Fever - case study No 1:
advertisement

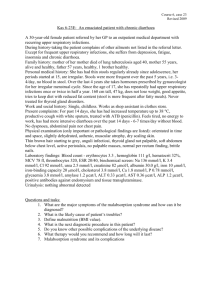
Course 1, Case 1 Revision 2010 Case 1-1E: An 18-year-old woman with mild fever, abdominal pain and dysuria Current illness: Two days she got fever up to 38 °C without chills, general malaise, dysuria burning at urination, lower abdominal pain, passing small portions of urine but frequently, the urine seems dark. Personal history: No severe illness before, only common colds, 3 times tonsillitis, treated with antibiotics. Occasional cervical spine complaints. No operation, no injury. No regular medication except contraceptive pills. Menstruation from age 12, regular period. No known allergy. Family history: Mother 43y healthy, father 45y had got nephrolithiasis, underwent lithotomy. One brother is healthy. Social history: Lives with parents and brother. Student of high school. Epidemiological history: One week on a camping trip, returned 2 days ago. Physical examination (only significant or pathological findings are listed): Patient conscious, well orientated, with no exanthem. T 38 °C; BP 120/70; pulse 90; tongue white and dry. Painful palpation of the lower abdomen, no resistance. Liver a spleen not palpable. Tapottement bilaterally negative. Meningeal signs: neck stiffness +1 cm, limited left and right rotation; Lassegue negative, spine sign negative. Laboratory results: ESR 28/45 Blood count: leukocytes 12 000/μl, differential blood count with 70% neutrophils, 5% bands, 20% lymphocytes, 5% monocytes. Serum: urea, creatinine, Na, K, Cl, liver tests - all within normal limits, CRP 61 mg/l. Urinalysis: protein +++, blood ++, bilirubin 0, urine sediment: leukocytes >5 per high-power field, erythrocytes >5 per high-power field, casts 0. Questions: 1. What kind of infection is concerned? 2. Comment the values of inflammatory parameters. Is the disease rather viral or bacterial? 3. What is the most likely etiological agent? 4. What test can detect the etiological agent? 5. What are the basic therapeutic principles (symptomatic, causal treatment)? 6. How is affected more commonly – women or men – and why? Pathophysiology: Factors predisposing to urinary tract infection. Pathology: Classification and characteristics of urinary tract inflammatory diseases. Course 1, Case 2 Revision 2010 Case 1-2E: A 43-year-old woman with fever, back pain and hypotension Current illness: One week bothered with frequent urination and overall malaise, drank a herbal tea. Last 3 days she has got back pain, took ibuprofen, fever 38-38,5 °C, she thought it was flu. Yesterday she mentioned cloudy urine, vomited, therefore stopped drinking, in the evening fever raised up to 39,7°C with shivering. At night she collapsed when going to the toilet. The attending physician sent her to the hospital. Personal history: Common childhood illnesses, appendectomy at 5 ys of age. Had got several biliary colics, at 30 ys of age cholecystectomy for lithiasis. Frequent low back pain, occasionally takes physiotherapy, once went to the spa. Previously frequent cystitis, she treated herself with herbal tea. No known alllergy. No regular medication except contraceptive pills. Family history: Mother has got diabetes type I, father died in a car accident, brother has got defect of immunity. Two children healthy. Gynecological history: menstruation from age 12, regular period, two labours, no previous gynecological illness. Social history: Office worker, lives with the family. Physical examination (only significant or pathological findings are listed): T 39,5 °C, patient consciouss, slightly desorientated, cold acra, no icterus, no rash, normal skin turgor, BP 80/45, pulse 120/min weak, tongue white and dry, abdomen meteoristic, but soft with no pain, liver and spleen not enlarged; tapottement right-positive, left-negative; meningeal signs negative. Laboratory results: ESR 45/89 Blood count: leukocytes 24.000 /μl, erythrocytes 3.8 mil/μl, hemoglobin 101 g/l, thrombocytes 120.000/μl. Differential count: 83% neutrophils, 15% bands, granulation of neutrophils, 2% lymphocytes. Serum: urea 10.4 mmol/l, creatinine 120 μmol/l, Na, K, Cl within normal limits, CRP 412 mg/l, glucose 10.4 mmol/l. Urinalysis: protein +++, blood +++, glucose ++; urine sediment: leucocytes >5 per highpower field, erythrocytes 15-20, casts 5-10. Questions: 1. Which organ is affected by infection? 