Module 2. Clinical Pharmacy in gastroenterology, hepatology
advertisement
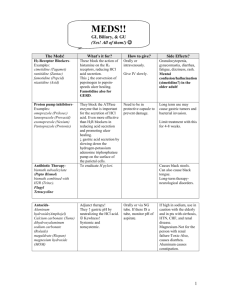
Module 2. Clinical Pharmacy in gastroenterology, hepatology, hematology, endocrinology, аllergology. Text test questions: 1. The major synthetic estrogens are following, EXCEPT: A. Dienestrol B. Diethylstilbestrol C. Benzestrol D. * Estradiol E. All of the above 2. Which of the following statements about estrogens are True: A. Estrogens are required for normal sexual maturation and growth of the female B. Estrogens decrease the rate of resorption of bone C. Estrogens enhance the coagulability of blood D. * All of the above E. None of the above 3. Indications of synthetic estrogens are following, EXCEPT: A. Primary hypogonadism B. Postmenopausal hormonal therapy C. Hormonal contraception D. * For treatment of simple obesity E. None of the above 4. Main complications of estrogens’ therapy include the following: A. Postmenopausal uterine bleeding B. Breast tenderness C. Hyperpigmentation D. * All of the above E. None of the above 5. Tamoxifen is: A. Antiprogestin B. Antiandrogen C. * Antiestrogen D. Androgen E. None of the above 6. Main contraindications of estrogens’ therapy include the following: A. Estrogen-dependent neoplasmas such as carcinoma of the endometrium or carcinoma of the breast B. Undiagnosed genital bleeding C. Liver disease D. * All of the above E. None of the above 7. Progesterone is secreted by: A. Ovarian follicles B. * Corpus luteum C. Granulosa and theca cells D. All of the above E. None of the above 8. The major natural progestin is: A. Estradiol B. Estron C. * Progesterone D. Estriol E. None of the above 9. Which of the following statements about progestins is True: A. Progesterone is rapidly absorbed following administration by any route B. In the liver, progesterone is metabolized to pregnanediol and conjugated with glucuronic acid. C. Significant amounts of progestins and their metabolites are excreted in the urine D. * All of the above E. None of the above 10. Noncontraceptive clinical uses of progestins are following: A. Hormone replacement therapy B. Dysmenorrhea C. Endometriosis D. * All of the above E. None of the above 11. All of the following statements about oral contraceptives are true, EXCEPT: A. The “combination pill” contains both estrogen and progestin B. Ethinyl estradiol and mestranol are commonly used in oral contraceptives C. The “minipill” contains progestin alone D. * The “triphasic pill” contains estrogen, progestin, and luteinizing hormine E. All of the above 12. The drug of choice for treatment of anaphylactic shock is: A. Noradrenaline. B. Naphthyzine. C. Isadrine. D. * Adrenaline. E. Anapriline. 13. Main effect of ganglion- blockers is: A. * Decrease of vessels’ tone. B. Increase of vessels’ tone. C. Decrease intraocular pressure. D. Analeptic action. E. Bronchial spasm. 14. What is the way of noradrenalin using? A. * Intravenous. B. Intramuscular. C. Per oral. D. Subcutaneous. E. Intracutaneous. 15. What is the effect of noradrenalin using? A. Vasodilating. B. * Vasoconstrictive. C. Bronchodilating. D. Bronchoconstrictive. E. Analeptic. 16. Which of the following agents is a respiratory analeptic? A. Piracetam B. Sydnocarb C. * Bemegride D. Pantocrin E. Morphine 17. Adaptogens cause: A. Improvement of efficiency using physical loads and acceleration of recovery after the load B. Stimulation of respiratory and vasomotor centers C. Temporary relief of the feeling of tiredness, facilitating the professional work and fighting somnolence D. * Increased resistance towards stress situations and adaptation to extreme conditions E. None of the above 18. Which of the following agents is a general tone-increasing drug of plant origin? A. Meridil B. * Eleuterococci’s extract C. Pantocrin D. Caffeine E. T-activin 19. Indicate a general tone-increasing drug, which is an agent of animal origin? A. * Pantocrin B. Amphetamine C. Sydnocarb D. Camphor E. All of the above 20. Cordiamine is useful in the treatment of: A. Hypotension B. Coronary insufficiency C. Respiratory insufficiency D. * All of the above E. None of the above 21. Tick the drug influencing the blood flow which is related to antiplatelet agents: A. Heparin B. * Aspirin C. Pyracetam D. Tanakan E. Indometacin 22. Which of the following drugs is related to anticoagulants and may be useful in disorders of cerebral circulation? A. Aspirin B. Trimetazidine C. Cinnarizine D. Nicergoline E. * Heparin 23. Antiaggregants are used in disorders of brain circulation for: A. Stimulation of the metabolic processes in neurons B. Dilation of cerebral vessels C. * Improving the microcirculation in cerebral tissue D. All the above E. None of the above 24. Immediate allergy reaction (type I allergic reaction) is: A. * An allergic or immune response that begins within a period lasting from a few minutes to about an hour after exposure to an antigen to which the individual has been sensitized B. An allergic reaction that becomes apparent only hours after contact C. An allergic reaction that results from the formation of antigen-antibody complexes between a foreign antigen and IgM or IgG immunoglobulins. (It occurs during blood transfusion reactions and in hemolytic disease of the newborn) D. An allergic reaction that is due to the presence of elevated levels of antigen-antibody complexes that cause tissue damage E. None of the above 25. Delayed allergy reaction (type IV allergic reaction) is: A. An allergic or immune response that begins within a period lasting from a few minutes to about an hour after exposure to an antigen to which the individual has been sensitized B. * An allergic reaction that becomes apparent only hours after contact C. An allergic reaction that results from the formation of antigen-antibody complexes between a foreign antigen and IgM or IgG. (It occurs during blood transfusion reactions and in hemolytic disease of the newborn) D. An allergic reaction that is due to the presence of elevated levels of antigen-antibody complexes that cause tissue damage E. All of the above 26. Immunodeficiency: A. A localized protective reaction of tissue to irritation, injury, or infection, characterized by pain, redness, swelling, and sometimes a loss of function B. * A disorder or deficiency of the normal immune response C. A disease resulting from an immune reaction produced by an individual's white blood cells or antibodies acting on the body's own tissues or extracellular proteins D. All of the above E. None of the above 27. H1 histamine receptor subtype is distributed in: A. * Smooth muscle, endothelium and brain B. Gastric mucosa, cardiac muscle, mast cells and brain C. Presynaptically in brain, mesenteric plexus and other neurons D. All of the above E. None of the above 28. H2 histamine receptor subtype is distributed in: A. Smooth muscle, endothelium and brain B. * Gastric mucosa, cardiac muscle, mast cells and brain C. Presynaptically in brain, mesenteric plexus and other neurons D. All of the above E. None of the above 29. Most tissue histamine is sequestered and bound in: A. Granules in mast cells or basophils B. Cell bodies of histaminergic neurons C. Enterochromaffin-like cell of the fondus of the stomach D. * All of the above E. None of the above 30. These categories of histamine H1 antagonists are noted for sedative effects, EXCEPT: A. * Piperidines; i.e. Loratadine, Fexofenadine B. Ethanolamines (aminoalkyl ethers); i.e. Dimedrol, Clistin C. Ethylenediamines; i.e. Suprastine D. Phenothiazines; i.e. Diprazine, Promethazine E. All of the above is true 31. Which category of