panel (including creatinine and transaminases). Oral or parenteral antihypertensives. Discharge planning 10. Day 2: Blood pressure normal or adequately controlled. Laboratory values normal or resolved to near normal. Up ad lib. Oral medication. Discharge B. Goal Length of Stay: Ambulatory to 1 day Note: Goal length of stay assumes optimal recovery, decision-making, and care. Patients may be discharged to a lower level of care (either later than or sooner than the goal) when it is appropriate for their clinical status and care needs. C Extended stay beyond goal length of stay may be needed for: 1. 2. VIII. Other hypertension-associated conditions (e.g., hemolysis, low platelets) - may require ongoing inpatient care. Expect moderate to prolonged stay extension. Uncontrolled hypertension or target organ damage (e.g., cerebral infarction). Home Care A. Restriction of activity B. Home blood pressure monitoring C. Discourage use of alcohol and tobacco D. Pharmacologic treatment for diastolic blood pressure greater than 100 mm Hg IMMUNIZATIONS Recommended childhood and adolescent immunization schedule- The guideline recommendations were approved by the Advisory Committee on Immunization Practices, the American Academy of Family Physicians, and the American Academy of Pediatrics. Primary Care Provider Recommendations: I. Ensure that the recommended childhood and adolescent immunization schedule is current with changes in manufacturers' vaccine formulations II. Provide Vaccine Information Statements to parents or guardian - The National Childhood Vaccine Injury Act requires that all health-care providers give parents or patients copies of Vaccine Information Statements before administering each dose of the vaccines listed in the schedule. III. Verify the status of child’s immunization by reviewing Form 121 for MSBH Immunization Registry. IV. Ensure entries are made to MSBH Immunization Registry when immunizations are given. If FHCC EMR records show immunizations were given and recorded in registry, ensure corrections are made. V. Advise parents or guardian of recommended immunization schedule if not current and/or when next immunizations are due according to the attached schedule. Papanicolaou (Pap) Smear The Primary Care Provider Recommended Guidelines: Cervical cytology is primarily a screening test that can link human papillomavirus (HPV) with cervical cancer and its precursors. Females patients ages 21 to 64 should be evaluated at least every two (2) years utilizing cervical cytology. I. Cervical cytology is primarily a screening test that in some instances may serve as a medical consultation by providing an interpretation that contributes to a diagnosis. A. Approximately 13,000 women in the US develop cervical cancer each year, and about 4,500 women die of the disease. Most women who develop cervical cancer have never had a Pap smear or have not had one in the past 5 years. B. Of the more than 50 million women who undergo Pap testing in the US each year, approximately 3.5 million (7%) are diagnosed with a cytological abnormality requiring additional follow-up or evaluation. II. Diagnosis/Evaluation/Plan/Management A. Pathogenesis 1. Oncogenic strains of HPV are present in more than 80% of cervical cancers. However, infection with an oncogenic strain does not mean that a woman will inevitably develop intraepithelial lesions. 2. Incidence of infection with HPV is directly related to sexual activity; the greater the number of partners, the greater the risk of HPV infection 3. Other cofactors that have a role in development of cervical neoplasia include smoking, sexual behavior (early onset and multiple partners), and immunological status of the woman B. Specimen Type: 1. 2. C. General Categorization 1. 2. 3. D. G. Trichomonas vaginalis Fungal organisms morphologically consistent with Candida spp Shift in flora suggestive of bacterial vaginosis Bacteria morphologically consistent with Actinomyces spp Cellular changes consistent with Herpes simplex virus Other Non-Neoplastic Findings 1. 2. 3. 4. 5. F. Negative for Intraepithelial Lesion or Malignancy Epithelial Cell Abnormality Other Organisms 1. 2. 3. 4. 