2. How will you name the illness? 3. What is the likely pathogenesis of the illness? 4. What are the most common etiological agents? 5. Which clinical and laboratory signs speaks for sepsis? 6. Why is the patient hypotensive? Pathophysiology: Pathophysiology of sepsis Pathology: Interstitial renal disease Course 1, Case 3 Revision 2010 Case 1-3E: A 6-year-old boy with fever, vomiting, diarrhoea, abdominal pain Current illness: Yesterday the boy was refusing the food, at night he vomited, complained of abdominal pain, had got fever 38,6 °C, was given cold compresses and paracetamol. In the morning a diarhoea started, the stools were watery and greenish, boy continues vomiting and fever 39 °C. Refuses drinks and urinates a little. Attending pediatrician sent the boy to the surgical office for suspected appendicitis. The surgeon examined the child, carried out the basic blood tests, excluded an acute abdomen and sent the child to the infectious diseases dept. Personal history: Perinatal data: child of 1st pregnancy, physiological, spontaneous in term delivery, head presentation, 3500g/51cm, not resuscitated, breast-fed 3months, hip joints with no dysplasia, postnatal development normal, vaccinated according schedule. At the age of five he had got chickenpox, three times otitis media with paracentesis. No injury, no operation. Since 4y of age has got pollinosis, allergy to pollen and dust, takes antihistamines seasonally. No regular medication. No other allergy. Fair social conditions, attends a grammar school. Family history: Both parents are healthy. Epidemiological history: Two days ago ate fried eggs. Physical examination (only significant or pathological findings are listed): T 39 °C. Child consciouss but sleepy, pale, with sunken appearance of eyes, decreased skin turgor, tongue white but moist. Breathing alveolar, rate 28/min, P 108/min regular, no heart murmur. Pain on palpation in the right lower abdomen, where palpable soft resistance, borborygms on palpation, liver and spleen not enlarged, per rectum a thin green stool on the glove, palpation not painful. No meningeal signs. Laboratory results: ESR 34/56 Blood count: leukocytes 13.000/μl, differential blood count: 80% neutrophils, 10% bands, 10% lymphocytes. Serum: urea 15.4 μmol/l, creatinine 120 μmol/l, Na 128 mmol/l, K 2,8 mmol/l, Cl 95 mmol/l, CRP 105 mg/l, glucose 3.5 mmol/l Urinalysis: protein +, acetone ++, urine sediment: leuko15-20, ery 0, casts 0. Questions: 1. What will you name the disease (without specifying the etiology)? 2. What are the most common etiological agents? 3. What test is applied for detection of the etiology? 4. What can be the major threat for the patient? 5. What are the basic therapeutical principles? 6. How are ketones built? Pathophysiology: Classification of diarhoea diseases with respect to causes and pathogenesis Pathology: Intestinal inflammations (of infectious and non-infectious origin) Course 1, Case 4 Revision 2010 Case 1-4E: A 6-year-old girl with fever, sore throat and rash Current illness: Yesterday the girl was tired, complained of abdominal pain and sore throat, at night she got fever 39 oC, was given paracetamol 200mg. This morning fever again 38,5 oC, sore throat, mother noticed some rash on the abdomen. Personal history: Perinatal data: child of 1st pregnancy, physiological, spontaneous in term delivery, head