histamine H1 antagonists is recognized for as second-generation antihistamines? A. Alkylamines (propylamines); i.e. Brompheniramine B. * Piperidines; i.e. Loratadine, Fexofenadine C. Ethylenediamines; i.e. Suprastine D. Phenothiazines; i.e. Promethazine E. None of the above 32. These histamine H1 antagonists are recognized for as second-generation antihistamines, EXCEPT: A. Astemizole B. desloratadine C. Loratadine (Claritin) D. Cetirizine (Zyrtec) E. * Suprastine 33. Indication for administration of histamine H1 antagonists is: A. Prevention or treatment of the symptoms of allergic reactions (rhinitis, urticaria) B. Motion sickness and vestibular disturbances C. Nausea and vomiting in pregnancy (“morning sickness”) D. * All of the above E. None of the above 34. Indications for administration of histamine H1 antagonists are the following EXCEPT: A. Prevention of the symptoms of allergic reactions B. Treatment of the symptoms of allergic reactions (rhinitis, urticaria) C. * Management of seizure states D. Nausea and vomiting in pregnancy (“morning sickness”) E. Treatment of sleep disorders 35. Side effect of first-generation histamine H1 antagonists is: A. Aplastic anemia B. Vomiting, tinnitus, C. Decreased hearing D. * Sedation E. Gastric ulcers and upper gastrointestinal bleeding 36. Immunosupressive effect of glucocorticoids is caused by A. * Reducing concentration of lymphocytes (T and B cells) and inhibiting function of tissue macrophages and other antigen-presenting cells B. Suppression of cyclooxygenase II expression that results in reducing amount of an enzyme available to produce prostaglandins C. Activation of phospholipase A2 and reducing prostaglandin and leukotriene synthesis D. All of the above E. None of the above 37. Antiallergic effect of glucocorticoids is caused by: A. Suppression of leukocyte migration and stabilizing lysosomal membranes B. Reverse the capillary permeability associated with histamine release C. Suppression of the immune response by inhibiting antibody synthesis D. * All of the above E. None of the above 38. The Immunosuppressive agent is: A. Corticosteroids B. Cyclosporine C. Tacrolimus (FK 506) D. * All of the above E. None of the above 39. Class of cyclosporine A is: A. Interferons B. * Immunosuppressive agents C. Monoclonal antibodies D. Immunoglobulins E. Glucocorticoids 40. Side effect of cyclosporine A is: A. Tremor B. GI disturbance C. Hepatotoxicity D. * All of the above E. None of the above 41. Side effect of cyclosporine A is: A. * Tremor B. Anorexia C. Chills D. Myalgia E. All of the above 42. Side effect of cyclosporine A is: A. Diarrhea B. Headache C. * GI disturbance D. Immunosuppression E. All of the above 43. Indication of cyclosporine A is: A. Secondary immunodeficiency B. Hairy cell leukemia C. Primary immunodeficiency D. * Idiopathic nephrotic syndrome E. All of the above 44. Class of I.V. IgG preparation is: A. Monoclonal antibodies B. Immunosuppressive agents C. Interferons D. * Immunoglobulins E. None of the above 45. Half-life of I.V. IgG preparation is: A. 25-35 minutes B. 19 hours C. 4 - 16 hours D. * 21 days E. 3 days 46. Mechanism of action of I.V. IgG preparation is: A. Inhibits CD3 receptor B. Inhibits calcineurin C. Complement-mediated cytolysis of T lymphocytes D. * Compete for Fc receptors with autoantibodies E. None of the above 47. Indication for I.V. IgG preparation administration is: A. Kaposi's sarcoma B. Acute rejection of organ transplant C. Condyloma acuminatum D. * Prophylaxis of certain infections E. Viral hepatitis 48. Cytotoxic agents are the following EXCEPT: A. Azathioprine B. * Cyclosporine C. Leflunomide D. Cyclophosphamide E. All of the above 49. Monoclonal antibodies is: A. Trastuzumab B. Rituximab C. OKT-3 D. * All of the above E. None of the above 50. The indication for interferon gamma administration is: A. Idiopathic nephrotic syndrome B. Hepatitis C virus infection C. * Chronic granulomatous disease D. Hairy cell leukemia E. Hepatitis B virus infection 51. The side effect of interferon gamma is: A. Hypertension B. Pulmonary edema C. Nephrotoxicity D. * Fatigue E. All of the above 52. Half-life of interferon gamma is: A. 21 days B. 19 hours C. 4 - 16 hours D. * 25-35 minutes E. 24 hours 53. Half-life of interferon alpha is: A. 18-24 hours B. * 4-16 hours C. 25-35 minutes D. 21 days E. 3 days 54. The indication for interferon alpha administration is: A. Hepatitis C virus infection B. Kaposi's sarcoma C. Condyloma acuminatum D. * All of the above E. None of the above 55. Indication for interferon alpha administration is: A. Autoimmune diseases B. Rheumatoid arthritis C. Organ transplantation D. * Hepatitis C virus infection E. None of the above 56. Indication for interferon alpha administration is: A. Prophylaxis of sensitization by Rh antigen B. Rheumatoid arthritis C. * Kaposi's sarcoma D. Chronic granulomatous disease E. Chronic pancreatitis 57. Immunomodulating agent is: A. Sirolimus (rapamycin) B. * Levamisole C. Tacrolimus D. All of the above E. None of the above 58. Mechanism of action of levamisole is: A. Inhibits CD3 receptor B. Complement-mediated cytolysis of T lymphocytes C. Substitution for patient's defiecient immunoglobulins D. * Increase the number of T-cells E. All of the above 59. Secretory products of pancreatic beta-cells are: A. Glucagon, proglucagon B. * Insulin, C-peptide, proinsulin, islet amyloid polypeptide (IAPP) C. Somatostatin D. Pancreatic polypeptide (PP) E. All of the above 60. Insulin is: A. A glycoprotein with a molecular weight of 6000 B. * A small protein with a molecular weight of 5808 having disulphide linkage C. A fructoolygosaccharide D. A catecholamine E. None of the above 61. Insulin is a polypeptide hence: A. It is resistant to destruction by gastric juice B. * It is destroyed by gastric juice C. It is not a polypeptide D. It is metabolized immediately by cellular enzymes E. None of the above 62. The primary reason for a physician to prescribe human insulin is that: A. It has a faster onset of action than other insulins B. It has a shorter duration of action than other insulins C. * It can be given to patients who have an allergy to animal insulins D. It is more effective in preventing the complications of diabetes than animal insulins E. All of the above 63. Diabetic coma is treated by the administration of: A. Insulin lente B. Glucose C. * Crystalline insulin D. Oral anti-diabetic drugs. E. All of the above 64. Sulphonylureas act by: A. Reducing the absorption of carbohydrate from the gut B. Increasing the uptake of glucose in peripheral tissues C. Reducing the hepatic gluconeogenesis D. * Stimulating the beta islet cells of pancreas to produce insulin E. All of the above 65. Currently used second-generation sulfonylureas include the following, EXCEPT: A. Glyburide (Glibenclamide) B. Glipizide (Glydiazinamide) C. Glimepiride (Amaril) D. * Tolbutamide (Orinase) E. All of the above 66. Currently used oral hypoglycemic thiazolidinediones include the following, EXCEPT A. Pioglitazone (Actos) B. Rosiglitazone (Avandia) C. * Troglitazone (Rezulin) D. All of the above E. None of the above 67. Thiazolidinediones act by: A. * Diminishing insulin resistance by increasing glucose uptake and metabolism in muscle and adipose tissues B. Reducing the absorption of carbohydrate from the gut C. Stimulating the beta islet cells of pancreas to produce insulin D. All of the above E. None of the above 68. Alpha-glucosidase inhibitors act by: A. Diminishing insulin resistance by increasing glucose uptake and metabolism in muscle and adipose tissues B. * Competitive