5. E. Conventional Smear Liquid-based Reactive cellular changes associated with inflammation (includes typical repair) Radiation Intrauterine contraceptive device (IUD) Glandular cells status post hysterectomy Atrophy Epithelial Cell Abnormalities 1. Squamous Cell 2. Glandular Cell Other malignant neoplasms III. Identification of endometrial cells if not associated with menses or after menopause may indicate risk for an endometrial abnormality, although most often this is a benign finding. Note: Cervical cytology, primarily a screening test for squamous epithelial lesions and squamous cancer, is unreliable for detection of endometrial lesions and should not be used to evaluate suspected endometrial abnormalities IV. Categories of women in need of paps smears A. B. C. D. E. Postmenopausal women Immunosuppressed women Pregnant women Adolescents Young women of reproductive age V. Refer for colposcopic evaluation and biopsy of lesions suspicious for high-grade disease or cancer VI. Educate patient concerning need for paps smear screening on a regular basis throughout her life time. Prenatal Care (1st Trimester)/ New Born Higher Birth Weight The primary Care Provider Recommended Guidelines: I. Be aware that the current 11 % rate of preterm birth has not changed significantly in the past 20 years despite increased rate of interventions, including bed rest, hydration, and enhanced prenatal care II. Educate pregnant women that risk factors are present in 50% of women with preterm labor: Risk factors include: A. Demographic risks: 1. 2. 3. 4. 5. B. Medical risks predating current pregnancy 1. 2. 3. 4. 5. 6. 7. C. Multiple gestation. Infection, including: bacterial vaginitis and urinary tract infection Incompetent cervix Short interval between pregnancies Bleeding in first trimester Placenta previa or abruptio placentae Fetal anomalies Premature rupture of membranes Behavioral and environmental risks: 1. 2. 3. 4. 5. 6. III. History of previous preterm birth Multiple abortions, spontaneous or elective. Uterine anomalies Low pregnancy weight for height. Parity (0 or >4) Diabetes Hypertension Medical risks in current pregnancy 1. 2. 3. 4. 5. 6. 7. 8. D. African-American. Below 17 or above 24 years of age Lower socioeconomic status Unmarried Lower level of education. Diethylstilbestrol exposure Smoking Poor nutrition Alcohol or other substance use, especially cocaine Late or lack of prenatal care. High stress Prenatal in Office Site A. B. C. Medically assess and stabilize comorbid medical conditions, including diabetes and hypertension Identify women at risk for preterm labor and tailor interventions to specific needs and resource availability. Most interventions designed to prevent preterm birth do not work Interventions may include 1. Toxocolytic agents, including: 2. 3. 4. IV. IV. a.. Beta agonists, e.g., ritodrine and terbutaline b. Prostaglandhn inhibitors, e.g., indomethacin. c. Calcium channel blockers, e.g., nifedipine. d. Oxytocin antagonists e. Magnesium sulfate Special programs targeted to high-risk conditions, including drug use Relaxation therapy Antibiotic treatment of urinary tract infections and bacterial vaginitis Educate patient, family, and caregiver about: A. How to recognize signs and symptoms of preterm labor. B. How to recognize signs and symptoms of complications, and when to report to health care professional If hospitalized, monitor daily progress: A. Ensure that patients with premature rupture of the membranes who test positive for group B Streptococcus receive antibiotic therapy B. Assess psychosocial factors, including: C. Fear for outcome, anxiety and depression. 1. 2. 3. Changes in lifestyle Changes in social roles. Provide support and referral, as needed. D. Corticosteroid therapy may promote fetal maturation E Facilitate decision about home care. Home healthcare may be suitable for patients with cervical dilatation of 3 cm or less, and fewer than 4 to 6 contractions per hour F Coordinate development of treatment goals and plans with multiple caregivers G. Facilitate transition to next level of care H. Regularly communicate with professional staff, patient, family, and caregiver I Ensure that follow-up appointment is made J Hospital Admission may be indicated for (any one of the following) 1. 2. 3. 4. 5. 6. 