presentation, 3350g/50cm, no resuscitation, physiological icterus, breast-fed 4 months, hip joints with no dysplasia, vaccinated according schedule. No severe illness before, only common colds. No injury, operation - nasal adenotomy in 3ys of age. No regular medication. No known allergy. Fair social conditions, attends a kindergarten. Family history: Father treated for high blood pressure, mother healthy, sister 3ys healthy. Physical examination: T 38oC, girl conscious, responds adequatelly, complains of sore throat and mild headache. On the skin of the abdomen and axillae there is tiny maculopapular rash of red colour, confluent, slightly itching, with blanching under pressure or scratching. Face erythem with circumoral pallor, reddened throat and palatal tonsills, white tongue. Mild bilateral submandibular lymphadenopathy, slightly painful. Eupnoic, normal lung and heart sounds, HR 100/min, BP 90/60. Abdomen soft, no resistance, not tender, no hepatomegaly, no splenomegaly. Meningeal signs negative. Questions: 1. What is the likely diagnosis? 2. What is the etiological agent? 3. In what material and what test can isolate the pathogen? 4. What other diseases can the pathogen cause? 5. What does cause the skin a mucosal signs in this disease? 6. What are the basic therapeutical principles? Pathophysiology: Fever, its specific features in childhood. Principles of body temperature regulation and its disorders. Pathology: Rheumatic fever Course 1, Case 5 Revision 2010 Case 1-5E: A 19-year-old man with fever and sore throat Current illness: About a week ago fever 38-38,5 °C started, general practitioner diagnosed acute tonsillitis and gave oral penicillin. There was no improvement with penicillin therapy. Last 2 days he can hardly swallow, lymph nodes on the neck are swollen, fever persists. Personal history: In childhood chickenpox, several times otitis media with paracentesis, once pneumonia, no hospitalization. No operation, injury: forearm fracture at the age of 8, treated conservatively. No regular medication. No known alllergy. Family history: Mother healthy, father was diagnosed with Bechterev´s disease, sister heatlhy. Social history: Student, lives with the parents. Alcohol occasionally beer, no smoking, no drug abuse. Physical examination: T 38,7 °C. Conscious, orientated. Normal hydration. Skin with no icterus, no rash, normal turgor. Nasal voice (rhinolalia), oral foetor, slight eyelids swelling, throat iflammed, tonsills reddened enlarged with yellowish pseudomembranes, petechiae on the palate, prominent submandibular lymphadenopathy – bilateral paquetts size 5x3 cm, painful. Eupnoic, normal lung and heart sounds, HR 90/min, reg., BP 120/70. Abdomen soft, well palpable, no pain, liver enlarged 2 cm, palpable spleen under left costal margin. signs negative. Laboratory results: ESR 18/30 Blood count: leukocytes 12.000/μl, differential count: 40% neutrophilic polymorphonuclears, 32% lymphocytes, 10% monocytes, 14 % atypical monocytes Serum: CRP 17 mg/l, bilirubin 20 mmol/l, ALT 3.2 μkat/l, AST 1.9 μkat/l, ALP 1.6 μkat/l, GMT 1.7 μkat/l Questions and tasks: 1. Is the disease rather of bacterial or viral origin? 2. Which of described data point on such origin? 3. What is the likely etiology? 4. Which organs belong to lymphatic system? 