inhibiting of intestinal alpha-ghucosidases and modulating the postprandial digestion and absorption of starch and disaccharides C. Reducing the absorption of carbohydrate from the gut D. Stimulating the beta islet cells of pancreas to produce insulin E. All of the above 69. Which of the following oral hypoglycaemic drugs stimulates both synthesis and release of insulin from beta islet cells: A. * Glibenclamide B. Phenformin C. Buformine D. Metformin E. All of the above 70. The action of insulin is potentiated by: A. Sulphonylureas B. Glucagon C. * Biguanides D. None of the above E. All of the above 71. Biguanides are used in the following conditions, EXCEPT: A. As a supplement to sulphonylurea, where it is insufficient to give good results B. In over weight diabetics C. To reduce insulin requirements D. * In case of hyperglycemic shock E. All of the above 72. Which of the following agents is/are important hormonal antagonists of insulin in the body? A. Glucagon B. Adrenal steroids C. Adrenaline D. None of the above E. * All of the above 73. Glucagon can be used in the following situations, EXCEPT: A. Severe hypoglycemia B. * Severe hyperglycemia C. Endocrine diagnosis D. Beta-blocker poisoning E. None of the above 74. Main complications of insulin therapy include the following: A. Hypoglycemia B. Insulin allergy C. Lipodystrophy at an injection site D. * All of the above E. None of the above 75. Tick the main approach of peptic ulcer treatment: A. Neutralization of gastric acid B. Eradication of Helicobacter pylori C. Inhibition of gastric acid secretion D. * All the above E. None of the above 76. Gastric acid secretion is under the control of the following agents EXCEPT: A. Histamine B. Acetylcholine C. * Serotonin D. Gastrin E. All of the above 77. Indicate the drug belonging to proton pump inhibitors: A. Pirenzepine B. Ranitidine C. * Omeprazole D. Trimethaphan E. Metoclopramid 78. Which of the following drugs is an agent of substitution therapy? A. Gastrin B. * Hydrochloric acid C. Hystamine D. Carbonate mineral waters E. Bradikinin 79. Choose the drug which is a H2-receptor antagonist: A. Omeprazole B. Pirenzepine C. Carbenoxolone D. * Ranitidine E. Loratadine 80. All of the following drugs are proton pump inhibitors EXCEPT: A. Pantoprozole B. Omeprazole C. * Famotidine D. Rabeprazole E. Esomeprazole 81. Indicate the drug belonging to M1-cholinoblockers: A. Cimetidine B. Ranitidine C. * Pirenzepin D. Omeprazole E. Pantoprazole 82. Which of the following drugs may cause reversible gynecomastia? A. Omeprazole B. Pirenzepine C. * Cimetidine D. Sucralfate E. Lansoprazole 83. Tick the drug forming a physical barrier to HCL and Pepsin: A. Ranitidine B. * Sucralfate C. Omeprazole D. Pirenzepine E. Loratadine 84. What term is used to describe a decrease in responsiveness to a drug which develops in a few minutes? A. Refractoriness B. Cumulative effect C. Idiosyncrazy D. Tolerance E. * Tachyphylaxis 85. Tachyphylaxis is: A. A drug interaction between two similar types of drugs B. * Very rapidly developing tolerance C. A decrease in responsiveness to a drug, taking days or weeks to develop D. An unexpected reaction to a drug E. None of the above 86. Idiosyncratic reaction of a drug is: A. A type of hypersensitivity reaction B. A type of drug antagonism C. * Unpredictable, inherent, qualitatively abnormal reaction to a drug D. Quantitatively exaggerated response E. The ability of a substance to cause cancer 87. Which drug is an analog of prostaglandin E1? A. * Misoprostol B. De-nol C. Sucralfate D. Omeprazole E. Ranitidine 88. Select the drug stimulating the protective function of the mucous barrier and the stability of the mucous membrane against damaging factors: A. De-nol B. Ranitidine C. * Misoprostol D. Omeprazole E. Gastrocepine 89. Most of drugs are antacids EXCEPT: A. * Misoprostol B. Maalox C. Mylanta D. Almagel E. Sodium bicarbonate 90. Indicate the drug that cause metabolic alkalosis: A. * Sodium bicarbonate B. Cimetidine C. Pepto-Bismol D. Carbenoxolone E. Maalox 91. Choose the drug that causes constipation: A. Sodium bicarbonate B. * Aluminium hydroxide C. Calcium carbonate D. Magnesium oxide E. None of the above 92. All of the following drugs stimulate appetite EXCEPT: A. Vitamins B. Bitters C. * Fepranone D. Insulin E. Caffeine 93. All of the following drugs intensify gastrointestinal motility EXCEPT: A. * Papaverine B. Metoclopramide C. Domperidone D. Cisapride E. Tegaserod 94. Choose an emetic drug of central action: A. Ipecacuanha derivatives B. Promethazine C. Tropisetron D. * Apomorphine hydrochloride E. None of the above 95. Tick the mechanism of Metoclopramide antiemetic action: A. H1 and H2-receptor blocking effect B. M-cholinoreceptor stimulating effect C. * D2-dopamine and 5-HT3-serotonin receptor blocking effect D. M-cholinoblocking effect E. H2-receptor blocking effect 96. Select the emetic agent having a reflex action: A. * Ipecacuanha derivatives B. Apomorphine hydroclorid C. Chlorpromazine D. Metoclopramide E. Ranitidine 97. All of the following drugs are antiemetics EXCEPT: A. Metoclopramide B. Ondansetron C. Chlorpromazine D. * Apomorphine hydrochloride E. None of the above 98. All of these drugs reduce intestinal peristalsis EXCEPT: A. Loperamide B. * Cisapride C. Methyl cellulose D. Magnesium aluminium silicate E. None of the above 99. The mechanism of stimulant purgatives is: A. Increasing the volume of non-absorbable solid residue B. * Increasing motility and secretion C. Altering the consistency of the feces D. Increasing the water content E. All of the above 100. Select the drug which inhibits peristalsis: A. Castor oil B. Bisacodyl C. * Loperamide D. Sorbitol E. 101. A. B. C. D. E. 102. A. B. C. D. E. 103. A. B. C. D. E. 104. A. B. C. D. E. 105. A. B. C. D. E. 106. A. B. C. D. E. 107. A. B. C. D. E. 108. A. B. C. D. E. 109. A. B. Mannit Choose the drug affecting the biliary system and relaxing Oddy sphincter: Cholosas Oxaphenamide * No-spa Cholenzyme Castor oil All of the following are normally involved in the pathogenesis of heart failure EXCEPT: A cardiac lesion that impairs cardiac output An increase in peripheral vascular resistance * A decrease in preload An increase in sodium retention An increase in water retention Which of these groups of drugs is used for asthma treatment? Methylxanthines M-cholinoblocking agents Beta2 – agonists Steroids * All of the above Tick the drug belonging to non-selective beta2-adrenomimics: Salbutamol * Isoprenaline Salmeterol Terbutaline All of the above Select the side effect characteristic for non-selective beta2-adrenomimics: Depression of the breathing centre * Tachycardia Peripheral vasoconstriction Dry mouth All of the above Pick out the bronchodilator drug related to xanthine: Atropine Ipratropium Orciprenaline Adrenaline * Theophylline Pick out the bronchodilator drug belonging to sympathomimics: Isoprenaline * Ephedrine Atropine Phormoterol Salbutamol The mechanism of methylxanthines action is: * Inhibition of the enzyme phosphodiesterase Beta2-adrenoreceptor stimulation Inhibition of the production of inflammatory cytokines Inhibition of M-cholinoreceptors Inhibition of COX-oxygenase Which of the following M-cholinoblocking agents is used especially as an anti-asthmatic? Atropine * Ipratropium C. Platiphylline D. Metacin E. None of the above 110. Indicate the side effect of Theophylline: A. Bradycardia B. * Increased myocardial demands for oxygen C. Depression of respiratory centre D. Elevation of the arterial blood pressure E. All of the above 111. All of the following drugs are inhaled glucocorticoids