7. Preterm rupture of membranes IV tocolytics (beta-adrenergic agonists) required Administration of IV magnesium as a tocolytic Suspected amnionitis Significant vaginal bleeding Maternal infection (e.g., pyelonephritis, pneumonia) Severe maternal disease trigger or comorbidity including: 8. 9. 10. L. Day 1 a. Uncontrolled diabetes b. Diabetic ketoacidosis c. Severe dehydration d. Preeclampsia e. Severe hypertension Delivery Fetal demise Condition requiring premature delivery (preeclampsia or presumed fetal growth restriction) Admit patient with significant contractions before term. Bed rest. Parenteral hydration, parenteral tocolytic therapy, and corticosteroids[A1 (if indicated for fetal maturation). Eliminate infectious or other medical causes. Usual diet. Discharge planning. Possible discharge, if contractions cease and parenteral medication not in use. Day 2: M. Contractions ceased. Activity as tolerated. Discharge. Goal Length of Stay: Ambulatory to 1 day Extended stay beyond goal length of stay may be needed for: 1. 2. 3. Significant infection - anticipate parenteral antibiotics, observation until contractions ceased; transition to home healthcare for continued parenteral antibiotics. Expect brief stay extension. Continued uterine contractions - anticipate continued parenteral tocolytics; for progression to delivery expect brief stay extension; if contractions controlled, continued IV tocolytics may or may not be necessary. Expect brief to prolonged stay extension. Fetal demise - anticipate progression to delivery and possible induction of delivery (near term); if contractions cease and delivery not elected, anticipate discharge while awaiting spontaneous delivery. Possible brief stay extension. Continued vaginal bleeding - anticipate rapid evaluation of placenta previa or abruption, may require surgical control, delivery, or both. Expect brief to moderate stay extension. 5. Other condition (e.g., severe maternal disease, premature delivery) requiring continued inpatient care. Expect brief to moderate stay extension. Alternatives to hospitalization 4. V. A. Outpatient care in labor and delivery unit B. 1. Observation, fetal and maternal monitoring 2. Tocolytic trial 3. Discharge if contractions ceased Home care 1. 2. 3. 4. Decreased activity Possible parenteral hydration Possible tocolytic therapy Corticosterohds[A] (if indicated for fetal maturation) Tobacco Use and Smoking Cessation The Primary Care Provider Recommended Guidelines: I. II. III. IV. Destructive health behavior involving use of tobacco (cigarettes, chewing tobacco, and snuff) A. Tobacco use is the leading preventive cause of death in US. One of every 5 deaths is the result of tobacco use. B. 23.5% of US adults smoked cigarettes in 2003. C. Tobacco smoke contains numerous substances which are toxic, mutagenic, or carcinogenic D. Tobacco smoke contains carbon monoxide, nicotine, and tars. E. Results to delicate pulmonary tissues are devasting. Assess effect of tobacco dependence on patient. A. Physiological factors B. Psychological factors C. Social/behavioral factors Psychological barriers to quitting include: A. Withdrawal syndrome with symptoms such as anxiety, irritability, anger, impatience, restlessness, difficulty concentrating, sleep disturbances, increased appetite, and depressed mood. B. Symptoms begin a few hours after last cigarette smoked. C. Frequently use tobacco to handle stress and negative emotions such as anger and anxiety. Diagnosis/Evaluation A. B. \ History 1. Number of years smoked and how many packs per day 2. How soon after arising 1st cigarette is smoked. 3. Past attempts at quitting. 4. Cough, sputum production, shortness of breath, recurring respiratory infections. Physical Examination 1. Monitor vital signs 2. Examine ears, nose, mouth, pharynx, mouth for inflammation 3. Complete exam of lungs 4. Complete exam of heart and peripheral vascular system. C. V. Diagnostic Tests 1. Consider spirometry 2. Screen for lipid disorders. Plan/Management A. Major intervention 1. Brief clinical intervention 2. Intensive clinical intervention 3. Systems interventions B. Identify all tobacco users at every visit – C. Advise all smokers to stop 1. Be clear. 2. Speak strongly. 3. Personalize advice. 4. Assess willingness to make a quit attempt. 5. Assist patient who is willing to quit 6. a. Counseling b. Pharmacotherapy Follow up