5. Does the liver belong to lymphatic system, too? 6. What types of cells are in the liver? Patophysiology: Spleen: pathophysiological consequencies Pathology: Inflammatory diseases of the upper respiratory tract Course 1, Case 6 Revision 2010 Case 1-6E: A 16-year-old boy with fever and meningeal syndrome Current illness: Three days of sore throat, with no fever, was training ice-hockey normally. Yesterday in the afternoon headache ant backache, fever 38,5 oC. At night he vomited, complained of severe headache, had fever 39 oC, small red spots occured on the skin of hands and legs. Since the morning is very sleepy. The emergency service took him to the hospital. Personal history: No severe illness before, only common colds. Vaccinated according schedule. Operations: appendectomy in 10ys of age. Sport injuries – fracture of the left forearm, fractures of right hand fingers. No regular medication, sometimes vitamins. No known allergy. Family history: Father was treated for duodenal ulcer, mother has got cervicobrachial syndrome, sister is healthy. Social history: Lives with parents, student of the 1st year of high school. Active ice-hockey player training 4 times a week. No alcohol, no smoking, no drugs. Epidemiological history: No known source of infection, no travel abroad in the last year. Physical examination (only significant or pathological findings are listed): T 39,2oC, patient somnolent, if wakened up can answer his name correctly, no more response. Neck stiffness 3 fingers, Lassegue + 60 degree bilat., other signs not examined. Small petechiae up to 3 mm on the skin of hands and legs. Skin turgor normal. Eyes – isocoric pupills, normal response to light. Throat slightly inflammed, dry tongue. No submandibular lymphadenopathy. Eupnoic, normal lung and heart sounds, HR 90/min, reg., BP 100/60, oxygen saturation 97%. No pathology on the abdomen. Laboratory results: ESR 20/40 Blood count: leukocytes 20.000/μl, erythrocytes 5.02 mil/μl,, hemoglobin 160 g/l, hematocrit 0.49, thrombocytes 120.000/μl Serum: glucose 6.6 mmol/l, urea 7.0 mmol/l, creatinine 67 μmol/l, Na 140 mmol/l, K 4.2 mmol/l, Cl 101 mmol/l, CRP 250 mg/l. Coagulation: Quick 19.2 s, INR 1.5, APTT 67 s, R 2.1, D-dimers 2.000 (high), antitrombin III 60% (decreased) CSF: turbid, polymorphonuclears 8.200/3μl, protein 4.5 g/l, glucose 0.8mmol/l, lactate 7mol/l Questions: 1. What type of meningitis is concerned? 2. What is the likely etiology? 3. What tests can detect the etiological agent? 4. What is the mechanism of fever? 5. Why is the patient uncouscious? 6. What kind of coagulation disorder is associated with the disease? Pathology: Inflammation of the central nervous system Pathophysiology: Acute adrenal failure Course 1, Case 7 Revision 2010 Case 1-7E: A 60-year-old woman with fever and impaired consciousness Current illness: Two weeks ago pain in the right ear started, with no fever, examined by general practitioner and given ear drops. The earache persisted. Last 2 days fever 38 oC and headache, vomited at night, since this morning she stays in bed, fever 39 oC, very sleepy, did not respond. The emergency service took her to the hospital. Personal history: Common diseases in childhood. Ten years ago was treated for duodenal ulcer, after therapy without complaints. Three years ago diabetes type II and hypertension was diagnosed, put on diabetic diet and betablocker. Operations: 10ys ago hysterectomy for myoma. Regular medication: betaxolol (betablocker). No known alllergy. Family history: Father with ischaemic heart disease and diabetes type II, died 70ys old due to acute myocardial infarction, mother died 80ys due to colonic carcinoma, 2 sons 30 and 34ys are healthy. Social history: Lives with husband. Retired, school teacher before. Alcohol sporadically, no smoking, 2 coffees per day. Epidemiological history: No known source of infection, no travel abroad in last year, a dog at home. Physical examination: T 39 oC, patient soporous, no response to speech, restless on painful stimuli, Glasgow Coma Scale score 8-9. Severe neck stiffness, Lassegue + 60 degrees bilat., other signs not examined. Skin with no icterus, no rash, no purpura, turgor normal. Eyes – isocoric pupillae, normal response to light. In the right ear dried purulent fluid. Throat not possible to examine fully, dry tongue mucosa. No palpable thyreopathy, carotid arteries palpable bilat. Normal lung and heart sounds, HR 80/min, reg., BP 145/100, sat O2 91%, snoring. No pathology on the abdomen. Laboratory results: Blood count: leukocytes 25.000/μl, erythrocytes 4.98 mil/μl, hemoglobin 163 g/l, hematocrite 0,50, thrombocytes 240.000/μl Serum: glucose 9.5 mmol/l, urea 16.0 mmol/l, creatinine 105 μmol/l, Na 140 mmol/l, K 4.0 mmol/l, Cl 105 mmol/l, CRP 360 mg/l Cerebrospinal fluid (CSF): turbid, polymorphonuclears 10.200/3μl, protein 6.5 g/l, glucose 0.5 mmol/l, lactate 8 μmol/l Questions: 1. What types of consciousness disordes do you know? 2. What type of meningitis is concerned? 