EXCEPT: A. Triamcinolone B. Beclometazone C. * Sodium cromoglycate D. Budesonide E. Fluticazone 112. Choose the drug belonging to membrane stabilizing agents: A. Zileutin B. * Sodium cromoglycate C. Zafirlucast D. Montelucast E. Budesonide 113. Indicate the drug which is a leucotriene receptor antagonist: A. Sodium cromoglycate B. * Zafirlucast C. Zileutin D. Triamcinolone E. Zopiclon 114. Indications of glucocorticoids are following, EXCEPT: A. Gastrointestinal diseases (inflammatory bowel disease) B. * Postmenopausal hormonal therapy C. Inflammatory conditions of bones and joints (arthritis, bursitis, tenosynovitis) D. Skin diseases (atopic dermatitis, dermatoses, localized neurodermatitis) E. All of the above 115. The main mechanism of most drugs absorption in GI tract is: A. Active transport (carrier-mediated diffusion) B. Filtration (aqueous diffusion) C. Endocytosis and exocytosis D. * Passive diffusion (lipid diffusion) E. None of the above 116. Pick out the appropriate alimentary route of administration when passage of drugs through liver is minimized: A. Oral B. Transdermal C. * Rectal D. Intraduodenal E. All of the above 117. Which route of drug administration is most likely to lead to the first-pass effect? A. Sublingual B. * Oral C. Intravenous D. Intramuscular E. Rectal 118. What is characteristic of the oral route? A. Fast onset of effect B. * Absorption depends on GI tract secretion and motor function C. A drug reaches the blood passing the liver D. The sterilization of medicinal forms is obligatory E. All of the above 119. In case of liver disorders accompanied by a decline in microsomal enzyme activity the duration of action of some drugs is: A. Decreased B. * Enlarged C. Remained unchanged D. Changed insignificantly E. Remained unchanged or changed insignificantly 120. The most specific agent for prevention of asthma is: A. * Salbutamolum B. Libexinum C. Adrenalini hydrochloridum D. Pertussinum E. Mucaltinum 121. Proposed cellular mechanisms of theophylline's action include: A. translocation of intracellular calcium B. those mediated by increasing accumulation of intracellular cyclic AMP C. those mediated by blockade of receptors for adenosine D. * All of the above E. None of the above 122. Theophylline clearance may be reduced by: A. phenobarbital B. warfarin C. tobacco smoking D. phenytoin E. * ciprofloxacin 123. Regarding its actions, cromolyn is best described as: A. bronchodilator B. anticholinergic C. beta agonist D. * inhibitor of mast cell degranulation E. glucocorticoid 124. Beta-2 selective adrenergic agonists include all EXCEPT: A. terbutaline B. albuterol C. metaproterenol D. * isoproterenol E. pirbuterol 125. Adverse effects of beta-2 adrenergic bronchodilators include all of the following EXCEPT: A. nervousness B. headache C. tachycardia D. tremulousness E. * lethargy 126. Which of the following work through cholinergic receptor antagonism? A. theophylline B. cromolyn C. ephedrine D. * ipratropium E. salmeterol 127. Which of the following pharmacologic agents antagonize adenosine? A. * theophylline B. glucocorticoids C. cromolyn sodium D. propranolol E. terbutaline 128. When comparing the relative adrenergic effects of the following drugs, the one which would have the bronchodilative effect at normal doses is: A. terbutaline B. epinephrine C. isoproterenol D. isoetharine E. * norepinephrine 129. Asthmatic patients could experience bronchoconstriction problems with which of the following agents? A. * isoproterinol (Isuprel) B. digoxin (Lanoxin) C. pindolol (Visken) – D. dextromethorphan E. labetalol 130. Which of the following can be administered orally and by inhalation? A. Epinephrine B. Albuterol C. Pirbuterol D. * Terbutaline E. Isoproterenol 131. Which of the following is not true about Salmeterol? A. administered by inhalation B. long acting anti-asthmatic with a duration of 12 hours C. * can lead to transient increase in PaO2, especially in poorly ventilated lung tissue D. associated with improvement in patients homozygous for glycine at the B-16 locus of the betareceptor E. none of the above 132. Which of the following is not true about Ipratropium bromide: A. Anticholinergic agent administered by inhalation B. better bronchodilator than Atropine C. * better anti-asthmatic than Epinephrine D. has no effect on mucocilliary clearance E. none of the above 133. Which of the following asthma severity categories has a treatment including inhaled low-dose steroid, cromolyn, nedocromil, zafirlukast or zileuton? A. Mild intermittent asthma B. * Mild persistent asthma C. Moderated persistent asthma D. Severe persistent asthma E. Exercise-induced asthma 134. Which of the following, along with Formoterol, is a long acting anti-asthmatic? A. Albuterol B. * Salmeterol C. D. E. 135. A. B. C. D. E. 136. A. B. C. D. E. 137. A. B. C. D. E. 138. A. B. C. D. E. 139. A. B. C. D. E. 140. A. B. C. D. E. 141. A. B. C. D. E. 142. A. B. C. D. E. 143. Metaproterenol Terbutaline Pirbuterol Which of the following is a short acting leukotriene synthesis (5-lipoxygenase) inhibitor? * Zileuton Zafirlukast Montelukast Omalizumab Theophyline Which one of the following drugs is a selective beta2-agonist? Epinephrine Norepinephrine * Salbutamol Isoproterenol Dobutamine Which of the following antibiotics is most closely associated with the development of hepatitis? kanamycin penicillin G tetracycline * isoniazid ethambutol Isoniazid-induced liver damage: occurs primarily in patients under 30 years of age occurs with increased frequency in patients receiving concomitant ethambutol therapy * is probably due to the formation of a toxic hydrazine metabolite that binds to liver protein is frequently associated with allergic manifestations such as eosinophilia, fever, and rash All of the above Cromolyn, regarding its actions, is best described as: bronchodilator anticholinergic beta agonist * inhibitor of mast cell degranulation glucocorticoid Indicate the group of drugs, stimulating intestine motility * Anticholinesterases M-cholinoblockers Ganglioblockers Amara (bitters) Anorexigenous Indicate the group of drugs, oppressing intestine contraction M-cholinomimetics * M-cholinoblockers Anticholinesterases N-cholinomimetics Adrenoblockers The indications for prescribing of H2 – histamine blockers Hypoacidic gastritis Anorexia Acute cholecystitis * The ulcerous disease of the stomach and duodenum Stomatitis Which drug belongs to the antacid? A. B. C. D. E. 144. A. B. C. D. E. 145. A. B. C. D. E. 146. A. B. C. D. E. 147. A. B. C. D. E. 148. A. B. C. D. E. 149. A. B. C. D. E. 150. A. B. C. D. E. 151. A. B. C. D. * Aluminii hydroxydum Ranitidin Atropine sulfas Cimetidine Pancreatinum Ranitidine, drug used for treatment of ulcer disease, block GABA-receptors Adrenergic receptors M-cholinoreceptors * H2-histamine receptors N-cholinoreceptors Which drug belongs to the laxatives? Pepsin * Radicis Rhei Ranitidin Atropine sulfas Apomorphinum Which of the following substances has its major activity as a saline cathartic? sodium bicarbonate methylcellulose * sodium phosphate castor oil mineral oil The correct statement regarding sucralfate: pharmacologic action is to reduce gastric acid secretion by antagonizing gastrin enhances N+-K+ ATPase antagonizes acetylcholine * most common side effects is constipation increases gastric motility Correct statement regarding metoclopramide: central nervous system dopamine receptor agonist peripheral blockage of acetylcholine at muscarinic synapse decreases lower esophageal sphincter pressure * adverse effects include dystonic or extrapyramidal effects increases