3. What is the likely etiology and pathogenesis in this patient? 4. What tests can detect the etiological agent? 5. Why the patient is soporous? 6. Why are the values of erythrocytes, hemoglobin and hematocrite elevated? 7. What are the basic therapeutic principles? 8. Explain the glucose concentration in CSF. Pathophysiology: Brain edema, intracranial hypertension; hydrocephalus Pathology: Purulent inflammation of the central nervous system Course 1, Case 8 Revision 2010 Case 1-8E: A 32-year-old man with fever and headache Current illness: A week ago he had got cold – mild fever 37,5 oC, myalgia, headache, which disappeared within 2 days. After 4 days without complaints he got again strong headache which worsens, fever 38,5 oC. Since yesterday he feels dizzy, vomited, fever 39 oC. His general practitioner sent him to the hospital. Personal history: Common childhood illnesses. In childhood checked for heart murmur which disappeared. No severe illnesses, only common colds. Regular vaccinations in childhood. Operations and injuries: osteosynthesis of tibial fracture 5ys ago, subsequently metal device extracted. No regular medication. No known alllergy. Family history: Father 62ys has got an ischaemic heart disease, once acute myocardial infarction, mother 59ys has got a chronic nephritis. Son 4ys is healthy. Social history: Lives with wife and son, is a carpenter. Alcohol – 2 beers daily, occasionally more, no smoking, sometimes coffee. Epidemiological history: No known contact with infection. No travel abroad in the last year. Three weeks ago had got a tick bite with no erythema. Physical examination: T 39 oC, patient conscious, orientated, but responds with some latency. Neck stiffness 2-3 fingers, spine sign ++, Lassegue + 70 degree bilat., tremor, mild ataxia, titubation in Romberg III. No paresis. Skin without icterus, rash or bleeding, turgor normal. Eyes – isocoric pupillae, normal response to light, mild conjunctival hyperemia. Throat slightly inflammed, tonsils with no exsudate. Eupnoic, normal lung and heart sounds, HR 100/min, reg., BP 110/60. No pathology on the abdomen. Laboratory results: ESR 20/35 Blood count: leukocytes 7.500/μl, erythrocytes 4.95 mil/μl, hemoglobin 150 g/l, hematocrit 0.46, thrombocytes 295.000/μl Serum: glucose 5.5 mmol/l, urea 4.5 mmol/l, creatinine 75 μmol/l, Na 141 mmol/l, K 4,3 mmol/l, Cl 107 mmol/l, CRP 18 mg/l Cerebrospinal fluid (CSF): clear, polymorphonuclears 20/3μl,, lymphocytes 456/3μl, erythrocytes 0, protein 1.0 g/l, glucose 3.9 mmol/l, lactate 3 /μmol/l Questions: 1. What infection can be transmitted by tick-bite? 2. What is the likely etiology in this patient, why? 3. What test can detect the etiology? 4. What are the characteristics of cerebral tissue inflammation? 5. What are the principles of treatment? 6. Is there possible person-to-person transmission? 7. How can the infection be prevented? 8. Explain the glucose concentration in CSF. Pathophysiology: Vertigo as a symptom of the CNS disorder Pathology: Viral encephalitis Course 1, Case 9 Revision 2010 Case 1-9E: A 52-year-old man with fever, cough and dyspnea Current illness: Two days ago he was fishing and got cold. Yesterday he did not feel well, at night he got chills, in the morning fever 39,2 oC, malaise, breathing troubles and dry cough. He took paracetamol and felt better, but breathing worsened. At night fever 40,5 °C, wife thinks he hallucinated when sleeping. The emergency service took him to the hospital. Personal history: At 20ys of age at a car accident he suffered from chest contusion and spleen rupture, underwent splenectomy. At 45ys cholecystectomy for lithiasis, at 48ys diabetes mellitus type II and arterial hypertension was diagnosed. Regular medication: Vasocardin (metoprolol), Glucobene (glibenclamid). No known alllergy. Family history: Father died 67ys for myocardial infarction, mother is 79ys, last 20ys has been treated for rheumatic disease not well specified, 3ys ago diabetes was diagnosed, put on diet. His brother has got arterial hypertension. Two sons 29 and 31years old who are healthy. Social history: Lives with his wife. Occupation: factory worker. Abusus: smoker 10-20cig per day, alcohol – 2 beers per day. Physical examination: T 39 oC, breath 28/min, HR 108/min, BP 150/100. Patient obese, conscious, orientated, malaised, dyspneic, with non-productive cough. Eyes, ears, nose with no pathology. Skin with no icterus, no rash, no purpura, turgor normal. Mild cyanosis of lips, throat slightly reddened, tongue white and dry. No submandibular or neck lymphadenopathy. Breath sounds decreased on the right side, with little crepitation. Heart sounds normal, regular. Abdomen soft, not well palpable due to obesity, old scar after splenectomy, liver 2 cm below the costal margin, tapottement bilat. negative. Extremities with no pathology. Mild neck stiffness, spine sign +. Laboratory results: ESR: 32/68 Blood count: leukocytes 27.600/μl, erythrocytes 4.7mil/ μl , hemoglobin 151 g/l, thrombocytes 210.000/ μl. Differential count: neutrophilic segments 75%, bands 12%, lymphocytes 13% Serum: glucose 15.8mmol/l, urea 12.4mmol/l, creatinine 98 μmol/l, ALT 0.55 μkat/l, CRP 210 mg/l Urinalysis: protein +, otherwise negative Questions and tasks: 1. What types of pneumonia do you know? With epidemiological aspect (communityacquired, hospital-acquired). 2. What type of pneumonia is concerned in this case? 3. What predisposing factors likely contributed to the disease? 4. Which other examinations are necessary? 5. What is the likely etiology? 6. What test can detect the etiology (what material, what examination)? Pathophysiology: Respiratory insuficiency Pathology: Pneumonia: pathomorphology with regard to etiology Course 1, Case 10 Revision 2010 Case 1-10E: A 24-year-old man with fever, dyspepsia and jaundice Current illness: About a week is feeling sick, may have fever (did not take the temperature), arthralgia, after acetylsalicylic acid short relief of symptoms. Last days does not eat, has no appetite, vomited once, feels puffy abdomen. Yesterday friends noticed his yellow eyes. Also noticed dark urine. Personal history: Common childhood illnesses. Does not remember vaccination, probably regular in childhood. Operations: left inguinal herniotomy at the age of 3, injuries: fracture of mandibula 2 ys ago after street fight. No regular medication. No known alllergy. Family history: Father has got high blood pressure, mother healthy, brother has got epilepsy. Social history: Unemployed. Lives with the parents. Several years i.v. use of pervitine, finished 6 months ago. Alcohol occasionally, sometimes more. Smoking 10 cig per day. Epidemiological history: No known contact with infection, no travel abroad, no transfusion, no surgery within last 6 months. Physical examination: T 38 °C. Conscious, orientated. Asthenic, hydration normal. Skin subicteric (mild jaundice), no rash. Old residual i.v. marks in both cubital fossae. Icteric sclerae, otherwise eyes, nose and ears with no pathology, throat with no inflammation. No lymphadenopathy. Eupnoic, normal lung and heart sounds, HR 84/min, reg., BP 120/70. Abdomen soft, well palpable, slightly painful right hypochondrium, no peritoneal signs, liver enlarged 3 cm, no splenomegaly. Meningeal signs negative. Laboratory results: Blood count: leukocytes 5.300/μl, erythrocytes 4.6 mil/μl, hemoglobin 147 g/l, hematocrit 0.45, thrombocytes 300.000/μl Serum: glucose 4.3 mmol/l, urea 6.8 mmol/l, creatinine 70 μmol/l, Na 139 mmol/l, K 4.4 mmol/l, Cl 110 mmol/l, bilirubin 127 mmol/l, ALT 48.5 μkat/l, AST 28.1 μkat/l, ALP 2.6 μkat/l, GMT 2.7 μkat/l, CRP 30 mg/l. Urinalysis: bilirubin and urobilinogen positive, others negative Questions and tasks: 1. Describe bilirubin metabolism. 