motility of colon In general, mechanisms of laxation include: adding bulk to the stool increasing peristaltic activity emulsifying aqueous and fatty substances with stool lubricating the passage of stool * All of the above Appropriate indications for and/or uses of laxatives include: prevent straining at the stool in patients with cardiovascular disease bulk forming agents for diverticular disease treatment of drug overdose * All of the above None of the above Which of the following substances is most likely to cause systemic alkalosis? * sodium bicarbonate methylcellulose sodium phosphate castor oil E. mineral oil 152. Saline cathartics, such as sodium sulfate or magnesium sulfate: A. are safe in patients with renal failure B. are readily absorbed from the gastrointestinal tract C. are slower acting than bulk-forming laxatives D. * act by increasing intestinal volume, hence stimulating peristaltic action E. lower the surface tension of the feces to facilitate fecal hydration 153. Adverse effect(s) of laxatives: A. electrolyte disturbances (hypernatremia, hypokalemia) B. dehydration C. spastic colitis with stimulant laxatives D. gastrointestinal obstruction with bulk forming agents E. * All of the above 154. In esophagitis, elevation of the head of the bed, abstinence from ethanol and tobacco, and small frequent meals are all useful adjunctive therapeutic measures. Other useful therapy may include all of the following EXCEPT: A. omeprazole B. metoclopramide C. maalox D. cimetidine E. * amitriptyline 155. Drug which exerts anti-peptic ulcer effects through histamine-2 receptor antagonism: A. sucralfate B. * ranitidine C. metoclopramide D. omeprazole E. Misoprostol 156. The substance which is principally an emollient laxative is: A. bran B. methylcellulose C. magnesium hydroxide D. phenolphthalein E. * mineral oil 157. Agents of potential use in peptic ulcer disease include: A. muscarinic antagonists B. proton pump inhibitors C. antacids D. prostaglandins E. All of the above 158. Possible drug interactions: Aluminium hydroxide antacids tend to interfere with the gastrointestinal absorption of: A. cephalexin B. penicillin G C. erythromycin D. chloramphenicol E. * tetracycline 159. Indicate which of the following substances has its major activity as a stimulant cathartic A. sodium bicarbonate B. methylcellulose C. sodium citrate D. * castor oil E. mineral oil 160. One mechanism to reduce gastric acid secretion is by blocking the K+-Na+ATPase pump in the parietal cell. One drug that has this pharmacologic action is: A. misoprostol B. pirenzepine C. * omeprazole D. serotonin E. isoniazid 161. The amount of sodium, phosphate or magnesium contained in an antacid should be assessed when selecting an antacid for patients with: A. renal insufficiency B. congestive heart failure C. ascitis D. * All of the above E. None of the above 162. The concomitant administration of calcium and/or magnesium antacids to patients receiving one of the tetracycline drugs may have which of the following effects upon the action of the tetracycline: A. enhances the action B. causes no significant change C. * decreases the action D. increases toxicity E. suppresses hypersensitivity reactions 163. Which of the following substances has its major activity as a saline cathartic? A. Sodium bicarbonate B. Aluminium hydroxide C. * Magnesium sulfate D. Calcium carbonate E. All of the above 164. All these Drugs are cause obstipation Except: A. Anticholinergic agents B. Ca2+ channel antagonists C. Opioids D. Tricyclic antidepressants E. * Muscarinic agonists 165. Plant fiber (a laxative, purgative) A. Decrease the bulk of the stools B. increases the bowel transit time C. * slowly distends the wall of the colon D. increases the effective caloric content of the diet E. takes down water and swells 166. Lactulose A. is a monosaccharide B. is broken down in the small intestine by bacteria C. is build to unabsorbed organic anions which retain fluid D. produces laxative effects after 2-3 hours E. * is of particular value in the treatment of hepatic encephalopathy 167. Lactulose is of particular value in the treatment of encephalopathy: A. * as it discourages the proliferation of ammonia producing organisms B. as it increases the absorption of ammonia C. as it decreases chronic portal hypertension D. as it treatment fever E. as it improves functions of CNS after absorption from the GIT 168. A. B. C. D. E. 169. A. B. C. D. E. 170. A. B. C. D. E. 171. A. B. C. D. E. 172. A. B. C. D. E. 173. A. B. C. D. E. 174. A. B. C. D. E. 175. A. B. C. D. E. 176. A. B. Magnesium sulfate is a laxative which acts within 1-2 days dilates the gallbladder and relaxes the sphincter of Oddi decreases the secretion of cholecystokinin decreases gastric, intestinal and pancreatic secretion * should be given in dilute solution to a fasting individual Senna alcaloids (anthraquinones) * act directly on the intramucosal plexus of the gut wall take about 8 minutes to produce an effect should be given to pregnant women should be given to nursing mothers can not induce diarrhea with excessive loss of water and electrolytes Glycerol (in the form of rectal suppositories) is useless if a rapid effect is required * acts as a rectal stimulant due to local irritant action cannot be used in children rectal suppositories promote colonic evacuation in 30 hours exerts severe diarrhea with loss of water and electrolytes In the treatment of acute diarrhea antibiotics are worst avoided in non-pathogenic diarrhea antibiotics are worst avoided in viral gastroenteritis oral rehydration should not be used for initial therapy electrolytes and glucose should not be supplemented for initial therapy * oral rehydration and electrolytes supplementation are required particularly in children and in the elderly All these drugs are increasing intestinal transit time Except: codeine (an opioid) morphine (an opioid) loperamide diphenoxylate * fysostigmin Peptic ulcer disease is an acute disorder * characterized by frequent recurrences comprises bones the incidence of duodenal ulcers is four to five times lower than that of gastric ulcer affects approximately 50% of the population All these are major factors of known importance for the etiology of ulceration Except acid-pepsin secretion mucosal resistance to attack by acid and pepsin * the age effects of non-steroidal anti-inflammatory drugs the presence of Helicobacter pylori Acid secretion is produced by endocrine cells in the gastric antrum cells * is stimulated by gastrin is inhibited by acetylcholine is inhibited by histamine is stimulated by prostaglandin E Antacids: * react with gastric acid to form a neutral salt produce sweating C. D. E. 177. A. B. C. D. E. 178. A. B. C. D. E. 179. A. B. C. D. E. 180. A. B. C. D. E. 181. A. B. C. D. E. 182. A. B. C. D. E. 183. A. B. C. D. E. 184. A. B. C. D. E. 185. are Ineffective at healing duodenal ulcer are very effective at healing gastric ulcers its effect on acid secretion lasts for long (5 hours) Antacids include: misoprostol orlistat cimetidine sucralfate * aluminium salts (hydroxide, phosphate, glycinate) Sodium bicarbonate (an antacid) acts only locally * excessive doses produce systemic alcalosis produces carbon monoxide by reacting with hydrochloric acid causes belching and distension of the large intestine sodium intake need not to be considered in patients with hypertension or heart failure Magnesium and aluminium salts do undergo absorption so are effective locally magnesium salts are constipating, aluminium salts may produce diarrhea can not reduce the rate and extent of absorption