2. What type of icterus is concerned? 3. What is the likely etiology? 4. What test can detect the etiology? 5. How was the infection transmitted and how the patient was infected? 6. How can be this infection prevented? Pathophysiology: Acute liver dysfunction Pathology: Viral hepatitis, consequencies of chronic hepatitis Course 1, Case 11 Revision 2010 Case 1-11E: A 45-year-old woman with fever, diarrhoea and vomiting Current illness: On Saturday (about 16 hours after the meal) she got fever 38 oC and vomited. Since Sunday morning she suffered from severe cramps in the abdomen, watery diarhea of green colour, with mucus and blood, fever up to 39o C. In the afternoon she collapsed when going to the toillet. Her husband brought her to the hospital. Personal history: Common diseases of childhood, several times was treated for urinary tract infections. In recent years she has got frequent back pain of vertebral origin, she occasionally uses ibuprofen and diclofenac. Allergy: hay fever, major problems in the spring. Family history: Mother has got cholecystolithiasis, father diabetes mellitus type II, children are healthy. Social history: married, lives with her family in an apartment building, occupation – clerk. Epidemiological history: No known contact with infection. No travel abroad recently. Two days ago - on Friday evening – she had got “steak tartar” (raw beef with egg). Physical examination (only significant or pathological findings are listed): T 38,6oC, patient conscious, orientated, tired, pale, sweating. Skin with no icterus, no rash. Eyes, ears and nose with no secretion. Throat with no inflammation, dry oral mucosa, brownish tongue surface. No submandibular lymphadenopathy. Eupnoic, 12 breaths/min, normal lung and heart sounds, HR 104/min, reg., BP 80/50. Abdomen soft, with diffuse tenderness on palpation, with no resistence, no hepatomegaly and splenomegaly. Meningeal signs negative. Laboratory results: ESR: 12/20 Blood count: leukocytes 14.000/μl, erythrocytes 4.8 mil/μl, hemoglobin 144 g/l, hematocrit 0,45, thrombocytes 234.000/μl Serum: urea 29.3 mmol/l, creatinine 168 μmol/l, Na 129 mmol/l, K 3.6 mmol/l, Cl 95 mmol/L, CRP 150 mg/l, pH 7.28, BE –7.5 mmol/l. Urinalysis: protein +, acetone + Questions and tasks: 1. Give the name of diagnosis in Latin? 2. What is the likely etiology? 3. What test can detect the etiology? 4. Do the laboratory results point on inflammation of the intestine? 5. Why has the patient worsened renal function? 6. What disorder do the biochemistry results point on? Pathophysiology: Metabolism of water Pathology: Acute intestinal inflammatory disease Course 1, Case 12 Revision 2010 Case 1-12E: A 2-year-old boy with fever, vomiting and diarrhoea Current illness: Yesterday the boy refused eating, at noon had got fever 39.6 oC, vomited, later had got diarhea with watery stools. He was examined by family paediatrician who recommended diet and paracetamol for fever. Today fever continues up to 39 oC, vomiting, watery stools with mucus occured every half an hour. No urine since the morning, refuses drinking, therefore sent to the hospital. Personal history: Perinatal data: child of 1st pregnancy, physiological, spontaneous in term delivery, head presentation, 2800g/48cm, no resuscitation, phototherapy for neonatal icterus, hip joints with no dysplasia. Breast-fed 4months, later infant formula, currently toddler food, D vitamin supplementation. Regular vaccination. No severe illness, once otitis media, twice upper respiratory infection. No severe injury, no operation. No known alllergy. Family history: Nonsignificant. Epidemiological history: No known dietary mistake or contact with diarrhoea. Physical examination (only significant or pathological findings are listed): Boy is peevish, crying, does not want to be examined. Body weight 12 kg, height 88 cm, T 37,8 oC. Skin with no icterus, no exanthem, no petechiae. Sunken eyes. Nose and ears – no pathological finding. Throat slightly reddened, oral cavity and tongue mucosa dry. Lymph nodes of normal size. Eupnoic, normal lung and heart sounds, HR 120/min, reg. Abdomen soft, no sensitivity on palpation, no peritoneal signs. Liver 1 cm below costal margin, no spleenomegaly. Meningeal signs negative. Laboratory results: Blood count: leukocytes 13.000/μl, erythrocytes 4.7 mil//μl, hemoglobin 156 g/l, hematokrit 0,48, thrombocytes 336.000/μl Serum: urea 8.2 mmol/l, creatinine 53 μmol/l, Na 157 mmol/L, K 3.2 mmol/l, Cl 130 mmol/l, AMS 2.7 μkat/l, CRP 16 mg/l, pH 7,3, BE –10 mmol/l Urinalysis: protein +, acetone + Stool culture negative. Questions and tasks: 1. Give the name of preliminary diagnosis. 2. What is the likely etiology? 3. What test can detect the etiological agent? 4. What is the source of mucus found in the stool? 5. What disorder do the biochemistry results point on? 6. How the disorder can be corrected? Pathophysiology: Disorders of potassium metabolism: causes and consequences Pathology: Acute intestinal inflammatory diseases Course 1, Case 13 Revision 2010 Case 1-13E: A 22-year-old woman with fever, dyspepsia and jaundice Current illness: About 5 days is feeling sick, has got fever 38-38,5 °C, myalgia, after ibuprofen some relief of symptoms. Last days has no appetite, nausea, abdominal pain. Today she noticed yellow eyes, therefore went to the doctor. Personal history: Common childhood illnesses, more common tonsillitis.Regular vaccination in childhood. Operations: tonsillectomy at the age of 10, injuries: cerebral comotion at the age of 15 after fall on ice. No regular medication. No known alllergy. Family history: Father healthy, mother has got cholecystolithiasis, sister healthy. Social history: Works as cashier at the supermarket. Lives with boy-friend. Alcohol occasionally, no smoking, no drug abuse. Epidemiological history: No known contact with infection, no travel abroad. A month ago she was camping with friends for a week. Physical examination: T 37,8 °C. Conscious, orientated. Eutrophic, hydration normal. Skin subicteric (mild jaundice), no rash. Icteric sclerae, otherwise eyes, nose and ears with no pathology, throat with no inflammation. No lymphadenopathy. Eupnoic, normal lung and heart sounds, HR 80/min, reg., BP 120/80. Abdomen soft, well palpable, slightly painful right hypochondrium, no peritoneal signs, liver enlarged 3 cm, no splenomegaly. Meningeal signs negative. Laboratory results: Blood count: leukocytes 6.000/μl, erythrocytes 4.3 mil/μl, hemoglobin 140 g/l, hematocrit 0.41, thrombocytes 310.000/μl Serum: glucose 4.6 mmol/l, urea 7.2 mmol/l, creatinine 75 μmol/l, Na 140 mmol/l, K 4.1 mmol/l, Cl 108 mmol/l, bilirubin total 90 mmol/l, conjugated 28 mmol/l, ALT 28.5 μkat/l, AST 18.1 μkat/l, ALP 2.1 μkat/l, GMT 1.5 μkat/l, CRP 22 mg/l. Urinalysis: bilirubin positive, urobilinogen positive, others negative Questions and tasks: 1. Describe bilirubin metabolism. 2. What is the likely etiology? 3. What test can detect the etiology? 4. How is this infection transmitted? 5. How can be this infection prevented? 6. What is fulminant hepatitis? Pathophysiology: Classification of icterus and its pathophysiology Pathology: Viral hepatitis