of other drugs aluminium salts should not be used with caution with any renal compromise * magnesium and aluminium salts are taken 1-3 hours after meals and at bedtime H2 lytics: at least 4 days treatment is required to achieve healing pain is relieved within 4 weeks treatment include morphine , tramadol * include nizatidine, ranitidine, famotidine include pirenzepine Ranitidine (ZANTAC) has higher affinity for cytochrome P 450 than cimetidine is less expensive than cimetidine * is preferable to cimetidine in the elderly has a similar profile of action to paracetamol increases the plasma levels of theophylline Pirenzepine * is an M1 muscarinic receptor antagonist can not cause mild difficulty with accomodation and dry mouth can not alter the rate of absorption of other drugs if given concurrently can be used in patients with concomitant glaucoma can be used in patients with pyloric stenosis and prostatic enlargement Omeprazol is an irreversible stimulator of the proton pump can be used only for healing gastric ulcer Is for women only is taken once weekly * degrades in the presence of moisture. Capsules are supplied in special containers Misoprostol * is a synthetic analog of prostaglandin E1 produces gastric acid secretion causes Stricture in the submucosa decreases production of protective mucus is indicated especially in pregnancy Sucralfate A. B. C. D. E. 186. A. B. C. D. E. 187. A. B. C. D. E. 188. A. B. C. D. E. 189. A. B. C. D. E. 190. A. B. C. D. E. 191. A. B. C. D. E. 192. A. B. C. D. E. 193. A. B. C. D. is less effective than cimetidine is not so effective in symptom relief antacids are contraindicated contains aliminium, diarrhea can not be induced * in severe renal failure accumulation is a potential hazard. Cisapride inhibits motility of the GIT decreases rate of gastric emptying is not used in gastroesophageal reflux * is used in dyspepsia and delayed gastric emptying is used in diarrhea Metoclopramide is effective for: preoperative vomiting vestibular disturbances motion sickness headache * facilitation of duodenal intubation and endoscopy Constipation results from increased peristaltic activity in the intestinal tract. occurs only if one does not have a bowel movement at least once a day. leads to decreased salt and water absorption from the large intestine. * symptoms can be artificially induced by increasing the volume of the large intestine. All of the above The pancreas is only an endocrine gland. secretes enzymes in response to an increased plasma glucose concentration. * neutralizes the hydrochloric acid secreted by the stomach. produces bile. None of the above Gastrin * stimulates acid secretion in the stomach. secretion is blocked by the products of protein digestion in the stomach. secretion is stimulated by acid in the duodenum. is responsible for the chemical or gastric phase of intestinal secretion. stimulates acid secretion in the intestine. The activities of the GI tract, movement and secretion, are controlled by the sympathetic nervous system. the parasympathetic nervous system. * local nerve reflexes initiated in the nerve plexus layer of the GI tract. the medulla. All of the above The presence of fat in the duodenum causes acid indigestion. decreased acid production. increased gastrin release. * contraction of the gallbladder. None of the above The basic type of movement that occurs in the small intestine is peristalsis. mass movement. churning. * segmentation E. all of the above 194. Most of the nutrients absorbed from the GI tract pass immediately into the portal venous system and are processed by the liver. This is possible because almost all absorption occurs through A. the lower section of the stomach. B. the top section of the large intestine. C. * the small intestine. D. the ileum. E. All of the above 195. Histamine-2 antagonists act to A. block the release of gastrin. B. selectively block histamine receptors, reducing swelling and inflammation. C. * selectively block H2 receptor sites, leading to a reduction in gastric acid secretion and reduction in overall pepsin production. D. are effective only with long-term use. E. none of the above 196. H2 receptors are found throughout the body, including A. in the nasal passages, upper airways, and stomach. B. in the CNS and upper airways. C. in the respiratory tract and the heart. D. * in the heart, CNS, and stomach. E. In the lungs 197. The H2 receptor blocker of choice for a patient with known liver dysfunction would be A. cimetidine. B. famotidine. C. * nizatidine. D. ranitidine. E. None of the above 198. Acid rebound is a condition that occurs when A. * lowering gastric acid to an alkaline level stimulates the release of gastric acid. B. raising gastric acid levels causes heartburn. C. combining protein, calcium, and smoking greatly elevates gastric acid levels. D. eating citrus fruit neutralizes gastric acid. E. All of the above 199. Misoprostol (Cytotec) is a prostaglandin that is used to A. prevent uterine contractions. B. * prevent NSAID-related gastric ulcers in patients at high risk. C. decrease hyperacidity with meals. D. relieve the burning associated with hiatal hernia at night. E. All of the above 200. The rate of drug absorption is greatest in: A. * The small intestine B. The large intestine C. The stomach D. All of the above E. The small intestine & the large intestine 201. Which of the following antibiotics is a tetracycline? A. Chloramphenicol B. * Doxycycline C. Streptomycin D. Erythromycin E. None of the above 202. Drug distribution may depend on tissue perfusion: A. B. C. D. E. Highly vascular organs rapidly acquire a drug Highly vascular organs acquire a drug slowly Levels of a drug in bone may rise quickly due to its high vascularity Levels of a drug in bone may rise slowly due to its reduced vascularity * Highly vascular organs rapidly acquire a drug & levels of a drug in bone may rise slowly due to its reduced vascularity 203. Correct statements about glucocorticoids include all of the following, EXCEPT: A. Effects of glucocorticoids are mediated by widely distributed glucocorticoid receptors that are members of the superfamily of nuclear receptors. B. Glucocorticoids have dose-related metabolic effects on carbohydrate, protein, and fat metabolism. C. * Glucocorticoids have pro-inflammatory effects. D. Glucocorticoids have catabolic effects in lymphoid and connective tissue, muscle, fat, and skin. E. Glucocorticoids have antiallergic effects 204. A drug allergy occurs: A. When too much drug has accumulated in an individual B. * When the body sees the drug as an antigen and an immune response is established against the drug C. An unwanted but predictable response to a drug D. None of the above E. All of the above 205. H. pylori is known to be a common cause of both duodenal and gastric ulcers, in a patient affected by H. pylori, the current regimen of choice is a two week course of triple therapy with Bismuth, Tetracycline and A. Loperamide B. Cimetidine C. * Metronidazole D. Pirenzepine E. Sucralfate 206. H2 antagonists are markedly safe drugs and relatively have a low incidence of side-effects. The most common side-effects being diarrrhoea, confusion and headaches and excitement in elderly patients, but one has weak anti-androgenic effects that can result in gynecomastia and impotence. What drug is this A. * Cimetidine B. Despramine C. Famotidine D. Nizatidine E. Ranitidine 207. An inexpensive H2 antagonist known to interfere with a wide variety of drugs metabolized by multiple forms of P-450 A. * Cimetidine B. Famotidine C. Nizatidine D. Ranitidine E. Loratadine 208. What additional agent, in addition to a H2 antagonist and PPI, could help treat oesophagitis by coating necrotic tissue with a protective barrier and thereby promote healing of the ulcer A. Calcium Carbonate B. Diphenoxylate C. Loperamide D. Pirenzepine E. * Sucralfate 209. Metoclopramide exerts its effects on the lower oesophageal sphincter tone and increases the rate of GI emptying and has anti-emetic effect by serving as A. Anti-Histamine B. Cholinergic stimulant C. Dopamine D2 antagonist D. GI Irritant E. * Cholinergic stimulant & Dopamine D2 antagonist 210. Antibiotic's clearance from the body most likely influenced by severe hepatic disease: A. Penicillins B. clindamycin (Cleocin) C. rifampin (Rimactane) D. * clindamycin & rifampin E. None of the above 211. While H2 antagonists can reduce 24hr acid secretion by 60-70%, a class of drugs can that are much more effective inhibitors of acid secretion by >90% are A. Cimetidine B. Metronidazole C. Misoprostol D. * Omeprasol E. Sucralfate 212. Which of these diseases is associated with chronic diarrhea? A. Celiac disease B. Irritable bowel syndrome C. Diabetes D. Asthma E. * Celiac disease & irritable bowel syndrome 213. Indication for glucocorticoids is: A. Chronic (Addison’s disease) and acute adrenocortical insufficiency B. Organ transplants (prevention and treatment of rejection – immunosuppression) C. Inflammatory conditions of bones and joints (arthritis, bursitis, tenosynovitis). D. * All of the above E. None of the above 214. Diarrhea is defined as ____ or more loose stools per day A. 1 B. 2 C. * 3 D. All of the above E. None of the above 215. Patients with cholera pass stools that resemble _____. A. * Rice water B. Stools with blood C. Anchovy sauce D. Apple jelly E. All of the above 216. The most common complication of diarrhea is _____. A. Intestinal perforation B. * Dehydration C. Septicemia D. Seizures E. All of the above 217. Signs of dehydration are A. Sunken eyes B. Excessive thirst C. Reduced urination D. * All of the above E. None of the above 218. Which of these are signs of anemia? A. * Pale gums B. Dark circles under the eyes C. Bleeding D. Numbness in hands and feet E. All of the above 219. To note vitamin which stimulates hemopoesis. A. Tocoferolum. B. Ergocalciferolum. C. * Cyanolocobalaminum. D. Retinolum. E. Riboflavin. 220. To name a vitamin drug, which is antagonist of indirect action anticoagulants. A. * Vitamin К. B. Tocoferolum. C. Tiamin. D. Cyanolocobalaminum. E. Riboflavin. 221. Which drug is basic for the medical treatment of pernicious megaloblastic anaemia? A. * Cyanocobalaminum. B. Folic acid. C. Fercoven. D. Coamid. E. Iron lactase. 222. Cyanocobalamin (vitamin B12) is indicated for the treatment of: A. Acute lymphocytic leukemia. B. * Pernicious anemia. C. Bone marrow suppression. D. Optic nerve atrophy. E. All of the above. 223. What drug from the narcotic analgesic group does have the least ulcer action? A. Butadion. B. Voltaren. C. Indometacin. D. * Meloxicam. E. Naproxen. 224. In oncologic patient the cellular immunity decreased after the radial therapy. Prescribe the proper drug. A. Prodigiosan. B. Interferon. C. * Т-aktivin. D. Betaferon. E. Reaferon. 225. Immunodepressive action of prednisolon is due to: A. Activating a synthesis of inhibitors of proteases. B. Depression of collagen production. C. * Decreasing of Т-lymphocytes level in the blood, limitation of cytotoxic influence of Тlymphocytes (killers) on В-lymphocytes. D. Depression of synthesis of mucopolysacharides. E. Decreasing of activity of plasmin. 226. Nonsteroid anti-inflammatory drugs are effective in case of medical treatment of rheumatism thanks to their power to depress: A. * Cyclooxygenase-2. B. Phospholipase-А2. C. Cyclooxygenase-1. D. Adenilatcyclase. E. Peroxydase. 227. Most nonsteroidal antiinflammatory drugs (NSAIDs) work by: A. Ameliorating pain perception. B. Increasing the supply of natural endorphins. C. Increasing blood flow to painful areas. D. * Inhibiting prostaglandin production. E. Stimulate prostaglandin production. 228. The advantage of cyclooxygenase-2 (COX-2) inhibitors over other NSAIDs is that they: A. Have a longer duration of action. B. Are less likely to cause hepatic toxicity. C. * Do not decrease the cytoprotective lining of the stomach. D. Have a more rapid onset of action. E. Decrease the cytoprotective lining of the stomach. 229. What agent is used for hemorrhagic diatheses treatment? A. Vit. A. B. Vit. C. C. Vit. E. D. * Vit. K. E. Vit. D. 230. What preparation belong to antifibrinolytic? A. * Acidum aminocapronicum. B. Pantothenic acid. C. Proserinum. D. Acidum salicylicum. E. Acidum nicotinicum. 231. Examples of autoimmune diseases A. rheumatoid arthritis B. insulin-dependent diabetes mellitus C. systemic lupus erythematosis D. none of the above E. * all above 232. Glucocorticoid effects: A. inhibition of leukotriene production B. inhibition of prostaglandins C. increased chemotaxis D. * inhibition of leukotriene production & inhibition of prostaglandins E. all of the above 233. Alkylating agent; destroys proliferating lymphoid cells; in low doses -- for effective against autoimmune disorders including systemic lupus erythematosus A. azathioprine (Imuran) B. methotrexate C. * cyclophosphamide (Cytoxan) D. antilymphocyte globulin (ALG) E. all the above 234. Cytotoxic agents with immunosuppressive properties: A. cyclophosphamide (Cytoxan) B. vincristine (Oncovin) C. methotrexate D. cytarabine (ARA-C) E. * all the above 235. Structural analog/antimetabolite: cytotoxic immunosuppressive drug: A. vincristine B. cyclophosphamide C. * azathioprine D. none of the above E. all of the above 236. Clinical uses of immunosuppressive drugs: A. organ transplantation B. hemolytic disease of the newborn C. autoimmune disorders D. none of the above E. * all of the above 237. The following is not true about corticosteroids: A. have anti-inflammatory activity B. highly lipophillic C. decrease the quantity and viscosity of mucus secretions D. * decrease the synthesis of adrenergic mediators E. decrease the transcription of genes coding for pro-inflammatory cytokines 238. Which of the following drugs used in the treatment of gout acts by preventing the migration of granulocytes: A. Allopurinol B. Sulfinpyrazone C. * Colchicine D. Indomethacin E. Cyclosporine 239. Etanercept produces its antirheumatic effects by direct A. Inhibition of cAMP phosphodiesterase in monocytic lineage leukocytes B. Selective inhibition of COX-2 C. Enhancement of leukotriene synthesis at the expense of prostaglandin synthesis D. * Reduction of circulating active TNF-alpha levels E. Inhibition of the production of autoantibodies 240. Status asthmaticus is best described by which of the following statements? A. Status asthmaticus is well-controlled asthma. B. * Status asthmaticus is a life-threatening exacerbation of asthma. C. Status asthmaticus is best treated with inhaled controller medication, such as cromolyn sodium or a leukotriene modulator. D. Status asthmaticus always resolves without drug treatment. E. Status asthmaticus occurs without warning in patients whose asthma symptoms are stable and well controlled. 241. The standard treatment regimen for asthma is best described by which of the following? A. Theophylline and exercise B. Inhaled beta2-adrenoceptor agonists only C. Inhaled corticosteroids only D. * A combination of inhaled bronchodilators and inhaled corticosteroids E. Oral corticosteroids 242. Gastric acid secretion is stimulated by the presence of A. B. C. D. E. * Gastrin and acetylcholine Histamine and motilin Norepinephrine and gastrin Norepinephrine and histamine Acetylcholine and pepsin Situational tasks: 1. Ditiline (lystenone) injected to patient before operation and intubation conducted. After operation 2. 3. 4. 5. 6. and stopping an anesthesia the independent breathing did not resume. Defect of what enzyme at the patient’s organism does lengthen the duration myorelaxants’ action? A. * Butirilcholinesterase of blood B. Succinatedehydrogenase C. Carboanhydrase D. N-acetyltransferase E. К-Nа-АТP–ase The problem of skeletal muscle contraction exist at child after poliomyelitis. What medicine is possible to prescribe? A. * Galantamine hydrobromide B. Platyphylline C. Methacine D. Atropine sulfate E. Tubacurarine For the patient with the femur fracture, for reducing of sceletal muscles tension during reposition of bone, it is necessary to prescribe short acting myorelaxant. A. * Dithyline B. Anapriline C. Tubacurarine D. Atropine E. Adrenaline After operation of reposition of femur fracture when Tubacurarine was used, breathing of patient did not resume. What is necessary to inject? A. * Proserine B. Platyphylline C. Cyclodole D. Atropine E. Acetylcholine At the patient after the short surgical operation with Dithyline after 30 minutes the depression of breathing appeared, the tonus of muscles did not renewal. What is necessary to prescribe to this patient? A. * Blood transfusion B. Hemodialysis C. Hemosorbtion D. Forced diuresis E. Peritoneum dialysis At the patient after the short surgical operation with Dithyline after 30 minutes the depression of breathing appeared, the tonus of muscles did not renewal. The absence of what enzyme in the blood serum caused this state? A. * Butirilcholinesterase B. Catalase C. Acetylcholinesterase D. Glucoso-6-phosphatase 7. The man appeared at the trauma department with diagnosis: fracture of femur with displacement. 8. 9. 10. 11. 12. For reposition of bone physician used 10 ml of 2 % solution of Dithyline i/v, as a result protracted apnoe and myorelaxation developed. Deficit of what enzyme caused such pharmacogenetic enzymepatia? A. * Pseudocholinesterase B. Uridindiphosphoglucoronic transferase C. Glucoso-6-phosphatdehydrogenase D. Met-hemoglobinreductase E. N-acetyltransferase Patient with the acute stomach-ache, vomit, heavy breathing, shortness of breath, delivers in intensive therapy. At the review of patient - skin moisture, hypersalivation, myosis, bradycardia, muscular fascilation. From anamnesis it is known, that patient – toxin abuse, used the aerosols to insects. To which group of agents, the substance that caused poisoning, belong? A. N-cholinomimetic B. М-choliniblockers C. Myorelaxants D. Ganglion-blockers E. * Anticholinesterase agents Patient with the complaints to dizziness, nausea, salivation and spastic stomach-aches was delivered to the hospital. The diagnosis set: poisoning by the phosphor organic substance. What must be included to the complex therapy? A. * Atropine sulfate and Dipirixim B. Tiosulfate sodium and Bemegridum C. Tetacin-calcium and Unitiolum D. Nalorphine hydrochloride and Bemegridum E. Glucose and Bemegridum The child by chance drank from the small bottle solution, which its grandmother used for the medical treatment of glaucoma. It appeared, there was pilocarpinum hydrochloridum. The doctor prescribed to the child an atropine sulfate. What mechanism lies in the basis of antydote action of atropine? A. * Influence on special receptors B. Co-operation with cellular metabolits C. Physico-chemical D. Antienzymic E. Enzymic The 6 years old child got in hospital with the acute express symptoms of motive and linguistic excitation, dryness in mouth, the bad swallowing, hoarse voice. A skin was dry, hot. Pupils were extended, photophobia, tachycardia. From anamnesis it is known, that child eat some berries of dark-violet color. Influencing of what toxic substance is cause of poisoning? A. * Atropine B. Pirenzepine C. Pilocarpine D. Platyphylline E. Methacine The patient with severe allergic bronchial asthma has been treated by oral drug during 7 months. Hypertension, “moon face”, obese trunk, oedema, insomnia occur. What drugs does he used? A. * Patient used one of orally used glucocorticoids, e.g. prednisolonum. B. Patient used one of beta-agonists. C. Patient used cromolynum. D. Patient used euphyllinum E. Patient used all above. 13. A 41-year-old man was admitted to the surgical department with the symptoms of acute 14. 15. 16. 17. 18. 19. 20. pancreatitis: vomiting, diarrhea, bradycardia, hypotention, weakness, dehydration of the organism. What medicine should be used first of all? A. Etaperazine B. No-spa C. Platyphylline D. Ephedrine E. * Contrycal A patient receiving intravenous cimetidine (Tagamet) for an acute ulcer problem needs to be monitored for A. GI upset. B. gynecomastia. C. * cardiac arrhythmias. D. constipation. E. Disbacteriosis A nurse taking care of a patient who is receiving a proton pump inhibitor should teach the patient A. to take the drug after every meal. B. to chew or crush tablets to increase their absorption. C. * to swallow tablets or capsules whole. D. to stop taking the drug after 3 weeks of therapy. E. to take the drug in the first part of day Woman (60 years old), that suffers by arthritis of hip joint, took butadion for a long time. After blood analysis the doctor abolished this drug. What complication did butadion cause? A. * Agranulocytosis. B. Anemia. C. Leukemia. D. Tromboembolic syndrome. E. Disturbance of hemocoagulation. Ms. Jones takes fexofenadine 60 mg twice a day for seasonal allergies. She comes to her physician with a sinus infection and receives a prescription for erythromycin, a drug known to inhibit CYP3A4. As a result of this drug interaction, you would expect Ms. Jones to A. * Exhibit no changes in fexofenadine elimination B. Exhibit decreased metabolism of erythromycin, with potential toxicity C. Be at risk for development of torsades de pointes, due to decreased metabolism of fexofenadine D. Exhibit decreased elimination of fexofenadine without risk of torsades de pointes E. Exhibit moderate anticholinergic effects commonly seen with fexofenadine Mr. Smith has severe motion sickness during air travel. He will be flying to Brazil next week, and you would like to prescribe an antihistamine to prevent motion sickness. Which of the following would be most effective? A. Scopolamine B. * Dimenhydrinate C. Chlorpheniramine D. Fexofenadine E. Tripelennamine A 36-year-old woman with severe erosive esophagitis is prescribed pantoprazole. One of the most common adverse side effects of such therapy is which of the following? A. Vomiting B. Constipation C. * Headache D. Heartburn E. Paresthesias While taking a NSAID for arthritis, a 65-year-old man developed a gastric ulcer. He was prescribed ranitidine for 8 weeks. This drug binds a receptor located where? A. Nucleus B. Nucleolus C. Cytoplasm D. * Cell membrane E. Cell wall 21. A 20-year-old woman goes to the emergency department, stating that within the past hour she ingested “a handful of sleeping pills.” She is still awake. Which of the following drugs can be given to induce vomiting? A. Metoclopramide B. * Ipecac C. Morphine D. Promethazine E. Ondansetron 22. A 17-year-old boy with a history of sulfa allergy is diagnosed with left-side ulcerative colitis after a 3-week history of bloody diarrhea and tenesmus. On examination he is afebrile and has no abdominal tenderness. The appropriate drug therapy to institute initially is which of the following? A. Metronidazole B. Sulfasalazine C. * Mesalamine D. Cyclosporine E. Prednisone